Abstract
Schistosoma mansoni disease is endemic in most parts of rural Zambia, and associated complications are common. We conducted a cross-sectional study among 754 people in rural communities of Kaoma District, western Zambia to determine the burden of S. mansoni infection and associated morbidity. Parasitology and ultrasonography assessments were conducted on consenting participants. The overall prevalence of S. mansoni infection and geometric mean egg count (GMEC) were 42.4% (304) and 86.6 eggs per gram (95% confidence interval = 75.6–99.6), respectively. Prevalence was highest in the age group of 15–19 years old (adjusted prevalence ratio = 1.70, P = 0.017). S. mansoni-related portal fibrosis was detected in 26% of the participants screened. Participants above 39 years old were 2.93 times more likely to have fibrosis than the 7–9 years old age group (P = 0.004). The study highlights the high burden of S. mansoni disease in this area and calls for immediate interventions to avert complications associated with the disease.
Introduction
Human schistosomiasis (or bilharzia) is a chronic and debilitating neglected parasitic disease affecting approximately 200 million people worldwide, of which 88% of the infections occur in sub-Saharan Africa.1 Schistosomiasis is the second leading parasitic disease after malaria in terms of public health importance.2 It is estimated that close to 800 million people living in endemic areas are at risk of getting the infection.3 According to van der Werf and others,4 close to 280,000 people worldwide die of schistosomiasis-related complications every year. The disease largely affects poor rural communities with limited access to basic sanitation and clean water.5 Although schistosomiasis-related mortality is low compared with mortality caused by human immunodeficiency virus (HIV) or malaria, morbidity is high and often underreported.6
Infections with schistosomes result in two main forms of the disease, namely urinary schistosomiasis caused by Schistosoma haematobium and intestinal schistosomiasis caused by either S. mansoni or S. japonicum. S. mansoni is responsible for bloody diarrhea and hepatosplenomegaly in 4.4 and 8.5 million people, respectively.4
Chronic S. mansoni infections are associated with anemia, growth retardation, impaired cognitive development, and reduction in productivity.4,7 In endemic areas, infection is normally acquired early in life, and children bear the highest burden of the infection, whereas complications are more commonly observed in adults.8 Complications of untreated chronic S. mansoni infection (also known as hepatosplenic disease) include thickening of the portal vein and surrounding branches, hepatosplenomegaly, portal hypertension, ascites, and formation of esophageal varices that cause life-threatening bleeding.8,9
According to a 200910 Zambia Bilharzia Control Program (ZBCP) report, approximately 15.4% (2 million) of people in Zambia have schistosomiasis caused by either S. haematobium or S. mansoni. The disease is endemic in most parts of the country, affecting people mainly in rural communities. In these areas, S. mansoni-related complications, such as hepatosplenomegaly, portal hypertension, esophageal varices, and hematemesis, are common.11 Kaoma District in the western part of Zambia is one of the areas long known for S. mansoni endemicity. Although most patients with esophageal varices undergoing endoscopy at the University Teaching Hospital in Lusaka, Zambia come from this particular area,11 the actual prevalence of the disease in the area remains unknown. Information on the distribution of the disease is obtained mainly from clinical records. However, they do not provide accurate information on the extent of the problem, because most individuals seeking medical attention in clinics are already in advanced stages of the disease. Thus, infected individuals who are asymptomatic remain undocumented.
The aim of this study was to determine the prevalence of S. mansoni infection and associated morbidity in four rural communities of Kaoma District in western Zambia. The study findings provide baseline information on which appropriate disease control interventions can be designed.
Materials and Methods
Study area and population.
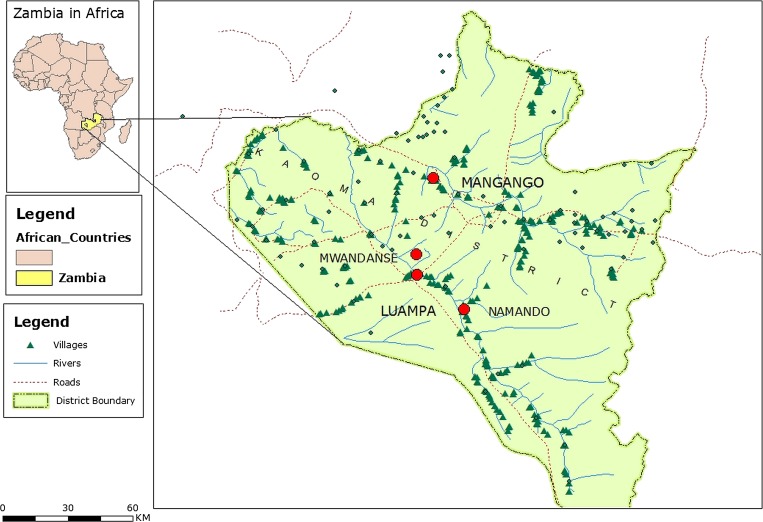
A cross-sectional survey was conducted in four selected areas, namely Luampa, Mwandansengo, Mangango, and Namando in Kaoma District, which is situated in the western part of Zambia (Figure 1). Kaoma District is approximately 550 km from Lusaka, the capital city of Zambia. Two main rivers are found in the district: the Luampa and Luena Rivers. The rivers provide a suitable environment of slow-moving waters and vegetation for the propagation of Biomphalaria snails, the intermediate hosts for S. mansoni parasites. People in these areas live along the rivers and are mostly subsistence farmers who cultivate maize and cassava for food. Contact with Schistosoma-infested water occurs when performing domestic chores, such as washing clothes, bathing, and drawing water for home use. Children get exposed during recreation activities, such as swimming. Exposure also occurs through the processing of cassava, which is the staple food, because long hours are spent soaking the cassava tubers in water along the river banks. Although these communities are well-known to be endemic for S. mansoni, there were no ongoing interventions at the time that this study was being conducted. However, there is a routine deworming program for under 5-years-old children and pregnant women attending maternal and child health clinics (MCHs) targeting soil-transmitted helminths (STH). Passive treatment of people who are diagnosed with schistosomiasis is provided at nearby hospitals.
Figure 1.
Map showing the four study areas in Kaoma District of western Zambia. The big red dots denote the areas where the study was conducted.
Study design.
