Abstract
Background:
Arteriovenous malformations (AVMs) are high-flow lesions with abnormal connections between arteries and veins without an intervening capillary bed. Infrequently, the radiographic diagnosis of a vascular lesion will not support the clinical diagnosis of an AVM. These “discrepant” lesions are not adequately captured within the current classification system and represent a treatment dilemma. The purpose of this study is to review our center’s experience with vascular malformations where incongruity in a patient’s clinical and radiographic presentation produces a diagnostic and therapeutic challenge.
Methods:
A retrospective chart review of patients with atypical AVM pre sen ta tions was performed. Parameters reviewed included patient history and demogra phics, clinical presentation, radiological imaging, and treatment modalities.
Results:
Over a 15-year period, we identified 7 cases of vascular malformations with discrepant clinical and radiological findings concerning flow characteristics. All patients were treated based on their radiological diagnosis and most were managed with sclerotherapy. No lesions evolved into a high-flow process, and there was no recurrence at a minimum of 24 months of follow-up.
Conclusions:
We have identified and described a unique subcategory of vascular malformations that have clinical features of high-flow malformations but radiological features of low-flow malformations. These lesions behave like low-flow malformations and should be treated as such. We propose that complex vascular malformations are best evaluated by both clinical and specialized diagnostic radiological means; the radiologic diagnoses should supplant what is found clinically, and ultimately treatment should be preferentially based on a radiological diagnosis.
The currently accepted classification system for vascular anomalies is defined by the International Society for the Study of Vascular Anomalies (ISSVA)1 and incorporates clinical, radiologic, hemodynamic, and histopathologic features in establishing a diagnosis. Vascular anomalies within the ISSVA classification system are classified into vascular tumors and vascular malformations. Malformations are further subclassified into low-flow and high-flow lesions.1 Arteriovenous malformations (AVMs) are vascular lesions that are thought to result from an error during fetal development marked by the persistence of the arteriovenous channel of the primitive retiform plexus.2 This developmental error leads to the formation of a high-flow lesion that is characterized by a nidus, a direct connection between an artery and a vein without an intervening capillary bed. AVMs vary from discrete localized lesions to extensive lesions covering a large volume.3
Schobinger4 described the natural history of AVMs into a 4-stage staging system. Stage I is the quiescent stage where lesions present as a warm, pink, or bluish stain with arteriovenous shunting that can be appreciated with ultrasound. Stage II is marked expansion of the lesion and the development of pulsations, thrills, and bruits. In stage III, the lesion progresses through a destructive phase evidenced by dystrophic skin changes, ulceration, bleeding, persistent pain, and tissue necrosis. In the fourth and final stage, the lesion can cause systemic decompensation with congestive heart failure.2 Based on this classification system, resection of an AVM is often reserved for stage III lesions unless there is an opportunity for complete resection of a stage II lesion.
The classic diagnosis of an AVM is based on patient history and physical examination with confirmation based on diagnostic imaging. AVMs clinically present as a cutaneous blush with increased warmth that may be associated with pain, swelling, trophic changes, ulceration, bleeding, hyperhidrosis, and hypertrichosis.5 On physical examination, findings include presence of a thrill or pulsation on palpation and/or bruit on auscultation, and using a handheld Doppler, findings of a high-flow signal are audible. This high- to low-pressure system can also be detected with Doppler Ultrasound, computed tomography (CT) angiography, and magnetic resonance angiography (MRA). Angiography has the distinct advantage of producing detailed information regarding vessel anatomy, arteriovenous shunting, fistulas, and tortuosity2 that ultimately aids in directing therapeutic embolization. As such, radiological imaging is a critical tool in both the diagnosis and treatment of AVMs. AVMs are the most challenging type of vascular malformation to manage as they are fraught with high recurrence rates and are locally destructive to surrounding tissues.
The specific flow characteristics influence the treatment options available for a given lesion. Low-flow lesions, for example, are frequently treated with sclerotherapy, whereas high-flow lesions are treated with complete embolization, complete excision, or a mixture of both.5 The treatment of high-flow lesions follows a logical algorithm provided that both the clinical features and radiological features of the lesion are congruent.
