Abstract
Substance use and sexual risk behaviors are common among adolescents. Although attention has focused primarily on alcohol use, less is known about the relationship between marijuana use and sexual risk behavior among high-risk youth. Since truant youth often experience problems in school, troubled family situations, and other psychosocial problems, they represent an important group of high-risk youth to study. Previous research suggests that truant youth are at considerable risk of continuing their troubled behavior in school and entering the juvenile justice system. It is also likely that truant youth are involved in marijuana use and sexual risk behavior at a higher rate, than the general youth population. Involving them in effective intervention services could reduce these risk behaviors. The current study presents interim findings from a NIDA-funded experimental, brief intervention (BI) study involving truant youths and their parents/guardians. Longitudinal data were analyzed to study: (1) the relationships between the youths’ marijuana use and engaging in sexual risk behavior over time, and (2) the effects of a substance use BI on their marijuana use and sexual risk behavior. Analyses examined a growth model for parallel processes in marijuana use and sexual risk behavior, and an assessment of the effect of the intervention on linear and quadratic trends, and on subgroups of youth differing in their sexual risk behavior and marijuana use. Implications of the results for future research and service delivery are considered.
Introduction
Substance use and engaging in sexual risk behavior are highly prevalent among adolescents (Brodbeck, Matter, & Moggi, 2007; Centers for Disease Control and Prevention [CDC], 2009; Elkington, Bauermeister, Brackis-Bott, Dolezal, & Mellins, 2009; Komro, Tobler, & Maldonado-Molina, 2010; Murphy, Brecht, Herbeck, & Huang, 2009; Wetherill & Fromme, 2007; Yan, Chiu, Stoesch, & Wang, 2007). Involvement in sexual risk behavior places individuals at high risk for sexually transmitted diseases (STDs), including HIV (CDC, 2005; Whaley, 1999). Adolescents are among the highest risk groups for acquiring STDs and HIV (CDC, 2005), particularly youths having contact with the juvenile justice system (Bryan, Ray, & Cooper, 2007; Dembo, Belenko, Childs, Wareham, & Schmeidler, 2009; Hendershot, Magnan, & Bryan, 2010; Kingree, Braithwaite, & Woodring, 2000; Kingree & Phan, 2002), when compared to the general adolescent population (Morris, Harrison, Knox, Tromanhauser, & Marquis, 1995). Likely reasons for this disparity may be due to justice-involved youth having sex at a younger age, having a greater number of sexual partners, reporting lower rates of condom use, and higher levels of deviant behavior (Schmiege, Levin, Broaddus, & Bryan, 2009; Teplin, Mericle, McClelland, & Abram, 2003).
Considerable research has focused on the relationship between alcohol use and involvement in sexual risk behavior (e.g., lack of condom use, having multiple sex partners) (Cooper, 2002; Elkington et al., 2009; Goldstein, Barnett, Pedlow, & Murphy, 2007; Komro et al., 2010; Morris, Baker, Valentine, & Pennisi, 1995; Morris et al., 1995; Murphy et al., 2009; Wetherill & Fromme, 2007). Less attention has been given to the relationship between marijuana use and engaging in sexual risk behavior among adolescents (e.g., Hendershot, Magnan, & Bryan, 2010). This is surprising for several reasons. First, marijuana use is the second most prevalent substance used (behind alcohol) by youths, with 35% of 12th graders, 28% of 10th graders, and 14% of 8th graders in 2010 reporting past-year use (Office of National Drug Control Policy, 2010). Further, 2010 Monitoring the Future survey data indicate the use of the marijuana continues to increase among youth in each of these three grades, with nearly 1 of 6 high school seniors being daily or near daily users (Johnston, O’Malley, Bachman, & Schulenberg, 2010). Second, a growing number of studies indicate a significant covariance between marijuana use and engaging in sexual risk behavior (e.g., DeGenna, Cornelius & Cook, 2007; Hendershot, Magnan, & Bryan, 2010; Shrier, Harris, Sternberg, & Beardslee, 2001; Smith, Ferris, Simpson, Shelley, Pitts, & Richters, 2009). Third, there is some indication that marijuana use may be a stronger indicator of involvement in sexual risk behavior than alcohol (e.g., Hendershot, Magnan, & Bryan, 2010), particularly in situational association analyses (Kingree, Braithwaite, & Woodring, 2000) and event-level analyses (Kingree & Betz, 2003).
Growing evidence of an association between marijuana use and involvement in sexual risk behavior needs to be complemented by additional research that examines longitudinal relationships between these two behaviors. It is especially important to consider possible covariance in the rates of change in these behaviors over time, and to include biological data on youths’ marijuana use (since at-risk youth are likely to underreport use [Dembo et al., 1999]). Further, it is necessary to extend this line of research to high-risk youth, other than those having contact with the justice system—such as truant youth.
Relatedly, there is a need to develop interventions to reduce marijuana use and sexual risk behavior among youth. Interventions targeted to different at-risk groups of youths can be especially beneficial in reducing their long-term participation in these behaviors, in addition to their associated, adverse outcomes, such as contracting STDs and HIV/AIDS. In this vein, there is some evidence to indicate that drug prevention interventions can have “spillover” effects in reducing sexual risk behavior among youths (Ellickson, McCaffrey, & Klein, 2009).
We have not been able to identify any longitudinal studies examining marijuana use and sexual risk behavior among truant youth. Yet, truancy represents a very significant problem, and truant youths are at high risk (Arnette, 1995; Baker, Sigmon & Nugent, 2001; Center for Labor Market Studies, 2009). In addition to truant youth having problems in school, they frequently experience troubled family situations, failing grades, and psychosocial difficulties including drug use (Dembo & Turner, 1994). The limited number of available studies involving selected samples of truant youths indicate they often experience serious interrelated problems in regard to a stressed family life (Baker et al., 2001; Kearney & Silverman, 1995), alcohol and other drug use (Baker et al., 2001; Dembo & Turner, 1994; Diebolt & Herlache, 1991; Pritchard, Cotton & Cox, 1992), emotional and psychological functioning (Diebolt & Herlache, 1991; Dembo, Briones-Robinson et al., in press; Egger, Costello, & Angold, 2003; Kearney & Silverman, 1995), and poor educational functioning (e.g., low grades, grade retention or placement in remedial or special programs) (Dembo & Turner, 1994; Garry, 1996; Ingersoll & LeBoeuf, 1997). Research also suggests that truant youths are at considerable risk of continuing their troubled behavior in school and entering the juvenile justice system (Garry, 1996; Ingersoll & LeBoeuf, 1997; Loeber & Farrington, 2000; Puzzanchera, Stahl, Finnegan, Tierney, & Snyder, 2003; also see: Henry, Thornberry, & Huizinga, 2009).
Given these problem behaviors found among truant youth, it is reasonable to hypothesize they are engaging in substance use and sexual risk behavior at a higher rate than the general youth population (Eaton, Brener, & Kann, 2008). There is a need to develop and evaluate intervention strategies to reduce at-risk behaviors, and best serve truant youth and their families (Hawkins et al., 2000). Further, there is a need to follow these youths over time to learn the long term relationships between marijuana use and engaging in sexual risk behavior, and to assess the impact of risk reduction interventions on them.
There were four major objectives for the present study, which presents interim findings from an ongoing NIDA-funded, experimental, prospective intervention project involving truant youths and their parents/guardians. First, using growth model analysis, we sought to examine the longitudinal relationships between the youths’ involvement in marijuana use and sexual risk behavior. Second, we sought to assess the impact of a Brief Intervention (BI) targeting the youths’ substance use on their marijuana use and sexual risk behavior over time. Third, we sought to identify subgroups of youths involved in marijuana use and sexual risk behavior over time, and to assess the differential, longitudinal effects of the BI on their marijuana use and sexual risk behavior over a 12-month follow-up period. Drawing on the literature reviewed above, we examined three main hypotheses. (1) The youths’ marijuana use and sexual risk behavior will be related to each other over time. (2) Compared to youths’ not receiving BI services, youths’ receiving the BI will show a reduction in marijuana use and sexual risk behavior over time. (3) Marijuana use and sexual risk behavior subgroups of youths will be identified, and they will respond differently to BI services.
Method
Subjects
The main place of recruitment into the BI project occurred at the Truancy Intake Center (TIC) in the Hillsborough County Juvenile Assessment Center. Eligible youths met the following criteria: (1) aged 11 to 15, (2) no official record of delinquency or up to two misdemeanor arrests, (3) some indication of alcohol or other drug use, as determined by a screening instrument (PESQ [Winters, 1992]) or as reported by a Hillsborough County School District (HCSD) social worker located at the TIC, and (4) lived within a 25 mile radius of the TIC. Eligible youths were recruited for participation in the project from a community diversion program or referred by a HCSD social worker or guidance counselor. Project services were provided in-home, were free, and participation was voluntary. A discussion of the enrollment process appears in Dembo, Briones et al. (in press).
