Abstract
Descending controls of spinal nociceptive processing play a critical role in the development of inflammatory hyperalgesia. Acute peripheral nociceptor sensitization drives spinal sensitization and activates spino–supraspinal–spinal loops leading to descending inhibitory and facilitatory controls of spinal neuronal activity that further modify the extent and degree of the pain state. The afferent inputs from hairy and glabrous skin are distinct with respect to both the profile of primary afferent classes and the degree of their peripheral sensitization. It is not known whether these differences in afferent input differentially engage descending control systems to different extents or in different ways. Injection of complete Freund's adjuvant resulted in inflammation and swelling of hairy hind foot skin in rats, a transient thermal hyperalgesia lasting <2 h, and longlasting primary mechanical hyperalgesia (≥7 days). Much longer lasting thermal hyperalgesia was apparent in glabrous skin (1 h to >72 h). In hairy skin, transient hyperalgesia was associated with sensitization of withdrawal reflexes to thermal activation of either A- or C-nociceptors. The transience of the hyperalgesia was attributable to a rapidly engaged descending inhibitory noradrenergic mechanism, which affected withdrawal responses to both A- and C-nociceptor activation and this could be reversed by intrathecal administration of yohimbine (α-2-adrenoceptor antagonist). In glabrous skin, yohimbine had no effect on an equivalent thermal inflammatory hyperalgesia. We conclude that acute inflammation and peripheral nociceptor sensitization in hind foot hairy skin, but not glabrous skin, rapidly activates a descending inhibitory noradrenergic system. This may result from differences in the engagement of descending control systems following sensitization of different primary afferent classes that innervate glabrous and hairy skin.
Introduction
Tissue damage and subsequent inflammation activate and sensitize peripheral nociceptors. This increases afferent input to central nociceptive circuits and leads to enhanced sensitivity to nociceptive stimuli (hyperalgesia), and sensations of pain to innocuous stimulation (allodynia) (Meyer et al. 2005; Latremoliere & Woolf, 2009). Peripheral nociceptive inputs drive both the sensitization of spinal nociceptive circuits and the activation of ascending and descending pathways that together modulate transmission, and ultimately perception, of nociceptive information (Mantyh & Hunt, 2004). The final perception of the intensity and quality of pain is determined by the degree of such modulation of information throughout the nociceptive neuraxis (Ossipov et al. 2010).
It is well established that spinal nociceptive processing is modulated by both inhibitory and facilitatory descending pathways that originate supraspinally (Millan, 2002). The midbrain periaqueductal grey (PAG) forms a major component of the descending nociceptive system and relays via brainstem nuclei such as the locus coeruleus (LC) and the rostroventral medulla (RVM) (Mantyh, 1983; Bajic & Proudfit, 1999) to exert controls on spinal nociceptive neurons. Descending controls from the PAG include opioidergic (Vasquez & Vanegas, 2000; Przewłocki & Przewłocka, 2001; Kwok et al. 2013) and monoaminergic (Pertovaara, 2006) inhibition, as well as prostanergic facilitation (Oliva et al. 2006; Leith et al. 2007; Palazzo et al. 2011). Medullary and brainstem nuclei are major sources of spinally projecting monoaminergic fibres (Westlund et al 1983; Yoshimura & Furue, 2006) that are known to exert inhibitory influences, which modulate the development of acute and persistent pain states (Vanegas & Schaible, 2004; Pertovaara, 2006, 2013; Yoshimura & Furue, 2006). Descending noradrenergic systems exert these inhibitory influences largely through presynaptic inhibition, primarily through α-2-adrenoceptor activation (Pertovaara, 2006; Yoshimura & Furue, 2006). α-2-Agonists, in particular those with affinity for α-2A receptors, are antinociceptive in both animals and humans (Pertovaara, 2006). Descending serotonergic systems exert complex pro- and antinociceptive effects at the spinal level, primarily through 5-HT1 and 5-HT3 receptors (Yoshimura & Furue, 2006; Dogrul et al. 2009; Jeong et al. 2012). Additionally, there are peripheral sources of monoamines, such as sympathetic fibres within the dorsal root ganglia, that are able to impact upon nociception during periods of prolonged inflammation or tissue damage (Pertovaara, 2006). Peripheral nerve stimulation evokes spinal release of monoamines in the presence of ganglionic blocking agents (Tyce & Yaksht, 1981), however, and thus it is widely accepted that the major sources of spinal noradrenaline and serotonin are projections from medullary and brainstem nuclei (Pertovaara, 2006; Yoshimura & Furue, 2006).
Acute cutaneous inflammation leads to sensitization of peripheral and central nociceptive neurons, resulting in primary and secondary hyperalgesia. Descending controls of the spinal processing of input from the area of primary hyperalgesia are initially facilitatory from, for example PAG/RVM, but are short-lived (up to 3 h), and are then overwhelmed by local spinal and supraspinal inhibitory influences (Ren & Dubner, 1996; Guan et al. 2002; Miki et al. 2002; Vanegas & Schaible, 2004). The dampening effect of the inhibitory systems on spinal dorsal horn activity effectively reduces the extent of inflammatory pain by limiting central sensitization (Vanegas & Schaible, 2004).
Current understanding of the development of inflammatory hyperalgesia and the influence of descending controls over spinal nociceptive processing is largely derived from animal models using inflammatory insults to the glabrous skin of the hind limb. There is little information on the contribution of descending controls to the development or maintenance of primary hyperalgesia in hairy skin, which is a potential shortcoming given this is the more prevalent skin type in mammals. Glabrous cutaneous tissue found on the plantar surface of the foot forms a major informative surface of the body providing critical sensory and discriminative information about the environment. This is reflected by a greater density of primary afferents innervating glabrous tissue and its over-representation in cortical somatotopic maps (Blake et al. 2002; Provitera et al. 2007; Boada et al. 2013). There are notable differences in the profiles of nociceptive afferent fibres that innervate glabrous and hairy cutaneous tissue: for instance, a three-fold higher proportion of fast-conducting to slowly conducting fibres innervates glabrous cutaneous tissue (Boada et al. 2013), and a large proportion of C-polymodal nociceptors innervate the hairy skin of the rat hind foot (Lynn & Carpenter, 1982; Leem et al. 1993). Critically, there are differences in the sensitization of unmyelinated nociceptive afferents innervating the two skin types. Following application of conditioning stimuli or sensitizing agents, a population of polymodal C-nociceptors found in glabrous skin fail to sensitize to thermal stimuli, but a similar population of polymodal C-nociceptors found in hairy cutaneous tissue do sensitize, with a lowering of activation threshold and/or increased suprathreshold response (Campbell & Meyer, 1983; Andrew & Greenspan, 1999; Koerber et al. 2010). We hypothesized that during inflammation, the differences in primary afferent input from different skin types might differentially drive descending control systems and hence differentially affect the development of inflammatory hyperalgesia in the two skin types.
Methods
All experiments were performed in accordance with the UK Animals (Scientific Procedures) Act (1986) and associated guidelines. Animals were housed in standard conditions with food and water provided ad libitum. Experiments were performed in a total of 58 male Wistar rats weighing 250–350 g. The majority of animals (n = 55) received a s.c. injection of 50 μg or 100 μg of complete Freund's adjuvant (CFA) (1 mg ml−1; cat. no. F5881; Sigma-Aldrich Co. Ltd, Gillingham, UK) into either the dorsal or ventral surface of the left hind foot under brief halothane (3% in O2) anaesthesia. Control animals (n = 3) received a s.c. injection of an equivalent volume of vehicle (mineral oil). CFA induces a dose-dependent increase in swelling, in both rat and mouse, up to doses of 250 μg and 500 μg, respectively. This CFA dose/volume (50 μg/50 μl) gives a mild, limited inflammation that is less than the maximal achievable with CFA, and that does not spread to involve the sides or other surface of the hind limb. Greater swelling and spread of inflammation can be seen with higher doses of CFA (Donaldson et al. 1993; Chillingworth et al. 2006). Although differences in oedema have been previously reported with higher CFA doses (Cook & Moore, 2006), we chose to investigate the effects of equivalent inflammatory stimuli in this study, rather than equivalent oedematous responses.
Nociceptive behavioural testing
To assess the effect of s.c. CFA injections at different sites on nociceptive behaviour, some animals (n = 7) underwent nociceptive testing before and at 3 h and 1 day, 3 days and 7 days after either dorsal or plantar s.c. CFA injection. Animals were habituated to the apparatus and experimenter beginning 3 days prior to the start of testing. For mechanical hyperalgesia, serrated laboratory forceps were adapted with strain gauges for the measurement of the force applied across the tips (contact area: 5.6 mm2 per tip; total area: 11.2 mm2) (Fig.1). The output signal was fed through a bridge amplifier and captured for subsequent offline analysis via a CED1401 [Cambridge Electronic Design (CED) Ltd, Cambridge, UK] on a computer running Spike2 software (CED Ltd). Grams per volt were calculated following calibration with standardized weights placed at the point of finger grip. The gram force delivered was then divided by the total contact area to give grams mm−2. The tips were placed across the dorsoventral aspect of the hind foot and ramped pressure was applied until the foot was withdrawn or the animal displayed pain-related behaviours (vocalization, biting, etc.), at which point the force applied was immediately stopped. As the duration and force applied were controlled manually, and cut off at the first appearance of pain-related behaviours, the intensity of this stimulus could be controlled to ensure that it did not result in additional tissue damage. Use of this stimulator did not result in any observable tissue damage in naïve or inflamed animals. The occurrence of withdrawal/response was marked using the input from a foot pedal through the CED1401 into a computer running Spike2 software. Two consecutive recordings were made and the mean threshold was calculated for each animal at each time-point.
