Abstract
There are limited data about the epidemiology of fascioliasis in Cuzco, Peru. We studied children 3–12 years old from six communities in the highlands of Cuzco to evaluate the epidemiology of fascioliasis; 227 children were included, one-half were female, the mean age was 7.5 (±2.6) years, and 46.2±% had one or more parasites, including Fasciola (9.7%), Ascaris (12.8%), Hymenolepis (9.3%), Trichuris (1.3%), hookworm (1.8%), Strongyloides (0.9%), and Giardia (27.8%). Fasciola was associated with the number of siblings in the household, drinking untreated water, and giardiasis. Eosinophilia was encountered in 21% of children and more common in those drinking untreated water at home and those infected with a parasite, but the differences were not significant. Eating water plants was not associated with Fasciola or eosinophilia. Fascioliasis and eosinophilia were common in the highlands of Cuzco. Fascioliasis was associated with socioeconomic factors and drinking water.
Background
Fascioliasis, a neglected food-borne trematode, causes human and livestock infections in most developed and developing countries.1,2 Fascioliasis is particularly common in the highlands of South America, where the prevalence of human infection can reach 70%.3–5 Little is known about the consequences of fascioliasis on health in endemic areas. Overt clinical manifestations of fascioliasis are present in a minority of those infected,6 and it is possible that most children with fascioliasis are never diagnosed, despite the fact that infections may last for years. Previous studies have suggested an association of fascioliasis with anemia and nutritional deficiencies, which could cause irreversible developmental deficits.7–10
Hyperendemic areas (prevalence > 10%) for fascioliasis have been described throughout the Peruvian highlands.11,12 A risk factor for Fasciola transmission recognized in a case-control study in children from the Peruvian Altiplano is the consumption of raw vegetables (alfalfa juice).13 Indirect epidemiological information suggests that transmission of Fasciola may be related to water.14 The objective of this study was to evaluate the epidemiology of Fasciola infection among children in the highlands of Cuzco considering demographic, socioeconomic, and exposure factors as markers of possible transmission routes.
Methods
We performed a cross-sectional study to evaluate the epidemiology of fascioliasis among apparently healthy children 3–12 years old in six communities (Ohuay, Piscohuata, Huayllapata, Queunacancha, Chinchayhuasi, and Huaqaycancha) from the Huancarani district in the Cuzco region of Peru (Figure 1). All of the villages are at altitudes of approximately 3,800 m. Children who assented to participate were enrolled from pre-kinder and primary schools between June and September of 2012. They were already receiving mass chemotherapy with albendazole two times per year provided by a non-profit organization working in the area. Two years before the study, children over 8 years old were screened for fascioliasis, and those found to be infected were treated with triclabendazole; 22 children who were infected with Fasciola 2 years before this study were excluded from the analysis. Parents were interviewed for data on demographics (i.e., sex, age, and family composition), socioeconomic status (parents' educations and livestock ownership), and exposures (i.e., source of drinking water and dietary habits). One blood sample and one or two stool samples were collected from children within 2 weeks of enrollment.
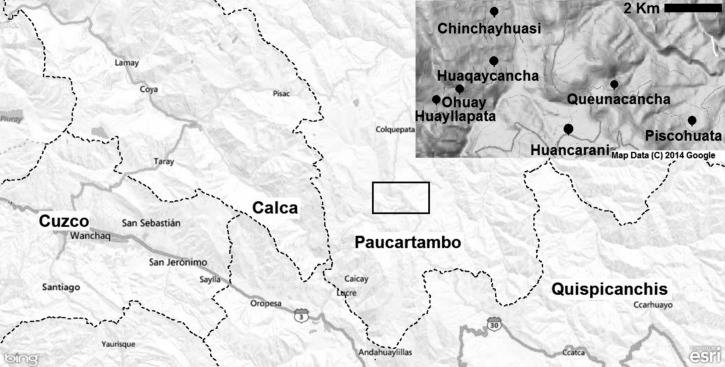
Figure 1.
Map of the provinces of Cuzco showing the location of the six communities studied. Adapted from Google Maps and EpiInfo.