Following the completion of the consent and assent processes, and separate baseline interviews with the youth and his/her parent/guardian, the youth and parent/guardian were randomly assigned to one of three project service conditions: (1) the Standard Truancy Services (STS) plus a referral service overlay involving three in-home visits by a project staff member, (2) two BI sessions with the youth (Y), or (3) two BI sessions with the youth and an additional session with the parent (YP). All study procedures were approved and monitored by a local IRB.
Overview of the Brief Intervention
The primary goal of the BI therapist sessions is to promote abstinence and prevent relapse among drug using adolescents through the development of adaptive beliefs and problem-solving skills. The BI incorporates elements of Rational-Emotive Therapy (RET) and Problem-Solving Therapy (PST) to develop these adaptive beliefs and coping skills. The BI regards drug involvement as learned behavior that develops within a context of personal, environmental, and social factors (Catalano, Hawkins, Wells, & Miller, 1991; Clark & Winters, 2002) that shape and define drug use attitudes and behaviors. Developed over the course of an adolescent’s learning history and prior experience with drugs, maladaptive beliefs and coping skill deficits are viewed as primary determinants of drug use. The goal of the BI therapist sessions is to diminish factors contributing to drug use (e.g., maladaptive beliefs) and promote factors that protect against relapse (e.g., problem solving skills) (Winters & Leitten, 2007).
Following is a brief description of these BI sessions. The focus of the first session is on discussing information about the youth’s substance use and related consequences, the level of willingness to change, examining the causes and benefits of change, and discussing what goals for change the youth would like to select and pursue. Youth are allowed to pursue goals of drug abstinence or reduction in drug use. In the second session, the BI therapist reviews the youth’s progress with the agreed upon goals, identifies risk situations associated with difficulty in achieving goals, discusses strategies to overcome barriers toward goal achievement, reviews where the youth is in the state of change process, and negotiates either continuation or advancement of goals. Informed by an integrated behavioral and family therapy approach, the parent session (the third session) addresses the youth’s substance use issues, parent attitudes and behaviors regarding this use, parent monitoring and supervision to promote progress towards their child’s intervention goals, and parent communication skills to enhance youth-parent connectedness. Each session lasts for 1-1/4 hours, and the sessions occur about a week apart. With youth and parent/guardian permission, the BI sessions are tape recorded for fidelity assessment.
Initial and Follow-Up Interviews
In addition to the BI therapy sessions, research staff collect various baseline and follow-up data on the youth and their family throughout the project. The main data collection instruments used in the study were the Adolescent Diagnostic Interview (ADI, Winters & Henly, 1993), and the Parent/Guardian ADI (Winters & Stinchfield, 2003). Baseline interviews were completed with 200 youths and their parents/guardians between March 6, 2007 and December 3, 2010. Each youth and parent/guardian was paid $15 for completing the baseline interview. The baseline interviews for parents/guardians averaged 30 minutes; the youth interviews averaged one hour.
Depending on the month/year youths entered the project, 3-month (n = 166), 6-month (n = 148), and 12-month (n = 107) follow-up interviews were completed. Youth who began participation early in the project completed all three follow-up interviews; whereas youth who enrolled later may not yet have been due for all three follow-up interviews at the time of the present study. The three month follow-up interviews followed 90 days from the date of the youth’s last participation in project services (i.e., the last BI intervention or STS session). The 6-month follow-up interview date was scheduled for 90 days following completion of the 3-month follow-up interview; and the 12-month follow-up interview was scheduled for 180 days after the completion date of the 6-month follow-up interview. Each youth and parent/guardian was paid $15 for each follow-up interview. The majority of youths were interviewed in their home at each follow-up time point, while a very small number of youths were interviewed in secure program settings, such as residential commitment programs, county jails, or a juvenile detention center. For 3-month, 6-month, and 12-month follow-up interviews, respectively, 1.8%, 2.7%, and 1.7% of youth were interviewed in a secure program setting. Overall completion rates of 92.2%, 92.6% and 90.8% were achieved for the 3-month, 6-month, and 12-month follow-up interviews, respectively. Importantly, there was a low refusal rate for each follow-up (<8%). Of the completed follow-up interviews, 97% of the 3-month, 95% of the 6-month, and 97% of the 12-month interviews were completed within 60 days following the anniversary of their preceding interview. Similarly, high percentages of follow-up interviews were completed within 30 days of the date of last participation: 84% of the 3-month follow-up interviews, 84% of the 6-month follow-up interviews, and 85% of the 12-month follow-up interviews. (Due to space concerns, a table reporting these results has been omitted. A copy is available from the senior author upon request.)
Sample Characteristics
Most youths in the study were male (65%), and averaged 14.79 years in age (SD = 1.31). Thirty-eight percent of the youths were Caucasian, 26% were African American, 28% were Hispanic, 2% were Asian, and 7% were from other, mainly multi-ethnic backgrounds. Relatively few youths (14%) lived with both of their biological parents. In contrast, a majority of the youths were living either with their biological mother alone (34%) or with their mother and another adult (34%). Parents/guardians were asked to indicate their annual income range. Ten percent of the caretakers reported an annual income of more than $75,000, while 38% reported annual incomes of $25,000 or less. Median family income was $25,000 to $40,000.
Psychosocial Characteristics
The youths reported significant problems that were experienced by their families. Specifically, 56% reported a family history of substance abuse problems, and 34% indicated a family history of mental health problems.
The youths also reported they had experienced significant psychosocial problems. Nineteen percent of the youths claimed ever having had a substance abuse problem, and 9% reported they had received substance abuse treatment. In addition, 46% of the youths claimed they had received treatment for emotional or behavioral problems; and, 19% reported they were sent to live away from home due to behavior problems at some point in their lives.
Measures
Covariate measure of ADHD
Four questions keyed to DSM-IV criteria for ADHD were included in the youth ADI interviews (Winters & Henly, 1993). Large percentages of youths (noted in parentheses) reported ever experiencing one or more of these issues: (1) Do you often get complaints from parents/teachers that you don’t listen to instructions or directions? (57%); (2) Do you frequently tend to act before thinking? (70%); (3) Do you often have difficulty waiting for your turn during games or when doing things with other people your age? (33%); and (4) Do you often fidget and find it difficult to sit still? (54%).
Confirmatory factor analysis (CFA) was used to assess how well a one factor model, involving each of the four ADHD items, fit the data (Muthèn & Muthèn, 1998–2010). Bayesian estimation (discussed in the Strategy of Analysis section) was used to assess the CFA model. Results indicated the CFA model fit the data quite well. Good convergence-mixing (Potential Scale Reduction = 1.07), model fit (Posterior Predictive p-value = 0.42), and significant standardized loadings were obtained. (A table reporting these results has been omitted due to space concerns. A copy is available from the corresponding author upon request.) Therefore, scores were saved for the single factor and used as a covariate in subsequent analyses.
Marijuana use
Marijuana use was measured through self-report questions on the ADI (Winters & Henly, 1993) and the results of urine tests (UA), both of which were administered at baseline interview and at each follow-up interview. The ADI questions probed the use of marijuana as: never, less than five times, or five or more times. Urine specimens were also collected to assess recent drug use. The use of four substances was probed using the Onsite CupKit® urine screen procedure (positive threshold levels are noted in parentheses): (1) methamphetamines (1000 nanograms per milliliter [ng/ml] of urine), (2) opiates (300 ng/ml of urine), (3) cocaine (300 ng/ml of urine), and (4) marijuana (THC) (50 ng/ml of urine). No urine testing was done for alcohol use. Following are the surveillance windows for the four drugs: methamphetamines and opiates = 48 hours; cocaine = 72 hours; marijuana: moderate users = 5 days, heavy users = 10 days, and chronic users = 20 days. At each time point, very few youths (<5%) were urine test positive for amphetamines, cocaine, or opiates. On the other hand, marijuana use was highly prevalent.
For each time point (baseline, 3-month, 6-month, and 12-month follow-ups), we combined the self-reported marijuana and marijuana urine test data into an overall measure of marijuana use involving six categories: (1) marijuana use denied, and UA test for marijuana negative; (2) marijuana use denied, and UA test data missing (due to reasons beyond the youth’s control [e.g., incarcerated]); (3) UA test data missing and UA sample/specimen refused (not due to reasons beyond the youth’s control [e.g., participant refusal]); (4) UA test missing or negative for marijuana, but youths reported marijuana use one to four times; (5) UA test missing or negative, but youth reported marijuana use five or more times; (6) UA test positive for marijuana. A frequency breakdown of the six marijuana use categories at each time point indicated there were few or no youths in categories 2 and 3. Hence, categories one to three were combined, and the resulting four ordinal category measure used in further analyses. The ordinal measure categories ranged from UA test confirmed non-use of marijuana to UA test positive results for use of the substance. The distribution of these data is presented in Table 1.
Table 1.