The study was aimed at determining the prevalence of S. mansoni infection and associated morbidity in selected areas of Kaoma District. The study areas were selected based on their proximity to the rivers (Figure 1) and previous reports of high disease burden. Three months before the survey, community sensitizations were conducted with the help of community health workers and environmental health technicians. Sensitizations were also conducted 1 week before the survey. A systematic random sampling method was used to select the sample for this study. Briefly, participants were lined up, and the first participant was picked at random as the starting point for selecting other participants. Thereafter, every participant with an odd number was included into the study. For logistical reasons, schools in the selected communities served as survey points. School-aged children and adults residing in the selected areas for more than 7 years or since birth were eligible for recruitment. Participants in this survey were assessed using parasitological methods and ultrasonography as described below.
Parasitological examinations.
Recruited participants were screened for the presence or absence of S. mansoni infections and other soil-transmitted helminths using the Kato–Katz method.12 In this method, two smears were prepared using a 41.7-mg Kato template from a single stool sample and left to settle for 30–60 minutes before being examined under a light microscope. Microscopy readings were conducted by two experienced technicians to enhance the validity of the readings. In addition to reading the slides for qualitative diagnosis, the intensity of infection was estimated from the average egg counts of the two examined slides. The intensity of infection for S. mansoni was classified by eggs per gram (epg) as light (1–99 epg), moderate (100–399 epg), and heavy (≥ 400 epg) based on the World Health Organization (WHO) classification guidelines.13 In addition, urine samples from each participant were screened for S. haematobium ova using the urine filtration technique according to a previously described method.14 Briefly, 10 mL urine was filtered through a nucleopore filter membrane that was then examined under a light microscope for presence of S. haematobium ova. Urine samples were collected between 10 AM and 2 PM and processed immediately after collection.
Because the study area is endemic for malaria, participants were also screened for malaria infection with the SD BIOLINE malaria antigen rapid diagnostic test (Standard diagnostics, Inc., Yongin si, Kyonggi, Korea) for detecting Plasmodium falciparum histidine-rich protein 2 (HRP2). The test was performed according to the manufacturers' recommendations, and results were interpreted as positive if both the control and the test line appeared red/pink and negative if only the control line appeared red/pink. Indeterminate results were repeated.
Ultrasonography examinations.
S. mansoni-related morbidity was assessed with a portable ultrasound machine (Mindray DP-1100 Plus Electronic Convex Transducer; 35C50EB; 2.5/3.5/5.0 MHz). Assessment was performed by a trained ultrasonographer with considerable experience in the diagnosis of schistosomiasis-related morbidity under field conditions. Presence of portal fibrosis was assessed using liver image pattern (LIP) scores according to WHO guidelines.15 Based on the degree of fibrosis, LIPs were recorded as C, D, E, and F.16 LIPs A and B were considered normal,17 whereas LIPs unrelated to S. mansoni were recorded as X, Y, or Z.
Statistical analysis.
Statistical analysis was performed using STATA software, version 11 (Stata Corp., College Station, TX), and P values < 0.05 were considered significant. We used the χ2 test to test for differences in infection prevalence and portal fibrosis by gender, age group, and study area. To account for clustering of dependent variables in the study areas, a multivariate negative binomial regression model was used with robust SEs to obtain estimates of the prevalence ratio. Age, gender, and area of residence were included in the model for S. mansoni infection and portal fibrosis.
Ethical consideration.
This study was reviewed and approved by the University of Zambia Biomedical Research and Ethics Committee. Informed written consent and assent were obtained from the participants before participation in the study. Before any procedures were conducted on child participants, the necessary consent from the parents or guardians was also obtained. Participants infected with either S. mansoni or soil-transmitted helminths were given praziquantel at a single dose of 40 mg/kg body weight or 500 mg mebendazole, respectively. Participants infected with malaria were treated according to the Zambia national guidelines for the treatment of malaria.
Results
Characteristics of the study participants.
In total, 754 participants comprising 469 (62.4%) females and 285 (37.6%) males from four study communities of Kaoma District (Luampa, Mangango, Mwandasengo, and Namando) were recruited into the study as shown in Table 1. The study population comprised 159 (21%) children (7–14 years old) and 595 (79%) adults (15–50 years old). The median age was 28 years old (interquartile range [IQR] = 16–40).
Table 1.
Characteristics of 754 study participants recruited from four study areas
| Study area | P value | |||||
|---|---|---|---|---|---|---|
| Overall | Luampa* | Mangango† | Namando‡ | Mwandasengo§ | ||
| Age, median (IQR) | 28 (16–40) | 32 (19–43) | 16 (11–19) | 25 (15–29) | 27 (16–39) | 0.0001¶ |
| Gender, n (%) | ||||||
| Male | 285 (37.8) | 111 (28.8) | 47 (56.0) | 72 (43.6) | 55 (45.8) | < 0.0001∥ |
| Female | 469 (62.2) | 274 (71.2) | 37 (44.1) | 93 (56.4) | 65 (54.2) | |
| Age category, n (%) | ||||||
| Adults | 595 (79.0) | 317 (82.3) | 47 (56.0) | 126 (76.4) | 105 (87.5) | < 0.0001∥ |
| Children | 159 (21.0) | 68 (17.7) | 37 (44.0) | 39 (23.6) | 15 (12.5) | |
| S. mansoni prevalence, n (%)** | ||||||
| Infected | 304 (42.4) | 145 (39.0) | 14 (17.3) | 104 (68.0) | 41 (36.6) | < 0.0001∥ |
| Not infected | 413 (57.6) | 226 (61.0) | 67 (82.7) | 49 (32.0) | 71 (63.4) | |
All comparisons are between characteristics and the study site, excluding the overall column. N = 754.
N = 385 (51%).
N = 165 (22%).
N = 120 (16%).
Kruskall–Wallis test.
χ2 test.
N = 717 (total examined for S. mansoni prevalence).
Among 754 participants recruited, 719 (95%) participants were examined for the presence of S. mansoni infection, of whom 304 (42.4%; 95% confidence interval [95% CI] = 38.7–46.0) tested positive by the Kato–Katz method. Thirty-five of the recruited participants did not provide stool samples and were excluded from analysis. The majority (61.2%) of individuals infected with S. mansoni had light infections, whereas moderate and heavy infections were recorded in 26.0% and 12.8% of the population, respectively.
Prevalence of S. mansoni infections by gender and age.