Stool samples were preserved in 10% formalin (Laboratorios Portugal SCRL, Arequipa, Peru). Direct examination and the rapid sedimentation method were used to detect protozoa and helminth ova or larvae.15 The Kato Katz test was performed to quantify worm burden on samples containing Fasciola ova. The aliquot for the Kato Katz test was taken from the central part of the stool specimen that was not dissolved in the formalin. All positive tests were confirmed by a second observer. Blastocystis hominis was not considered a pathogen. The blood specimen was collected to perform a complete blood count, including absolute eosinophil numbers, using an automated analyzer (BC-5300 Auto Hematology Analyzer; MindRay, Shenzhen, China). Eosinophilia was defined as an eosinophil count of ≥ 500 cells/μL.
Data were analyzed using the Statistical Package for the Social Sciences, version 18 (SPSS Inc., Chicago, IL). Frequencies, means (±SDs), and medians with interquartile ranges (IQRs) were used to describe the variables' distribution; t and χ2 tests were used for bivariate analyses of characteristics of children with and without fascioliasis or eosinophilia. Backward logistic regression analysis was used to calculate adjusted odds ratios (ORs) with 95% confidence intervals (95% CIs). Clinical and epidemiological relevant variables and variables with a P ≤ 0.1 in the bivariate analysis were entered in the models. Variables were excluded from the model using the likelihood ratio test. A P < 0.05 was considered statistically significant.
The study protocol was approved by the Institutional Review Board for Human Subjects' Research of the University of Texas Medical Branch. Informed consents and assents were obtained verbally from parents and participants before any study procedure.
Results
Three hundred thirty-four children 3–12 years old were evaluated; however, 107 (32%) children were excluded because of previous diagnosis of fascioliasis, missing stool or blood specimens, or missing information about community of residence, age, or sex. The remaining 227 of 334 (68%) children were included in the analysis. Only 85 of 227 (37.4%) children provided two stool samples for evaluation. The mean age of the participants was 7.5 (±2.6) years, and 53.7% (122 of 227) were male. The median duration of school attendance was 3 years for mothers (IQR = 2–6 years) and 5 years for fathers (IQR = 3–6 years). Most households (99.4%; 172 of 173) owned livestock, including cattle (79.8%; 138 of 173), sheep (83.8%; 145 of 173), horses (62.4%; 108 of 173), pigs (80.4%; 148 of 173), and goats (2.7%; 5 of 173). The demographic characteristics of the participants are shown in Table 1.
Table 1.
Demographic characteristics of the participants
| Characteristic | Percent (n) | Mean (±SD)/ median (IQR) |
|---|---|---|
| Mean age (years) | – | 7.5 (±2.7) |
| Sex | ||
| Male | 53.7 (122) | – |
| Female | 46.3 (105) | – |
| Mean number of people in the household | – | 6.3 (±1.8) |
| Mean number of siblings | – | 4.2 (±1.9) |
| Median years of school attendance | ||
| Mother | – | 3 (2–6) |
| Father | – | 5 (3–6) |
| Community | ||
| Huaqaycancha | 23.3 (53) | – |
| Huayllapata | 19.8 (45) | – |
| Piscohuata | 18.9 (43) | – |
| Ohuay | 16.3 (37) | – |
| Chinchayhuasi | 13.7 (31) | – |
| Queunacancha | 7.9 (18) | – |
| Owns livestock | ||
| Yes | 99.4 (172) | – |
| No | 0.6 (1) | – |
| Source of drinking water at home | ||
| Municipal reservoir | 92.2 (165) | – |
| Well | 4.5 (8) | – |
| Stream | 2.2 (4) | – |
| Irrigation channel | 1.1 (2) | – |
Most children (86.1%; 155 of 180) participated in livestock-raising activities (e.g., grazing cattle). During these field activities, 49 of 154 (31.8%) children drank treated (chlorinated) water, 41 of 154 (26.6%) children drank from streams, 22 of 154 (14.7%) children drank from rivers, 20 of 154 (13%) children drank from wells, 18 of 154 (11.7%) children drank irrigation water, and 4 of 154 (2.6%) children drank from ponds. The main source of drinking water at home was the municipal reservoir (165 of 179; 92.2%), which is piped into homes (Table 1). Lettuce (179 of 184; 97.2%), watercress (99 of 184; 53.8%), spinach (96 of 184; 52.1%), and alfalfa (60 of 184; 32.6%) were common items in the children's diets.