Marijuana Use Over Time (Self-Report and Urine Test Results)
| Baseline | n | % |
|---|---|---|
| Denied use and urine test results negative (n = 12) or refused to provide urine specimen (n = 2) | 14 | 7 |
| Urine test missing or negative, but youth reported use 1–4 times | 36 | 18 |
| Urine test missing or negative, but youth reported use 5 or more times | 58 | 29 |
| Urine test positive | 92 | 46 |
|
| ||
| 200 | 100% | |
| 3-Month follow-up | n | % |
|---|---|---|
| Denied use and urine test results negative (n = 66) or not provided due reasons beyond youth’s control (n = 3) or refused to provide urine specimen (n = 5) | 74 | 45 |
| Urine test missing or negative, but youth reported use 1–4 times | 21 | 13 |
| Urine test missing or negative, but youth reported use 5 or more times | 12 | 7 |
| Urine test positive | 59 | 36 |
|
| ||
| 166 | 101% | |
| 6-Month follow-up | n | % |
|---|---|---|
| Denied use and urine test results negative (n = 46) or not provided due reasons beyond youth’s control (n = 6) or refused to provide urine specimen (n = 6) | 58 | 39 |
| Urine test missing or negative, but youth reported use 1–4 times | 12 | 8 |
| Urine test missing or negative, but youth reported use 5 or more times | 14 | 10 |
| Urine test positive | 64 | 43 |
|
| ||
| 148 | 100% | |
| 12-Month follow-up | n | % |
|---|---|---|
| Denied use and urine test results negative (n = 35) or not provided due reasons beyond youth’s control (n = 2) | 37 | 35 |
| Urine test missing or negative, but youth reported use 1–4 times | 7 | 6 |
| Urine test missing or negative, but youth reported use 5 or more times | 12 | 11 |
| Urine test positive | 51 | 48 |
|
| ||
| 107 | 100% | |
As can be seen, following baseline there is an increase in the percent of youths with marijuana involvement, especially urine test positive results, from 3-month to 12-month follow-up interview. There is a corresponding, general decrease in the percent of youths with less marijuana use. It is important to note that, at each time point, urine test results confirmed denial of use in the vast majority of cases (86%, 89%, 79%, and 94% at baseline, 3-month follow-up, 6-month follow-up, and 12-month follow-up, respectively).
Sexual risk behavior
We probed the youths’ involvement in sexual risk behavior at baseline and at each follow-up interview using the POSIT HIV/STD Risk Behavior instrument. The POSIT 11-item HIV/STD risk scale was developed by the NOVA Research Company (Young & Rahdert, 2000). The instrument has been pilot tested and IRT analysis has found the scale to have very good psychometric properties (e.g., internal consistency = 0.80, one-week test-retest reliability = 0.90; concurrent validity with the Sexual Risk Questionnaire scores: r = 0.80). In the present study, the internal consistency (Cronbach’s Alpha) of the 11-item HIV/STD risk scale was 0.76.
Table 2 presents the baseline (lifetime) data for all 11 items. As can be seen, large percentages of youths reported close friends having had sex, and 66% of the youths reported they had sexual intercourse. Importantly, sizable percentages of youths indicated they had sexual intercourse without using a condom (34%), and had 2 or more sexual partners (32%). Comparison of these results with findings reported in the Centers of Disease Control, 2009 Youth Risk Behavior Surveillance (YRBS, CDC, 2009), indicates a higher rate of ever having had sexual intercourse among youths in our study, than that reported by youths in the YRBS (46%). This result is consistent with the expectation, noted earlier, that truant youth engage in sexual risk behavior at a higher rate than the general youth population.
Table 2.
Self-Reported Sexual Risk Behaviors: Baseline
| Baseline (Ever) (n=198 or 200) (%) | |
|---|---|
| 1. Have any of your close friends had sex? | 80 |
| 2. Have you had any kind of sexual contact with another person? | 82 |
| 3. Have you had sexual intercourse? | 66 |
| 4. Have you had sexual intercourse without using a condom? | 34 |
| 5. Do you find it difficult to use condoms every time you have sex? | 13 |
| 6. Have you thought you or your partner might be pregnant? | 28 |
| 7. Have you been or gotten someone pregnant? | 4 |
| 8. Have you been tested for HIV? | 16 |
| 9. Have you had sex with two or more people? | 32 |
| 10. Have you had anal intercourse (sex in the butt)? | 6 |
| 11. Have you had a sexually transmitted disease (STD)? | 2 |
Lack of condom use and number of sexual partners are widely used sexual risk behavior measures in related research (Brook, Balka, Abernathy, & Hamburg, 1994; Bryan et al., 2007; Cooper, 2002; Elkington et al., 2009; Goldstein et al., 2007; Komro et al., 2010; Morris et al., 1995, 1998; Murphy et al., 2009; Wetherill & Fromme, 2007). Hence, we developed a measure to focus on engaging in these two most prominent indicators of sexual risky behaviors at each time point from the youths’ replies to these items, which consisted of three ordinal categories: 0 = engaged in none of the two sexual risk behaviors (i.e., sexual intercourse without using a condom, had 2 or more sexual partners), 1 = engaged in one of the two sexual risk behaviors, 2 = engaged in both sexual risk behaviors.
The top half of Table 3 shows the percent of youths replying affirmatively to each sexual risk behavior item at each time point. The bottom half of the table displays the results for the summary measure we developed from the youths’ replies to these questions across the four time points. For the summary measure, there is a gradual increase in the percent of youths reporting engaging in both sexual risk behaviors from 3-month to 12-month follow-up, and a corresponding, general decrease in the percent of youths reporting not engaging in any of these behaviors or in one of them. (Although from 45% to 55% of youths did not report engaging in one or the other of the two sexual risk behaviors, it is important to note that the vast majority of youths reported having some sexual experience [e.g., sexual contact with another person] at each time point [baseline, 82%; 3-month follow-up, 72%; 6-month follow-up, 76%; 12-month follow-up, 81%]).
Table 3.
Prevalence of Sexual Risk Behavior Items and Summary Measure at Various Time Points
| Lifetime at Baseline (n=199) | 3-month follow up (n=164 or 165) | 6-month follow up (n=147) | 12-month follow up (n=107) | |
|---|---|---|---|---|
| Sexual Risky Behavior | ||||
| Had sexual intercourse without using a condom | 34% | 29% | 31% | 36% |
| Had sex with two or more people | 32% | 33% | 36% | 41% |
|
| ||||
| Sexual Risk Summary Measure | ||||
| None | 53% | 55% | 50% | 45% |
| 1 sexual risk behavior | 29% | 29% | 32% | 34% |
| Both sexual risk behaviors | 18% | 16% | 18% | 22% |
| Total | 100% | 100% | 100% | 101% |
Note. Percents may not total 100% due to rounding. The sexual risk summary measure combines (1) had sexual intercourse without using a condom, and (2) had sex with two or more people.
Comparison of Intervention Groups Demographics and Baseline Marijuana Use and Sex Risk Behavior Measures
Comparisons were made across the three intervention groups (Brief Intervention-Youth, Brief Intervention-Youth-Parent, and Standard Truancy Services) in regard to: (a) gender, age, African American and Hispanic ethnicity, (b) marijuana use and lifetime involvement in sexual risk behavior (measured at baseline), and (c) the factor scores for ADHD (a covariate in our analyses, following the work of Bryan et al., 2007). Results indicated the three groups were similar on all these comparison variables.
Results
The Parallel Growth Model
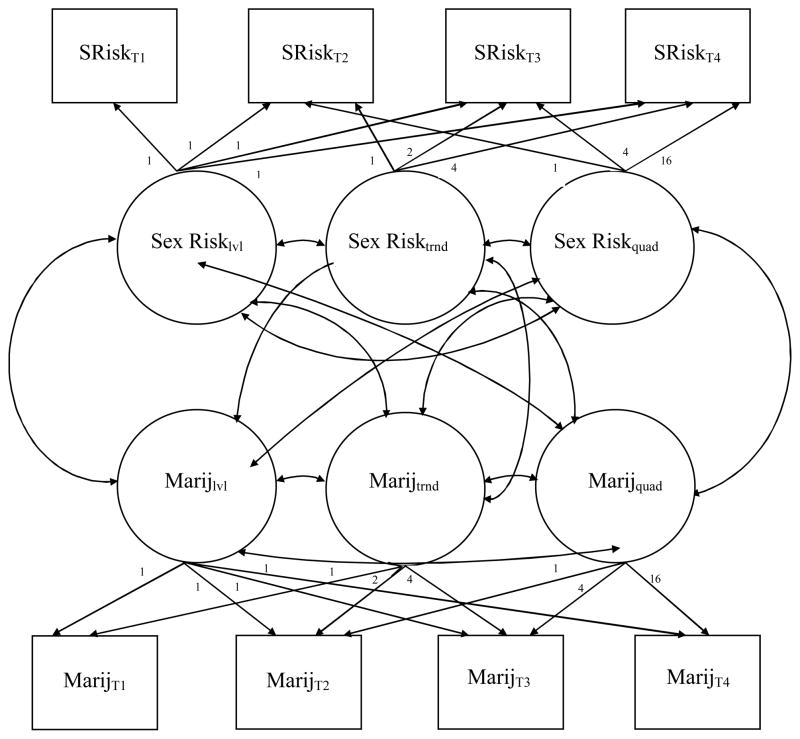
Figure 1 presents the parallel growth model we tested. The sexual risk portion of the model was estimated with linear and quadratic growth trends across four time points, and, as discussed below, the marijuana use portion of the model was estimated with linear and quadratic growth trends across the four time points. The time specification of the model accommodated to the unequal measurement points (3-month follow-up, 6-month follow-up, and 12-month follow-up). Covariances were specified between each pair of growth model latent variables reflecting sexual risk level, sexual risk linear trend, and sexual risk quadratic trend, and marijuana use level, marijuana use linear trend, and marijuana use quadratic trend.
