Abstract
Background
Psoriasis has a serious impact on patients’ lives. However, adherence to medications is often poor, potentially compounding the burden of disease. Identifying patients who need support with psychosocial problems, or issues with adherence, can be complex.
Objectives
We aimed to develop statements that could assist the consultation process, identifying the relative importance of factors related to effective management of psoriasis for patients.
Methods
A two-stage study design was used to comprehensively identify, and assess validity of, statements describing psoriasis impact and management issues. Both components were conducted in Canada, France, Germany, Italy, Spain, the United Kingdom and the United States. Findings from patient observation and interviews were analysed for pattern strength, and were then used to inform the development of statements that were quantitatively assessed using a survey. The association of drivers towards agreement with ‘my psoriasis dictates how I lead my life’ was assessed using anova.
Results
Fifty-six patients participated in the qualitative component, and 1,884 patients using prescription medications completed the survey. Two thematic categories were identified; disappointment with treatments, and confusion regarding psoriasis associated with a lack of direction. When assessed quantitatively, key statements associated with a strong burden of psoriasis on patients’ lives were related to isolation, social stigma, visible symptoms, impact on activities and feelings of hopelessness. A mixture of patient-, doctor- and treatment-related factors were among the most common reasons for non-adherence.
Conclusion
Questioning using the statements most associated with psychosocial impact and non-adherence could help identify patients with additional support needs, and assist in overcoming adherence issues.
Introduction
Psoriasis can have a significant impact on patients’ health-related quality of life (HRQoL), and is often linked to depressive symptoms.1–3 Poor self-esteem, sexual dysfunction, anxiety and suicidal ideation have all been reported in patients with psoriasis.1–4 Moreover, it is now recognized that the psychosocial impact of the disease, including feelings of stigmatization and depression, can have an even greater impact than physical symptoms.1,2,5,6
Depressive symptoms associated with psoriasis have in turn been associated with behaviour patterns that could further impact health,1,2 including smoking, drinking and decreased physical activity or obesity.7,8 However, identifying which patients are in need of additional support to overcome or avoid such serious comorbidities can be challenging, since symptom severity is not an accurate predictor of psychological distress.9,10 Indeed, lesion severity accounts for less than half the impact of psoriasis on patients’ HRQoL.5
It has previously been suggested that identifying and focusing on issues that are most important to patients might also have a positive impact on adherence to therapy.11 Indeed, non-adherence has been shown to occur when the patient’s preferences, expectations and beliefs have not been considered sufficiently in the prescribing process.12 Patients with psoriasis often struggle to adhere to therapeutic regimens, including topical medications,13 with up to 40% not using their medication as recommended.14 Deliberate non-adherence, due to misconceptions about treatment efficacy and safety, and non-intentional non-adherence, arising from difficulties with application and complexities of the treatment regimen, can contribute to poor outcomes.13,15–17
To help patients overcome the impact of psoriasis on their lives, both psychosocial and adherence issues need to be addressed. In this two-component, mixed-method qualitative and quantitative study, we aimed to develop and assess key questions that could help to identify patients who are in need of additional support for psychological or adherence issues.
Methods
A two-stage study design was used to (i) comprehensively identify issues faced by patients, as well as their current practices and beliefs, relating to their psoriasis (qualitative component) and then (ii) determine the applicability of the issues identified by this necessarily small group to a much wider patient population (quantitative component). This design was used to minimize the influence of any preconceptions held by the investigators about the issues that patients might face. It allowed patients themselves to discuss and show their real-life situation, before quantitative assessment of the issues.
The qualitative component of the study was ethnographic in methodology. It was conducted in June 2010 among patients with psoriasis from Canada, France, Germany, Italy, Spain, the United Kingdom and the United States. Patients were recruited from pre-existing databases, which were set up using convenience and snowball sampling, to represent a range of demographics and psoriasis severities. They were visited by an ethnographer, who accompanied them as they went about their day, participating in their normal activities and documenting their behaviours using video and photographs over an initial 4–8 h-period. Within this participant observation period, a 2-h semi-structured interview was conducted, exploring the patient’s psoriasis, values and needs. A quarter of the patients, who were willing to participate further in the study, were then visited a second time. This enabled an even more candid session due to the pre-established rapport between patient and interviewer. Using well-established qualitative research methods,18 observations were recorded into a photo field note template, while coding and the objective analysis of pattern strength were performed using ATLAS.ti 7 software (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany). The themes and language identified in the qualitative component were then used to inform the development of the quantitative survey.
