Abstract
Non-alcoholic fatty liver disease (NAFLD) is an important health problem worldwide. NAFLD encompasses a histological spectrum ranging from bland liver steatosis to severe steatohepatitis (nonalcoholic steatohepatitis, NASH) with the potential of progressing to cirrhosis and its associated morbidity and mortality. NAFLD is thought to be the hepatic manifestation of insulin resistance (or the metabolic syndrome); its prevalence is increasing worldwide in parallel with the obesity epidemic. In many developed countries, NAFLD is the most common cause of liver disease and NASH related cirrhosis is currently the third most common indication for liver transplantation. NASH related cirrhosis is anticipated to become the leading indication for liver transplantation within the next one or two decades. In this review, we discuss how liver transplantation is affected by NAFLD, specifically the following: (1) the increasing need for liver transplantation due to NASH; (2) the impact of the increasing prevalence of NAFLD in the general population on the quality of deceased and live donor livers available for transplantation; (3) the long term graft and patient outcomes after liver transplantation for NASH, and finally; and (4) the de novo occurrence of NAFLD/NASH after liver transplantation and its impact on graft and patient outcomes.
Keywords: Liver transplantation, Non-alcoholic fatty liver disease, Hepatic steatosis, Steatohepatitis, Liver cirrhosis, Metabolic syndrome, Insulin resistance, Obesity
Core tip: Nonalcoholic steatohepatitis (NASH) related cirrhosis is anticipated to become the leading indication for liver transplantation within the next one or two decades. In this review, we discuss how liver transplantation is affected by non-alcoholic fatty liver disease (NAFLD), specifically the following: the increasing need for liver transplantation due to NASH; the impact of the increasing prevalence of NAFLD in the general population on the quality of deceased and live donor livers available for transplantation; the long term graft and patients outcomes after liver transplantation for NASH, and, finally; the de novo occurrence of NAFLD/NASH after liver transplantation and its impact on graft and patient outcomes.
INTRODUCTION
The term non-alcoholic fatty liver disease (NAFLD) covers a wide spectrum of non-alcohol related, fatty liver disorders, ranging from bland steatosis (NAFL, non-alcoholic fatty liver) to severe steatohepatitis (nonalcoholic steatohepatitis, NASH) (Figure 1). NAFL is thought to be a benign condition, characterized by the presence of hepatocyte steatosis without evidence of hepatocellular injury or fibrosis. Thus, NAFL is, in general, believed not to progress to relevant liver disease. In contrast, NASH is histologically characterized by hepatocyte damage (e.g., ballooning) and inflammation with the potential to progress to fibrosis and cirrhosis, and its associated morbidity (including hepatocellular carcinoma) and mortality[1].
Figure 1.
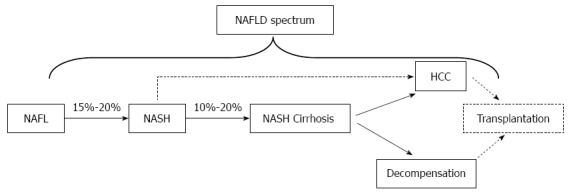
Natural history of the nonalcoholic fatty liver disease. NAFL: Nonalcoholic fatty liver; NASH: Nonalcoholic steatohepatitis; HCC: Hepatocellular carcinoma; NAFLD: Nonalcoholic fatty liver disease.
NAFLD is associated with obesity, type 2 diabetes mellitus, dyslipidemia, and the metabolic syndrome. It is presumed that the underlying common pathophysiology among these conditions is insulin resistance (IR) and that NAFLD is the hepatic manifestation of IR[1-3].
Not too surprisingly, patients with NAFLD (NAFL and NASH) have an increased mortality due to cardiovascular disease, while liver-related mortality is, in addition, increased in patients with NASH[1,4,5].
In parallel with the obesity epidemic, the prevalence of NAFLD is increasing worldwide. Thus, it is estimated that NASH will become the most common cause of advanced liver disease within the next ten to twenty years, and that NASH-related end-stage liver disease will become the most common indication for liver transplantation[6]. In addition, the increasing prevalence of NAFLD in the general population, also affects the presence of steatosis in deceased and live donor livers available for transplantation. Furthermore, liver transplantation for NASH related end-stage liver disease, does not improve factors (such as IR) predisposing to NAFLD. Thus, these recipients are at risk for recurrence of NAFLD in the graft. Finally, the prevalence of IR is high after liver transplantation for any (also non NAFLD related) indications, and these patients may develop de novo NAFLD in the graft (Figure 2). In the following, all the above aspects are reviewed in sequence.