Figure 1. Parallel Process Model for Sexual Risk Behavior and Marijuana Use.
Note. SRiskT1, SRiskT2, SRiskT3, SRiskT4 = Sexual Risk Behavior at time 1 (baseline) to time 4 (12-month follow-up), respectively. MarijT1, MarijT2, MarijT3, MarijT4 = Marijuana Use at time 1 (baseline) to time 4 (12-month follow-up), respectively. Lvl = Level. Trnd = Linear Trend. Quad = Quadratic Trend.
Strategy of Analysis
Latent growth modeling (see Duncan, Duncan, Strycker, Li, & Alpert, 1999) was used to examine growth in two constructs, marijuana use and sexual risk behavior, across the four time points over the period of one year. In latent growth models, longitudinal data are modeled as resulting from latent variables of a mean trend for the population while allowing for differences among individuals. The growth model analyses were completed using Mplus Version 6.1 (Muthèn & Muthèn, 2010), a multivariate statistical modeling program that estimates a variety of models for continuous and categorical observed and latent variables. We estimated separate growth models for the youths’ marijuana use and involvement in sexual risk behavior, as well as the parallel process growth model shown in Figure 1, using Bayesian estimation procedures.
Maximum likelihood (ML) estimation procedures are currently widely used in statistical analyses. In recent years, however, Bayesian analysis has become increasingly used. Bayesian estimation is a preferred approach for analyzing relatively complex models, when data are sparse or samples are small—where asymptotic distributions, underlying ML/other frequentist estimation procedures, are unlikely to hold (Gelman, Carlin, Stern, & Rubin, 2004; Lynch, 2010; Rupp, Dey & Zumbo, 2004; Scheines, Hoijtink, & Boomsma, 1999). When samples are large, the results of ML and Bayesian analyses tend to be similar. Bayesian analysis is firmly established in mainstream statistics.
Two estimates of model adequacy are important in Bayesian analysis: convergence and mixing, and model fit. In Bayesian analysis, Markov Chain Monte Carlo (MCMC) estimation algorithms are used to make random draws of parameter values, resulting in an approximation of the joint distribution of all parameters in the analysis. Usually, several MCMC chains are used, involving different starting values and different random seeds in making the random draws (Muthén & Asparouhov, 2010; also see: Lynch, 2010). The Gelman-Rubin diagnostic (Gelman & Rubin, 1992; also see: Gelman et al., 2004), referred to as the potential scale reduction (PSR) factor, is often used to assess convergence-mixing. A PSR value close to 1, and below 1.1, is considered as evidence that convergence and adequate mixing has been achieved.
Model fit refers to assessing whether the model fits the data well enough to permit the drawing of inferences about the parameters (Lynch, 2010). A widely used approach for examining model fit is posterior predictive distribution checking, introduced by Gelman, Meng, Stern, and Rubin (1996), and refined by Gelman et al. (2004). As implemented in Mplus (Muthèn & Muthèn, 2010), a posterior predictive p-value (PPP) fit statistic is based on the commonly used likelihood-ratio chi-square test of an H0 model against an unrestricted H1 model (Muthèn & Asparouhov, 2010). A low PPP value (e.g., .05 or .01 [see: Asparouhov & Muthèn, 2010]) indicates a poor fit, whereas values around 0.5 reflect an excellent fit.
Because the time of entry into the study determined the number of follow-up interviews each youth and parent/guardian received, the data that are missing are a consequence of the study design. Accordingly, in the Bayesian analyses missing data were replaced in Mplus by a simulated value using a regression-prediction algorithm (Muthèn & Muthèn, 2010).1 Since there is a scant literature on the topic of this paper, the Bayesian analyses were performed without informed priors.
We began our analyses by estimating separate latent growth models to examine whether there: (1) were linear or quadratic trends in marijuana use over time, and whether there was individual variability in this behavior, and (2) were linear or quadratic trends in involvement in sexual risk behavior over time, and whether there was individual variability in these activities. For these constructs, the intercept (i.e., level) and linear and quadratic trend factors were estimated across four time points (baseline, 3-month follow-up, 6-month follow-up, and 12-month follow-up). Finally, we combined the separate models to examine a growth model for parallel processes in these two types of behavior.
Adjusting for Time at Risk
Time in a secure setting reduces the likelihood of engaging in risk behavior. Hence, for each youth, we determined in each follow-up period, the number of days he/she spent in a secure facility (e.g., detention center, jail, residential commitment program, detoxification facility, treatment program). Study of the data indicated there was no need to adjust for time at risk in our analyses for four main reasons: (1) relatively few youths were placed in a secure facility during the 3-month, 6-month (a 90 day period), and 12-month (a 180 day period) follow-up periods: 5%, 7% and 11%, respectively, (2) the average number of days placed in a secure facility during each of these follow-up periods were relatively few (1.4 days, 3.2 days, 4.2 days, respectively), (3) the correlations between the number of the days spent in a secure facility during each follow-up period and the youths’ reported marijuana use during that period were low and non-significant (correlation range: −.102 to .036), and (4) the correlations between the number of the days spent in a secure facility during each follow-up period and the youths’ reported involvement in sexual risk behavior during that period were also low and non-significant (correlation range: −.121 to .145).
Marijuana Use Growth Model
Growth model analysis of the hypothesized model indicated acceptable convergence-mixing and fit of the model to the data. A PSR value of 1.06 and a PPP value of 0.11 were obtained.2
Sexual Risk Behavior Growth Model
Next, we completed a growth model analysis of the sexual risk behavior summary measures. Results indicated a good fit of the model to the data (PSR = 1.07; PPP = 0.31)3
Growth Model for Parallel Marijuana Use—Sexual Risk Behavior Processes
As Table 4 shows, parallel process growth model analysis of marijuana use and sexual risk behavior indicated good model convergence-mixing and fit (PSR = 1.08; PPP = 0.19). As can be seen, overall three of the fifteen latent variable covariances (20%) were statistically significant, including one of the nine quadratic trend covariances. The significant covariances were: (1) marijuana use level and marijuana use linear trend (estimate = 0.509, posterior SD = 0.182, one-tailed p-value <.001), (2) sexual risk behavior level and marijuana use level (estimate = 0.624, posterior SD = 0.197, one-tailed p-value <.001), and (3) sexual risk behavior linear trend and sexual risk behavior quadratic trend (estimate = −0.059, posterior SD = 0.041, one-tailed p-value <.01). Of particular note, compared to youths with no or little involvement in marijuana use at baseline, youths more involved in marijuana use were significantly more likely to report a greater level of involvement in sexual risk behavior. These results provide partial support for Hypothesis 1 informing this study. Significant variances were also obtained for sexual risk level, linear trend, and quadratic trend, as well as marijuana use level, linear trend, and quadratic trend, indicating significant variation in both these behaviors at baseline and over time.
Table 4.