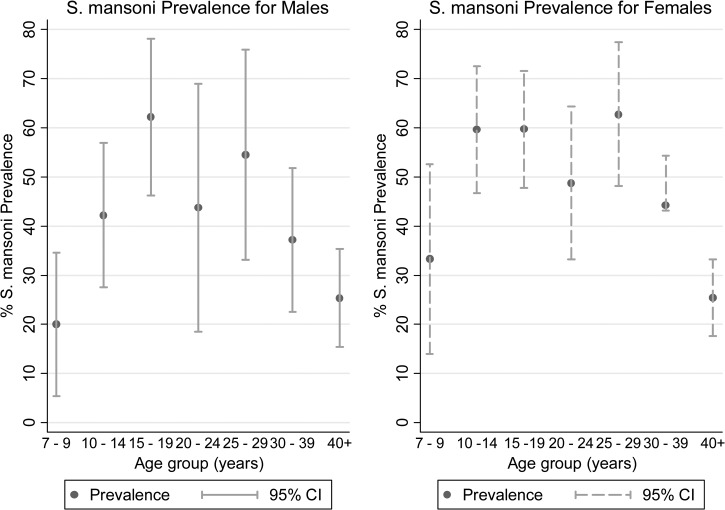
S. mansoni infections were detected in 45% (202) and 38% (102) of the female and male participants, respectively (χ2 = 3.29; P = 0.069). When stratified by age, the highest prevalence of infection was observed in the age group of 15–19 years (60.6%; 95% CI = 51.1–70.0), whereas lower infection prevalence was recorded in participants above the age of 39 years old (25.4%; 95% CI = 19.3–31.5). Additional stratification of the age groups into gender showed the highest prevalence (62.2%; 95% CI = 46.2–78.1) in male participants in the age group 15–19 years, whereas the highest prevalence (62.8%; 95% CI = 48.1–77.4) was observed in the age group 25–29 years in female participants (Figure 2). Female participants in most of the age groups had higher infection prevalence than males, although the difference was not statistically significant, which was shown by the overlapping of 95% CIs (Figure 2). The proportion of individuals infected with S. mansoni was highest in the Namando area (68%; 95% CI = 60.5–75.4), whereas the lowest proportion was recorded in the Mangango area (17.3%; 95% CI = 9.0–25.0). Compared with Luampa, Mwandasengo, and Mangango, Namando recorded higher S. mansoni infection prevalence across all age groups.
Figure 2.
Prevalence of S. mansoni infection in female and male participants by age group with 95% CIs. The middle dots represent the observed prevalence, whereas the upper and lower CIs are represented by vertical lines.
S. mansoni intensity of infection.
The intensity of S. mansoni infection recorded as geometric mean egg count (GMEC) is shown in Table 2.The overall GMEC was 86.8 epg (95% CI = 75.6–99.6), with no significant differences observed between male and female participants. Although there was an association between S. mansoni and age group (P = 0.008), differences among some groups were not statistically significant, except for the 15–19 years and 40+ years age groups (110.9 epg; 95% CI = 79.6–154.6; 51.9 epg; 95% CI = 38.2–70.5). In females, the highest GMEC was recorded in the age group 10–14 years (123.77; 95% CI = 75.08–204.03) followed by the age group 15–19 years (102 epg; 95% CI = 66.89–155.62). Males had the highest GMEC in the age group 25–29 years (168.27 epg; 95% CI = 73.22–386.69) followed by the 15–19 years age group (128.47; CI = 72.32–228.23). The differences observed in these groups were not statistically significant when stratified by gender. Intensity of infection across four study areas varied significantly, with Mwandasengo recording the highest GMEC (χ2 = 15.65, P = 0.001).
Table 2.
S. mansoni GMECs by gender, age group, and study area
| Study variables | GMEC (epg) | 95% CI | P value |
|---|---|---|---|
| Overall | 86.8 | 75.6–99.6 | |
| Gender | |||
| Female | 89.2 | 69.6–114.3 | |
| Male | 85.6 | 72.5–101.1 | 0.915* |
| Age group (years) | |||
| 7–9 | 80.3 | 32.7–196.6 | |
| 10–14 | 120.0 | 81.8–175.94 | |
| 15–19 | 110.9 | 79.6–154.6 | |
| 20–24 | 94.6 | 63.7–140.7 | |
| 25–29 | 101.8 | 69.8–148.8 | |
| 30–39 | 67.7 | 53.1–86.3 | |
| 40+ | 51.9 | 38.2–70.5 | 0.0087† |
| Study area | |||
| Luampa | 68.6 | 56.4–84.6 | |
| Mangango | 65.1 | 29.0–146.0 | |
| Mwandasengo | 141.8 | 96.0–209.7 | |
| Namando | 103.2 | 82.72–128.78 | 0.001† |
Mann–Whitney test.
Kruskall–Wallis test.
Ultrasonography detected S. mansoni-related portal fibrosis.
The overall distribution of portal fibrosis is shown in Table 3. Of the 706 participants who underwent ultrasonography for liver pathology, 181 participants (25.6%; 95% CI = 16.3–22.3) had abnormal LIPs suggestive of S. mansoni-related fibrosis. Four (0.56%) participants had liver disease unrelated to S. mansoni infection and were excluded from additional analysis. The prevalence of fibrosis was 28.0% (95% CI = 23.7–32.1) in female participants and 22.0% (95% CI = 17.0–27.0) in male participants (P = 0.077). Based on image pattern findings, 13.0% and 6.8% of the participants had liver patterns C (peripheral fibrosis) and D (main portal branch fibrosis), respectively. LIPs E and F associated with advanced fibrosis were recorded in 4.7% and 1.3% of the participants, respectively (Table 4).
Table 3.
Prevalence of S. mansoni-related portal fibrosis among 706 recruited participants who underwent abdominal ultrasound examination
| Variables | Total examined | Portal fibrosis (%) | 95% CI | P value |
|---|---|---|---|---|
| Overall | 706 | 25.6 | 22.4–28.8 | |
| Gender | ||||
| Female | 437 | 28.0 | 23.7–32.1 | |
| Male | 269 | 22.0 | 16.9–26.9 | 0.077* |
| Age group (years) | ||||
| 7–9 | 50 | 14.0 | 4.3–23.7 | |
| 10–14 | 96 | 16.7 | 9.1–24.2 | |
| 15–19 | 98 | 18.4 | 10.6–26.0 | |
| 20–24 | 54 | 18.5 | 8.0–29.0 | |
| 25–29 | 67 | 28.3 | 17.4–39.2 | |
| 30–39 | 140 | 31.4 | 23.7–39.1 | |
| 40+ | 201 | 33.3 | 26.8–39.9 | 0.002* |
| Study area | ||||
| Luampa | 362 | 30.0 | 25.3–34.7 | |
| Mangango | 81 | 16.0 | 9.0–23.1 | |
| Mwandasengo | 105 | 21.2 | 12.2–30.3 | |
| Namando | 158 | 27.2 | 20.2–34.2 | 0.017* |
χ2 test.