For the quantitative component, adults from the same countries that were included in the qualitative component had been recruited to join a database using a mix of telephone and online methods, including banner adverts and direct email. Those who indicated their willingness to participate and confirmed in initial screening questions that they suffered from psoriasis and/or psoriatic arthritis were subsequently invited to complete an online survey during December 2010–January 2011. This method of recruitment was used to ensure that those entering the survey were not biased by knowing the subject matter beforehand. The 68-part survey included questions on demographics, comorbidities, general self-perception, symptoms, diagnosis of severity (using broader categories than in the qualitative component, to be more reflective of a doctor’s diagnosis), relationships with health care professionals (HCPs), attitudes to treatments (including reasons for non-adherence), attitudes to psoriasis and information seeking.
The quantitative analyses were restricted to patients who reported current prescription medication use. To assess the factors that contribute to a high impact on the patients’ lives, the contribution of drivers towards agreement with the statement ‘my psoriasis dictates how I lead my life’ was assessed using anova with the F-test to compare components of the total deviation (SPSS; SPSS Inc., Chicago, IL, USA). Drivers assessed included those describing components of symptom burden, HCP relationships, patient factors and the psychosocial impact of psoriasis.
Reasons for non-adherence to prescription medications were assessed by a direct question: ‘are you taking [patient’s medicine] according to your doctor’s exact instructions (for example, taking the medication at the right time, the right number of times, the right amount)?’ Patients who indicated that they were not adherent all of the time were asked whether any of 24 pre-defined statements applied to them, in response to the question ‘why are you not taking your [patient’s medicine] according to your doctor’s instructions’. Statements related to the treatment, the doctor or the patient. The reasons for non-adherence were ranked for topical prescription medications in this analysis because the high number of patients using this treatment-type gave a sufficient sample size.
Results
Qualitative component
A total of 26 men and 30 women participated in the qualitative component, with a mean age of 42 years (range, 20–67 years). Of these 56 patients, 71% saw a dermatologist most often, 13% a general practitioner (GP), 4% a combination of different medical professionals, 2% a rheumatologist and 11% were not regularly seeing any doctor at that time. Prescription topical medications were being used alone by 34% of patients. Prescription topicals were used in combination with oral-, photo- or injected- therapies or combinations of these by 4%, 9%, 7% and 4% of patients respectively. Non-topical prescription medications were used without a prescribed topical by 9% of patients (5% oral-, 2% photo- and 2% injected- therapies), and 34% used no prescription medication. Only one patient (2%) did not use a prescription or over-the-counter treatment. The mean duration of psoriasis was 16 years (range, <1–53 years). Patients reported that their psoriasis symptoms were mild (25%), mild-moderate (18%), moderate (29%), moderate-severe (5%) or severe (23%).
Two thematic categories were generated from the raw data (Table 1); disappointment with treatments, and confusion regarding psoriasis, associated with a lack of direction.
Table 1.
Key categories and property codes relevant to psoriasis management
| Thematic category | Property code (characteristics) |
|---|---|
| Disappointment with treatments | Treatments are not seen as effective |
| Perceived burden of treatment is amplified | |
| Vicious circle of low satisfaction and adherence | |
| Loss of trust in prescription medications leads to cosmetic and OTC alternatives | |
| Confusion regarding psoriasis, associated with a lack of direction | Tangible and emotional psoriasis costs are substantial |
| Psoriasis is hidden and has no clear identity | |
| Patients bear the burden of psoriasis alone | |
| Patients experience a lack of direction and authority |
OTC, over-the-counter.
Confusion and lack of direction regarding psoriasis
Patients reported a high impact of psoriasis on their lives, independent of their diagnosed symptom severity. Physical symptoms, including pain, itching and bleeding, drove some patients to desperation and impaired physical activities, while social reactions (real or perceived) were also traumatic. The psychological impact of psoriasis was characterized by constant worry, a struggle for control and a fear of stress triggering symptoms. Patients reported that a combination of these factors led to avoidance, limitation, hiding and isolation.
It was felt among the patients that other people do not understand their disease, and could think them unhygienic. In accordance with this, they considered psoriasis to be a ‘dirty’ and an uninteresting topic for discussion, with some not talking to friends or family about the burden of the disease. Patients felt that doctors are unable to provide a clear diagnosis and that prescriptions are automated or random. They also felt that doctors do not understand the seriousness of psoriasis, particularly the non-physical aspects.