Figure 1. Apparatus for mechanical stimulation of the hind limb.
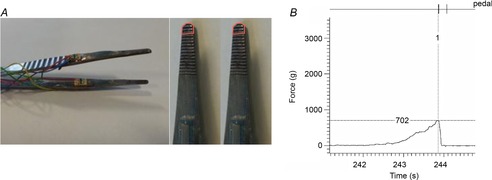
A, the mechanical stimulator. Strain gauges were attached to both arms of laboratory forceps to allow for the measurement of force delivered across the tips. The picture of the tips of the forceps shows the area in contact with the foot (area: 5.6 mm2 for each tip; total: 11.2 mm2). B, digitized trace of raw data showing actual force applied to the rat hind foot. Withdrawal is marked with input from a foot pedal (top trace), at which point the withdrawal threshold was determined.
To test for thermal hyperalgesia, a custom-built Peltier heating device (contact area: 18 mm2) was used to deliver a ramped thermal stimulus to the hind foot of the rat from an initial contact temperature of 30°C. The maximum temperature was cut off at 55°C to prevent tissue damage. Surface (contact) temperature was measured with a T-type thermocouple (made in-house) and captured for subsequent offline analysis via a CED1401 on a computer running Spike5 software. Again, the occurance of withdrawal/response was marked using the input from a foot peddle through the CED1401 into a computer running Spike2 software. The extent of limb oedema was assessed by measuring the thickness across the midline dorsoventral aspect of the hind foot using callipers before, and at 1 h, and 1, 3 and 7 days after CFA injection.
Surgical preparation
Surgical preparation for electromyograph (EMG) recordings was performed under initial halothane anaesthesia (2–3% in O2) and consisted of: (i) external jugular branch cannulation for anaesthetic maintenance [constant i.v. infusion of alphaxalone (∼40 mg kg h, Alfaxan; Jurox Pty Ltd, Rutherford, NSW, Australia)]; (ii) external carotid artery branch cannulation for blood pressure measurement, and (iii) tracheal cannulation for airway maintenance. Body temperature was maintained within physiological limits (37–38°C) by means of a feedback-controlled heating blanket and rectal probe. For placement of the intrathecal catheter (Størkson et al. 1996), a longitudinal incision was made along the back midline, starting at the level of the iliac crest and advancing 2–3 cm rostrally. A 6 cm length of 32G polyurethane catheter (external diameter: 0.25 mm; internal diameter: 0.13 mm) with a manufacturer-supplied internal metal stylet for increased rigidity (cat. no. 0041; ReCathCo LLC, Allison Park, PA, USA) was back-loaded into a 25G needle (Terumo UK Ltd, Egham, Surrey, UK) so that the end of the catheter was flush with the needle tip. Animals were positioned with the vertebral column flexed and the catheter-loaded needle was inserted bevel up between the L5 and L6 vertebrae until a tail flick indicated penetration of dura. The catheter was then advanced ∼3 cm rostrally along the intrathecal space to approximately the level of the lumbar enlargement. The needle and stylet were then carefully removed, leaving in place the catheter, which was then fixed in position with cyanoacrylate glue (Superglue). A small (∼2 cm) length of polyethylene tubing (external diameter: 6.1 mm; internal diameter: 2.8 mm) was then attached to the free end of the catheter by inserting the catheter end just into the polyethylene tubing, which was then secured with cyanoacrylate, to allow for connection to a Hamilton syringe for drug delivery.
For the measurement of EMG activity, a bi-polar electrode was custom-made using Teflon-coated stainless steel wires (0.075 mm diameter; Advent Research Materials, Eynsham, Oxford, UK) that were stripped at both ends; one end was inserted into the bicep femoris of the hind limb using a 25-gauge hypodermic needle. The signal across the electrodes was amplified (×1k, Neurolog NL104 amplifier, A-B configuration; Digitimer Ltd, Letchworth Garden City, UK) and filtered (50 Hz to 5 kHz, Neurolog NL125) and raw data were digitized via the CED1401 and stored for offline analysis using Spike2. Animals were left under a constant level of anaesthesia for a minimum of 1 h after surgical preparation before further experiments. The level of anaesthesia was maintained by constant infusion such that EMG activity could be detected in response to stimulation without overt limb movement.
Preferential activation of A- and C-heat nociceptors
A- and C-nociceptors were preferentially activated using a custom-made heat lamp in contact with the dorsal hind foot. A constant voltage was applied to the lamp to provide fast (7.5 ± 1°C s−1) or slow (2.5 ± 1°C s−1) rates of heating, which preferentially activate A-fibre (myelinated, capsaicin-insensitive) and C-fibre (unmyelinated, capsaicin-sensitive) heat nociceptors, respectively (Yeomans & Proudfit, 1996; McMullan et al. 2004; McMullan & Lumb, 2006a; Leith et al. 2007). Stimuli were applied with an inter-stimulus interval of ≥8 min to prevent tissue damage and sensitization. The heat ramp apparatus was placed in contact with the foot for a minimum of 60 s before the start of the heat stimulation to allow for adaptation of low-threshold mechanoreceptors. A feedback-controlled cut-off was set at 58°C for fast thermal ramps and at 55°C for slow thermal ramps to prevent tissue damage. In recordings in which thermal ramps reached the cut-off temperature without the occurrence of measurable EMG activity, threshold was recorded as cut-off +2°C (Leith et al. 2007). For stimulation of glabrous skin, a slow ramp (2.5 ± 1°C s−1) contact heat stimulus was applied immediately behind the footpad using the same apparatus. As it has not yet been determined whether this stimulus is able to preferentially activate A- or C-nociceptors in glabrous skin, no attempt was made to draw conclusions on A- or C-nociceptor activation at this site.
Subsurface heating rate measurement
To determine whether CFA-induced foot oedema affected the subcutaneous heating rates required for preferential activation of A- and C-nociceptors, subcutaneous heating rates were directly measured using a T-type thermocouple. Heating rates were recorded before, for 3 h and on day 7 after s.c. CFA injection. Care was taken to implant the thermocouple as closely as possible to the dermal–epidermal junction as nociceptive terminals are found in the epidermis and superficial dermal layers. Two ramps were delivered at each experimental time-point.
Drugs
The α-2-adrenoreceptor antagonist yohimbine 30 μg in 10 μl in vehicle (80% saline, 20% DMSO, cat. no. 1127; Tocris Biosciences, Bristol, UK) was delivered intrathecally via the implanted catheter 2.5 h after CFA (n = 9) so that the peak drug effect coincided with the third hour following CFA. The concentration of yohimbine used was based on previous reports of effective intrathecal α-2 adrenoceptor blockade (Ossipov et al. 1989; Takano & Yaksh, 1992; Green et al. 1998). At the time of injection the tip of a 100 μl Hamilton syringe was inserted into the PE10 tubing and 10 μl of the drug was delivered over several minutes. This was washed through with an equivalent volume of saline. In a separate group of animals (n = 6), the non-specific opioid antagonist naloxone (3 mg kg−1 in 0.9% saline) (cat. no. N7758; Sigma-Aldrich Co. Ltd) was delivered i.p. so that the peak drug effect coincided with the second hour following CFA.
At the end of the experiment the position of the cannula was determined by injecting 20 μl of xylocaine (2%) through the cannula. If pinch-evoked EMG activity was abolished, the cannula was deemed to be correctly positioned; if not, the data were not included in subsequent analyses (n = 1, CFA injected). Additionally, in some experiments the location of the distal tip of the catheter was determined by injection of pontamine Sky Blue (20 μl of 5%) and visual confirmation of the location of the catheter tip.
Statistical analyses
Data are displayed as the mean ± s.e.m. unless otherwise noted in figure legends. Data were analysed using Graphpad Prism Version 4/5 (GraphPad Software, Inc., La Jolla, CA, USA) using the Mann–Whitney test (two-group comparisons) or Kruskal–Wallis test, one- or two-way ANOVA (three or more groups) as appropriate and as stated in figure legends.
Results
Consequences of CFA-induced inflammation of the hairy skin of the rat hind foot
Injection of 50 μg CFA into the hind foot dorsum resulted in foot oedema that was evident after 1 h and persisted for 7 days (baseline, 4.2 ± 0.1 mm vs. 7 days, 6.3 ± 0.2 mm; P < 0.001) (Fig.2A). CFA also produced a mechanical hyperalgesia to a noxious pinch (baseline, 87 ± 33 g mm−2 vs. 7 days, 39 ± 5 g mm−2; P < 0.05) (Fig.2B), but did not induce a thermal hyperalgesia in hairy skin (baseline, 49 ± 1.1°C; 3 h, 49 ± 2.3°C; 24 h, 47 ± 1.3°C; 3 days, 51 ± 1.0°C) (Fig.2C). An equivalent s.c. injection of CFA into the plantar surface of the hind foot resulted in thermal hyperalgesia that persisted for at least 3 days (baseline, 47 ± 0.9°C vs. 3 days, 42 ± 1.2°C; P < 0.05) (Fig.2D).