In our Vascular Anomalies Clinic (VAC) at BC Children’s Hospital over the past 15 years, we observed a rare subset of patients with vascular malformations who do not fit in the current classification system. Some of these patients presented with AVMs that have high-flow lesion characteristics on both physical examination and 8-MHz handheld Doppler study, yet exhibit no evidence of a nidus or arteriovenous shunt on magnetic resonance angiography or angiography. These lesions, though clinically consistent with an AVM, are not radiologically consistent with a true AVM. A thorough literature search revealed no such entities in previously reported studies.
Given the controversy surrounding several patients with vascular malformations seen in our clinic that do not belong to the current classification system, the purpose of this study was to review and summarize these cases and discuss the challenges in their diagnosis and treatment. We believe the new entity we have identified introduces an important diagnostic and treatment dilemma that warrants further discussion.
METHODS
We retrospectively reviewed all patients over the last 15 years seen in the VAC at BC Children’s Hospital who presented with atypical AVMs with discrepant clinical and radiological features. Conceptualized as a retrospective records review, the study obtained ethics approval from the University of British Columbia/Children’s and Women’s Research Ethics Board (H13-00773). Inclusion criterion was a vascular malformation clinically categorized as a high-flow AVM with no radiological findings of a nidus or high-flow shunt.
Study subjects were identified through a search of the VAC patient database. The search included all patients seen in the period from 1998 to 2013. Once the study subjects were identified, their hospital records were reviewed and data were collected. Data collection included patient demographics, medical history, clinical presentation, handheld Doppler findings, radiological characteristics, treatment, and outcome.
RESULTS
A summary of each case was assembled, and a table of the main characteristics is presented (Table 1). Seven subjects were identified in this study. Two were male and 5 were female. In 2 of the 7 patients, a malformation was noted at birth. The present case series included a heterogeneous anatomical group of patients with primary lesions on leg, thigh, ear, face, and back, all of which presented with a high-flow Doppler signal. Most of the lesions had high-flow characteristics such as a palpable bruit, thrill, or warmth.
Table 1.
Summary of Patient Characteristics, Clinical and Radiological Findings, and Treatment
There were 2 male and 5 female patients with a mean age at presentation of 22 years (range, 4–67) and a mean follow-up period of 5 years (range, 2–10). The primary modality of imaging was angiogram, which showed a contradictory low-flow signal in 5 of 7 patients. In the remaining 2 patients, low flow was illustrated by MRA. Three patients were treated with sclerotherapy only. One patient was treated with a combination of sclerotherapy and surgical excision. One patient was treated with a combination of laser, surgical excision, and observation. One patient was managed expectantly, and one patient was lost to follow-up. At a minimum of 24 months of follow-up, no lesions had evolved into a high-flow process.
REPRESENTATIVE CASES
Patient 1
History
A 24-year-old healthy Asian male presented with a congenital vascular lesion of the left lateral shin measuring approximately 10 cm × 8 cm (Fig. 1). The lesion was detected at birth and became increasingly symptomatic during pubertal growth. The lesion demonstrated rapid growth, ulceration with poor wound healing, tissue friability, easy bleeding with minimal trauma, and pain exacerbated by hot weather and prolonged periods of standing.
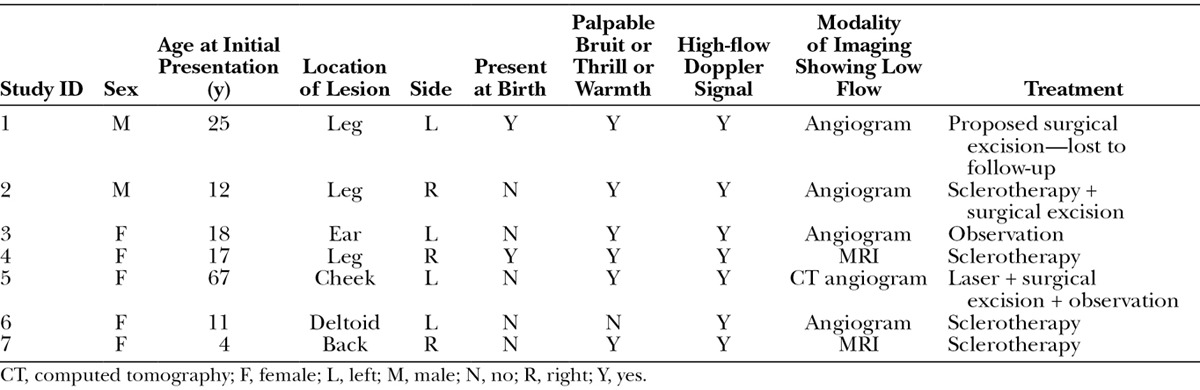
Fig. 1.