Disappointment with treatments
Patients felt that topical medications were not helping their psoriasis to a great extent. One reason was that they had been through a long and burdensome process with trial-and-error, and had developed negative attitudes towards topical medications by the time they received more potent options. This led to a loss of faith in medical topical treatments, and doctors. Patients also expressed unrealistic expectations of their treatments, and stated that their doctor had not communicated what to expect.
Poor opinions of treatments were compounded by the time taken to apply them, fear of side effects and undesirable features of treatments making patients feel unclean. These features included touch (oiliness and stickiness), smell and visibility. However, patients were more likely to accept inconvenience when they perceived that treatments were effective. Overall, the high perceived burden of treatments led to sporadic use of prescription topical medications.
Statements derived from these findings that are most relevant to the current analysis are shown in Tables 2–4.
Table 2.
Patient agreement with attitudinal statements regarding their psoriasis*
| Statement | Patients using prescription medications (n = 1,884), agreement (%) |
|---|---|
| I would do anything to improve my psoriasis | 82 |
| I’m worried that when I stress out too much about my psoriasis, it further provokes my psoriasis symptoms | 72 |
| I try to hide my psoriasis from others | 66 |
| My psoriasis makes me often wonder - why me? | 51 |
| I’m very worried that other people think I’m dirty or unclean when they see my psoriasis | 51 |
| People think my psoriasis is contagious | 49 |
| There isn’t really anything that I can do about my psoriasis | 48 |
| I worry constantly about my psoriasis | 44 |
| No one can understand what I’m going through | 43 |
| I often feel dirty or unclean due to my psoriasis | 40 |
| Without my psoriasis, I’d be able to enjoy a lot of activities that I cannot enjoy now | 38 |
| My psoriasis interferes with my work life and productivity† | 34 |
| I don’t have a lot of support from family or friends in dealing with my psoriasis‡ | 34 |
| I cannot be intimate/have sex as often as I would like because of my psoriasis | 31 |
| My psoriasis dictates how I lead my life | 27 |
| My relationships with family, friends have been negatively affected by my psoriasis | 21 |
| People avoid me because of my psoriasis | 17 |
subset of full survey shown;
question was posed negatively; numbers have been adapted accordingly.
question was posed positively; numbers have been adapted accordingly.
Table 4.
Patient agreement with attitudinal statements regarding their relationships with health care providers*
| Statement | Patients using prescription medications and currently seeing a physician (n = 1,813), agreement (%) | Subset who see a GP most often (n = 739), agreement (%) | Subset who see a dermatologist most often (n = 939), agreement (%) | Subset who see another physician† most often (n = 135), agreement (%) |
|---|---|---|---|---|
| My doctor gives me clear instructions on how to use my psoriasis treatment | 81 | 77 | 83 | 87 |
| I am comfortable asking my doctor about new psoriasis treatment options that I have heard about | 81 | 80 | 82 | 81 |
| My doctor takes his/her time listening to me about my psoriasis | 78 | 73 | 81 | 84 |
| I trust my doctor completely when it comes to my psoriasis | 77 | 71 | 80 | 80 |
| If I disagree with my doctor’s recommendations, I am comfortable speaking to him/her about it | 74 | 74 | 74 | 78 |
| My doctor has helped me a lot with my psoriasis | 73 | 69 | 76 | 77 |
| My doctor considers which treatment would best fit my lifestyle and wishes | 74 | 70 | 76 | 78 |
| Nurses have a good understanding of psoriasis treatments | 54 | 53 | 54 | 53 |
| My doctor keeps me informed about the latest treatment options for my psoriasis | 53 | 40 | 60 | 67 |
| Nobody seems able to help me regarding my psoriasis | 35 | 38 | 35 | 23 |
| My doctor does not tell me what I am supposed to expect from my treatment | 35 | 40 | 33 | 26 |
| My doctor does not know which treatments work and which ones do not work | 33 | 38 | 32 | 22 |
| I don’t think that my doctor takes my psoriasis very seriously | 30 | 35 | 27 | 22 |
subset of full survey shown;
including ‘psychologist/psychiatrist’, ‘rheumatologist’, ‘alternative therapists’ or ‘other’.
Quantitative component
Nearly two thousand (1,884) patients who stated that they were currently taking prescription medications for their psoriasis completed the quantitative survey. The mean age of these patients was 43 years (range, 18–83 years), with 45% men and 55% women. Approximately a quarter reported stress (29%), anxiety (27%) or depression (21%) as comorbid conditions. Patients reported that their symptoms normally affected their body in 77% of cases, with the scalp/ears/neck, palms/soles, flexures, or nails normally affected in 73%, 37%, 32% and 20% of cases respectively.