Parallel Process Growth Model of Youths’ Sex Risk Behavior and Marijuana Use
| Bayesian Estimation | Estimate | Posterior SD | One-Tailed P-Value | 95% CI
|
|
|---|---|---|---|---|---|
| Lower 2.5% | Upper 2.5% | ||||
| Marijuana Use Level | |||||
| Marijuana T1 | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Marijuana T2 | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Marijuana T3 | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Marijuana T4 | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Marijuana Use Linear Trend | |||||
| Marijuana T1 | 0.000 | 0.000 | 1.000 | 0.000 | 0.000 |
| Marijuana T2 | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Marijuana T3 | 2.000 | 0.000 | 0.000 | 2.000 | 2.000 |
| Marijuana T4 | 4.000 | 0.000 | 0.000 | 4.000 | 4.000 |
| Marijuana Use Quadratic Trend | |||||
| Marijuana T1 | 0.000 | 0.000 | 1.000 | 0.000 | 0.000 |
| Marijuana T2 | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Marijuana T3 | 4.000 | 0.000 | 0.000 | 4.000 | 4.000 |
| Marijuana T4 | 16.000 | 0.000 | 0.000 | 16.000 | 16.000 |
| Sexual Risk Level | |||||
| Sexual Risk T1 | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Sexual Risk T2 | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Sexual Risk T3 | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Sexual Risk T4 | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Sexual Risk Linear Trend | |||||
| Sexual Risk T1 | 0.000 | 0.000 | 1.000 | 0.000 | 0.000 |
| Sexual Risk T2 | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Sexual Risk T3 | 2.000 | 0.000 | 0.000 | 2.000 | 2.000 |
| Sexual Risk T4 | 4.000 | 0.000 | 0.000 | 4.000 | 4.000 |
| Sexual Risk Quadratic Trend | |||||
| Sexual Risk T1 | 0.000 | 0.000 | 1.000 | 0.000 | 0.000 |
| Sexual Risk T2 | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Sexual Risk T3 | 4.000 | 0.000 | 0.000 | 4.000 | 4.000 |
| Sexual Risk T4 | 16.000 | 0.000 | 0.000 | 16.000 | 16.000 |
| Marijuana Use Linear Trend WITH | |||||
| Marijuana Use Level | 0.509 | 0.182 | 0.000 | 0.194 | 0.967 |
| Marijuana Use Quadratic Trend WITH | |||||
| Marijuana Use Level | −0.030 | 0.068 | 0.325 | −0.167 | 0.091 |
| Marijuana Use Linear Trend | −0.120 | 0.123 | 0.174 | −0.384 | 0.072 |
| Sexual Risk Level WITH | |||||
| Marijuana Use Level | 0.624 | 0.197 | 0.000 | 0.296 | 1.075 |
| Marijuana Use Linear Trend | 0.361 | 0.459 | 0.146 | −0.260 | 1.580 |
| Marijuana Use Quadratic Trend | 0.140 | 0.191 | 0.244 | −0.214 | 0.537 |
| Sexual Risk Linear Trend WITH | |||||
| Marijuana Use Level | 0.032 | 0.133 | 0.382 | −0.230 | 0.302 |
| Marijuana Use Linear Trend | 0.043 | 0.190 | 0.396 | −0.372 | 0.412 |
| Marijuana Use Quadratic Trend | −0.020 | 0.066 | 0.276 | −0.235 | 0.057 |
| Sexual Risk Level | −0.224 | 0.351 | 0.218 | −1.062 | 0.333 |
| Sexual Risk Quadratic Trend WITH | |||||
| Marijuana Use Level | 0.023 | 0.039 | 0.271 | −0.061 | 0.098 |
| Marijuana Use Linear Trend | 0.037 | 0.066 | 0.269 | −0.069 | 0.194 |
| Marijuana Use Quadratic Trend | 0.011 | 0.021 | 0.252 | −0.022 | 0.061 |
| Sexual Risk Level | 0.121 | 0.094 | 0.052 | −0.037 | 0.348 |
| Sexual Risk Linear Trend | −0.059 | 0.041 | 0.010 | −0.172 | −0.008 |
| Means | |||||
| Marijuana Use Level | 0.000 | 0.000 | 1.000 | 0.000 | 0.000 |
| Marijuana Use Linear Trend | −0.983 | 0.159 | 0.000 | −1.279 | −0.654 |
| Marijuana Use Quadratic Trend | 0.255 | 0.049 | 0.000 | 0.152 | 0.349 |
| Sexual Risk Level | 0.000 | 0.000 | 1.000 | 0.000 | 0.000 |
| Sexual Risk Linear Trend | 0.023 | 0.158 | 0.445 | −0.315 | 0.348 |
| Sexual Risk Quadratic Trend | −0.035 | 0.043 | 0.222 | −0.109 | 0.062 |
| Thresholds | |||||
| Sexual Risk T1$1 | 0.065 | 0.152 | 0.306 | −0.191 | 0.416 |
| Sexual Risk T1$2 | 1.893 | 0.182 | 0.000 | 1.514 | 2.242 |
| Sexual Risk T2$1 | 0.065 | 0.152 | 0.306 | −0.191 | 0.416 |
| Sexual Risk T2$2 | 1.893 | 0.182 | 0.000 | 1.514 | 2.242 |
| Sexual Risk T3$1 | 0.065 | 0.152 | 0.306 | −0.191 | 0.416 |
| Sexual Risk T3$2 | 1.893 | 0.182 | 0.000 | 1.514 | 2.242 |
| Sexual Risk T4$1 | 0.065 | 0.152 | 0.306 | −0.191 | 0.416 |
| Sexual Risk T4$2 | 1.893 | 0.182 | 0.000 | 1.514 | 2.242 |
| Marijuana T1$1 | −1.497 | 0.110 | 0.000 | −1.679 | −1.230 |
| Marijuana T1$2 | −0.745 | 0.098 | 0.000 | −0.924 | −0.521 |
| Marijuana T1$3 | 0.019 | 0.101 | 0.405 | −0.143 | 0.253 |
| Marijuana T2$1 | −1.497 | 0.110 | 0.000 | −1.679 | −1.230 |
| Marijuana T2$2 | −0.745 | 0.098 | 0.000 | −0.924 | −0.521 |
| Marijuana T2$3 | 0.019 | 0.101 | 0.405 | −0.143 | 0.253 |
| Marijuana T3$1 | −1.497 | 0.110 | 0.000 | −1.679 | −1.230 |
| Marijuana T3$2 | −0.745 | 0.098 | 0.000 | −0.924 | −0.521 |
| Marijuana T3$3 | 0.019 | 0.101 | 0.405 | −0.143 | 0.253 |
| Marijuana T4$1 | −1.497 | 0.110 | 0.000 | −1.679 | −1.230 |
| Marijuana T4$2 | −0.745 | 0.098 | 0.000 | −0.924 | −0.521 |
| Marijuana T4$3 | 0.019 | 0.101 | 0.405 | −0.143 | 0.253 |
| Variances | |||||
| Marijuana Use Level | 0.587 | 0.152 | 0.000 | 0.362 | 0.951 |
| Marijuana Use Linear Trend | 1.051 | 0.519 | 0.000 | 0.239 | 2.137 |
| Marijuana Use Quadratic Trend | 0.140 | 0.061 | 0.000 | 0.065 | 0.299 |
| Sexual Risk Level | 2.949 | 0.784 | 0.000 | 1.497 | 4.515 |
| Sexual Risk Linear Trend | 0.250 | 0.146 | 0.000 | 0.101 | 0.667 |
| Sexual Risk Quadratic Trend | 0.056 | 0.015 | 0.000 | 0.035 | 0.093 |
Note. T1 = Baseline. T2 = 3-month follow-up. T3 = 6-month follow-up. T4 = 12-month follow-up. Convergence: Potential Scale Reduction = 1.08. Model fit: Posterior Predictive p-value = 0.19.
Demographic and Intervention Condition Predictors of Growth Model Latent Variables
We also examined the relationship between: (1) the youths’ age, gender, being African-American, being Hispanic, and ADHD factor scores and the marijuana use and sexual risk behavior level, linear trend, and quadratic trend latent variables, and (2) intervention condition. Since there were a relatively small number of cases in each of the intervention conditions (Y, n = 65; YP, n = 68; STS, n = 67), limiting statistically meaningful three group comparisons, an overall intervention effect was studied—involving a comparison between Y and YP vs STS youths.
The following significant effects were found: (a) older youths reported more involvement in sexual risk behavior at baseline than younger youths; (b) girls had lower rates of increase in sexual risk behavior over time than male youths; (c) youths with higher ADHD scores had a higher rate of linear increase in marijuana use over time; and (d) the quadratic trend for marijuana use over time was less marked for high ADHD youths than youths with lower baseline ADHD scores. In contrast to the work of Bryan et al. (2007), we found no significant impulsivity effect (measured by our ADHD variable) on sexual risk trend. Further, no overall, significant intervention effects were found on the marijuana use and sexual risk behavior linear trend or quadratic trend latent variables.4
Growth Mixture Modeling with Sexual Risk Behavior and Marijuana Use Latent Trajectory Classes
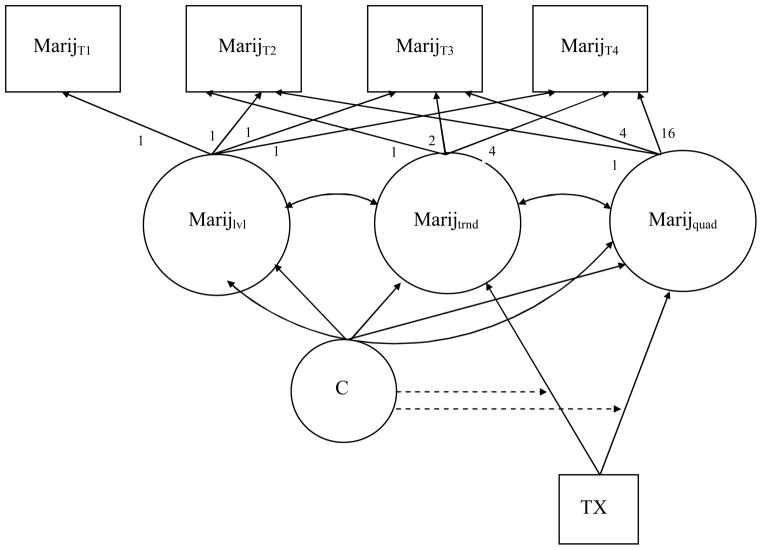
We examined the possibility that the data across the four time points contained youth subgroups differing in their sexual risk behavior (Murphy et al., 2009) and marijuana use over time. Growth mixture modeling was used in this effort (Muthèn & Muthèn, 2010). Figure 2 presents the growth mixture model we estimated. The model depicts marijuana use over time. A similar model was estimated for involvement in sexual risk behavior.
Figure 2. Growth Mixture Model of Intervention Effect on Marijuana Use Among Marijuana Use Subgroups.