Table 4.
Distribution of S. mansoni-related LIPs in 706 recruited participants according to gender, age group, and study area
| Variable | Total examined | LIP scores, n (%)* | P value | ||||
|---|---|---|---|---|---|---|---|
| LIPs A and B | LIP C | LIP D | LIP E | LIP F | |||
| Overall | 706 | 525 (74.2) | 91 (13.0) | 48 (6.8) | 33 (4.7) | 9 (1.3) | |
| Gender | |||||||
| Female | 437 | 315 (72.1) | 57 (13.0) | 33 (7.5) | 26 (6.0) | 6 (1.4) | |
| Male | 269 | 210 (78.1) | 34 (12.6) | 15 (5.6) | 7 (2.6) | 3 (1.1) | 0.210 |
| Age group (years) | |||||||
| 7–9 | 50 | 43 (86.0) | 7 (14.0) | 0 (0) | 0 (0) | 0 (0) | |
| 10–14 | 96 | 80 (83.4) | 14 (14.6) | 1 (1.0) | 1 (1.0) | 0 (0) | |
| 15–19 | 98 | 80 (81.6) | 16 (16.3) | 0 (0) | 2 (2.1) | 0 (0) | |
| 20–24 | 54 | 44 (81.6) | 4 (7.4) | 3 (5.5) | 3 (5.5) | 0 (0) | |
| 25–29 | 67 | 48 (71.6) | 8 (11.9) | 4 (6.0) | 6 (9.0) | 1 (1.5) | |
| 30–39 | 140 | 96 (68.6) | 17 (12.1) | 13 (9.3) | 11 (7.9) | 3 (2.1) | |
| 40+ | 201 | 134 (67.7) | 25 (12.4) | 27 (13.4) | 10 (5.0) | 5 (2.5) | < 0.001 |
| Study area | |||||||
| Luampa | 362 | 256 (70.7) | 50 (13.8) | 28 (7.7) | 22 (6.1) | 6 (1.7) | |
| Mangango | 81 | 65 (80.2) | 16 (19.8) | 0 (0) | 0 (0) | 0 (0) | |
| Mwandasengo | 105 | 89 (84.7) | 7 (6.7) | 7 (6.7) | 2 (1.9) | 0 (0) | |
| Namando | 158 | 115 (72.7) | 18 (11.4) | 13 (8.2) | 9 (5.7) | 3 (2) | 0.010 |
LIP scores denote the degree of fibrosis and are based on the Niamey image pattern scoring.15
A and B = normal liver texture; C–F = abnormal liver texture; E and F = advanced forms of fibrosis.
Multivariate analysis for predictors of S. mansoni infection and portal fibrosis.
Multivariate binomial regression to estimate prevalence ratios (PRs) of S. mansoni infection for risk factors showed that age and area of residence were strongly associated with increased S. mansoni infections (Table 5). After controlling for age and gender, participants in Namando were 1.50 times (95% CI = 1.26–1.74; P < 0.001) more likely to be infected than those in Luampa, whereas age groups 15–19 and 25–29 years were significantly associated with S. mansoni infection (adjusted PR = 1.70; P = 0.017 and adjusted PR = 1.62; P = 0.033, respectively).
Table 5.
Logistic regression models for S. mansoni infection and periportal fibrosis controlling for age and gender
| Variable | Crude PR | Adjusted PR | ||
|---|---|---|---|---|
| PR (95% CI) | P value | PR (95% CI) | P value | |
| S. mansoni infection | ||||
| Gender | ||||
| Male | 1.00 | 1.00 | ||
| Female | 1.18 (0.98–1.42) | 0.075 | 1.28 (0.95–1.29) | 0.201 |
| Age group (years) | ||||
| 7–9 | 1.00 | 1.00 | ||
| 10–14 | 2.00 (1.23–3.26) | 0.005 | 1.56 (1.00–2.41) | 0.047 |
| 15–19 | 2.34 (1.45–3.76) | < 0.001 | 1.70 (1.10–2.62) | 0.017 |
| 20–24 | 1.82 (1.08–3.10) | 0.025 | 1.35 (0.84–2.18) | 0.219 |
| 25–29 | 2.31 (1.41–3.78) | 0.001 | 1.62 (1.04–2.52) | 0.033 |
| 30–39 | 1.62 (0.99–2.65) | 0.121 | 1.23 (0.79–1.94) | 0.356 |
| 40+ | 0.98 (0.58–1.63) | 0.935 | 0.73 (0.45–1.61) | 0.181 |
| Study area | ||||
| Luampa | 1.00 | 1.00 | ||
| Mwandasengo | 0.94 (0.71–1.23) | 0.641 | 0.84 (0.65–1.10) | 0.206 |
| Mangango | 0.44 (0.27–0.72) | 0.001 | 0.39 (0.24–0.64) | < 0.001 |
| Namando | 1.74 (1.47–2.06) | < 0.001 | 1.50 (1.26–1.74) | < 0.001 |
| Periportal fibrosis infection | ||||
| Gender | ||||
| Male | 1.00 | 1.00 | ||
| Female | 1.25 (0.97–1.62) | 0.086 | 1.26 (0.97–1.64) | 0.088 |
| Age group (years) | ||||
| 7–9 | 1.00 | 1.00 | ||
| 10–14 | 1.39 (0.62–3.11) | 0.415 | 1.44 (0.65–3.23) | 0.369 |
| 15–19 | 1.64 (0.75–3.58) | 0.212 | 1.85 (0.84–4.05) | 0.125 |
| 20–24 | 1.41 (0.59–3.38) | 0.437 | 1.34 (0.54–3.31) | 0.520 |
| 25–29 | 2.14 (0.98–4.70) | 0.057 | 2.10 (0.93–4.72) | 0.073 |
| 30–39 | 2.34 (1.13–4.89) | 0.023 | 2.48 (1.20–5.23) | 0.017 |
| 40+ | 2.76 (1.35–5.64) | 0.005 | 2.93 (1.42–6.07) | 0.004 |
| Study area | ||||
| Luampa | 1.00 | 1.00 | ||
| Mwandasengo | 0.53 (0.34–0.82) | 0.005 | 0.49 (0.30–0.78) | 0.003 |
| Mangango | 0.76 (0.49–1.16) | 0.199 | 0.91 (0.58–1.44) | 0.699 |
| Namando | 0.93 (0.70–1.25) | 0.640 | 0.91 (0.67–1.24) | 0.555 |
| Other infections | ||||
| Malaria | 1.12 (0.71–1.78) | 0.613 | 1.50 (0.90–2.48) | 0.114 |
In this study population, individuals above the age category of 15 years were 1.76 times more likely to have portal fibrosis than those below the age of 15 years (95% CI = 1.17–2.62, P = 0.006). When age was further stratified into groups, age groups 35–39 and 40+ years were strong predictors of fibrosis (adjusted PR = 2.48; P = 0.017 and adjusted PR = 2.93; P = 0.004, respectively) (Table 5). Of note was the lack of association in this study between increased egg count and fibrosis (odds ratio = 0.99; P = 0.273). In this study, infection with malaria was not associated with fibrosis (PR = 1.52; P = 0.114).