Figure 2. A single s.c. injection of complete Freund's adjuvant (CFA) into the hind foot dorsum leads to a primary mechanical but not thermal hyperalgesia.
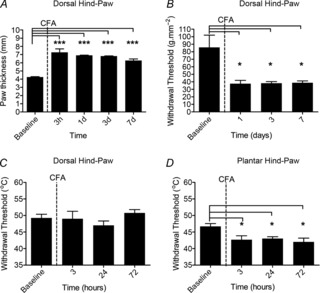
A, delivery of CFA (50 μl) into the hind foot dorsum produced significant oedema [one-way repeated-measures (RM) ANOVA, P < 0.0001, F(4,3) = 33.54; Bonferroni's post-test, *P < 0.001 compared with baseline; n = 4]. B, CFA-induced inflammation was associated with a primary mechanical hyperalgesia (one-way RM ANOVA, P < 0.001, F(3,3) = 7.13; Bonferroni's post-test, *P < 0.05 compared with baseline; n = 4). C, CFA-induced inflammation did not, however, result in thermal hyperalgesia (n = 4). D, by contrast, a 50 μl s.c. injection of CFA into the plantar surface of the hind foot produced a persistent primary thermal hyperalgesia (one-way RM ANOVA, P < 0.05, F(3,2) = 11.88; Bonferroni's post-test, *P < 0.05 compared with baseline; n = 3).
The ability of the thermal ramp stimuli to preferentially activate A- and C- nociceptors is reliant on the achievement of subsurface cutaneous heating rates of 2.5°C s−1 (fast) for A-nociceptors and 0.8°C s−1 (slow) for C-nociceptors (Yeomans & Proudfit, 1996; McMullan et al. 2004; McMullan & Lumb, 2006a; Leith et al. 2007). As limb oedema could affect the heat transfer through the skin, and thus subcutaneous heating rates, we first determined the effect of acute inflammatory oedema on cutaneous heating rates. Surface heating rates elicited by both fast and slow heating ramps were kept within limits previously shown to elicit correct subsurface heating rates in normal skin (fast: – 7.5°C s−1; slow – 2.5°C s−1) (McMullan et al. 2004) and the corresponding subsurface heating rates were recorded. Subsurface heating rates to both fast and slow thermal ramps were unchanged over the 3 h of acute inflammation (P > 0.05) (Fig.3). However, at 7 days following CFA, subsurface heating rates elicited by slow thermal ramps were significantly faster than pre-CFA values (baseline subsurface rate, 0.6 ± 0.03°C s−1 vs. 7 day subsurface rate, 1.2 ± 0.1°C s−1; P < 0.05) (Fig.3).
Figure 3. A single s.c. injection of complete Freund's adjuvant (CFA) into the hind foot dorsum does not affect the subcutaneous heating rates required to preferentially activate A- and C-nociceptors during acute inflammation.
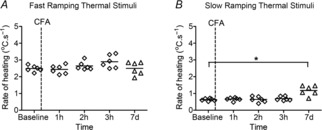
A, acute (1–3 h) or more chronic (7 days) CFA-induced inflammation of the dorsal hind foot did not affect the ability of fast surface ramps to deliver subcutaneous heating rates to preferentially activate A-nociceptors. B, acute inflammation did not affect the ability of slow surface ramps to deliver subcutaneous heating rates to preferentially activate C-nociceptors (Kruskal–Wallis test, P > 0.05; n = 3 both groups). However, 7 days following CFA, subsurface rates delivered by slow ramps were slightly but significantly faster than in naïve animals (Kruskal–Wallis test, P < 0.05; Dunn's multiple comparison test, *P < 0.05; n = 3).
Effect of CFA-induced inflammation on the spinal processing of thermal nociceptor inputs from hairy and glabrous skin
We sought to determine the effects of CFA-induced inflammation of hairy skin on the spinal processing of A- and C-nociceptor inputs. Withdrawal thresholds to thermal A- and C-nociceptor stimulation were both significantly lower at 1 h after CFA injection (baseline A-nociceptors vs. 1 h A-nociceptors, 57 ± 0.8°C vs. 45 ± 0.9°C; P < 0.001) (Fig.4A) (baseline C-nociceptors vs. 1 h C-nociceptors, 53 ± 0.4°C vs. 40 ± 1.8°C; P < 0.001) (Fig.4B). After 2 h, the withdrawal threshold to C-nociceptor stimulation had returned to slightly above baseline levels (baseline vs. 2 h, 53 ± 0.4°C vs. 54 ± 2.0°C) (Fig.4B), whereas A-nociceptor thresholds were still lowered (baseline vs. 2 h, 57 ± 0.8°C vs. 49 ± 2.0°C; P < 0.001) (Fig.4A). By 3 h, A- and C-nociceptor thresholds had returned to baseline values (P > 0.05) (Fig.4A and B). Vehicle injection had no significant effect on A- or C-nociceptor thresholds (P > 0.05) (Fig.4A and B). It should be noted that in three of five animals, at 2 h and 3 h following CFA, no EMG activity to C-nociceptor stimulation was evoked before stimulation reached the imposed cut-off temperature. Furthermore, in two additional animals (data not shown and not used in further analysis) the cut-off was not imposed and in these animals we found thresholds for withdrawal to C-nociceptor activation to be greater than 60°C. By contrast, thresholds of withdrawal to A-nociceptor activation were always below the imposed temperature cut-off.
Figure 4. A single s.c. injection of complete Freund's adjuvant (CFA) into the hind foot dorsum produces a transient sensitization of withdrawal reflexes to A- and C-nociceptor activation.
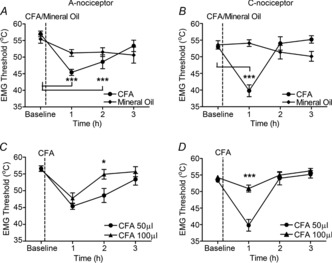
A, CFA-induced inflammation of the dorsal hind foot resulted in a transient reduction in the withdrawal threshold to A-nociceptor stimulation that resolved fully by 3 h after CFA injection [one-way repeated-measures (RM) ANOVA, P < 0.0001, F(3,4) = 21.22; Bonferroni's post-test, ***P < 0.001 compared with baseline; n = 5]. B, responses to C-nociceptor activation showed that inflammation resulted in an even more transient response, resolving after 2 h (one-way RM ANOVA, P < 0.0001, F(3,4) = 20.39; Bonferroni's post-test, *P < 0.001 compared with baseline; n = 5). An equivalent injection of vehicle (mineral oil) had no significant effect on withdrawal thresholds to A- or C-nociceptor activation (mineral oil group, Friedman test, P > 0.05; n = 3). C, a larger dose of CFA (100 μg/100 μl) resulted in a more rapid resolution of sensitization to A-nociceptor activation, causing a more rapid return to baseline (two-way RM ANOVA, main dose effect, P = 0.08, F(3,1) = 3.98; Bonferroni's post-test, *P < 0.05 between groups; n = 5 for both groups). D, a larger dose of CFA (100μg) resulted in a more rapid resolution of sensitization to C-nociceptor activation so that withdrawal thresholds were significantly higher than with a 50 μg dose at the 1 h time-point (two-way RM ANOVA, main dose effect, P = 0.0022, F(3,1) = 19.53; Bonferroni's post-test, ***P < 0.001 between groups; n = 5 for both groups).
Doubling the amount of injected CFA resulted in significantly less sensitization of the reflex pathway over the 3 h period (Fig.4C and D). Compared with the 50 μg dose, a 100 μg CFA injection caused similar reduction in the A-nociceptor withdrawal threshold at 1 h, but surprisingly significantly less reduction in the C-nociceptor threshold at this time (50 μg at 1 h vs. 100 μg at 1 h, 40 ± 1.8°C vs. 51 ± 1.0°C; P < 0.001) (Fig.4D). At 2 h, both C- and A-nociceptor withdrawal thresholds had returned to baseline values and A-nociceptor withdrawal thresholds were significantly higher than threshold values for the 50 μg dose at the same time-point (50 μl at 2 h vs. 100 μl at 2 h, 49 ± 2.0°C vs. 55 ± 1.4°C; P < 0.05) (Fig.4C).