A 24-year-old man with a left lateral lower leg vascular lesion diagnosed as a “little AVM” illustrating clinical properties (A), MRI findings (B), and angiographic results (C).
Clinical Examination
At presentation, a large red area of cutaneous blush was observed with venous ectasia, hyperkeratosis, and areas of skin breakdown. The lesion was warm to touch and had a palpable thrill. It had a boggy consistency that displayed a mild increase in swelling when dependent, which did not correct significantly with leg elevation. A bruit was auscultated over the lesion, and a handheld Doppler produced a high-flow pulsatile signal. A working diagnosis of an AVM was made.
Radiological Findings
An MRA was obtained to support the working diagnosis. The MRA showed dilated vessels in the subcutaneous tissue with a minimal amount of muscle involvement, a pattern atypical of an AVM. Subsequent antegrade angiography revealed an atypical vascular anomaly with a varix, shunting without a true nidus.
Figure 1 illustrates the clinical and radiological findings.
Treatment
An excision, where a staged approach embolizing the AVM before surgical resection, was proposed using a split-thickness skin graft. The treatment plan was never implemented as the patient moved out-of-province and was lost to follow-up.
Patient 2
History
A 12-year-old white boy presented with a mass on the medial aspect of his right thigh (Fig. 2). The lesion was not present at birth and was first appreciated at age 12 as a small mass. The lesion was largely asymptomatic other than discomfort brought on by extended periods of sitting. There were no overlying cutaneous changes or neurovascular symptoms associated with the lesion.
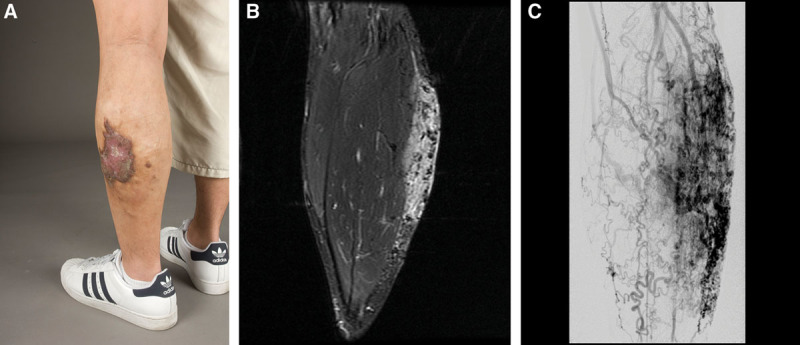
Fig. 2.
A 12-year-old boy with a right thigh vascular lesion diagnosed as a “little AVM” illustrating clinical properties (A), MRI findings (B), and angiographic results (C).
Clinical Examination
On physical examination, the lesion was warm, a handheld Doppler clearly showed increased arterial flow in the lesion, and a working clinical diagnosis of an AVM was made.
Radiological Findings
Both a CT angiogram and MRA were performed. An MRI of the right thigh showed no evidence of bony involvement or infiltrative local disease to the muscle. Angiogram supported the venous phase abnormality seen on CT and MRA and suggested a perforator type arterial shunt into the venous varix, consistent with the clinically demonstrated high flow seen on the Doppler examination. The lesion was more consistent with a venous malformation with microshunts rather than a true nidus presenting AVM. Figure 2 illustrates the clinical and radiological findings.
Treatment
The lesion was initially treated with direct puncture embolization of the outflow track and direct sclerotherapy of the venous varix itself. It was concluded that the lesion was more in keeping with a venous malformation with a micro arteriovenous shunt. The lesion remained symptomatic, however, and it was successfully treated with a surgical excision.