Most patients stated that they saw a dermatologist (52%) or GP (41%) most often (based on 1,813 patients who answered this question). Most (58%) also reported that they had plaque psoriasis, with 33% uncertain of their subtype and 13% reporting other types. Patients reported that their doctor’s assessment of their psoriasis was mild (31%), moderate (53%) or severe (12%), with 5% of patients unsure. The mean number of flares per year was nine, and mean duration of psoriasis was 15 years (range, <1–68 years). Nearly all (92%) were using topical prescription medications, with 23%, 10% and 7% using oral-, photo- or injected- therapies respectively. Topical prescription medications were used in combination with other prescription therapies by 25% of patients.
Itching was the most commonly reported physical symptom, affecting 87% of patients. Half (54%) of the patients reporting itch experienced problems sleeping due to itching. Most patients (60%) responded 6–10 to ‘how much impact do you think psoriasis has on your life’ (using a discrete visual analogue scale: 1, no impact at all; 10, extremely high impact), while 40% of patients responded 1–5. Few patients (3%) felt that their psoriasis had ‘no impact at all’ (responding ‘1’), while 7% reported an ‘extremely high impact’ (responding ‘10’).
Issues raised in the qualitative component regarding worry, hiding and concern about hygiene perceptions affected more than half of patients (Table 2). Feelings of isolation, and impact on activities and personal relationships were less common, but still affected many patients (Table 2). A quarter (27%) of patients agreed with ‘my psoriasis dictates how I lead my life’. Statements derived from the qualitative research that were most strongly associated with this agreement are shown in Fig. 1. Key statements related to isolation, social stigma, visible symptoms, impact on activities and feelings of hopelessness. In accordance with themes raised in the qualitative component, symptom severity was not significantly associated with agreement.
Figure 1.
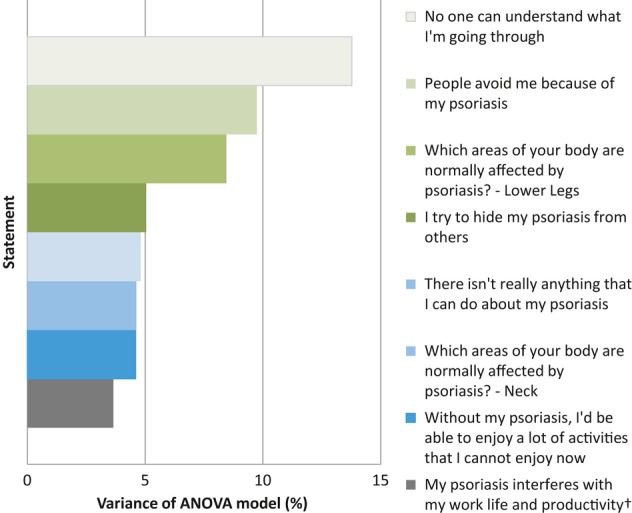
Factors most strongly associated with ‘my psoriasis dictates how I lead my life’*. *all P < 0.03; Adjusted R-squared 0.61; †question was posed negatively, which gave a negative coefficient.
While 85% of patients expressed willingness to stay on medications for extended periods of time, many expressed unrealistic expectations regarding medications (Table 3). In contrast with feelings expressed during the qualitative component, the majority of patients (81%) reported that they receive clear instructions from with their doctor; however, approximately a third felt that their doctor does not take their psoriasis seriously (Table 4). The patterns observed in attitudes to health care provider relationships were similar for patients seeing a GP or dermatologist most often, although scores were slightly better for patients seeing a dermatologist most often (Table 4).
Table 3.
Patient agreement with attitudinal statements regarding their treatments*
| Statement | Patients using prescription medications (n = 1,884), agreement (%) |
|---|---|
| I’m willing to keep switching treatments or medications until I find the one that works best for my psoriasis | 85 |
| I am willing to stay on prescription medication for extended periods of time for my psoriasis | 85 |
| I don’t mind taking a psoriasis medication every day as long as it works | 83 |
| I expect treatments to work quickly | 79 |
| I want to control how and when my medications are taken for my psoriasis | 78 |
| I am eager to try new treatments or medications for my psoriasis | 78 |
| I always treat my psoriasis, whether it’s with prescription medication or just something I buy over-the-counter | 77 |
| I expect a cure when I try a new psoriasis treatment | 69 |
| I only take my treatment if I experience a flare-up | 56 |
| I am fearful of the side effects associated with prescription medications for my psoriasis | 55 |
| All creams work the same, it does not matter if it is prescribed by the doctor or not | 26 |
subset of full survey shown.