Figure 2.
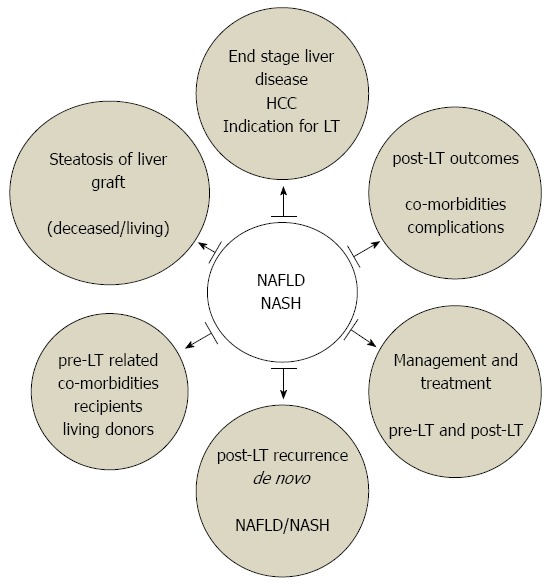
Impact of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis on liver transplantation. LT: Liver transplantation; NASH: Nonalcoholic steatohepatitis; HCC: Hepatocellular carcinoma; NAFLD: Nonalcoholic fatty liver disease.
NASH RELATED END-STAGE LIVER DISEASE AS INDICATION FOR LIVER TRANSPLANTATION
As mentioned above, the prevalence of NAFLD is increasing worldwide in parallel with the obesity epidemic. It is estimated that the prevalence of NAFLD in the adult US population is 30%-40%, while studies from other parts of the world report a prevalence ranging from 6% to 35% (median approximately 20%)[6]. Furthermore, it has been estimated that 15%-20% of patients with NAFLD have NASH. This translates into a NASH prevalence in the general population of 3%-5%. Thus, millions of people are at risk of their liver disease progressing to cirrhosis, and potentially requiring liver transplant (LT)[7]. A more recent study from the US observed an even higher prevalence of NAFLD and NASH in the general population (46% and 12%, respectively), and 2.7% in the entire cohort had established, advanced NASH related liver fibrosis, leading to an estimated > 2 million US adults with NASH related, advanced liver disease[8]. The prevalence of NAFLD increases to 70%-90% among patients in high risk populations such as the morbidly obese or diabetics[1,6,8].
According to the scientific registry of transplant recipients (SRTR) in the United States[9], NASH related cirrhosis is currently the third most common indication for liver transplantation surpassed only by hepatitis C virus (HCV), and alcoholic related cirrhosis. During the last 10 years there was a substantial increase in the proportion of transplants performed for NASH, from 1.2% in 2001 to 9.7% in 2009. In another recent analysis, using the united network for organ sharing (UNOS) database, Kemmer et al[10] reported that 7.7% of all adult LT recipients had a diagnosis of NASH-cirrhosis during the period 2007-2010. They also found a steady increase in LT for NASH related end-stage liver disease from 5.1% in 2007 to 7.5% in 2010, which held true for all age groups. Furthermore, NASH-cirrhosis was the most common non-malignant indication for LT in patients older than 65 years, whereas it was the third indication for LT in patients younger than 65 years.
Based on organ procurement and transplantation network data as of November 1, 2013, 16629 patients were registered on the waiting list for liver transplantation in the US. NASH cirrhosis was the indication for 1427 of these patients (8.5%), and cryptogenic cirrhosis (CC) for another 954 patients (5.7%). Taking into account that the majority of cryptogenic cirrhosis is considered to be secondary to unrecognized NASH[11,12], NASH related end-stage liver disease is likely the indication for liver transplantation in more than 10% of the patients currently listed in the United States (Table 1).
Table 1.
Nonalcoholic steatohepatitis related cirrhosis as an indication for liver tranplantation
| Ref. | Database | Years | NASH Cirrhosis Tx | NASH Cirrhosis waiting list |
| Charlton et al[9] | SRTR | 2001-2009 | Increased | |
| 1.2%→9.7% | ||||
| Kemmer et al[10] | UNOS | 2007-2010 | Increased | |
| 5.1%→7.5% | ||||
| http://optn.transplant.hrsa.gov | OTPN | 2013 Nov 1st | 8.5% + 5.5% for CC |
NASH: Nonalcoholic steatohepatitis; CC: Cryptogenic cirrhosis; Tx: Transplantation; SRTR: Scientific registry of transplant recipients, United States; UNOS: United network for organ sharing, United States; OTPN: Organ procurement and transplantation network, United States.