Note. MarijT1, MarijT2, MarijT3, MarijT4 = Marijuana Use at time 1 (baseline) to time 4 (12-month follow-up), respectively; lvl = level; trnd = linear trend; quad = quadratic trend. C = latent class. TX = BI treatment effect.
Latent class analysis (LCA) models were estimated for a series of models including one, two, three, and four classes. Maximum likelihood estimation, involving standard errors and chi-square test statistics that are robust to non-normality, was used in these analyses. The LCA fit indices indicated a three class-solution best fit the sexual risk behavior data, and a three class-solution best fit the marijuana use data. For each of the sexual risk behavior and marijuana use subgroups involved in the growth mixture model analyses, the intercepts and slopes were permitted to vary within each class.
Three subgroups were identified in the sexual risk behavior data over time: (1) a low sexual risk behavior group (n = 100, 50.0% of the 200 youths), (2) a moderate level sexual risk behavior group (n = 62, 31.0%), and (3) a high level sexual risk behavior group (n = 38, 19.0%).5 Analysis found no significant, overall BI intervention effect (Y & YP vs STS) for any of these three sexual risk behavior subgroups.
The three subgroups identified in the marijuana use data over time were: (1) a lower level, escalating marijuana use group (n = 90, 44.8% of the 200 youths), (2) a continuing, high level marijuana use group (n = 81, 40.4%), and (3) a higher rate of escalating marijuana use group (n = 29, 14.5%)—characterized by an increasing involvement in marijuana use from baseline to 12-month follow-up.6 Analysis indicated a non-significant, overall BI intervention effect (Y & YP vs STS) on linear trend for subgroup (2), continuing, high level of use (estimate = −1.723, SE = 1.101, critical ratio = −1.565, p = 0.118 [.059 for a one-tailed test]).
We also regressed the latent class variables on the overall BI treatment effect (Y & YP vs STS). No significant effects were found.
We appreciate the power of the comparisons for the sexual risk behavior and marijuana use subgroups is rather low, due to the small sample sizes. The p-value for the treatment effect (Y & YP vs STS) was just above the .10 significance level for continuing, high level marijuana use youths. We plan to study these relationships again in planned, future analyses, at which time we expect more youths/families will be involved in the project and the power for analyses will be increased.
Conclusion
The main objectives of this study involved: (1) completion of a parallel growth model analysis of the longitudinal relationships between sexual risk behavior and marijuana use for truant youth, (2) examining the overall effect of a Brief Intervention on marijuana use and sexual risk behavior linear and quadratic trends among these youths, and (3) completing a growth mixture model analysis to identify subgroups of sexual risk and marijuana use subgroups to, among other things, test the effect of a Brief Intervention on these two risk behaviors over time. Several important findings were obtained in achieving these objectives, which were noted in the results section. In particular, youths who were more involved in marijuana use at baseline were significantly more likely to report a greater level of involvement in sexual risk behavior. This finding provides partial support for Hypothesis 1 informing this study. One explanation for this relationship asserts that involvement in marijuana use and engaging in sexual risk behavior are indicators of an underlying “proneness to deviance,” wherein engaging in one risk behavior is associated with engaging in others (Jessor & Jessor, 1977; Winters, Botzet, Fahnhorst, Baumel, & Lee, 2009). It would be important for future research to include assessments of multiple risk behaviors in their modeling frameworks, in order to gain a more comprehensive understanding of this phenomenon.
As noted in the results section, no overall, significant intervention effects were found on the sexual risk behavior or marijuana use linear trend or quadratic trend latent variables. The lack of an overall BI effect on these two risk behaviors over time did not support Hypothesis 2. However, as discussed below, further analysis indicated different subgroups existed among youths involved in sexual risk behavior and marijuana use over time, which provided a more nuanced understanding of the BI effect.
As reported in the results section, relatively few sociodemgraphic effects were found: (a) age was positively related to reported involvement in sexual risk behavior at baseline, (b) girls reported lower rates of increase in sexual risk behavior over time, compared to males, (c) youths with higher ADHD scores had a higher rate of linear increase in marijuana use over time; and (d) the quadratic trend for marijuana use over time was less marked for high ADHD youths, than youths with lower baseline ADHD scores. Since our ADHD variable reflects a sense of impulsivity, it is not surprising that youths with higher ADHD scores increase their marijuana use over time. King and associates (King, Fleming, Monahan, & Catalano, 2011) found similar findings when examining the effect of self-control (i.e., impulsivity) on growth models of marijuana use among high school students. Impulsivity led to higher levels of marijuana use, but did not affect the linear growth in marijuana use. Unfortunately, King et al. did not examine a quadratic trend in marijuana use, which may have helped inform the findings of the present study. The negative quadratic trend for marijuana use by ADHD scores could reflect a “balloon effect” for youths with moderate ADHD scores. Future research is needed to clarify the dynamics underlying this relationship.
We found no significant impulsivity effect (measured by our ADHD variable) on sexual risk linear or quadratic trend. While studies have associated impulsivity with sexual risk behaviors, some studies revealed little to no association between impulsivity and sexual risk behaviors. For example, Dévieux et al. (2002) compared sexual risk behaviors across low and high impulsivity groups of adolescent offenders. Similar to our findings, they found more impulsive youth had significantly higher levels of marijuana use but not acts of unprotected sex or the number of sexual partners. When accounting for the interaction of substance use and sexual risk behaviors, however, there were significant differences across the impulsivity groups examined by Dévieux et al. Future research should examine the role of impulsivity on the interaction of marijuana use and sexual risk behaviors longitudinally. Further, Pack, Crosby, and St. Lawrence (2001) have suggested that impulsivity may explain little of the variance in sexual risk behaviors because these behaviors are “often not impulsive, but planned or even habitual” (p. 44). Research on impulsivity and at-risk behaviors may, therefore, benefit from greater consideration of the role of reasoning or rationality in determining action.
As noted earlier, growth mixture model analyses confirmed the existence of sexual risk and marijuana use youth subgroups: (a) a low sexual risk behavior group; a moderate level sexual risk behavior group; and a high level sexual risk behavior group; and (b) a lower level, escalating marijuana use group; a continuing, high level marijuana use group; and a higher rate of escalating marijuana use group. As discussed in the results section, no significant, overall BI intervention effect (Y & YP vs STS) was found for any of the three sexual risk behavior subgroups. There was also no significant intervention effect for the three marijuana use subgroups. The treatment effect for the linear trend for the continuing, high level of marijuana use subgroup was just shy of significance. We plan to reexamine this issue when additional youth and families have been enrolled in the project. An increased sample size will allow for greater power in the analyses, which may or may not lead to significant treatment effects on the sexual risk and marijuana use subgroups of youth.
Research should take into consideration different marijuana use and sexual risk behavior subgroups. Such subgroups may differ significantly in their psychosocial experiences and vulnerabilities, and, most importantly, their response to marijuana use and sexual risk behavior reduction efforts. Youths who are significantly involved in marijuana use are likely to require more intensive and prolonged intervention services, whereas youths less involved in this behavior will likely benefit from brief interventions designed to strengthen their resilience to such involvements. More nuanced approaches to understanding these complex relationships are needed.
Our growth model analyses suggest several implications for research and intervention services. There is a need to complete more longitudinal studies on the relationship between marijuana use and engagement in sexual risk behavior, especially among high-risk youths. It is especially important to pursue such studies among truant youth, on whom few scientifically informed investigations have been completed. As our results highlight, these studies should involve growth model analyses to study these and other risk behaviors in concert, as they are likely to be intertwined. Further, such analyses should allow for the identification of linear and non-linear trends in these relationships.
In regard to interventions for truant, and other at risk, youth, there is a need to develop and test interventions to reduce both marijuana use and sexual risk behavior. Such interventions targeted to different at-risk groups of youths can be especially beneficial in reducing their long-term participation in these behaviors, in addition to their associated, adverse outcomes--such as contracting STDs and HIV/AIDS. Targeting interventions to subgroups of at-risk youths might well be preceded by an inquiry into their identification. We are not aware of interventions targeting both these risk behaviors among truant and other at-risk youth (Hendershot, Magnan, & Bryan, 2010). In this vein, there is a need to allow for the assessment of drug prevention intervention “spillover” effects in reducing sexual risk behavior among youths (Ellickson, McCaffrey, & Klein, 2009).
The findings of this study are consistent with related research suggesting marijuana use is a marker for STD/HIV risk, particularly among high-risk youth (Hendershot, Magnan, & Bryan, 2010). In fact, some studies have suggested that marijuana use is more likely to lead to unprotected sex, than alcohol use (see: Kingree, Braithwaite, & Woodring, 2000).
Among the strengths of this study are its use of a combined measure of marijuana use, incorporating self-report and urine test data, its longitudinal analyses, and its examination of linear and non-linear effects. It would be important for future research to examine the longitudinal relationships between marijuana use and sexual risk behavior among youth, taking into consideration situational circumstances and the nature of sexual partner relationships. It is especially important that intervention programs developed to reduce sexual risk behavior and substance use be informed by empirical research that examines their longitudinal relationships.