Although CFA is known to produce persistent afferent sensitization lasting days or weeks (Ren & Dubner, 1999), following dorsal CFA we found thermal nociceptive behaviour to be unchanged at 3 days (Fig.2). Additionally, at 7 days after CFA injection, withdrawal thresholds to A- and C-nociceptor activation were also unchanged (C-nociceptor naïve vs. C-nociceptor 7 day CFA, 53 ± 0.6°C. vs. 55 ± 2.0°C; Mann–Whitney test, P > 0.05; n = 4; A-nociceptor naïve vs. A-nociceptor 7 day CFA, 58 ± 0.5°C vs. 58 ± 0.6°C; Mann–Whitney test, P > 0.05; n = 4, not shown). By contrast, although the withdrawal threshold did increase slightly towards baseline over 3 h, injection of CFA into the glabrous skin of the plantar hind foot resulted in a significant reduction in withdrawal thresholds to the thermal stimulus for the 3 h studied (P < 0.05 at all time-points) (Fig.5). It has been previously shown that s.c. CFA delivered to the plantar surface of the foot leads to thermal hyperalgesia lasting >1 week (Ren & Dubner, 1999). Differences in sensitization may be attributable to differences in inflammatory reaction and/or oedema. There was significantly greater swelling in the plantar surface of the hind foot 3 h after injection of CFA compared with the dorsal surface (dorsal, 5.9 ± 0.2 mm, n = 7; plantar, 6.9 ± 0.2 mm, n = 6; P < 0.05) (Fig.6). The degree of swelling of the hind foot did not differ significantly after injection of 100 μg CFA, compared with 50 μg CFA injected into the dorsal surface (3 h 100 μg dorsal, 6 ± 0.2 mm, n = 5) (Fig.6).
Figure 5. Sensitization resulting from acute inflammation of the plantar hind foot is unaffected by intrathecal yohimbine.
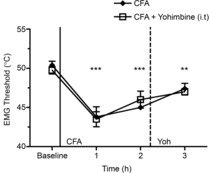
Acute complete Freund's adjuvant (CFA)-induced inflammation of the plantar hind foot resulted in a reduction in thermal withdrawal threshold that persisted for the 3 h tested [one-way repeated-measures (RM) ANOVA, P < 0.0001, F(3,4) = 19.30; Bonferroni's post-test, ***P < 0.001, **P < 0.01 compared with baseline]. This was unaffected by intrathecal yohimbine at 3 h following CFA (n = 5 CFA, n = 4 CFA + yoh).
Figure 6. Foot swelling is different following complete Freund's adjuvant (CFA) injection into the dorsal or plantar hind foot.
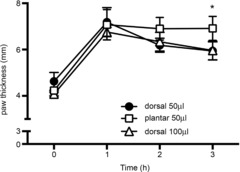
Injection of 50 μg CFA resulted in greater swelling in the plantar than the dorsal surface of the hind foot. Injection of a larger CFA concentration (100 μg) in the dorsal surface did not increase the swelling above that caused by 50 μg (one-way ANOVA, P < 0.0001, F(12,70) = 59.13; Bonferroni post hoc tests, *P < 0.05 plantar cf. both other groups; data shown as mean ± s.d.).
Effect of spinal α-2-adrenoceptor receptor blockade on the processing of thermal nociceptor inputs during hind foot inflammation
Following inflammation of hairy skin, the observation of sensitization followed by a reversal over minutes or hours suggested that descending inhibitory mechanisms may affect spinal processing in acute inflammation. Intrathecal delivery of the α-2-adrenoceptor antagonist, yohimbine (30 μg in 10 μl) (Takano & Yaksh, 1992; Green et al. 1998; Hughes et al. 2013), 2 h after CFA, when thresholds had returned (C-nociceptors) or were returning (A-nociceptors) to baseline, significantly inhibited the reversal of both A- and C-nociceptor withdrawal thresholds (3 h A-nociceptor CFA only vs. 3 h A-nociceptor CFA + yohimbine, 55 ± 1.3°C vs. 50 ± 0.9°C; P < 0.05) (Fig.7A) (3 h C-nociceptor CFA only vs. 3 h C-nociceptor CFA + yohimbine, 55 ± 1.1°C vs. 47 ± 2.3°C; P < 0.05) (Fig.7B). By contrast, yohimbine did not affect the withdrawal to thermal stimulation applied to inflamed glabrous skin (Fig.5), which was apparent at 1 h and was maintained for the 3 h studied (CFA only 3 h threshold vs. CFA + yohimbine 3 h withdrawal threshold, 47 ± 0.7°C vs. 47 ± 0.4°C (Fig.5). Intrathecal delivery of the same volume of vehicle did not affect withdrawal thresholds in either experiment (n = 3 for both experiments; data not shown).
Figure 7. Blockade of spinal α-2 adrenoceptors reveals a rapid inhibitory control on withdrawal reflexes to A- and C-nociceptor activation during acute inflammation.
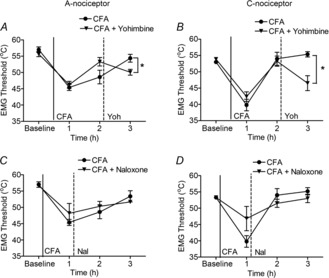
A, the loss of acute sensitization to A-nociceptor stimulation 3 h after complete Freund's adjuvant (CFA) injection was partially reversed by the intrathecal injection of the noradrenergic α-2 receptor antagonist yohimbine [Mann–Whitney U test, *P < 0.05; n = 7 CFA (3 h), n = 5 yoh]. B, the loss of acute sensitization to C-nociceptor stimulation 3 h after CFA injection was reversed by yohimbine [Mann–Whitney U test, *P < 0.05; n = 8 CFA (3 h), n = 5 yoh]. C, D, systemic administration of the pan-opioid antagonist, naloxone, had no effect on either A-nociceptor evoked withdrawals (CFA, n = 5; CFA + nal, n = 6) (C) or C-nociceptor evoked withdrawals (CFA, n = 5; CFA + nal, n = 6) (D).
Spinal and supraspinal opioidergic systems are known to have robust inhibitory effects on spinal nociceptive processing during inflammation (Stanfa & Dickenson, 1995; Przewłocki & Przewłocka, 2001). We therefore also determined the contribution of opioidergic systems to the degree of hyperalgesia in acute hind foot CFA inflammation. Systemic delivery of the pan-opioid receptor antagonist naloxone (3 mg kg−1) (Stanfa & Dickenson, 1995) had no effect on either A- or C-nociceptor withdrawal thresholds in hairy skin at either 2 h or 3 h following CFA (Fig.7C and D). It has been previously shown that naloxone has no effect on withdrawal latencies to thermal stimuli at 4 h following plantar inflammation (Hylden et al. 1991; Tsuruoka & Willis, 1996).
Discussion
Two key observations arise from these data: (i) there is a differential descending noradrenergic inhibitory control on different skin types in acute inflammation, and (ii) there is a greater descending inhibitory control of C- than A-nociceptor evoked reflexes from hairy skin.
Subcutaneous injection of CFA is a well characterized and widely utilized cutaneous inflammatory model, primarily used to study inflammatory hypersensitivity in glabrous (plantar) skin (Iadarola et al. 1988; Ren & Dubner, 1999). The oedema generated in glabrous or hairy skin is not equivalent for the same dose of CFA (Cook & Moore, 2006), but as CFA produces a dose-dependent inflammatory response (Donaldson et al. 1993) that should be equivalent at different sites, inflammation of hairy and glabrous skin might be predicted to induce equivalent primary hyperalgesia. The literature reports that CFA injection results in a robust primary mechanical and, usually, following plantar injection, thermal behavioural hypersensitivity to stimulation from as early as 1 h, which reportedly lasts for weeks (Iadarola et al. 1988; Ren & Dubner, 1999; Terayama et al. 2002; Soignier et al. 2011). Plantar inflammation also results in mechanical hypersensitivity (Ren & Dubner, 1999; Cook & Moore, 2006; Soignier et al. 2011). By contrast, dorsal (hairy) hind foot inflammation results in no change in the thermal reflex withdrawal response, despite the thermal sensitization of single peripheral nociceptors in the same model (Dunham et al. 2008; Koerber et al. 2010). CFA-induced inflammation results in robust longlasting peripheral nociceptor thermal sensitization in rats, guinea pigs and primates (Kocher et al. 1987; Davis et al. 1993; Andrew & Greenspan, 1999; Djouhri & Lawson, 1999; Djouhri et al. 2001; Dunham et al. 2008; Koerber et al. 2010), irrespective of whether hairy or glabrous skin is inflamed, which is inconsistent with the behavioural data. We therefore determined whether the observed lack of thermal behavioural responses in acute inflammation might be attributable to descending inhibitory control of nociceptive processing from inflamed hairy skin sites. The observation that plantar inflammation produces greater swelling, but little obvious descending inhibition, whereas dorsal inflammation produces less swelling but more profound inhibition with increasing severity of inflammation suggests that it is the overall degree of inflammation, rather than just the oedema, that engages descending control systems. This is consistent with previous findings, in which much higher CFA doses produced acute thermal analgesia (i.e. less nociception than control) in hairy but not glabrous skin (Cook & Moore, 2006). Therefore, differences in inflammatory oedema in different sites may not accurately predict nociceptive responses as this aspect of inflammation may more accurately reflect local tissue compliance (Reed & Rubin, 2010) rather than nociceptive input.