Collectively, these observations indicate that NASH is a rapidly growing, in fact, the only growing indication for liver transplantation in the United States.
IMPACT OF NAFLD ON DONOR LIVERS AVAILABLE FOR TRANSPLANTATION
The increasing prevalence of NAFLD in the general population translates directly into an increasing prevalence of NAFLD in both, potential deceased and live liver donors. Graft steatosis, in turn, affects both, the quality and the quantity of donor livers available for transplantation[13-16].
Thus, it is well known that primary graft non-function, primary graft dysfunction/delayed graft function, and, consecutively graft outcome, are associated with graft steatosis[15,16]. Upon reperfusion, steatosis induces microcirculatory and cellular changes in the liver graft potentially leading to hepatocyte necrosis. In addition, the regeneration potential of steatotic livers is impaired[17-19].
Compared to microvesicular steatosis, macrovesicular steatosis renders livers more vulnerable to injury and cell death[20]. In addition, mild steatosis (< 30%) is associated with less postoperative complications than more severe degrees of steatosis (> 30%)[13,14,21]. A recent study using UNOS data showed that the presence of more than 30% of macrovesicular steatosis was an independent risk factor for impaired 1-year graft survival[16].
The gold standard for assessing the severity and type of steatosis in a potential donor liver remains the liver biopsy. Routine imaging modalities (ultrasonography, computed tomography or magnetic resonance imaging) are not sensitive and precise enough to quantitate steatosis below 30%, and cannot discriminate between micro- and macrovesicular steatosis. Unfortunately, waiting for the result of a liver biopsy prior to decision making regarding accepting a deceased donor organ, will unduly prolong cold ischemia time and is therefore not feasible in most instances (and a frozen section is notoriously inadequate for this purpose).
For live liver donation, most programs exclude donors with macrovesicular steatosis > 10%-15%[22,23]. Noninvasive preoperative evaluation of living donors for liver steatosis has its limitations. Some programs therefore perform donor liver biopsies universally, others only in cases where steatosis > 10%-15% can otherwise not be ruled out with reasonable certainty[24]. In a recent study, Ahn et al[25] assessed histologically the degree and type of steatosis in a cohort of 492 living liver donors with negative liver US and normal aminotransferase levels. They found that although most of these patients had minimal or mild degrees of steatosis, a few had moderate microsteatosis that had not been detected by imaging.
LONG TERM OUTCOMES OF LIVER TRANSPLANTATION FOR NAFLD AND NASH
There are several recent, retrospective, single center series reporting on outcomes after liver transplantation for NASH related end-stage liver disease (Table 2). Malik et al[26] compared the outcomes in patients transplanted for NASH cirrhosis with those transplanted for other indications [primary biliary cirrhosis, primary sclerosing cholangitis (PSC), alcoholic liver disease and HCV]. Early mortality in NASH recipients was increased, but the 5-year mortality was similar to patients transplanted for other indications. Infection was the main cause of death (50%) in the NASH, but not the control group. Recipients characterized by NASH cirrhosis, older age (> 60 years), higher BMI (> 30 kg/m2), pre-LT diabetes mellitus, and hypertension had 1-year post-transplant mortality of 50%.
Table 2.
Post liver transplantation outcomes for nonalcoholic fatty liver disease, nonalcoholic steatohepatitis
| Ref. | NASH | Non-NASH | Remarks |
| Post-LT mortality | |||
| Malik et al[26] | |||
| 24 h | 4.0% | 1%-3% | Non-NASH: PBC, PSC, ALD, HCV |
| 30-d | 6.0% | 2%-5% | NASH group: Increased early mortality |
| 1-yr | 21.5% | 13%-18% | Infection: Main cause of death in NASH group (50%) |
| 3-yr | 25.5% | 16%-30% | High risk NASH group: 50% 1-yr mortality |
| 5-yr | 27.5% | 19%-35% | Older age (> 60 yr), Higher BMI (> 30 kg/m2), Pre-LT diabetes mellitus and Hypertension |
| Post-LT survival | |||
| Bhagat el al[27] | |||
| 1-yr | 82.0% | 92.0% | Non-NASH: ETOH |
| 3-yr | 79.0% | 86.0% | NASH group |
| 5-yr | 75.0% | 86.0% | Higher cardiovascular morbidity |
| 9-yr | 62.0% | 76.0% | Higher risk of acute rejection and recurrent steatohepatitis |
| Barrit et al[28] | |||
| 30-d | 81.0% | 97.0% | NASH group: Increased early mortality |
| 1-yr | 76.0% | 89.5% | All recipients: Diabetes, risk factor for increased 3-yr mortality |
| 3-yr | 76.0% | 83.5% | |
| Afzali et al[29] | |||
| 1-yr | 87.6% | Non-NASH: Any other indication | |
| 3-yr | 82.2% | Variable | NASH group: Excellent survival, similar to PSC and HBV |
| 5-yr | 76.7% | ||
| Singal et al[30] | |||
| 1-yr | 89.0% | Non-NASH: PSC, PBC, ALD, HCV, HBV, CC, HCC | |
| 3-yr | 85.5% | Variable | NASH group: Excellent survival, 3-, 5-yr survival best of all |
| 5-yr | 84.0% | ||
| 10-yr | 84.0% | ||
Post-LT: Post liver transplantation; NAFLD: Nonalcoholic fatty liver disease; NASH: Nonalcoholic steatohepatitis; PSC: Primary sclerosing cholangitis; PBC: Primary biliary cirrhosis; ALD: Alcoholic liver disease (ETOH); HCV: Hepatitis C virus; HBV: Hepatitis B virus; CC: Cryptogenic cirrhosis; HCC: Hepatocellular carcinoma.