Twenty-two (9.7%) children had F. hepatica eggs in the stool. The geometric mean for the egg count was 39.4 eggs/g stool. The prevalence of Fasciola-positive stools among those who provided two stool samples was not statistically different from the prevalence found in those who provided only one stool sample (9 of 85 versus 13 of 142; P = 0.72). The prevalence of Fasciola-positive stools varied by community, being highest in Huayllapata (9 of 45; 20%) followed by Piscohuata (7 of 43; 16.2%), Huaqaycancha (4 of 53; 7.5%), and Chinchayhuasi (2 of 31; 6.5%; P = 0.01) (Table 2); 0 of 37 children from Ohuay and 18 children in Queunacancha had Fasciola eggs in the stool. Children with Fasciola-positive stool had a lower mean number of siblings at home than uninfected children [3.4 ± 2.1 siblings versus 4.2 ± 1.8 siblings; t (171) = 1.98; P = 0.04]. Those who had an untreated source of drinking water at home had Fasciola eggs in the stool more often than those with treated water (4 of 21 [19%] versus 10 of 158 [6.3%]), but the difference did not reach statistical significance (OR = 3.4 [95% CI = 0.8–14]; P = 0.06). Similarly, those drinking water from a pond in the field were more likely to have Fasciola eggs in the stool than those drinking treated water or water from flowing sources (i.e., rivers or streams; 1of 4 [25%] versus 18 of 151 [12%]), but the difference did not reach statistical significance (OR = 2.4 [95% CI = 0.1–29]; P = 0.4). Fasciola eggs were more commonly found in those with Giardia than among those without it (10 of 63 [15.9%] versus 12 of 164 [7.3%]; P = 0.05). The comparison of characteristic between children with Fasciola eggs in the stool and those without Fasciola eggs in the stools is shown in Table 3. The variables retained as predictors of finding Fasciola eggs in stool in the logistic regression analysis were number of siblings, years of schooling of the father, giardiasis, and not having a treated water source at home (Table 4). There were no associations between finding Fasciola eggs in the stool and dietary items, owning livestock, or participating in raising livestock.
Table 2.
Prevalence of helminths and protozoa-positive stool tests by community
| Huayllapata (n = 45; %) | Piscohuata (n = 43; %) | Huaqaycancha (n = 53; %) | Chinchayhuasi (n = 31; %) | Ohuay (n = 37; %) | Queunacancha (n = 18; %) | P | |
|---|---|---|---|---|---|---|---|
| F. hepatica | 9 (20) | 7 (16.3) | 4 (7.5) | 2 (6.5) | 0 (0) | 0 (0) | 0.01 |
| A. lumbricoides | 7 (15.6) | 0 (0) | 8 (15.1) | 7 (22.6) | 5 (13.5) | 2 (11.1) | 0.08 |
| T. trichiura | 1 (2.2) | 1 (2.3) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 0.86 |
| Hookworm | 3 (6.7) | 0 (0) | 0 (0) | 0 (0) | 1 (2.7) | 0 (0) | 0.1 |
| S. stercoralis | 1 (2.2) | 0 (0) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 0.74 |
| H. nana | 3 (6.7) | 0 (0) | 8 (15.1) | 2 (6.5) | 5 (13.5) | 3 (16.7) | 0.1 |
| G. intestinalis | 18 (40) | 12 (27.9) | 8 (15.1) | 6 (19.4) | 15 (40.5) | 4 (22.2) | 0.03 |
Table 3.
Epidemiologic characteristics of subjects with and without Fasciola eggs in the stool
| Characteristic | Fasciola (+) percent (n) | Fasciola (−) percent (n) | P |
|---|---|---|---|
| Source of water at home | |||
| Municipal reservoir | 81 (17) | 93.7 (148) | 0.06 |
| Untreated water | 19 (4) | 6.3 (10) | |
| Vegetable consumption | |||
| Watercress | 45.4 (10) | 54.9 (89) | 0.4 |
| Lettuce | 100 (22) | 96.9 (157) | 1 |
| Spinach | 59.1 (13) | 51.5 (83) | 0.5 |
| Alfalfa | 27.2 (6) | 33.3 (54) | 0.56 |
| Livestock | |||
| Cattle | 77.2 (17) | 80.1 (121) | 0.7 |
| Sheep | 86.3 (19) | 83.4 (126) | 0.7 |
| Horse | 72.7 (16) | 60.9 (92) | 0.28 |
| Pig | 90.9 (20) | 79.0 (128) | 0.18 |
| Goat | 4.5 (1) | 2.4 (4) | 0.57 |
| Takes cattle grazing | 90.4 (19) | 85.5 (136) | 0.53 |
| Source of water in the field | |||
| Treated | 47.3 (9) | 29.6 (40) | 0.5 |
| Steam | 15.7 (3) | 28.1 (38) | 0.5 |
| River | 10.5 (2) | 14.8 (20) | 0.5 |
| Well | 15.7 (3) | 12.6 (17) | 0.5 |
| Irrigation water | 5.2 (1) | 12.6 (17) | 0.5 |
| Pond | 5.2 (1) | 2.2 (3) | 0.5 |
| Eosinophilia | 22.7 (5) | 21.5 (44) | 0.9 |
Table 4.