There were several limitations to this study. First, there were limitations due to the nature of the sample, which consisted of truant youths picked up by law enforcement or placed in a diversion program. The results of the study may not be generalizable to truant youths who do not have such agency contact or involvement. Second, the sample size was relatively small, precluding an examination of the fit of the models across various sociodemographic groups (e.g., gender). Third, we were not able to assess the influence of such moderating factors as the nature of sexual partner relationship and event factors on our results. Examination of these factors in future longitudinal research is important. Fourth, the global association level of the analyses precludes deeper understanding of the situational, relationship, and event factors contributing to the findings we obtained regarding the marijuana use—sexual risk behavior nexus. Additional longitudinal research is needed on these issues. The present study should be regarded as a beginning effort in illuminating the dynamics of this important public health issue.
Acknowledgments
We are grateful for the collaboration and support of our work by the National Institute on Drug Abuse, the Tampa Police Department, the Hillsborough County Sheriff’s Office, the Hillsborough County Public Schools, the Agency for Community Treatment Services, Inc., and 13th Judicial Circuit, Juvenile Diversion Program. The research reported in this article was funded by NIDA grant# DA021561. We are grateful for NIDA’s support.
Footnotes
The proportion of data present for each model can be obtained from the corresponding author upon request.
Due to space concerns, tables reporting these results has been omitted. Copies are available from the corresponding author upon request.
Contributor Information
Richard Dembo, Criminology Department, University of South Florida
Rhissa Briones-Robinson, Criminology Department, University of South Florida
Kimberly Barrett, Criminology Department, University of South Florida
Rocio Ungaro, Criminology Department, University of South Florida
Ken C. Winters, Department of Psychiatry, University of Minnesota (and also Treatment Research Institute)
Steven Belenko, Department of Criminal Justice, Temple University (and also Treatment Research Institute)
Lora M. Karas, Mediation Program, 13th Judicial Circuit
Laura Gulledge, School of Criminal Justice, University of Southern Mississippi
Jennifer Wareham, Department of Criminal Justice, Wayne State University
References
- Arnette JL. School safety update. Washington, DC: U.S. Department of Justice, Office of Juvenile Programs, Office of Juvenile Justice and Delinquency Prevention; 1995. Place for every youth in America’s schools. [Google Scholar]
- Asparouhov T, Muthèn BO. Technical appendix. Los Angeles: Muthèn & Muthèn; 2010. Bayesian analysis using Mplus: Technical implementation. Retrieved February 26, 2011, from http://www.statmodel.com. [Google Scholar]
- Baker ML, Sigmon JN, Nugent ME. Juvenile justice bulletin. Washington, DC: U.S. Department of Justice, Office of Juvenile Justice Delinquency Prevention; 2001. Truancy reduction: Keeping students in school. [Google Scholar]
- Brodbeck J, Matter M, Moggi F. Association between cannabis use and sexual risk behavior among young heterosexual adults. AIDS Behavior. 2006;10:599–605. doi: 10.1007/s10461-006-9103-9. [DOI] [PubMed] [Google Scholar]
- Brook JS, Balka EB, Abernathy T, Hamburg BA. Sequence of sexual behavior and its relationship to other problem behaviors in African American and Puerto Rican adolescents. The Journal of Genetic Psychology. 1994;155:107–114. doi: 10.1080/00221325.1994.9914763. [DOI] [PubMed] [Google Scholar]
- Bryan AD, Ray LA, Cooper LM. Alcohol use and protective sexual behaviors among high-risk adolescents. Journal of Studies on Alcohol and Drugs. 2007;68(3):327–335. doi: 10.15288/jsad.2007.68.327. [DOI] [PubMed] [Google Scholar]
- Catalano RF, Hawkins JD, Wells EA, Miller J. Evaluation of the effectiveness of adolescent drug abuse treatment, assessment of risks for relapse, and promising approaches for relapse prevention. The International Journal of Addictions. 1991;25:1085–1140. doi: 10.3109/10826089109081039. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS among youth. Centers for Disease Control and Prevention; 2005. Retrieved May 27, 2011, from http://www.cdc.gov/hiv/pubs/facts/youth.pfd. [Google Scholar]
- Center for Disease Control and Prevention. Youth Risk Behavior Survey: United States-2009. Centers for Disease Control and Prevention; 2009. Retrieved May 27, 2011, from http://www.cdc.gov/yrbs. [Google Scholar]
- Center for Labor Market Studies. Left behind in America: The nation’s dropout crisis. Boston: Northeastern University; 2009. [Google Scholar]
- Clark DB, Winters KC. Measuring risks and outcomes in substance use disorders prevention research. Journal of Consulting and Clinical Psychology. 2002;70:1207–1223. doi: 10.1037//0022-006x.70.6.1207. [DOI] [PubMed] [Google Scholar]
- Cooper LM. Alcohol use and risky sexual behavior among college students and youth: Evaluating the evidence. Journal of Studies on Alcohol. 2002;14:101–117. doi: 10.15288/jsas.2002.s14.101. [DOI] [PubMed] [Google Scholar]
- DeGenna NM, Cornelius MD, Cook RL. Marijuana use and sexually transmitted infections in young women who were teenage mothers. Women’s Health Issues. 2007;5:300–309. doi: 10.1016/j.whi.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dembo R, Belenko S, Childs K, Wareham J, Schmeidler J. Drug use and sexually transmitted diseases among female and male arrested youths. Journal of Behavioral Medicine. 2009;32(2):129–141. doi: 10.1007/s10865-008-9183-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dembo R, Briones R, Ungaro R, Gulledge L, Karas L, Winters KC, Belenko S, Greenbaum PE. Emotional/Psychlogical and Related Problems Among Truant Youths: An exploratory latent class analysis. Journal of Emotional and Behavioral Disorders. doi: 10.1177/1063426610396221. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dembo R, Briones-Robinson R, Gulledge LM, Karas L, Winters KC, Belenko S, Greenbaum PE. Stress, mental health and substance abuse problems in a sample of diversion program youth: An exploratory latent class analysis. Journal of Child & Adolescent Substance Abuse. doi: 10.1080/1067828X.2012.662115. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dembo R, Shemwell M, Guida J, Schmeidler J, Baumgartner W, Ramirez Garnica G, Seeberger W. Comparison of self-report, urine sample and hair testing for drug use: A longitudal study. In: Mieczkowski T, editor. Drug testing methods: Assessment and evaluation. New York: CRC Press; 1999. [Google Scholar]
- Dembo R, Turner G. A pilot study of truants processed at the Hillsborough County Juvenile Assessment Center. The Journal of At-Risk Issues. 1994;1:38–42. [Google Scholar]
- Dévieux J, Malow R, Stein JA, Jennings TE, Lucenko BA, Averhart C, Kalichman S. Impulsivity and HIV risk among adjudicated alcohol- and other drug-abusing adolescent offenders. AIDS Education and Prevention. 2002;14(Supplement B):24–35. doi: 10.1521/aeap.14.7.24.23864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diebolt A, Herlache L. The school psychologist as a consultant in truancy prevention. Paper presented at the annual meeting of the National Association of School Psychologists; Dallas, Texas. 1991. [Google Scholar]
- Duncan TE, Duncan SE, Stryker LA, Li F, Alpert A. An introduction to latent variable growth curve modeling: Concepts, issues, and applications. Mahwah, NJ: Lawrence Erlbaum; 1999. [Google Scholar]
- Eaton DK, Brener N, Kann L. Associations of health risk behaviors with school absenteeism. Does having permission for the absence make a difference? Journal of School Health. 2008;78(4):223–229. doi: 10.1111/j.1746-1561.2008.00290.x. [DOI] [PubMed] [Google Scholar]
- Egger HL, Costello EJ, Angold A. School refusal and psychiatric disorders: A community study. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;7:797–807. doi: 10.1097/01.CHI.0000046865.56865.79. [DOI] [PubMed] [Google Scholar]
- Elkington KS, Bauermeister JA, Brackis-Cott E, Dolezal C, Mellins CA. Substance use and sexual risk behaviors in perinatally human immunodeficiency virus-exposed youth: Roles of caregivers, peers and HIV status. Journal of Adolescent Health. 2009;45(2):133–141. doi: 10.1016/j.jadohealth.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellickson PL, McCaffrey DF, Klein DJ. Long-term effects of drug prevention on risky sexual behavior among young adults. Journal of Adolescent Health. 2009;45(2):111–117. doi: 10.1016/j.jadohealth.2008.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garry EM. Juvenile justice bulletin. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Office of Juvenile Justice and Delinquency Prevention; 1996. Truancy: First step to a lifetime of problems. [Google Scholar]
- Gelman A, Carlin JB, Stern HS, Rubin DB. Bayesian data analysis. 2. Boca Raton, FL: Chapman & Hall; 2004. [Google Scholar]