Processing of noxious inputs is known to be subject to both descending inhibitory and facilitatory controls (Millan, 2002; Vanegas & Schaible, 2004). Primary inflammatory hyperalgesia is widely accepted as being dominated by descending inhibitory controls, which are both rapidly activated and longlasting. These are hypothesized to protect against spinal hyperexcitability following inflammation by limiting mechanisms of central sensitization (Ren & Dubner, 1996; Vanegas & Schaible, 2004). However, they are not usually reported to completely obliterate the nociceptive sensitivity resulting from the insult (Tsuruoka & Willis, 1996; Tsuruoka et al. 2003; Vanegas & Schaible, 2004). This contrasts with our findings, in which thermal hyperalgesia in hairy skin was more short-lived, particularly so when inflammation was more severe (100 μg CFA dose).
Descending fibres from areas such as the LC and RVM exert profound modulatory influences on spinal nociceptive processing (Fields et al. 1991; Tsuruoka & Willis, 1996; Miki et al. 2002; Millan, 2002; Tsuruoka et al. 2003) through monoaminergic systems (Pertovaara, 2006; Yoshimura & Furue, 2006). Descending monoaminergic systems, particularly noradrenaline acting through spinal α-2 receptors, are reported to modulate the development of inflammatory hyperalgesia (Tsuruoka & Willis, 1996; Tsuruoka et al. 2003; Pertovaara, 2006). Our findings confirm this for hairy cutaneous tissue and additionally indicate that, at acute time-points, yohimbine blockade modulates thermal inflammatory sensitivity differentially in hairy and glabrous skin.
It has been proposed that the descending noradrenergic systems form a stimulus-driven negative feedback circuit that impinges onto spinal nociceptive processing and so regulates the onward flow of ascending nociceptive information (Pertovaara, 2006, 2013). Our finding of a greater inhibition in more severe inflammation in hairy skin would support this. By contrast, in glabrous skin hypersensitivity persists (>4 h) (Tsuruoka & Willis, 1996) and at acute time-points (<3 h) we find little evidence of either monoaminergic or opioidergic inhibition, consistent with previous findings (Hylden et al. 1991; Tsuruoka & Willis, 1996).
Although yohimbine has high affinity for α-2 receptors and is commonly used as a specific α-2-adrenoceptor antagonist, it has moderate affinity at α-1-adrenoceptors, 5-HT1A, 5-HT1B and dopamine D2 receptors [Ki determinations generously provided by the National Institute of Mental Health's Psychoactive Drug Screening Program (http://pdsp.med.unc.edu/pdsp.php)]. As a result of the latter effects, systemic yohimbine can decrease 5-HT and increase dopamine and noradrenaline levels in rat CNS, probably through blockade of autoreceptors (Paalzow & Paalzow, 1983; Millan et al. 2000). In inflammation, spinal 5-HT1A receptors both enhance (Zhang et al. 2001; Wang et al. 2003) and inhibit (Liu et al. 2002; Yu et al. 2011; Horiguchi et al. 2013) acute inflammatory nociception; known descending 5-HT3 receptor-mediated facilitatory pathways do not seem to contribute to inflammatory nociception (Asante & Dickenson, 2010). There are no published data on contributions of spinal D2 receptors to acute inflammatory nociception. Although this concentration of yohimbine administered intrathecally has been widely interpreted as exerting actions primarily at α-2 adrenoceptors (Ossipov et al. 1989; Takano & Yaksh, 1992; Green et al. 1998; De Felice et al. 2011; Hughes et al. 2013), we cannot exclude an additional contribution of modulation of α-1-adreno or 5-HT receptors at the spinal level to the observed effects of yohimbine. Actions of yohimbine on 5-HT1A receptors would be consistent with a concurrent antinociceptive effect of 5-HT in this model (Liu et al. 2002; Yu et al. 2011; Horiguchi et al. 2013).
The nocifensive flexor reflex is thought to provide an objective measure of noxious threshold and is the most commonly used in pain studies in both humans and animals (Wiesenfeld-Hallin, 1995; Sandrini et al. 2005). In animals the nocifensive flexor reflex typically involves recording EMG activity from the biceps femoris evoked by stimulation of the hind limb (Wiesenfeld-Hallin, 1995). α-Motor neurons serving the biceps femoris have receptive fields on both the dorsal and plantar surfaces (Cook & Woolf, 1985) and thus the effects of drugs on reflexes evoked from both foot surfaces can be directly compared and contrasted. Thus, although the musculotopic organization of reflexes may have meant that recording from different muscular sites may have yielded slightly different results (Schouenborg et al. 1994; Harris & Clarke, 2002), these may not have been directly comparable for stimulation of different sites on the hind limb. In addition, as α-2-adrenoceptor agonists are analgesic (Pertovaara, 2006) and presumably inhibit the sensory afferent arm of the withdrawal reflex, it could be hypothesized that the result of yohimbine blockade would affect, to a greater or lesser extent, all muscle groups involved in noxious withdrawal reflexes. This is supported by the behavioural data.
A differential descending inhibitory control on glabrous versus hairy skin may relate to the functional importance of the footpad/glabrous skin. The plantar surface forms the main exploratory hind foot surface in rodents, providing important sensory and discriminative information about the environment (Boada et al. 2013). Pain provides a critical protective mechanism in which nociceptive sensitization, including increased reflex sensitivity, serves to protect injured areas that might regularly come into contact with physical stimuli (Schouenborg et al. 1994) and it has been shown that load-bearing parts of the foot have special significance in generating reflex sensitization (Clarke & Harris, 2004). However, effective locomotion is essential to survival, being central to feeding and escape behaviours, and therefore the positive impact of nociceptive reflex hypersensitivity and its protective function must be traded against its negative impact on locomotion. Thus peripheral domains that rarely come into contact with nociceptive stimuli (dorsal hind foot) may have a reduced capacity to produce reflex sensitization following inflammation.
The differences in descending inhibition of spinal processing of afferent input from different peripheral domains may also represent a difference in both innervation and the effects of inflammation on innervating neuronal properties. The inflammatory sensitization of unmyelinated afferents differs in glabrous versus hairy skin in both the rat and the primate (Campbell & Meyer, 1983; Kocher et al. 1987; Andrew & Greenspan, 1999; Dunham et al. 2008) in that peripheral thermal sensitization occurs in C-nociceptors innervating hairy skin (Campbell & Meyer, 1983; Davis et al. 1993; Dunham et al. 2008; Koerber et al. 2010), but not in glabrous skin (Meyer & Campbell, 1981; Campbell & Meyer, 1983; Andrew & Greenspan, 1999; Du et al. 2006), in which C-nociceptors may become desensitized instead (Campbell & Meyer, 1983; Andrew & Greenspan, 1999). C-nociceptors play critical roles in driving mechanisms of central sensitization and of descending controls from supraspinal sites (Woolf & Wall, 1986; Sivilotti et al. 1993; Suzuki et al. 2002; Ikeda et al. 2003; Mantyh & Hunt, 2004; You et al. 2010). Sensitization of C-nociceptors in inflamed hairy skin would drive ascending and therefore also descending systems to a greater extent than in glabrous skin, in which C-nociceptors do not readily sensitize, leading to the differences in inhibition observed. This is supported by the enhanced inhibition seen in a more severe inflammation, in which nociceptors are sensitized more rapidly and afferent barrage is greater (Fig.4C and D).
Previous findings from our laboratory indicate that descending inhibitory controls arising from the PAG preferentially target C-nociceptive inputs to spinal nociceptive networks (McMullan & Lumb, 2006b). Here, during acute inflammation of hairy skin, we observe a fast-acting and potent inhibition of C-nociceptor evoked withdrawals: at 2 h and 3 h following CFA the withdrawal thresholds to C-nociceptor stimulation were greater than baseline values and three of five animals displayed no evoked EMG activity before the cut-off temperature was reached. Additionally, in the two cases in which the cut-off was removed, thresholds for EMG activity were >60°C (data not shown). By contrast, at 2 h following CFA, thresholds for A-nociceptor evoked withdrawals were still significantly lower than baseline values and, at 3 h following CFA, all five animals responded to the thermal stimuli before the cut-off temperature was reached. It is likely that the effect of yohimbine on C- versus A-nociceptor evoked withdrawals failed to reach significance (data not shown) as a result of the inherent underestimation of the full effect of yohimbine on C-nociceptor withdrawal thresholds caused by the imposed temperature cut-off (55°C). Descending inhibitory systems have been shown to preferentially target thermal spinal nociceptive processing in both normal and inflamed rats (Kauppila et al. 1998; Howorth et al. 2009), which is consistent with our observations. Additionally, as noxious mechanical stimuli are thought to be conveyed by A-fibre nociceptors (Ziegler et al. 1999; Magerl et al. 2001), an alternative interpretation of these findings is that there is a preferential inhibition of spinal nociceptive processing of C- versus A-nociceptor inputs.