Other parasitic infections detected.
Apart from S. mansoni infections, hookworm and malaria were also detected. Hookworm was detected in 26.9% (95% CI = 23.6–30.2) of 717 participants screened, with higher prevalence observed in males than in females (31.3% versus 24.3%; P = 0.039). The prevalence was also significantly higher in children than in adults (44.8%; 95% CI = 37.0–52.7 versus 22.0%; 95% CI = 18.5–25.4; P < 0.001). Malaria was detected in 6.5% (48) of the participants screened, with significantly higher prevalence observed in children than in adults (13.4% versus 4.8%; P < 0.001). S. mansoni malaria coinfections were detected in 5.2% of the population, whereas S. mansoni and hookworm coinfections were detected in 12.3% of the population. Triple infections (S. mansoni, hookworm, and malaria combined) were detected in 1.9% of the population screened. Other helminths detected were Taenia (0.56%), Hymenolpsis nana (0.14%), Ascaris lumbricoides (0.14%), and Trichuris trichiura (0.14%). Of interest was the absence of S. haematobium in this population. (Additional detailed results of the coinfections part of the study with respect to health status of coinfected school-aged children are being reported elsewhere; unpublished data).
Discussion
In this study, almost one-half of the studied population in the respective communities had S. mansoni infection, and children were shown to harbor most of the infections. The observed prevalence of 42% could be an underestimation of the actual prevalence of the infection in this area, because we used the Kato–Katz method, which has shown low sensitivity when a single stool sample is obtained.18,19 This study also showed that S. mansoni-related liver pathology was relatively high in this population compared with that observed elsewhere.20,21
The prevalence of infection in our study population followed a convex distribution: peaking at ages 15–18 years and declining thereafter. However, the highest intensity of infection was observed at a much younger age group (11–14 years). Similar trends in the intensity of infection have been documented in other S. mansoni-endemic areas.22,23 Differences in parasite distribution among the different age groups have been attributed to behavioral changes and acquisition of immunity to infection in the older age groups.24,25 Although it is true that immunity to Schistosoma infection develops over time and in line with increasing age, the trend may not be so for behavioral change as a factor for infection reduction among adults living in S. mansoni-endemic areas. For instance, in most households in our study area, piped water is not available, with the only source of water being the nearby Schistosoma-infested rivers or streams. In such instances, adults are equally more likely to be exposed to acquiring the infection as they carry out activities, such as washing, bathing, and gardening. Other studies, however, have shown reduction in water contact activities as children get older.26 Thus, water contact is more of a social and traditional issue, where roles change as one attains adulthood.
In this study, although not statistically significant, the prevalence of S. mansoni infection was relatively higher in female participants than in male participants. Variations in infection prevalence in male and female participants are mostly attributed to differences in exposure habits, which are usually occupation-based.22 For instance, in our study communities, women have more contact hours with these Schistosoma-infested water bodies carrying out domestic chores, such as washing, than men, because access to a clean water supply and good sanitation is limited in most households. However, findings from a recent study in Uganda23 showed that men were more likely to be infected with S. mansoni than their female counterparts, because they have more water contact hours with infested water during their fishing activities.
Furthermore, we observed variability in the distribution of S. mansoni infection among the four communities that we studied, although epidemiological patterns, such as social and environmental characteristics, were similar. Microgeographical variations in schistosomiasis-endemic areas have been documented 27–29 and are probably caused by factors, such as differences in transmission dynamics involving both the intermediate snail host and the human host.30,31 The variations in infection distributions in different communities have implications for control activities, because affected areas may require targeted interventions as opposed to mass interventions.
In chronic untreated S. mansoni infections, portal fibrosis is a common finding in endemic areas.32 As has been observed in other S. mansoni-endemic countries, the prevalence of fibrosis was shown to increase with increasing age.20,32–34 We also observed in our study population that adults were more likely to present with portal fibrosis on ultrasound than children. Although this is sometimes reported in children, severe forms of the disease are rarely observed in younger populations. The milder form (LIP C) of portal fibrosis is normally seen in younger age groups.6,35 In endemic areas, most people infected with S. mansoni present with LIP C and D forms of fibrosis,36 whereas severe disease characterized with advanced fibrosis (LIPs E and F) is only observed in 5–10% of the people.37 In our study population, advanced fibrosis characterized with LIPs E and F was recorded in 4.8% and 1.2% of the participants, respectively. The observed prevalence of advanced portal fibrosis cases in this study correlates with the findings from other studies.20 Factors associated with increased risk of severe fibrosis have been documented, and they include age, duration of residency in an S. mansoni-endemic region, intensity of infection, and presence of other infections, like hepatitis B.20,23 In our study, however, no association between intensity of S. mansoni infection and disease severity was observed. This finding contrasts with some studies that have that the intensity of infection correlates with disease severity.20,23,32–34 The lack of association observed in our study could be explained by other possible factors, including the observed high prevalence of S. mansoni infection in this study population, suggesting that the studied participants have repeated exposure.