- Gelman A, Meng XL, Stern HS, Rubin DB. Posterior predictive assessment of model fitness via realized discrepancies (with discussion) Statistical Sinica. 1996;6:733–807. [Google Scholar]
- Gelman A, Rubin DB. Inference from iterative simulation using multiple sequences. Statistical Science. 1992;7:457–511. [Google Scholar]
- Goldstein AL, Barnett NP, Pedlow CT, Murphy JG. Drinking in conjunction with sexual experiences among at-risk college student drinkers. Journal of Studies on Alcohol and Drugs. 2007;68(5):697–705. doi: 10.15288/jsad.2007.68.697. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Herrenkohl TI, Farrington DP, Brewer E, Catalano RF, Harachi TW, Cothern L. Juvenile justice bulletin. Washington, DC: U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention; 2000. Predictors of youth violence. [Google Scholar]
- Hendershot CS, Magnan RE, Bryan AD. Associations of marijuana use and sex-related marijuana expectancies with HIV/STD risk behavior in high-risk adolescents. Psychology of Addictive Behaviors. 2010;24:404–414. doi: 10.1037/a0019844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry KL, Thornberry TP, Huizinga DH. A discrete-time survival analysis of the relationship between truancy and the onset of marijuana use. Journal of Studies on Alcohol and Drugs. 2009;70:5–15. doi: 10.15288/jsad.2009.70.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll S, LeBoeuf D. Reaching out to youth out of the education mainstream. Washington, DC: U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention; 1997. [Google Scholar]
- Jessor R, Jessor SL. Problem behavior and psychosocial development: A longitudinal study of youth. New York: Academic Press; 1977. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Marijuana use is rising; ecstasy use is beginning to rise; and alcohol use is declining among US teens. University of Michigan New Service; Ann Arbor, MI: Dec 14, 2010. Retrieved February 26, 2011, from http://www.monitoringthefuture.org. [Google Scholar]
- Kearney CA, Silverman WK. Family environment of youngsters with school refusal behavior: A synopsis with implications for assessment and treatment. American Journal of Family Therapy. 1995;23(1):59–72. [Google Scholar]
- King KM, Fleming CB, Monahan KC, Catalano RF. Changes in self-control problems and attention problems during middle school predict alcohol, tobacco, and marijuana use during high school. Psychology of Addictive Behaviors. 2011;25:69–79. doi: 10.1037/a0021958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingree JB, Betz H. Risky sexual behavior in relation to marijuana and alcohol use among African-American, male adolescent detainees and their female partners. Drug and Alcohol Dependence. 2003;72:197–203. doi: 10.1016/s0376-8716(03)00196-0. [DOI] [PubMed] [Google Scholar]
- Kingree JB, Braithwaite R, Woodring T. Unprotected sex as a function of alcohol and marijuana use among adolescent detainees. Journal of Adolescent Health. 2000;27:179–185. doi: 10.1016/s1054-139x(00)00101-4. [DOI] [PubMed] [Google Scholar]
- Kingree JB, Phan D. Marijuana use and unprotected sexual intercourse among adolescent detainees: An event analysis. Criminal Justice and Behavior. 2002;29:705–717. [Google Scholar]
- Komro KA, Tobler AL, Maldonado-Molina MM, Perry CL. Effects of alcohol use initiation patterns on high-risk behaviors among urban, low-income, young adolescents. Prevention Science. 2010;11(1):14–23. doi: 10.1007/s11121-009-0144-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R, Farrington DP. Young children who commit crime: Epidemiology, developmental origins, risk factors, early interventions, and policy implications. Development and Psychopathology. 2000;12(4):737–762. doi: 10.1017/s0954579400004107. [DOI] [PubMed] [Google Scholar]
- Lynch S. Introduction to applied Bayesian statistics and estimation for social scientists. New York, NY: Springer; 2010. [Google Scholar]
- Morris RE, Baker CJ, Valentine M, Pennisi AJ. Variations in HIV risk behaviors of incarcerated juveniles during a four-year period: 1989–1992. Journal of Adolescent Health. 1998;23:39–48. doi: 10.1016/s1054-139x(97)00268-1. [DOI] [PubMed] [Google Scholar]
- Morris RE, Harrison EA, Knox GW, Tromanhauser E, Marquis DK. Health risk behavioral survey from 39 juvenile correctional facilities in the United States. Journal of Adolescent Health. 1995;17:334–344. doi: 10.1016/1054-139X(95)00098-D. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Brecht M, Herbeck D, Huang D. Trajectories of HIV risk behavior from age 15 to 25 in the national longitudinal survey of youth sample. Journal of Youth and Adolescence. 2009;38(9):1226–1239. doi: 10.1007/s10964-008-9323-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, Asparouhov T. Bayesian SEM: A more flexible representation of substantive theory. 2010 doi: 10.1037/a0026802. Submitted for publication. Retrieved May 27, 2011, from http://www.statmodel.com. [DOI] [PubMed]
- Muthèn LK, Muthèn BO. Mplus user’s guide version 6. Los Angeles, CA: Muthèn & Muthèn; 1998–2010. [Google Scholar]
- Office of National Drug Control Policy. 2010 Monitoring the Future Study: Highlights. University of Michigan; Dec, 2010. Retrieved Februrary 26, 2011, from http://www.whitehousedrugpolicy.gov. [Google Scholar]
- Pack RP, Crosby RA, St Lawrence JS. Associations between adolescents’ sexual risk behavior and scores on six psychometric scales: Impulsivity predicts risk. Journal of HIV/AIDS Prevention & Education for Adolescents & Children. 2001;4(1):33–47. [Google Scholar]
- Pritchard C, Cotton A, Cox M. Truancy and illegal drug use, and knowledge of HIV infection in 932 14–16-year-old adolescents. Journal of Adolescence. 1992;15(1):1–17. doi: 10.1016/0140-1971(92)90061-9. [DOI] [PubMed] [Google Scholar]
- Puzzanchera C, Stahl AL, Finnegan TA, Tierney N, Snyder HN. Juvenile court statistics 1998. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Office of Juvenile Justice Delinquency Prevention; 2003. [Google Scholar]
- Rupp AA, Dey DK, Zumbo BD. To Bayes or not to Bayes, from whether to when: Applications of Bayesian methodology to modeling. Structural Equation Modeling. 2004;11:424–451. [Google Scholar]
- Scheines R, Hoijtink H, Boomsma A. Bayesian estimation and testing of structural equation models. Psychometrika. 1999;64:37–52. [Google Scholar]
- Schmeige S, Levin M, Broaddus M, Bryan A. Randomized trial of group interventions to reduce HIV/STD risk and change theoretical mediators among detained adolescents. Journal of Consulting and Clinical Psychology. 2009;77:38–50. doi: 10.1037/a0014513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrier LA, Harris SK, Sternberg M, Beardslee WR. Association of depression, self-esteem, and substance use with sexual risk among adolescents. Preventive Medicine. 2001;33:179–189. doi: 10.1006/pmed.2001.0869. [DOI] [PubMed] [Google Scholar]
- Smith AMA, Ferris JA, Simpson JM, Shelley J, Pitts M, Richters J. Cannabis use and sexual health. Journal of Sexual Health. 2010;7:787–793. doi: 10.1111/j.1743-6109.2009.01453.x. [DOI] [PubMed] [Google Scholar]
- Teplin LA, Mericle AA, McClelland GM, Abram KM. HIV and AIDS risk behaviors in juvenile detainees: Implications for public health policy. American Journal of Public Health. 2003;93:906–912. doi: 10.2105/ajph.93.6.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherill RR, Fromme K. Alcohol use, sexual activity, and perceived risk in high school athletes and non-athletes. Journal of Adolescent Health. 2007;41(3):294–301. doi: 10.1016/j.jadohealth.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whaley AL. Preventing the high-risk sexual behavior of adolescents: Focus on HIV/AIDS transmission, unintended pregnancy, or both? Journal of Adolescent Health. 1999;24:376–382. doi: 10.1016/s1054-139x(98)00153-0. [DOI] [PubMed] [Google Scholar]
- Winters KC. Development of an adolescent alcohol and other drug abuse screening scale: Personal Experience Screening Questionnaire. Addictive Behaviors. 1992;17:479–490. doi: 10.1016/0306-4603(92)90008-j. [DOI] [PubMed] [Google Scholar]
- Winters KC, Botzet AM, Fahnhorst T, Baumel L, Lee S. Impulsivity and its relationship to risky sexual behaviors and drug abuse. Journal of Child & Adolescent Substance Abuse. 2009;18:43–56. doi: 10.1080/15470650802541095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters KC, Henly GA. Adolescent Diagnostic Interview Schedule and Manual. Los Angeles: Western Psychological Services; 1993. [Google Scholar]
- Winters KC, Leitten W. Brief intervention for drug-abusing adolescents in a school setting. Psychology of Addictive Behaviors. 2007;21:249–254. doi: 10.1037/0893-164X.21.2.249. [DOI] [PubMed] [Google Scholar]
- Winters KC, Stinchfield RD. Adolescent Diagnostic Interview-Parent. Minneapolis: University of Minnesota; 2003. [Google Scholar]
- Yan AF, Chui YW, Stesen CA, Wang MQ. STD-/HIV-related sexual risk behaviors and substance use among US rural adolescents. Journal of the National Medical Association. 2007;99:1386–1394. [PMC free article] [PubMed] [Google Scholar]
- Young P, Rahdert E. Development of a POSIT-related HIV/STD risk scale. Bethesda, MA: NOVA Research Company; 2000. [Google Scholar]