Variables associated with F. hepatica infection and eosinophilia among children from Huancarani by logistic regression
| Variable | Fascioliasis adjusted OR (95% CI) | P | Eosinophilia adjusted OR (95% CI) | P |
|---|---|---|---|---|
| Number of siblings at home | 1.33 (1.01–1.75) | 0.03 | NIM | |
| Years of schooling of the father | 1.18 (0.97–1.42) | 0.08 | NIM | – |
| Giardiasis | 3.21 (1.1–9.34) | 0.03 | NIM | – |
| Untreated drinking water source at home | 4.86 (1.18–19.97) | 0.02 | 5.77 (0.7–46.99) | 0.1 |
| Any parasite infection | NIM | – | 1.57 (0.99–2.49) | 0.05 |
Variables entered in the model: community of residence, age, sex, number of siblings at home, years of schooling of the mother, years of schooling of the father, giardiasis (only Fasciola model), any parasite infection (only eosinophilia model), and having an untreated drinking water source at home. Fascioliasis model: Cox and Snell R2 = 0.09, Hosmer–Lemeshow test P = 0.15. Eosinophilia model: Cox and Snell R2 = 0.04, Hosmer–Lemeshow test P = 0.78. NIM = not in the model.
Many of the children had positive stool tests for other intestinal parasites, including Ascaris lumbricoides (29 of 227; 12.8%), Hymenolepis nana (21 of 227; 9.3%), Trichuris trichiura (3 of 227; 1.3%), hookworm (4 of 2,270; 1.8%), Strongyloides stercoralis (2 of 227; 0.9%), and G. intestinalis (63 of 227; 27.8%). Overall, 105 of 227 (46.2%) children were infected with at least one pathogenic helminth or protozoon. Table 2 shows the prevalence of parasite eggs found in the stool stratified by community.
Eosinophilia was identified in 49 of 226 (21.7%) children. In the bivariate analysis, the prevalence of eosinophilia varied by community, and it was highest in Ohuay (17 of 36; 47.2%) followed by Huayllapata (14 of 45; 31.1%), Chinchayhuasi (8 of 31; 25.8%), Huaqaycancha (6 of 53; 11.3%), Piscohuata (4 of 43; 9.3%), and Queunacancha (0 of 18; 0%; P < 0.01). Having an untreated source of drinking water at home and having any helminth or protozoa in the stool, including Blastocystis, were retained as predictors of eosinophilia in the backward logistic regression model (Table 4).
Discussion
Fascioliasis is an important public health problem in Andean countries of South America.2 Younger children are at higher risk for complications stemming from this chronic infection.16 Health authorities are beginning to implement control measures to decrease the burden of fascioliasis. Mass chemotherapy has been suggested as an intervention for fascioliasis in hyperendemic areas.17 This study in a sample of young children receiving mass chemotherapy with albendazole showed a fairly low prevalence of soil-transmitted helminths but a significant number of children with Fasciola eggs in the stool and eosinophilia. The former was associated with water sources.
The World Health Organization (WHO) advocates mass therapy with triclabendazole for fascioliasis in areas with a prevalence over 10%.17 However, the best practices to estimate prevalence have not been defined. In our study, the number of children with fascioliasis identified approached 10% when screening with one or two stool specimens. However, this number varied significantly between villages, ranging from 0% to 20%. Despite recent uncontrolled trials suggesting that triclabendazole is efficacious and safe in the treatment of fascioliasis, there are limited data on its safety in large populations with mainly uninfected children.18 Current diagnostic tests are too cumbersome to be implemented on a large scale in endemic communities. Thus, defining high prevalence areas is problematic. Sensitive and less burdensome tests for fascioliasis are needed to better define regions for either mass or targeted chemotherapy. In addition, the impact of preventive chemotherapy for fascioliasis on anemia and malnutrition should be evaluated before implementation.19,20
We noted an association between giardiasis and having Fasciola eggs in the stool. Esteban and others21,22 also noted this association in studies in high prevalence areas of the Peruvian and Bolivian Altiplano. We found that children who had an untreated water source at home were more likely to have Fasciola-positive stools, suggesting a role for water in transmission. However, the source of drinking water at home could also be a surrogate for poverty level and other unmeasured factors. By contrast, there was no clear association with consumption of watercress or other aquatic plants traditionally linked to fascioliasis transmission. Additional research is needed to clarify the route of transmission in the region studied, which may be important for control and prevention.