As has been reported elsewhere,11 disease-associated complications, such as portal fibrosis, hepatosplenomegaly, portal hypertension, ascites, and hematemesis, are common in areas of high S. mansoni endemicity. It is of concern, however, that children in our population had high prevalence of infection and intensity. Because complications are consequences of untreated chronic infections, some of these children are likely to end up with complications later in their adult life if they are not treated. Chronic infections in children are associated with anemia, stunted growth, and impaired cognitive development.7 It has also been shown that neglected tropical diseases (NTDs), such as schistosomiasis, are predictors of poverty, because they have a negative effect on productivity and economic growth.38 Although most countries have adopted the WHO model of reducing infection and morbidity, which is based on the set thresholds, reinfections are common in endemic areas, because not all individuals are treated. The untreated population becomes a reservoir of infection, contributing significantly to transmission.
The overall S. mansoni prevalence rate of 44% in this study is likely to be an underestimation of the burden of S. mansoni in this area. We used the Kato–Katz method, which has been shown to have low sensitivity.18,39 Studies have shown that this method is less sensitive and less accurate when one stool sample is used, resulting in an underestimation of the prevalence.18 The low sensitivity using the Kato–Katz method is attributed to a number of reasons, such as daily variation in egg output and inability to detect light infections.19,40 Sensitivity can be enhanced by examining multiple stool samples and smears.40–44 In a study by Enk and others,40 S. mansoni prevalence increased from 13.8% with 1 smear to 27.2% with 10 smears. Additional increase was observed when three samples were examined. In our study, only one sample was examined because of financial constraints. To increase the rate of parasite detection, duplicate smears were prepared from each stool sample collected.
Accurate diagnosis of S. mansoni is important for not only control of morbidity at an individual level but more so, control efforts directed at the communities. The WHO guideline on treatment is based on set thresholds that determine when to intervene using mass treatment or otherwise.45 With the low sensitivity of the Kato–Katz technique, many affected communities may not be eligible for mass treatment.
These findings of high S. mansoni disease burden that we report here highlight the urgent need for carrying out preventive chemotherapy in this area. Other interventions, such as provision of safe water points and good sanitation, health education, and targeted mollusciding, should also be considered. Furthermore, it is also of utmost importance that an effective monitoring and evaluation system is put in place to monitor the effectiveness of the interventions on morbidity.
ACKNOWLEDGMENTS
The authors thank all participants from the four study communities for taking part in this study. We also extend our gratitude to the provincial and district health office for their support. Support from the Ministry of Health (Public Health Directorate, Department of Pathology and Microbiology, Diagnostic and Laboratory Services) and the Southern African Consortium for Research Excellence (SACORE) country team is also acknowledged. We sincerely thank all study team members (laboratory and ultrasound technicians, clinical officers, and community health workers) for their dedication to this work. The authors also acknowledge the exceptional inputs of Dr. Patrick Musonda, a biostatician, who helped with the in-depth data analysis. We also acknowledge Mr. Gabriel Mushinge who assisted with the GPS mapping of the study area. The American Society of Tropical Medicine and Hygiene (ASTMH) assisted with publication expenses.
Footnotes
Financial support: This study was financed by the Southern African Consortium of Research Excellence (SACORE) Wellcome Trust-supported project. The study is part of the PhD work on immunogenetics of S. mansoni disease by the principal investigator (M.M.M.).
Authors' addresses: Mable M. Mutengo, James Mwansa, and Sandie Sianongo, Department of Pathology and Microbiology, University of Zambia School of Medicine, Lusaka, Zambia, and Department of Pathology and Microbiology, University Teaching Hospital, Lusaka, Zambia, E-mails: mmutengo@yahoo.com, mwansaj@gmail.com, and ssianongo@yahoo.com. Takafira Mduluza, Department of Biochemistry, University of Zimbabwe, Harare, Zimbabwe, E-mail: tmduluza@yahoo.com. James Chipeta, Department of Pediatrics and Child Health, University of Zambia School of Medicine, Lusaka, Zambia, E-mail: Jameschipeta@smuth-mru.org.zm.
References
- 1.Handzel T, Karanja DM, Addiss DG, Hightower AW, Rosen DH, Colley DG, Andove J, Slutsker L, Secor WE. Geographic distribution of schistosomiasis and soil-transmitted helminths in western Kenya: implications for anthelminthic mass treatment. Am J Trop Med Hyg. 2003;69:318–323. [PubMed] [Google Scholar]
- 2.Mazigo HD, Nuwaha F, Kinung'hi SM, Morona D, Pinot de Moira A, Wilson S, Heukelbach J, Dunne DW. Epidemiology and control of human schistosomiasis in Tanzania. Parasit Vectors. 2012;5:274. doi: 10.1186/1756-3305-5-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steinmann P, Keiser J, Bos R, Tanner M, Utzinger J. Schistosomiasis and water resources development: systematic review, meta-analysis, and estimates of people at risk. Lancet Infect Dis. 2006;6:411–425. doi: 10.1016/S1473-3099(06)70521-7. [DOI] [PubMed] [Google Scholar]
- 4.van der Werf MJ, de Vlas SJ, Brooker S, Looman CW, Nagelkerke NJ, Habbema JD, Engels D. Quantification of clinical morbidity associated with schistosome infection in sub-Saharan Africa. Acta Trop. 2003;86:125–139. doi: 10.1016/s0001-706x(03)00029-9. [DOI] [PubMed] [Google Scholar]