Non-adherence to prescription medications (at least some of the time) was reported by 46% of patients using topicals, and 25%, 35% and 18%, of patients using oral-, photo- or injected- therapies respectively. The statements most often chosen as reasons for non-adherence to topical prescription medications are shown in Fig. 2. A mixture of patient-, doctor- and treatment-related factors were confirmed as affecting more than 10% of non-adherent patients in the quantitative sample, with 47% of patients reporting that they only use their medication when they feel it is needed.
Figure 2.
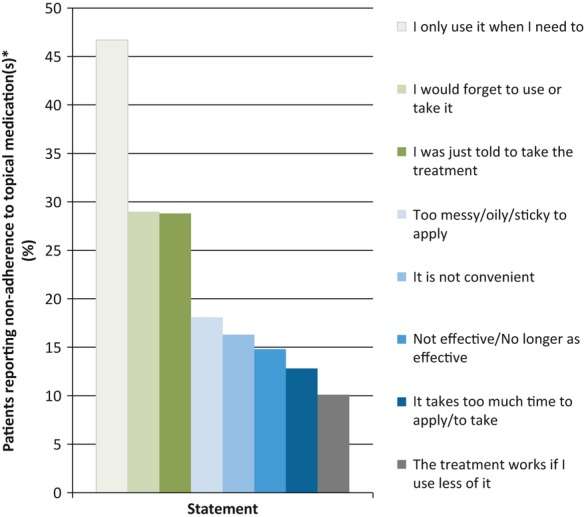
Reasons for non-adherence given by patients using topical prescription medication(s). *n = 799. Statements agreed with by >10% patients reporting non-adherence are shown.
Discussion
This large, multinational study has identified for the first time the relative importance of factors related to effective management in psoriasis using a patient-centric development process. Traditional survey methods provide useful data, but use questions based on assumptions about the patient experience. Elucidating the pattern of patient experience first minimizes the risk of missing key issues that are important to patients, and enhances the validity of the questions being posed. The wider applicability of specific questions related to this experience can then be tested quantitatively.
The importance of psychosocial and subjective factors to patients is well established in psoriasis.19–21 However, in a limited consultation period, it has been unclear which questions to focus on to identify areas most likely to contribute to significant impact on a patient’s life. Our research indicates that there is a subset of patients who are in particular need of additional support to overcome this impact. These patients could be identified by considering the key questions with the highest influence on the feeling that psoriasis dictates daily life: whether their psoriasis is ‘usually’ visible, whether they feel others understand the effect psoriasis has had on them, whether they feel others avoid them, whether they take any measures to hide their psoriasis, whether they feel helpless with regards to their disease and whether they feel unable to participate in activities. However, it should be noted that this list is not exhaustive, since the model accounted for 60% of the effect. Questioning whether these statements apply to a patient could help to identify a significant burden of psoriasis, but could also help to highlight specific issues regarding the patient’s individual problems, beliefs and symptoms, which could be addressed with targeted interventions.
Discrepancies between doctor and patient expectations of treatments, and factors that each group consider to be important measures of ‘effectiveness’, have been documented by previous studies that either use a survey approach or in-depth interviews.11,22 In terms of treatment, a previous in-depth qualitative investigation in the United Kingdom identified that in addition to factors relating to efficacy, desirability (smell, consistency, staining), the time required for application, awareness of treatment risks and patients choosing to use treatments differently than recommended were considered components of ‘effectiveness’ from a patient’s perspective.11 The current data show that these factors also contributed to the likelihood that patients adhered to topical medications. Interestingly, half of the non-adherent population stated that they are making a personal choice about how to use their medicine and nearly a third felt that they were not given sufficient explanation regarding how to take their medicine. A recent qualitative study on self-management experiences in psoriasis also identified that a lack of understanding of how treatments work contributed to decisions not to adhere to treatment regimens.23 This is reinforced by the large proportion of patients in the current population unrealistically expecting a cure and rapid results from their treatment. These findings highlight the importance of education for patients about treatments and how to self-manage their condition effectively, which patients also desire and expect.23
A positive, empathetic relationship between patients and doctors is vital in psoriasis.24 While our survey results suggest that the majority of patients experienced this – expressing comfort and the feeling that sufficient time is taken to discuss their issues – the contrasting high levels of unrealistic expectations suggest that the right information might not be reaching patients. It could also mean that information might be given in a sub-optimal format. While our analysis has focussed on patient-doctor relationships, nurses are playing an increasingly important role in psoriasis care in many countries. A recent pilot of a nurse-led educational programme used a combination of group learning, action planning, take-away materials and follow-up telephone support.25 Each component was found to be moderately to very useful by participants.25 The optimal design of such support programmes, to give the highest HRQoL benefit, will become clearer as more and larger studies become available.