The prevalence of eosinophilia (> 500 eosinophils/μL) was 21%, suggesting the presence of tissue-invasive helminths.23 In addition, drinking water source at home was retained by the logistic regression model for eosinophilia. Despite the very high OR, this association failed to reach statistical significance, perhaps because of our small sample size. We suspect that many of the children with eosinophilia may have had acute or chronic Fasciola infection.24,25 Testing of one stool specimen probably limited our ability to detect low-intensity infections. Furthermore, Marcos and others13 described a strong association between eosinophil counts and Fasciola infection in highly endemic areas. Unfortunately, we were unable to perform serologic tests to confirm this finding. The low hookworm and Strongyloides prevalence in the area and the possible association of eosinophilia with water sources make these parasites unlikely explanations for the high eosinophil counts. However, the eosinophilia may have been caused by another unrecognized parasite.
Interestingly, some communities with a high prevalence of eosinophilia had a low number of children with Fasciola ova in stool. For example, the frequency of Fasciola eggs in stool in Ohuay was 0%, whereas eosinophilia was present in one-half of children. Stool studies 2 years before this study documented Fasciola ova in 6% of children in Ohuay,9 and the current absence of ova may reflect the poor sensitivity of a single microscopic examination, especially in early phases of infection. In acute infection before invasion of the biliary tract, fascioliasis cannot be detected by stool examination. Differences in timing of testing or transmission within communities may also have had an impact. The highest transmission rates are thought to occur during the rainy months (December to April) in inter-Andean valleys similar to Huancarani.2 However, it has been noted that the epidemiology of Fasciola infection is highly variable, even within small geographic regions.9,26 Thus, studies evaluating local patterns of transmission are important to tailor interventions based on regional data.
This study has limitations that may affect our ability to draw firm conclusions from our data. The small number of children included in the study, the number of children who were excluded because of missing information, and the small geographic area studied limit the power of our analysis and may affect the generalizability of our results. Most of our participants (62.6%) provided only one stool sample for testing. Testing of one stool specimen is an insensitive method to detect intestinal helminths and Fasciola, which likely led us to underestimate the prevalence of Fasciola infection in the area. Thus, our results may vary if more stringent diagnostic criteria are used. Nonetheless, the prevalence of Fasciola was only modestly different between those providing one versus two stool samples (9.1% versus 10.5%; P = 0.72). In addition, we were not able to test for antibodies against Fasciola, which would have been needed to detect acute infection. Therefore, we cannot directly address whether acute fascioliasis was the cause of eosinophilia.
In conclusion, our study showed a high prevalence of Fasciola-positive stools and eosinophilia in the communities of the Huancarani district in Cuzco receiving mass albendazole chemotherapy. Our data suggest that finding Fasciola eggs in the stool of children is associated with socioeconomic factors, giardiasis, and drinking water source in the Huancarani district. Importantly, we documented an association with water source rather than food, suggesting waterborne transmission in the area. A comprehensive approach to the study of these factors is required to generate creative and effective control interventions.
ACKNOWLEDGMENTS
The authors thank Ms. Limit Canales from Yanapanakusun non-profit organization for her assistance in data collection.
Disclaimer: The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the National Institutes of Health.
Footnotes
Financial support: This study was supported, in part, by National Institute for Allergies and Infectious Disease at the National Institutes of Health Grant 1R01AI104820-01.
Authors' addresses: Miguel M. Cabada, Universidad Peruana Cayetano Heredia and University of Texas Medical Branch Collaborative Research Center–Cuzco, Cuzco, Peru, and Department of Internal Medicine, University of Texas Medical Branch, Galveston, TX, E-mail: micabada@utmb.edu. Mary R. Goodrich, Brittany Graham, Pablo G. Villanueva-Meyer, and A. Clinton White Jr., School of Medicine, University of Texas Medical Branch, Galveston, TX, E-mails: mrgoodri@utmb.edu, bmgraham@utmb.edu, pevillan@utmb.edu, and acwhite@utmb.edu. Martha Lopez and Eulogia Arque, UPCH-UTMB Collaborative Research Center–Cuzco, Cuzco, Peru, E-mails: martlop2000@gmail.com and picis_11_90@hotmail.com.