- 5.Gazzinelli A, Correa-Oliveira R, Yang GJ, Boatin BA, Kloos H. A research agenda for helminth diseases of humans: social ecology, environmental determinants, and health systems. PLoS Negl Trop Dis. 2012;6:e1603. doi: 10.1371/journal.pntd.0001603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Samuels AM, Matey E, Mwinzi PN, Wiegand RE, Muchiri G, Ireri E, Hyde M, Montgomery SP, Karanja DM, Secor WE. Schistosoma mansoni morbidity among school-aged children: a SCORE project in Kenya. Am J Trop Med Hyg. 2012;87:874–882. doi: 10.4269/ajtmh.2012.12-0397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.King CH, Dangerfield-Cha M. The unacknowledged impact of chronic schistosomiasis. Chronic Illn. 2008;4:65–79. doi: 10.1177/1742395307084407. [DOI] [PubMed] [Google Scholar]
- 8.Vennervald BJ, Dunne DW. Morbidity in schistosomiasis: an update. Curr Opin Infect Dis. 2004;17:439–447. doi: 10.1097/00001432-200410000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Wilson S, Vennervald BJ, Dunne DW. Chronic hepatosplenomegaly in African school children: a common but neglected morbidity associated with schistosomiasis and malaria. PLoS Negl Trop Dis. 2011;5:e1149. doi: 10.1371/journal.pntd.0001149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.ZBCP . Baseline Survey for Schistosomiasis and Soil-Transmitted Helmithiasis. Lusaka, Zambia: Ministry of Health; 2009. [Google Scholar]
- 11.Lubeya M, Muloshi C, Baboo KS, Sianongo S, Kelly P. Hepatosplenic schistosomiasis. Lancet. 2010;376:1645. doi: 10.1016/S0140-6736(10)62095-8. [DOI] [PubMed] [Google Scholar]
- 12.Katz N, Chaves A, Pellegrino J. A simple device for quantitative stool thick smear technique in Schistosoma mansoni. Rev Inst Med Trop Sao Paulo. 1972;14:397–400. [PubMed] [Google Scholar]
- 13.WHO . Prevention and Control of Schistosomiasis and Soil-Transmitted Helminthiasis. Geneva: World Health Organization; 2002. [PubMed] [Google Scholar]
- 14.Peters PA, Mahmoud AA, Warren KS, Ouma JH, Siongok TK. Field studies of a rapid, accurate means of quantifying Schistosoma haematobium eggs in urine samples. Bull World Health Organ. 1976;54:159–162. [PMC free article] [PubMed] [Google Scholar]
- 15.Richter J, Hatz C, Campagne G, Bergquist NR, Jenkins JM. Ultrasound in Schistosomiasis. A Practical Guide to the Standardized Use of Ultrasonography for the Assessment of Schistosomiasis Related Morbidity. Geneva: World Health Organization; 2000. [Google Scholar]
- 16.Berhe N, Geitung JT, Medhin G, Gundersen SG. Large scale evaluation of WHO's ultrasonographic staging system of schistosomal periportal fibrosis in Ethiopia. Trop Med Int Health. 2006;11:1286–1294. doi: 10.1111/j.1365-3156.2006.01665.x. [DOI] [PubMed] [Google Scholar]
- 17.Vennervald BJ, Kenty L, Butterworth AE, Kariuki CH, Kadzo H, Ireri E, Amaganga C, Kimani G, Mwatha J, Otedo A, Booth M, Ouma JH, Dunne DW. Detailed clinical and ultrasound examination of children and adolescents in a Schistosoma mansoni endemic area in Kenya: hepatosplenic disease in the absence of portal fibrosis. Trop Med Int Health. 2004;9:461–470. doi: 10.1111/j.1365-3156.2004.01215.x. [DOI] [PubMed] [Google Scholar]
- 18.de Vlas SJ, Gryseels B. Underestimation of Schistosoma mansoni prevalences. Parasitol Today. 1992;8:274–277. doi: 10.1016/0169-4758(92)90144-q. [DOI] [PubMed] [Google Scholar]
- 19.Engels D, Sinzinkayo E, Gryseels B. Day-to-day egg count fluctuation in Schistosoma mansoni infection and its operational implications. Am J Trop Med Hyg. 1996;54:319–324. doi: 10.4269/ajtmh.1996.54.319. [DOI] [PubMed] [Google Scholar]
- 20.Berhe N, Myrvang B, Gundersen SG. Intensity of Schistosoma mansoni, hepatitis B, age, and sex predict levels of hepatic periportal thickening/fibrosis (PPT/F): a large-scale community-based study in Ethiopia. Am J Trop Med Hyg. 2007;77:1079–1086. [PubMed] [Google Scholar]
- 21.Kariuki HC, Mbugua G, Magak P, Bailey JA, Muchiri EM, Thiongo FW, King CH, Butterworth AE, Ouma JH, Blanton RE. Prevalence and familial aggregation of schistosomal liver morbidity in Kenya: evaluation by new ultrasound criteria. J Infect Dis. 2001;183:960–966. doi: 10.1086/319247. [DOI] [PubMed] [Google Scholar]
- 22.Kabatereine NB, Kemijumbi J, Ouma JH, Kariuki HC, Richter J, Kadzo H, Madsen H, Butterworth AE, Ornbjerg N, Vennervald BJ. Epidemiology and morbidity of Schistosoma mansoni infection in a fishing community along Lake Albert in Uganda. Trans R Soc Trop Med Hyg. 2004;98:711–718. doi: 10.1016/j.trstmh.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 23.Tukahebwa EM, Magnussen P, Madsen H, Kabatereine NB, Nuwaha F, Wilson S, Vennervald BJ. A very high infection intensity of Schistosoma mansoni in a Ugandan Lake Victoria fishing community is required for association with highly prevalent organ related morbidity. PLoS Negl Trop Dis. 2013;7:e2268. doi: 10.1371/journal.pntd.0002268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Black CL, Mwinzi PN, Muok EM, Abudho B, Fitzsimmons CM, Dunne DW, Karanja DM, Secor WE, Colley DG. Influence of exposure history on the immunology and development of resistance to human Schistosomiasis mansoni. PLoS Negl Trop Dis. 2010;4:e637. doi: 10.1371/journal.pntd.0000637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pinot de Moira A, Fulford AJ, Kabatereine NB, Ouma JH, Booth M, Dunne DW. Analysis of complex patterns of human exposure and immunity to schistosomiasis mansoni: the influence of age, sex, ethnicity and IgE. PLoS Negl Trop Dis. 2010;4:e820. doi: 10.1371/journal.pntd.0000820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seto EY, Sousa-Figueiredo JC, Betson M, Byalero C, Kabatereine NB, Stothard JR. Patterns of intestinal schistosomiasis among mothers and young children from Lake Albert, Uganda: water contact and social networks inferred from wearable global positioning system dataloggers. Geospat Health. 2012;7:1–13. doi: 10.4081/gh.2012.99. [DOI] [PubMed] [Google Scholar]