There may be a possible evolutionary advantage of greater inhibitory control on C- compared with A-nociceptor evoked reflexes, which may relate to the different functions of these afferents. In humans, rapidly conducting A-nociceptors convey sharp, well-localized, painful sensations (Magerl et al. 2001), information which is encoded with high fidelity by spinal neurons (in the rat) (McMullan & Lumb, 2006a). By contrast, slowly conducting C-nociceptors convey dull and diffuse pain (Ziegler et al. 1999; Magerl et al. 2001) encoded with low fidelity by spinal neurons in rats (McMullan & Lumb, 2006a). Thus A-nociceptors are hypothesized to convey more detailed information relating to the protective function of pain (i.e. localization and magnitude assessment). A greater acute inhibition of C-nociceptor inputs may serve to filter extraneous C-nociceptive information and limit saturation in the reflex pathway (Tsuruoka et al. 2012) while concurrently preserving A-nociceptive information, which is essential to the protective function of reflex withdrawals. Thus differential inhibitory control of inputs from body areas with different functions and from different nociceptor types would be hypothesized to limit central sensitization and protect against spinal hyperexcitability following inflammation, whilst maintaining adequate locomotor and protective nociceptive function to enable healing and survival.
Acknowledgments
The authors would like to thank Professor Bruce Matthews, School of Physiology and Pharmacology, University of Bristol, for assistance with the design and build of the mechanical pincher, and additionally Dr Louise Hickey and Sam Hughes, School of Physiology and Pharmacology, University of Bristol, for their helpful discussions and input on technical issues.
Glossary
- CFA
complete Freund's adjuvant
- LC
locus coeruleus
- PAG
periaqueductal grey
- RVM
rostroventral medulla
Key points
Acute inflammation engages various descending control systems in the brain that alter the resulting inflammatory pain, usually by inhibiting it.
In this study we looked at the differences in inhibition of acute (up to 3 h) inflammatory pain from smooth (glabrous) and hairy skin in the rat hind foot.
In hairy skin, inflammatory pain is rapidly inhibited by descending systems that release noradrenaline, but not opiates, into the spinal cord.
In glabrous skin, neither descending noradrenergic nor opioidergic controls affect inflammatory pain.
These results tell us that the controls on the spinal processing of cutaneous inflammatory pain differ according to the skin type affected.
Additional information
Competing interests
None declared.
Author contributions
Experiments were performed in laboratories in the School of Physiology and Pharmacology, University of Bristol. R.A.R.D., B.M.L. and L.F.D. contributed to the experimental design, and to data analysis and interpretation. R.P.H. designed and built the mechanical stimulator. R.A.R.D. contributed to data collection. R.A.R.D., B.M.L. and L.F.D. wrote the paper and all authors approved the final manuscript for submission.
Funding
This work was funded by the Medical Research Council (MRC) through a Doctoral Training Partnership studentship to R.A.R.D., project grant G0801381 to B.M.L. and a Biotechnology and Biological Sciences Research Council/MRC/British Pharmacological Society Strategic Skills Award to L.F.D. and B.M.L.
References
- Andrew D, Greenspan J. Mechanical and heat sensitization of cutaneous nociceptors after peripheral inflammation in the rat. J Neurophysiol. 1999;82:2649–2656. doi: 10.1152/jn.1999.82.5.2649. [DOI] [PubMed] [Google Scholar]
- Asante CO, Dickenson AH. Descending serotonergic facilitation mediated by spinal 5-HT3 receptors engages spinal rapamycin-sensitive pathways in the rat. Neurosci Lett. 2010;484:108–112. doi: 10.1016/j.neulet.2010.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajic D, Proudfit HK. Projections of neurons in the periaqueductal grey to pontine and medullary catecholamine cell groups involved in the modulation of nociception. J Comp Neurol. 1999;405:359–379. [PubMed] [Google Scholar]
- Blake DT, Byl NN, Merzenich MM. Representation of the hand in the cerebral cortex. Behav Brain Res. 2002;135:179–184. doi: 10.1016/s0166-4328(02)00163-8. [DOI] [PubMed] [Google Scholar]
- Boada MD, Houle TT, Eisenach JC, Ririe DG. Differing neurophysiologic mechanosensory input from glabrous and hairy skin in juvenile rats differing neurophysiologic mechanosensory input from glabrous and hairy skin in juvenile rats. J Neurophysiol. 2013;104:3568–3575. doi: 10.1152/jn.00415.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JN, Meyer RA. Sensitization of unmyelinated nociceptive afferents in monkey varies with skin type. J Neurophysiol. 1983;49:98–110. doi: 10.1152/jn.1983.49.1.98. [DOI] [PubMed] [Google Scholar]
- Chillingworth NL, Morham SG, Donaldson LF. Sex differences in inflammation and inflammatory pain in cyclooxygenase-deficient mice. Am J Physiol Regul Integr Comp Physiol. 2006;291:R327–R334. doi: 10.1152/ajpregu.00901.2005. [DOI] [PubMed] [Google Scholar]
- Clarke RW, Harris J. The organization of motor responses to noxious stimuli. Brain Res Brain Res Rev. 2004;46:163–172. doi: 10.1016/j.brainresrev.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Cook AJ, Woolf CJ. Cutaneous receptive field and morphological properties of hamstring flexor α-motorneurones in the rat. J Physiol. 1985;364:249–263. doi: 10.1113/jphysiol.1985.sp015742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook CD, Moore KI. Effects of sex, hind limb injection site and stimulus modality on nociceptive sensitivity in arthritic rats. Physiol Behav. 2006;87:552–562. doi: 10.1016/j.physbeh.2005.12.005. [DOI] [PubMed] [Google Scholar]
- Davis KD, Meyer RA, Campbell JN. Chemosensitivity and sensitization of nociceptive afferents that innervate the hairy skin of monkey. J Neurophysiol. 1993;69:1071–1081. doi: 10.1152/jn.1993.69.4.1071. [DOI] [PubMed] [Google Scholar]
- DeFelice M, Sanoja R, Wang R, Vera-Portocarrero L, Oyarzo J, King T, Ossipov MH, Vanderah TW, Lai J, Dussor GO, Fields HL, Price TJ, Porreca F. Engagement of descending inhibition from the rostral ventromedial medulla protects against chronic neuropathic pain. Pain. 2011;152:2701–2709. doi: 10.1016/j.pain.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djouhri L, Dawbarn D, Robertson A, Newton R, Lawson SN. Time course and nerve growth factor dependence of inflammation-induced alterations in electrophysiological membrane properties in nociceptive primary afferent neurons. J Neurosci. 2001;21:8722–8733. doi: 10.1523/JNEUROSCI.21-22-08722.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djouhri L, Lawson SN. Changes in somatic action potential shape in guinea-pig nociceptive primary afferent neurones during inflammation in vivo. J Physiol. 1999;520:565–576. doi: 10.1111/j.1469-7793.1999.t01-1-00565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dogrul A, Ossipov MH, Porreca F. Differential mediation of descending pain facilitation and inhibition by spinal 5HT3 and 5HT7 receptors. Brain Res. 2009;1280:52–59. doi: 10.1016/j.brainres.2009.05.001. [DOI] [PubMed] [Google Scholar]
- Donaldson LF, Seckl JR, McQueen DS. A discrete adjuvant-induced monoarthritis in the rat: effects of adjuvant dose. J Neurosci Methods. 1993;49:5–10. doi: 10.1016/0165-0270(93)90103-x. [DOI] [PubMed] [Google Scholar]
- Du J, Zhou S, Carlton SM. Kainate-induced excitation and sensitization of nociceptors in normal and inflamed rat glabrous skin. Neuroscience. 2006;137:999–1013. doi: 10.1016/j.neuroscience.2005.10.008. [DOI] [PubMed] [Google Scholar]
- Dunham JP, Kelly S, Donaldson LF. Inflammation reduces mechanical thresholds in a population of transient receptor potential channel A1-expressing nociceptors in the rat. Eur J Neurosci. 2008;27:3151–3160. doi: 10.1111/j.1460-9568.2008.06256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fields HL, Heinricher MM, Mason P. Neurotransmitters in nociceptive modulatory circuits. Annu Rev Neurosci. 1991;14:219–245. doi: 10.1146/annurev.ne.14.030191.001251. [DOI] [PubMed] [Google Scholar]