References
- 1.World Health Organization Fascioliasis: Infection with the “Neglected” Neglected Worms. 2007. http://www.who.int/neglected_diseases/integrated_media/integrated_media_fascioliasis/en Available at. Accessed March 18, 2014.
- 2.Mas-Coma S, Valero MA, Bargues MD. Chapter 2: Fasciola, lymnaeids, and human fascioliasis, with a global overview of disease transmission, epidemiology, evolutionary genetics, molecular epidemiology, and control. Adv Parasitol. 2009;69:41–146. doi: 10.1016/S0065-308X(09)69002-3. [DOI] [PubMed] [Google Scholar]
- 3.Cabada MM, White AC., Jr New developments in the epidemiology, diagnosis, and treatment of fascioliasis. Curr Opin Infect Dis. 2012;25:518–522. doi: 10.1097/QCO.0b013e3283567b7e. [DOI] [PubMed] [Google Scholar]
- 4.Marcos LA, Maco V, Florencio L, Terashima A, Samalvides F, Espinoza JR, Miranda E, Tantaleán M, Gotuzzo E. Altas tasas de prevalencia de fasciolosis humana en el Peru: una enfermedad emergente. Rev Peru Enferm Infecc Trop. 2005;3:8–13. [Google Scholar]
- 5.Parkinson M, O'Neill SM, Dalton JP. Endemic human fasciolosis in the Bolivian Altiplano. Epidemiol Infect. 2006;26:1–6. doi: 10.1017/S095026880600728X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marcos LA, Maco V, Terashima A, Samalvides F, Gotuzzo E. Caracteristicas clínicas de la infección crónica por Fasciola hepatica en niños. Rev Gastroenterol Peru. 2002;22:228–233. [PubMed] [Google Scholar]
- 7.Marcos LA, Maco V, Castillo M, Terashima A, Serpa R, Gotuzzo E. Reporte de casos de fasciolasis en el Instituto Especializado de Salud del Nino, Lima- Peru (1988–2003) Rev Gastroenterol Peru. 2005;25:198–205. [PubMed] [Google Scholar]
- 8.El-Shazly AM, El-Nahas HA, Abdel-Mageed AA, El Beshbishi SN, Azab MS, Abou El Hasan M, Arafa WA, Morsy TA. Human fascioliasis and anaemia in Dakahlia governorate, Egypt. J Egypt Soc Parasitol. 2005;35:421–432. [PubMed] [Google Scholar]
- 9.Lopez M, White AC, Cabada MM. Burden of Fasciola hepatica infection among children from Paucartambo in Cuzco, Peru. Am J Trop Med Hyg. 2012;86:481–485. doi: 10.4269/ajtmh.2012.11-0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karahocagil MK, Akdeniz H, Sunnetcioglu M, Cicek M, Mete R, Akman N, Ceylan E, Karsen H, Yapici K. A familial outbreak of fascioliasis in eastern Anatolia: a report with review of literature. Acta Trop. 2011;118:177–183. doi: 10.1016/j.actatropica.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 11.Marcos LA, Terashima A, Leguia G, Canales M, Espinoza JR, Gotuzzo E. La infeccion por Fasciola hepatica en el Peru: una enfermedad emergente. Rev Gastroenterol Peru. 2007;27:389–396. [PubMed] [Google Scholar]
- 12.Mas-Coma S. Epidemiology of fascioliasis in human endemic areas. J Helminthol. 2005;79:207–216. doi: 10.1079/joh2005296. [DOI] [PubMed] [Google Scholar]
- 13.Marcos L, Maco V, Samalvides F, Terashima A, Espinoza JR, Gotuzzo E. Risk factors for Fasciola hepatica infection in children: a case-control study. Trans R Soc Trop Med Hyg. 2006;100:158–166. doi: 10.1016/j.trstmh.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 14.Zumaquero-Rıos JL, Sarracent-Perez J, Rojas-Garcıa R, Rojas-Rivero L, Martınez-Tovilla Y, Valero MA, Mas-Coma S. Fascioliasis and intestinal parasitoses affecting schoolchildren in Atlixco, Puebla State, Mexico: epidemiology and treatment with nitazoxanide. PLoS Negl Trop Dis. 2013;7:e2553. doi: 10.1371/journal.pntd.0002553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maco-Flores V, Marcos-Raymundo L, Terashima-Iwashita A, Samalbvides-Cuba F, Miranda-Sanchez E, Espinoza-Babilon J, Gotuzzo-Herencia J. Fas-2 ELISA and the Rapid Sedimentation Technique Modified by Lumbreras for Fasciola Hepatica Infection Diagnosis. 2002. http://www.scielo.org.pe/pdf/rmh/v13n2/v13n2ao3.pdf Available at. Accessed March 18, 2014.