Once a baseline level of education has been established, a positive, constructive concordance process that takes account of the way that a patient actually uses their medicine has been recommended. In the 2005 UK National Co-ordinating Centre for NHS Service Delivery and Organisation R&D (NCCSDO) report, Horne et al. postulated that prescribing is a ‘therapeutic experiment’, and the role of the prescriber is to help the patient make an informed choice – placing responsibility on both parties for designing an appropriate regimen and supporting ‘informed adherence’ to that regimen.26 This ‘appropriate’ regimen does not necessarily mean using medicines exactly as set out in prescribing information. However, it is important that patients understand how their medicines work so they are informed enough to know what using a medicine when they ‘need to’ really means.
Forgetfulness was also a key factor in non-adherence, and patients can be supported to overcome this problem using validated techniques such as text-messaging.27 However, it should be noted that this type of ‘non-intentional’ non-adherence has been shown to be predictable to some extent by beliefs about treatment,28 further highlighting the need for a non-judgemental consultation approach to elucidate the real factors driving non-adherence for each patient. Observations have been made in smaller qualitative11 and survey-based studies29 that ‘desirability’ features of medicine and inconvenience are important to patients. Our data confirm that these were contributors to non-adherence for a significant proportion of patients, and should therefore be discussed as part of the collaborative management process.
A limitation of our study is the use of a non-population-based quantitative sample. However, demographic features including age30–33 and gender,3,30–32 together with comorbidities such as depression34 are similar to those seen in previous data sets. The population-based EUROPSO study found features including age of psoriasis onset (30.5 years) that are largely in accordance with our data. There were also similarities seen in prevalence of itch (72%) and difficulties relating to sexual activities (27%).3 It should also be noted that while 58% of patients reported plaque psoriasis in this study, a proportion of the 33% who did not know their subtype were also likely to fit into this category.
The design of this study differs from traditional HRQoL assessment, since it includes a qualitative research phase to develop questions based on themes raised by patients. Qualitative research is increasingly recognized as a key first step to unravelling complex issues caused by diseases such as psoriasis,35 but has been used to a limited extent in this field and patient group to date. The quantitative phase of this study was used to validate the relevance of key statements in a larger population. However, the effectiveness of employing questions developed from this study should be assessed by further research. Potentially, the questions relating to impact on life could be employed at a first consultation, and also during follow-up to help inform and refine management discussions with the patient. Tools that suggest specific support-types available in a particular country could be a useful adjunct. The questions relating to adherence could be used at a first follow-up after a new topical treatment is prescribed, then at intervals for as long as the treatment continues to be prescribed.
In conclusion, specific questions relating to isolation, social stigma, impact of psoriasis on activities and feelings of hopelessness should be included in consultations. Patients should also be helped to develop realistic expectations of newly prescribed treatments, followed by constructive discussion of the reasons for non-adherence over time. This approach has the potential to maximize the chances of optimal adherence. It could also help to identify patients who might benefit from approaches to optimize treatment effectiveness, through adherence enhancement and related support of patient self-management and coping.
Acknowledgments
This article was developed using data collected on behalf of and funded by LEO Pharma. The company also funded the statistical analysis. Scientific and editorial control resides with the authors. Data collection and analysis was performed with the assistance of Kantar Health, Penn Schoen Berland and ReD Associates.