Patient 4
History
A 17-year-old white girl presented with a long-standing history of a vascular anomaly of the right distal lateral lower leg (Fig. 3). The lesion was present at birth and has grown with her. The lesion had a history of temperature and color variation and easy bruising.
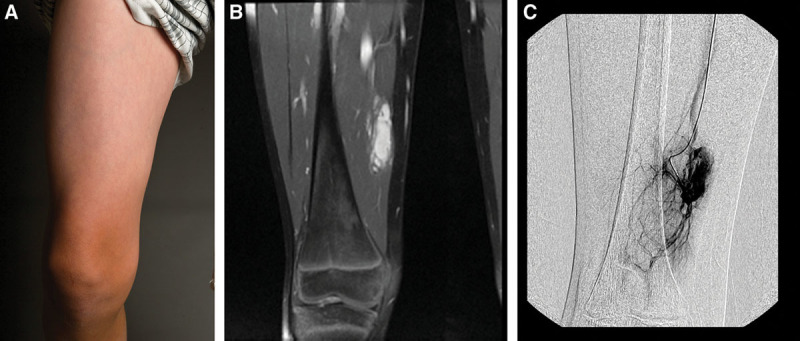
Fig. 3.
A 17-year-old girl with a left lateral lower leg vascular lesion diagnosed as a “little AVM” illustrating clinical properties (A) and MRI findings (B).
Clinical Examination
The lesion was a 5 cm × 6 cm soft, warm compressible swelling that was nontender. A thrill was evident on palpation, and handheld Doppler examination revealed high arterial flow at the site.
Radiological Imaging
MRI revealed a subtle 2 cm × 1 cm × 4 cm focus of subcutaneous soft-tissue thickening, which contained 2 small arterial branches. This was consistent with a small, subcutaneous venous malformation with no frank nidus in the lesion. Figure 3 illustrates the clinical and radiological findings.
Treatment
It was determined that sclerotherapy would be the most appropriate treatment approach. This was performed without complication.
Patient 6
History
An 11-year-old girl presented with a lesion of the superficial lateral left shoulder (Fig. 4). The lesion was noted at birth and had no associated symptoms. It was initially presumed to be a venous vascular malformation.
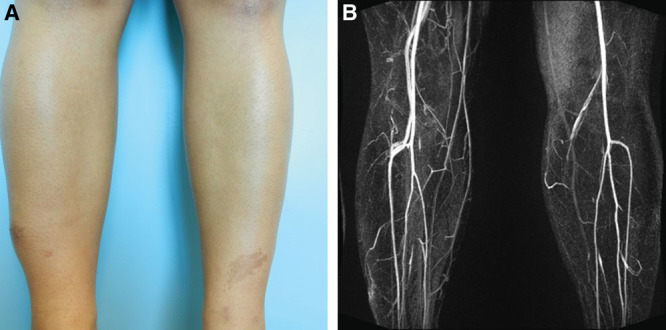
Fig. 4.
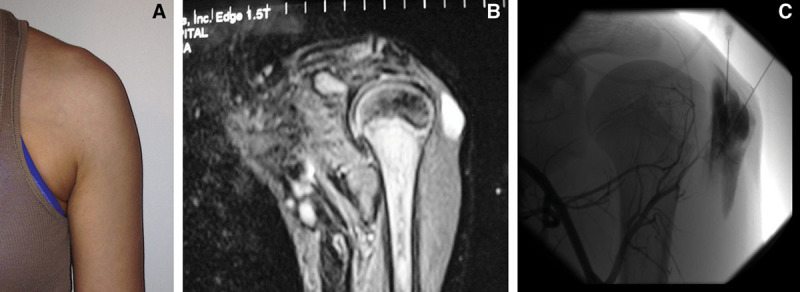
A 11-year-old girl with a left shoulder vascular lesion diagnosed as a “little AVM” illustrating clinical properties (A), MRI findings (B), and angiographic results (C).
Clinical Examination
On examination, the skin over the lesion appeared normal and the lesion became more prominent during contraction of the deltoid and when the shoulder was hanging and relaxed. The patient had an episode of superficial thrombophlebitis and was thought to have a small palpable phlebolith. On examination with a handheld Doppler, the lesion revealed a high-flow signal.