- Green GM, Lyons L, Dickenson AH. α2-adrenoceptor antagonists enhance responses of dorsal horn neurones to formalin induced inflammation. Eur J Pharmacol. 1998;347:201–204. doi: 10.1016/s0014-2999(98)00217-9. [DOI] [PubMed] [Google Scholar]
- Guan Y, Terayama R, Dubner R, Ren K. Plasticity in excitatory amino acid receptor-mediated descending pain modulation after inflammation. J Pharmacol Exp Ther. 2002;300:513–520. doi: 10.1124/jpet.300.2.513. [DOI] [PubMed] [Google Scholar]
- Harris J, Clarke RW. Organization of sensitization of hind limb withdrawal reflexes from acute noxious stimuli in the rabbit. J Physiol. 2002;546:251–265. doi: 10.1113/jphysiol.2002.025023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horiguchi N, Ago Y, Hasebe S, Higashino K, Asada K, Kita Y, Takuma K, Matsuda T. Isolation rearing reduces mechanical allodynia in a mouse model of chronic inflammatory pain. Pharmacol Biochem Behav. 2013;113:46–52. doi: 10.1016/j.pbb.2013.10.017. [DOI] [PubMed] [Google Scholar]
- Howorth PW, Thornton SR, O'Brien V, Smith WD, Nikiforova N, Teschemacher AG, Pickering AE. Retrograde viral vector-mediated inhibition of pontospinal noradrenergic neurons causes hyperalgesia in rats. J Neurosci. 2009;29:12855–12864. doi: 10.1523/JNEUROSCI.1699-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes SW, Hickey L, Hulse RP, Lumb BM, Pickering AE. Endogenous analgesic action of the pontospinal noradrenergic system spatially restricts and temporally delays the progression of neuropathic pain following tibial nerve injury. Pain. 2013;154:1680–1690. doi: 10.1016/j.pain.2013.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hylden J, Thomas D, Iadarola M, Nahin R, Dubner R. Spinal opioid analgesic effects are enhanced in a model of unilateral inflammation/hyperalgesia: possible involvement of noradrenergic mechanisms. Eur J Pharmacol. 1991;194:135–143. doi: 10.1016/0014-2999(91)90097-a. [DOI] [PubMed] [Google Scholar]
- Iadarola M, Brady L, Draisci G, Dubner R. Enhancement of dynorphin gene expression in spinal cord following experimental inflammation: stimulus specificity, behavioral parameters and opioid receptor binding. Pain. 1988;35:313–326. doi: 10.1016/0304-3959(88)90141-8. [DOI] [PubMed] [Google Scholar]
- Ikeda H, Heinke B, Ruscheweyh R, Sandkühler J. Synaptic plasticity in spinal lamina I projection neurons that mediate hyperalgesia. Science. 2003;299:1237–1240. doi: 10.1126/science.1080659. [DOI] [PubMed] [Google Scholar]
- Jeong H-J, Mitchell VA, Vaughan CW. Role of 5-HT1 receptor subtypes in the modulation of pain and synaptic transmission in rat spinal superficial dorsal horn. Br J Pharmacol. 2012;165:1956–1965. doi: 10.1111/j.1476-5381.2011.01685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauppila T, Kontinen VK, Pertovaara A. Influence of spinalization on spinal withdrawal reflex responses varies depending on the submodality of the test stimulus and the experimental pathophysiological condition in the rat. Brain Res. 1998;797:234–242. doi: 10.1016/s0006-8993(98)00379-5. [DOI] [PubMed] [Google Scholar]
- Kocher L, Anton F, Reeh P, Handwerker H. The effect of carrageenan-induced inflammation on the sensitivity of unmyelinated skin nociceptors in the rat. Pain. 1987;29:363–373. doi: 10.1016/0304-3959(87)90051-0. [DOI] [PubMed] [Google Scholar]
- Koerber HR, McIlwrath SL, Lawson JJ, Malin SA, Anderson CE, Jankowski MP, Davis BM. Cutaneous C-polymodal fibers lacking TRPV1 are sensitized to heat following inflammation, but fail to drive heat hyperalgesia in the absence of TPV1 containing C-heat fibers. Mol Pain. 2010;6:58. doi: 10.1186/1744-8069-6-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok CH, Devonshire IM, Bennett AJ, Hathway GJ. Postnatal maturation of endogenous opioid system within the periaqueductal grey and spinal dorsal horn of the rat. Pain. 2014;155:168–178. doi: 10.1016/j.pain.2013.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10:895–926. doi: 10.1016/j.jpain.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leem JW, Willis WD, Chung JM. Cutaneous sensory receptors in the rat foot. J Neurophysiol. 1993;69:1684–1699. doi: 10.1152/jn.1993.69.5.1684. [DOI] [PubMed] [Google Scholar]
- Leith JL, Wilson AW, Donaldson LF, Lumb BM. Cyclooxygenase-1-derived prostaglandins in the periaqueductal grey differentially control C- versus A-fibre-evoked spinal nociception. J Neurosci. 2007;27:11296–11305. doi: 10.1523/JNEUROSCI.2586-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z-Y, Zhuang D-B, Lunderberg T, Yu L-C. Involvement of 5-hydroxytryptamine1A receptors in the descending anti-nociceptive pathway from periaqueductal grey to the spinal dorsal horn in intact rats, rats with nerve injury and rats with inflammation. Neuroscience. 2002;112:399–407. doi: 10.1016/s0306-4522(02)00038-6. [DOI] [PubMed] [Google Scholar]
- Lynn B, Carpenter S. Primary afferent units from the hairy skin of the rat hind limb. Brain Res. 1982;238:29–43. doi: 10.1016/0006-8993(82)90768-5. [DOI] [PubMed] [Google Scholar]
- Magerl W, Fuchs PN, Meyer RA, Treede RD. Roles of capsaicin-insensitive nociceptors in cutaneous pain and secondary hyperalgesia. Brain. 2001;124:1754–1764. doi: 10.1093/brain/124.9.1754. [DOI] [PubMed] [Google Scholar]
- Mantyh PW. Connections of midbrain periaqueductal grey in the monkey. II. Descending efferent projections. J Neurophysiol. 1983;49:582–594. doi: 10.1152/jn.1983.49.3.582. [DOI] [PubMed] [Google Scholar]
- Mantyh PW, Hunt SP. Setting the tone: superficial dorsal horn projection neurons regulate pain sensitivity. Trends Neurosci. 2004;27:582–584. doi: 10.1016/j.tins.2004.07.007. [DOI] [PubMed] [Google Scholar]
- McMullan S, Lumb BM. Spinal dorsal horn neuronal responses to myelinated versus unmyelinated heat nociceptors and their modulation by activation of the periaqueductal grey in the rat. J Physiol. 2006a;576:547–556. doi: 10.1113/jphysiol.2006.117754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMullan S, Lumb BM. Midbrain control of spinal nociception discriminates between responses evoked by myelinated and unmyelinated heat nociceptors in the rat. Pain. 2006b;124:59–68. doi: 10.1016/j.pain.2006.03.015. [DOI] [PubMed] [Google Scholar]
- McMullan S, Simpson DA, Lumb BM. A reliable method for the preferential activation of C- or A-fibre heat nociceptors. J Neurosci Methods. 2004;138:133–139. doi: 10.1016/j.jneumeth.2004.03.020. [DOI] [PubMed] [Google Scholar]
- Meyer RA, Campbell JN. Myelinated nociceptive afferents account for the hyperalgesia that follows a burn to the hand. Science. 1981;213:1527–1529. doi: 10.1126/science.7280675. [DOI] [PubMed] [Google Scholar]
- Meyer RA, Ringkamp M, Campbell JN, Raja SN. Neural mechanisms of hyperalgesia after tissue injury. Johns Hopkins APL Tech Dig. 2005;26:56–66. [Google Scholar]
- Miki K, Zhou QQ, Guo W, Guan Y, Terayama R, Dubner R, Ren K. Changes in gene expression and neuronal phenotype in brain stem pain modulatory circuitry after inflammation. J Neurophysiol. 2002;87:750–760. doi: 10.1152/jn.00534.2001. [DOI] [PubMed] [Google Scholar]
- Millan MJ. Descending control of pain. Prog Neurobiol. 2002;66:355–474. doi: 10.1016/s0301-0082(02)00009-6. [DOI] [PubMed] [Google Scholar]
- Millan MJ, Newman-Tancredi A, Audinot V, Cussac D, Lejeune F, Nicolas J, Coge F, Galizzi J, Boutin J, Rivet J, Dekeyne A, Gobert A. Agonist and antagonist actions of yohimbine as compared to fluparoxan at α2-adrenergic receptors (ARs), serotonin (5-HT1A), 5-HT1B, 5-HT1D and dopamine D2 and D3 receptors. Significance for the modulation of frontocortical monoaminergic transmission and depressive states. Synapse. 2000;35:79–95. doi: 10.1002/(SICI)1098-2396(200002)35:2<79::AID-SYN1>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- Oliva P, Berrino L, de Novellis V, Palazzo E, Marabese I, Siniscalco D, Scafuro M, Mariani L, Rossi F, Maione S. Role of periaqueductal grey prostaglandin receptors in formalin-induced hyperalgesia. Eur J Pharmacol. 2006;530:40–47. doi: 10.1016/j.ejphar.2005.11.025. [DOI] [PubMed] [Google Scholar]