References
- Stern RS, Nijsten T, Feldman SR, et al. Psoriasis is common, carries a substantial burden even when not extensive, and is associated with widespread treatment dissatisfaction. J Investig Dermatol Symp Proc. 2004;9:136–139. doi: 10.1046/j.1087-0024.2003.09102.x. [DOI] [PubMed] [Google Scholar]
- Schmitt J, Ford DE. Psoriasis is independently associated with psychiatric morbidity and adverse cardiovascular risk factors, but not with cardiovascular events in a population-based sample. J Eur Acad Dermatol Venereol. 2010;24:885–892. doi: 10.1111/j.1468-3083.2009.03537.x. [DOI] [PubMed] [Google Scholar]
- Dubertret L, Mrowietz U, Ranki A, et al. European patient perspectives on the impact of psoriasis: the EUROPSO patient membership survey. Br J Dermatol. 2006;155:729–736. doi: 10.1111/j.1365-2133.2006.07405.x. [DOI] [PubMed] [Google Scholar]
- Young M. The psychological and social burdens of psoriasis. Dermatol Nurs. 2005;17:15–19. [PubMed] [Google Scholar]
- Rapp SR, Feldman SR, Exum ML, et al. Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol. 1999;41:401–407. doi: 10.1016/s0190-9622(99)70112-x. [DOI] [PubMed] [Google Scholar]
- Hrehorow E, Salomon J, Matusiak L, et al. Patients with psoriasis feel stigmatized. Acta Derm Venereol. 2011;92:67–72. doi: 10.2340/00015555-1193. [DOI] [PubMed] [Google Scholar]
- Naldi L, Chatenoud L, Linder D, et al. Cigarette smoking, body mass index, and stressful life events as risk factors for psoriasis: results from an Italian case-control study. J Invest Dermatol. 2005;125:61–67. doi: 10.1111/j.0022-202X.2005.23681.x. [DOI] [PubMed] [Google Scholar]
- Setty AR, Curhan G, Choi HK. Obesity, waist circumference, weight change, and the risk of psoriasis in women: nurses’ health study II. Arch Intern Med. 2007;167:1670–1675. doi: 10.1001/archinte.167.15.1670. [DOI] [PubMed] [Google Scholar]
- Finzi A, Colombo D, Caputo A, et al. Psychological distress and coping strategies in patients with psoriasis: the PSYCHAE Study. J Eur Acad Dermatol Venereol. 2007;21:1161–1169. doi: 10.1111/j.1468-3083.2007.02079.x. [DOI] [PubMed] [Google Scholar]
- Colombo D, Caputo A, Finzi A, et al. Evolution of and risk factors for psychological distress in patients with psoriasis: the PSYCHAE study. Int J Immunopathol Pharmacol. 2010;23:297–306. doi: 10.1177/039463201002300128. [DOI] [PubMed] [Google Scholar]
- Ersser SJ, Surridge H, Wiles A. What criteria do patients use when judging the effectiveness of psoriasis management? J Eval Clin Pract. 2002;8:367–376. doi: 10.1046/j.1365-2753.2002.00372.x. [DOI] [PubMed] [Google Scholar]
- Horne R. One to be taken as directed: reflections on non-adherence (non-compliance) J. Soc. Adm. Pharm. 1993;10:150–156. [Google Scholar]
- Bewley A, Page B. Maximizing patient adherence for optimal outcomes in psoriasis. J Eur Acad Dermatol Venereol. 2011;25(Suppl 4):9–14. doi: 10.1111/j.1468-3083.2011.04060.x. [DOI] [PubMed] [Google Scholar]
- Augustin M, Holland B, Dartsch D, et al. Adherence in the treatment of psoriasis: a systematic review. Dermatology. 2011;222:363–374. doi: 10.1159/000329026. [DOI] [PubMed] [Google Scholar]
- Fortune DG, Richards HL, Main CJ, et al. What patients with psoriasis believe about their condition. J Am Acad Dermatol. 1998;39:196–201. doi: 10.1016/s0190-9622(98)70074-x. [DOI] [PubMed] [Google Scholar]
- Carroll CL, Feldman SR, Camacho FT, et al. Better medication adherence results in greater improvement in severity of psoriasis. Br J Dermatol. 2004;151:895–897. doi: 10.1111/j.1365-2133.2004.06174.x. [DOI] [PubMed] [Google Scholar]
- Schaarschmidt ML, Schmieder A, Umar N, et al. Patient preferences for psoriasis treatments: process characteristics can outweigh outcome attributes. Arch Dermatol. 2011;147:1285–1294. doi: 10.1001/archdermatol.2011.309. [DOI] [PubMed] [Google Scholar]
- Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ. 2000;320:114–116. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heydendael VM, de Borgie CA, Spuls PI, et al. The burden of psoriasis is not determined by disease severity only. J Investig Dermatol Symp Proc. 2004;9:131–135. doi: 10.1111/j.1087-0024.2004.09115.x. [DOI] [PubMed] [Google Scholar]