Radiological Findings
Doppler examination performed following ethanol ablation revealed both an accessory brachial artery proximally and an accessory artery in the distal arm, immediately anterior to the brachial artery. Angiogram showed a rare variant of the brachial artery that was superficial and continued distally as the common interosseous artery. Abnormally early pooling of contrast into the varix structures was demonstrated and the lesion appeared to be supplied by very small branches of the profunda brachii artery despite the absence of a nidus typical of an AVM. It was concluded that despite the arterial filling, based on flow characteristics, it was difficult to classify this lesion as a true AVM. Figure 4 illustrates the clinical and radiological findings.
Treatment
Due to the predominant low-flow characteristics of the lesion, sclerotherapy was decided upon as the primary treatment, which was performed without complication.
DISCUSSION
Historically, the nomenclature and subtyping of vascular anomalies has been fraught with confusion.6 The most recent ISSVA classification system has clarified the subcategories of vascular lesions based on both clinical and radiological features.7 Although a useful classification tool, it omits a subcategory of vascular anomalies that we have encountered in our clinic. This subcategory includes lesions that have clinical features incongruous with their radiological features. As such, the definitive diagnosis of these lesions is unclear as is their corresponding treatment.
The lesions that we have described herein all share the following description: clinical features of a high-flow lesion but radiological features of a low-flow lesion. The present case series posit the important question of whether a spectrum of clinical presentation and severity of high-flow vascular malformations exist. Are these lesions simply immature AVMs or are they primarily venous malformations with a clinically identifiable arterial feeding vessel? Regardless of their true etiology, we have found success when these lesions are treated based on their radiological diagnoses as low-flow lesions; no lesions evolved into a high-flow “typical” AVM. Under these circumstances, we propose that the radiologic diagnosis take precedence and that the lesion be treated based on the radiological diagnosis alone.
CONCLUSIONS
We have identified and described a unique subcategory of vascular anomalies that have clinical features of a high-flow malformation but radiological features of a low-flow malformation. Although it is difficult to commit to an affirmed diagnosis for these lesions, we have found that they respond when treated based on their radiological findings. From a practical treatment standpoint, these lesions behave like low-flow lesions and should be treated as such. We propose that these lesions belong to a novel category that is not currently captured in the ISSVA system, namely, one which describes a low-flow AVM. Additional, multicenter, larger cohort studies are warranted to further elucidate this novel category of vascular malformation.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The article processing charge for this article was paid for by the author.
REFERENCES
- 1.Enjolras O, Mulliken JB. Vascular tumors and vascular malformations (new issues). Adv Dermatol. 1997;13:375–423. [PubMed] [Google Scholar]
- 2.Arneja JS, Gosain AK. Vascular malformations. Plast Reconstr Surg. 2008;121:195e–206e. doi: 10.1097/01.prs.0000304607.29622.3c. [DOI] [PubMed] [Google Scholar]
- 3.Van Aalst JA, Bhuller A, Sadove AM. Pediatric vascular lesions. J Craniofac Surg. 2003;14:566–583. doi: 10.1097/00001665-200307000-00032. [DOI] [PubMed] [Google Scholar]
- 4.Mulliken B. Vascular anomalies. In: Thorne CH, Bartlett SP, Beasley RW, editors. Grabb and Smith’s Plastic Surgery. Philadelphia: Lippincott-Raven; 1997. [Google Scholar]
- 5.Spring MA, Bentz ML. Cutaneous vascular lesions. Clin Plast Surg. 2005;32:171–186. doi: 10.1016/j.cps.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Arneja JS. Where have we arrived in the care of vascular anomalies a generation after Mulliken’s classification system? Can J Plast Surg. 2012;20:65. doi: 10.1177/229255031202000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lowe LH, Marchant TC, Rivard DC, et al. Vascular malformations: classification and terminology the radiologist needs to know. Semin Roentgenol. 2012;47:106–117. doi: 10.1053/j.ro.2011.11.002. [DOI] [PubMed] [Google Scholar]