- Ossipov MH, Dussor GO, Porreca F. Central modulation of pain. J Clin Invest. 2010;120:3779–3787. doi: 10.1172/JCI43766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ossipov MH, Suarez LJ, Spaulding TC. Antinociceptive interactions between α, -adrenergic and opiate agonists at the spinal level in rodents. Anesth Analg. 1989;68:194–200. [PubMed] [Google Scholar]
- Paalzow G, Paalzow L. Yohimbine both increases and decreases nociceptive thresholds in rats: evaluation of the dose–response relationship. Naunyn Schmiedebergs Arch Pharmacol. 1983;322:193–197. doi: 10.1007/BF00500764. [DOI] [PubMed] [Google Scholar]
- Palazzo E, Guida F, Gatta L, Luongo L, Boccella S, Bellini G, Marabese I, de Novellis V, Rossi F, Maione S. EP1 receptor within the ventrolateral periaqueductal grey controls thermonociception and rostral ventromedial medulla cell activity in healthy and neuropathic rat. Mol Pain. 2011;7:82. doi: 10.1186/1744-8069-7-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pertovaara A. Noradrenergic pain modulation. Prog Neurobiol. 2006;80:53–83. doi: 10.1016/j.pneurobio.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Pertovaara A. The noradrenergic pain regulation system: a potential target for pain therapy. Eur J Pharmacol. 2013;716:2–7. doi: 10.1016/j.ejphar.2013.01.067. [DOI] [PubMed] [Google Scholar]
- Provitera V, Nolano M, Pagano A, Caporaso G, Stancanelli A, Santoro L. Myelinated nerve endings in human skin. Muscle Nerve. 2007;35:767–775. doi: 10.1002/mus.20771. [DOI] [PubMed] [Google Scholar]
- Przewłocki R, Przewłocka B. Opioids in chronic pain. Eur J Pharmacol. 2001;429:79–91. doi: 10.1016/s0014-2999(01)01308-5. [DOI] [PubMed] [Google Scholar]
- Reed RK, Rubin K. Transcapillary exchange: role and importance of the interstitial fluid pressure and the extracellular matrix. Cardiovasc Res. 2010;87:211–217. doi: 10.1093/cvr/cvq143. [DOI] [PubMed] [Google Scholar]
- Ren K, Dubner R. Enhanced descending modulation of nociception in rats with persistent hind limb inflammation. J Neurophysiol. 1996;76:3025–3037. doi: 10.1152/jn.1996.76.5.3025. [DOI] [PubMed] [Google Scholar]
- Ren K, Dubner R. Inflammatory models of pain and hyperalgesia. ILAR J. 1999;40:111–118. doi: 10.1093/ilar.40.3.111. [DOI] [PubMed] [Google Scholar]
- Sandrini G, Serrao M, Rossi P, Romaniello A, Cruccu G, Willer JC. The lower limb flexion reflex in humans. Prog Neurobiol. 2005;77:353–395. doi: 10.1016/j.pneurobio.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Schouenborg J, Weng H, Holmberg H. Modular organization of spinal nociceptive reflexes: a new hypothesis. Physiology. 1994;9:261–265. [Google Scholar]
- Sivilotti LG, Thompson SWN, Woolf CJ. Rate of rise of the cumulative depolarization evoked by repetitive stimulation of small-caliber afferents is a predictor of action potential windup in rat spinal neurons in vitro. J Neurophysiol. 1993;69:1621–1631. doi: 10.1152/jn.1993.69.5.1621. [DOI] [PubMed] [Google Scholar]
- Soignier RD, Taylor BK, Baiamonte BA, Lee FA, Paul D, Gould HJ. Measurement of CFA-induced hyperalgesia and morphine-induced analgesia in rats: dorsal vs. plantar mechanical stimulation of the hind limb. Pain Med. 2011;12:451–458. doi: 10.1111/j.1526-4637.2011.01066.x. [DOI] [PubMed] [Google Scholar]
- Stanfa L, Dickenson A. Spinal opioid systems in inflammation. Inflamm Res. 1995;44:231–241. doi: 10.1007/BF01782974. [DOI] [PubMed] [Google Scholar]
- Størkson RV, Kjørsvik A, Tjølsen A, Hole K. Lumbar catheterization of the spinal subarachnoid space in the rat. J Neurosci Methods. 1996;65:167–172. doi: 10.1016/0165-0270(95)00164-6. [DOI] [PubMed] [Google Scholar]
- Suzuki R, Morcuende S, Webber M, Hunt SP, Dickenson AH. Superficial NK1-expressing neurons control spinal excitability through activation of descending pathways. Nat Neurosci. 2002;5:1319–1326. doi: 10.1038/nn966. [DOI] [PubMed] [Google Scholar]
- Takano Y, Yaksh TL. Characterization of the pharmacology of intrathecally administered α-2 agonists and antagonists in rats. J Pharmacol Exp Ther. 1992;261:764–772. [PubMed] [Google Scholar]
- Terayama R, Dubner R, Ren K. The roles of NMDA receptor activation and nucleus reticularis gigantocellularis in the time-dependent changes in descending inhibition after inflammation. Pain. 2002;97:171–181. doi: 10.1016/s0304-3959(02)00017-9. [DOI] [PubMed] [Google Scholar]
- Tsuruoka M, Matsutani K, Inoue T. Coeruleospinal inhibition of nociceptive processing in the dorsal horn during unilateral hind limb inflammation in the rat. Pain. 2003;104:353–361. doi: 10.1016/s0304-3959(03)00042-3. [DOI] [PubMed] [Google Scholar]
- Tsuruoka M, Tamaki J, Maeda M, Hayashi B, Inoue T. Biological implications of coeruleospinal inhibition of nociceptive processing in the spinal cord. Front Integr Neurosci. 2012;6:87. doi: 10.3389/fnint.2012.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuruoka M, Willis WD. Descending modulation from the region of the locus coeruleus on nociceptive sensitivity in a rat model of inflammatory hyperalgesia. Brain Res. 1996;743:86–92. doi: 10.1016/s0006-8993(96)01025-6. [DOI] [PubMed] [Google Scholar]
- Tyce GM, Yaksht TL. Monoamine release from cat spinal cord by somatic stimuli: an intrinsic modulatory system. J Physiol. 1981;314:513–529. doi: 10.1113/jphysiol.1981.sp013722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanegas H, Schaible HG. Descending control of persistent pain: inhibitory or facilitatory? Brain Res Brain Res Rev. 2004;46:295–309. doi: 10.1016/j.brainresrev.2004.07.004. [DOI] [PubMed] [Google Scholar]
- Vasquez E, Vanegas H. The antinociceptive effect of PAG-microinjected dipyrone in rats is mediated by endogenous opioids of the rostral ventromedical medulla. Brain Res. 2000;854:249–252. doi: 10.1016/s0006-8993(99)02303-3. [DOI] [PubMed] [Google Scholar]
- Wang W, Wu S-X, Wang Y-Y, Liu X-Y, Li Y-Q. 5-Hydroxytryptamine1A receptor is involved in the bee venom induced inflammatory pain. Pain. 2003;106:135–142. doi: 10.1016/s0304-3959(03)00315-4. [DOI] [PubMed] [Google Scholar]
- Westlund KN, Bowker RM, Ziegler MG, Coulter JD. Noradrenergic projections to the spinal cord of the rat. Brain Res. 1983;263:15–31. doi: 10.1016/0006-8993(83)91196-4. [DOI] [PubMed] [Google Scholar]
- Wiesenfeld-Hallin Z. Neuropeptides and spinal cord reflexes. Prog Brain Res. 1995;104:271–280. doi: 10.1016/s0079-6123(08)61795-1. [DOI] [PubMed] [Google Scholar]
- Woolf CJ, Wall PD. Relative effectiveness of C primary afferent fibers of different origins in evoking a prolonged facilitation of the flexor reflex in the rat. J Neurosci. 1986;6:1433–1442. doi: 10.1523/JNEUROSCI.06-05-01433.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeomans DC, Proudfit HK. Nociceptive responses to high and low rates of noxious cutaneous heating are mediated by different nociceptors in the rat: electrophysiological evidence. Pain. 1996;68:141–150. doi: 10.1016/S0304-3959(96)03177-6. [DOI] [PubMed] [Google Scholar]
- Yoshimura M, Furue H. Mechanisms for the anti-nociceptive actions of the descending noradrenergic and serotonergic systems in the spinal cord. J Pharmacol Sci. 2006;101:107–117. doi: 10.1254/jphs.crj06008x. [DOI] [PubMed] [Google Scholar]
- You H-J, Lei J, Sui M-Y, Huang L, Tan Y-X, Tjølsen A, Arendt-Nielsen L. Endogenous descending modulation: spatiotemporal effect of dynamic imbalance between descending facilitation and inhibition of nociception. J Physiol. 2010;588:4177–4188. doi: 10.1113/jphysiol.2010.196923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Z, Aihui L, Jiajia X, Lixing L, Ke R, Brian B, Ming T, Zhang R-X. Involvement of spinal serotonin receptors in electroacupuncture anti-hyperalgesia in an inflammatory pain rat model. Neurochem Res. 2011;36:1785–1792. doi: 10.1007/s11064-011-0495-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Yang Z, Gao X, Wu G. The role of 5-hydroxytryptamine1A and 5-hydroxytryptamine1B receptors in modulating spinal nociceptive transmission in normal and carrageenan-injected rats. Pain. 2001;92:201–211. doi: 10.1016/s0304-3959(01)00259-7. [DOI] [PubMed] [Google Scholar]
- Ziegler EA, Magerl W, Meyer RA, Treede RD. Secondary hyperalgesia to punctate mechanical stimuli. Central sensitization to A-fibre nociceptor input. Brain. 1999;122:2245–2257. doi: 10.1093/brain/122.12.2245. [DOI] [PubMed] [Google Scholar]