- 27.Boisier P, Ramarokoto CE, Ravoniarimbinina P, Rabarijaona L, Ravaoalimalala VE. Geographic differences in hepatosplenic complications of schistosomiasis mansoni and explanatory factors of morbidity. Trop Med Int Health. 2001;6:699–706. doi: 10.1046/j.1365-3156.2001.00781.x. [DOI] [PubMed] [Google Scholar]
- 28.Simoonga C, Kazembe LN, Kristensen TK, Olsen A, Appleton CC, Mubita P, Mubila L. The epidemiology and small-scale spatial heterogeneity of urinary schistosomiasis in Lusaka province, Zambia. Geospat Health. 2008;3:57–67. doi: 10.4081/gh.2008.232. [DOI] [PubMed] [Google Scholar]
- 29.Meurs L, Mbow M, Boon N, van den Broeck F, Vereecken K, Dieye TN, Abatih E, Huyse T, Mboup S, Polman K. Micro-geographical heterogeneity in Schistosoma mansoni and S. haematobium infection and morbidity in a co-endemic community in northern Senegal. PLoS Negl Trop Dis. 2013;7:e2608. doi: 10.1371/journal.pntd.0002608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kariuki HC, Clennon JA, Brady MS, Kitron U, Sturrock RF, Ouma JH, Ndzovu ST, Mungai P, Hoffman O, Hamburger J, Pellegrini C, Muchiri EM, King CH. Distribution patterns and cercarial shedding of Bulinus nasutus and other snails in the Msambweni area, Coast Province, Kenya. Am J Trop Med Hyg. 2004;70:449–456. [PubMed] [Google Scholar]
- 31.Clennon JA, King CH, Muchiri EM, Kariuki HC, Ouma JH, Mungai P, Kitron U. Spatial patterns of urinary schistosomiasis infection in a highly endemic area of coastal Kenya. Am J Trop Med Hyg. 2004;70:443–448. [PubMed] [Google Scholar]
- 32.Malenganisho WL, Magnussen P, Friis H, Siza J, Kaatano G, Temu M, Vennervald BJ. Schistosoma mansoni morbidity among adults in two villages along Lake Victoria shores in Mwanza District, Tanzania. Trans R Soc Trop Med Hyg. 2008;102:532–541. doi: 10.1016/j.trstmh.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 33.King CH, Magak P, Salam EA, Ouma JH, Kariuki HC, Blanton RE. World Health O Measuring morbidity in schistosomiasis mansoni: relationship between image pattern, portal vein diameter and portal branch thickness in large-scale surveys using new WHO coding guidelines for ultrasound in schistosomiasis. Trop Med Int Health. 2003;8:109–117. doi: 10.1046/j.1365-3156.2003.00994.x. [DOI] [PubMed] [Google Scholar]
- 34.Mohamed-Ali Q, Elwali NE, Abdelhameed AA, Mergani A, Rahoud S, Elagib KE, Saeed OK, Abel L, Magzoub MM, Dessein AJ. Susceptibility to periportal (Symmers) fibrosis in human Schistosoma mansoni infections: evidence that intensity and duration of infection, gender, and inherited factors are critical in disease progression. J Infect Dis. 1999;180:1298–1306. doi: 10.1086/314999. [DOI] [PubMed] [Google Scholar]
- 35.Strahan R, Chiyesu KO, Schneider-Kolsky ME. Ultrasound study of liver disease caused by Schistosoma mansoni in rural Zambian schoolchildren. J Med Imaging Radiat Oncol. 2012;56:390–397. doi: 10.1111/j.1754-9485.2012.02371.x. [DOI] [PubMed] [Google Scholar]
- 36.Meurs L, Mbow M, Vereecken K, Menten J, Mboup S, Polman K. Bladder morbidity and hepatic fibrosis in mixed Schistosoma haematobium and S. mansoni infections: a population-wide study in northern Senegal. PLoS Negl Trop Dis. 2012;6:e1829. doi: 10.1371/journal.pntd.0001829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith PM, Shainheit MG, Bazzone LE, Rutitzky LI, Poltorak A, Stadecker MJ. Genetic control of severe egg-induced immunopathology and IL-17 production in murine schistosomiasis. J Immunol. 2009;183:3317–3323. doi: 10.4049/jimmunol.0901504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.King CH. Parasites and poverty: the case of schistosomiasis. Acta Trop. 2010;113:95–104. doi: 10.1016/j.actatropica.2009.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lodh N, Mwansa JC, Mutengo MM, Shiff CJ. Diagnosis of Schistosoma mansoni without the stool: comparison of three diagnostic tests to detect Schiostosoma mansoni infection from filtered urine in Zambia. Am J Trop Med Hyg. 2013;89:46–50. doi: 10.4269/ajtmh.13-0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Enk MJ, Lima AC, Drummond SC, Schall VT, Coelho PM. The effect of the number of stool samples on the observed prevalence and the infection intensity with Schistosoma mansoni among a population in an area of low transmission. Acta Trop. 2008;108:222–228. doi: 10.1016/j.actatropica.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 41.Booth M, Vounatsou P, N'Goran EK, Tanner M, Utzinger J. The influence of sampling effort and the performance of the Kato-Katz technique in diagnosing Schistosoma mansoni and hookworm co-infections in rural Cote d'Ivoire. Parasitology. 2003;127:525–531. doi: 10.1017/s0031182003004128. [DOI] [PubMed] [Google Scholar]
- 42.Berhe N, Medhin G, Erko B, Smith T, Gedamu S, Bereded D, Moore R, Habte E, Redda A, Gebre-Michael T, Gundersen SG. Variations in helminth faecal egg counts in Kato-Katz thick smears and their implications in assessing infection status with Schistosoma mansoni. Acta Trop. 2004;92:205–212. doi: 10.1016/j.actatropica.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 43.Carneiro TR, Pinheiro MC, de Oliveira SM, Hanemann AL, Queiroz JA, Bezerra FS. Increased detection of schistosomiasis with Kato-Katz and SWAP-IgG-ELISA in a northeastern Brazil low-intensity transmission area. Rev Soc Bras Med Trop. 2012;45:510–513. doi: 10.1590/s0037-86822012000400019. [DOI] [PubMed] [Google Scholar]
- 44.Knopp S, Mgeni AF, Khamis SI, Steinmann P, Stothard RJ, Rollinson D, Mart H, Utzinger J. Diagnosis of soil-transmitted helminths in the era of preventive chemotherapy: effect of multiple stool sampling and use of different diagnostic techniques. PLoS Negl Trop Dis. 2008;2:e331. doi: 10.1371/journal.pntd.0000331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.WHO . Preventive Chemotherapy in Human Helminthiasis: Coordinated Use of Anthelminthic Drugs in Control Interventions: A Manual for Health Professionals and Programme Managers. Geneva: World Health Organization; 2006. [Google Scholar]