- 16.Lozoff B, Beard J, Connor J, Barbara F, Georgieff M, Schallert T. Long-lasting neural and behavioral effects of iron deficiency in infancy. Nutr Rev. 2006;64((Suppl 2)):S34–S43. doi: 10.1301/nr.2006.may.S34-S43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization Fascioliasis Diagnosis, Treatment and Control Strategy. 2013. http://www.who.int/foodborne_trematode_infections/fascioliasis/fascioliasis_diagnosis/en/index.html Available at. Accessed March 11, 2014.
- 18.Villegas F, Angles R, Barrientos R, Barrios G, Valero MA, Hamed K, Grueninger H, Ault SK, Montresor A, Engels D, Mas-Coma S, Gabrielli AF. Administration of triclabendazole is safe and effective in controlling fascioliasis in an endemic community of the Bolivian Altiplano. PLoS Negl Trop Dis. 2012;76:e1720. doi: 10.1371/journal.pntd.0001720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taylor-Robinson DC, Maayan N, Soares-Weiser K, Donegan S, Garner P. Deworming drugs for soil-transmitted intestinal worms in children: effects on nutritional indicators, haemoglobin and school performance. Cochrane Database Syst Rev. 2012;11 doi: 10.1002/14651858.CD000371.pub5. CD000371. [DOI] [PubMed] [Google Scholar]
- 20.Awasthi S, Peto R, Read S, Richards SM, Pande V, Bundy D. DEVTA (Deworming and Enhanced Vitamin A) Team Population deworming every 6 months with albendazole in 1 million pre-school children in north India: DEVTA, a cluster-randomized trial. Lancet. 2013;381:1478–1486. doi: 10.1016/S0140-6736(12)62126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Esteban JG, Gonzalez C, Bargues MD, Angles R, Sánchez C, Náquira C, Mas-Coma S. High fascioliasis infection in children linked to a man-made irrigation zone in Peru. Trop Med Int Health. 2002;7:339–348. doi: 10.1046/j.1365-3156.2002.00870.x. [DOI] [PubMed] [Google Scholar]
- 22.Esteban JG, Flores A, Aguirre C, Strauss W, Angles R, Mas-Coma S. Presence of very high prevalence and intensity of infection with Fasciola hepatica among Aymara children from the northern Bolivian Altiplano. Acta Trop. 1997;66:1–14. doi: 10.1016/s0001-706x(97)00669-4. [DOI] [PubMed] [Google Scholar]
- 23.Heukelbach J, Poggensee G, Winter B, Wilcke T, Kerr-Pontes LR, Feldmeier H. Leukocytosis and blood eosinophilia in a polyparasitised population in north-eastern Brazil. Trans R Soc Trop Med Hyg. 2006;100:32–40. doi: 10.1016/j.trstmh.2005.06.021. [DOI] [PubMed] [Google Scholar]
- 24.Fica A, Dabanch J, Farias C, Castro M, Jercic MI, Weitzel T. Acute fascioliasis—clinical and epidemiological features of four patients in Chile. Clin Microbiol Infect. 2012;18:91–96. doi: 10.1111/j.1469-0691.2011.03575.x. [DOI] [PubMed] [Google Scholar]
- 25.Kaya M, Beştaş R, Çetin S. Clinical presentation and management of Fasciola hepatica infection: single-center experience. World J Gastroenterol. 2011;17:4899–4904. doi: 10.3748/wjg.v17.i44.4899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Esteban JG, Flores A, Angles R, Mas-Coma S. High endemicity of human fascioliasis between Lake Titicaca and La Paz valley, Bolivia. Trans R Soc Trop Med Hyg. 1999;93:151–156. doi: 10.1016/s0035-9203(99)90289-4. [DOI] [PubMed] [Google Scholar]