- Evers AW, Lu Y, Duller P, et al. Common burden of chronic skin diseases? Contributors to psychological distress in adults with psoriasis and atopic dermatitis. Br J Dermatol. 2005;152:1275–1281. doi: 10.1111/j.1365-2133.2005.06565.x. [DOI] [PubMed] [Google Scholar]
- Schneider G, Heuft G, Hockmann J. Determinants of social anxiety and social avoidance in psoriasis outpatients. J Eur Acad Dermatol Venereol. 2013;27:383–386. doi: 10.1111/j.1468-3083.2011.04307.x. [DOI] [PubMed] [Google Scholar]
- Uttjek M, Dufaker M, Nygren L, et al. Psoriasis care consumption and expectations from a gender perspective in a psoriasis population in northern Sweden. Acta Derm Venereol. 2005;85:503–508. doi: 10.1080/00015550510036667. [DOI] [PubMed] [Google Scholar]
- Ersser SJ, Cowdell FC, Latter SM, et al. Self-management experiences in adults with mild-moderate psoriasis: an exploratory study and implications for improved support. Br J Dermatol. 2010;163:1044–1049. doi: 10.1111/j.1365-2133.2010.09916.x. [DOI] [PubMed] [Google Scholar]
- Menter A, Griffiths CE. Current and future management of psoriasis. Lancet. 2007;370:272–284. doi: 10.1016/S0140-6736(07)61129-5. [DOI] [PubMed] [Google Scholar]
- Ersser SJ, Cowdell FC, Nicholls PG, et al. A pilot randomized controlled trial to examine the feasibility and efficacy of an educational nursing intervention to improve self-management practices in patients with mild-moderate psoriasis. J Eur Acad Dermatol Venereol. 2012;26:738–745. doi: 10.1111/j.1468-3083.2011.04158.x. [DOI] [PubMed] [Google Scholar]
- Horne R, Weinman J, Barber N, et al. 2005. Concordance, adherence and compliance in medicine taking. Report for the National Co-ordinating Centre for NHS Service Delivery and Organisation R & D (NCCSDO). http://www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1412-076_V01.pdf (last accessed: 27 September 2012)
- Armstrong AW, Watson AJ, Makredes M, et al. Text-message reminders to improve sunscreen use: a randomized, controlled trial using electronic monitoring. Arch Dermatol. 2009;145:1230–1236. doi: 10.1001/archdermatol.2009.269. [DOI] [PubMed] [Google Scholar]
- Gadkari AS, McHorney CA. Unintentional non-adherence to chronic prescription medications: how unintentional is it really? BMC Health Serv Res. 2012;12:98. doi: 10.1186/1472-6963-12-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KK, Rehmus WE, Kimball AB. Determining the relative importance of patient motivations for nonadherence to topical corticosteroid therapy in psoriasis. J Am Acad Dermatol. 2006;55:607–613. doi: 10.1016/j.jaad.2005.12.021. [DOI] [PubMed] [Google Scholar]
- Gerdes S, Zahl VA, Weichenthal M, et al. Smoking and alcohol intake in severely affected patients with psoriasis in Germany. Dermatology. 2009;220:38–43. doi: 10.1159/000265557. [DOI] [PubMed] [Google Scholar]
- Yu AP, Tang J, Xie J, et al. Economic burden of psoriasis compared to the general population and stratified by disease severity. Curr Med Res Opin. 2009;25:2429–2438. doi: 10.1185/03007990903185557. [DOI] [PubMed] [Google Scholar]
- Fouere S, Adjadj L, Pawin H. How patients experience psoriasis: results from a European survey. J Eur Acad Dermatol Venereol. 2005;19(Suppl 3):2–6. doi: 10.1111/j.1468-3083.2005.01329.x. [DOI] [PubMed] [Google Scholar]
- Fleischer AB, Jr, Feldman SR, Rapp SR, et al. Disease severity measures in a population of psoriasis patients: the symptoms of psoriasis correlate with self-administered psoriasis area severity index scores. J Invest Dermatol. 1996;107:26–29. doi: 10.1111/1523-1747.ep12297659. [DOI] [PubMed] [Google Scholar]
- Schmitt JM, Ford DE. Role of depression in quality of life for patients with psoriasis. Dermatology. 2007;215:17–27. doi: 10.1159/000102029. [DOI] [PubMed] [Google Scholar]
- Jobling R, Naldi L. Assessing the impact of psoriasis and the relevance of qualitative research. J Invest Dermatol. 2006;126:1438–1440. doi: 10.1038/sj.jid.5700223. [DOI] [PubMed] [Google Scholar]