Bhagat et al[27] compared he outcomes of liver transplantation in patients with NASH cirrhosis and alcoholic cirrhosis (ETOH), and found that the overall and cardiovascular mortality was numerically - albeit not significantly - increased in the NASH group. Barritt et al[28] reported that NASH cirrhosis as indication for LT is an independent factor associated with early (30-d) post-LT mortality, hazard ratio 8.96 (95%CI: 1.06-75.8), P = 0.04.
Two large national US studies addressing outcomes of LT for NASH cirrhosis were recently published. Charlton et al[9] used the SRTR database, Afzali et al[29] the UNOS database. Both studies found that the post-LT survival of NASH recipients was excellent (1-year 87.6%, 3-year 82.2%, 5-year 76.7%) and similar to recipients with non-NASH indications. Another recent study by Singal et al[30] corroborated that 1-10 year graft and patient survival rates were similar in patients transplanted for NASH, PSC and HBV related cirrhosis, respectively.
Finally, a recent systematic review and meta-analysis compared survival, and causes of death after liver transplantation for NASH and other etiologies[31]. One-, 3- and 5-year patient survivals were similar in NASH and non-NASH recipients. However, cardiovascular (CV) events and sepsis were more frequent as causes of death in NASH recipients. The authors concluded that patients with NASH cirrhosis must be carefully evaluated and selected for transplantation and that post-LT cardiovascular and infection complications must be treated aggressively.
These observations are further corroborated by the study of VanWagner et al[32] who found that NASH patients had an increased risk for the development of CV events during the first year of liver transplantation compared to ETOH patients (26% vs 8%, P < 0.001, respectively). The majority of the CV events occurred during the immediate perioperative period, and over 50% of NASH patients with a post-LT CV event had underlying risk factors such as the metabolic syndrome. CV events were the second most common cause of death in NASH recipients (9% vs 4% in EtOH recipients), surpassed only by sepsis (11% vs 1%).
Collectively, liver transplantation for NASH seems, with the current selection process, to result in excellent overall graft and patient survival (up to 10 years). However, CV events and mortality, as well as sepsis events and mortality seem to be more frequent in recipients transplanted for NASH compared to other indications.
FATTY LIVER DISEASE AFTER LIVER TRANSPLANTATION
The prevalence of IR and of other risk factors for NAFLD increase after liver transplantation. Thus, not too surprisingly, both recurrent NAFLD and de novo NAFLD in the allograft have been described.
Recurrence of NAFLD in the allograft is common post-LT. Bhagat et al[27] reported 33% recurrence of steatohepatitis in biopsy specimens at any time during the first 6 mo post-LT in NASH-cirrhosis recipients, but the course of recurrent NASH was benign since none of these patients developed cirrhosis or required re-transplantation during a 10-year follow-up. Yalamanchili et al[33] studied the post-LT outcomes in a 257 patients transplanted for CC or NASH cirrhosis. They found that, in the CC/NASH group, the probability of developing hepatic steatosis (NAFL) at 1, 2, 5 and 10 years post-LT was with 8.2%, 13.6%, 24.9%, and 32.9% at all time points higher than in patients transplanted for other indications (3.1%, 5.9%, 9.6%, and 10%, respectively). However, development of NASH in the graft was rare (13 out of 257 patients), advanced fibrosis was uncommon, and overall survival in the CC/NASH group was the same as in patients transplanted for other indications. Finally, Dureja et al[34] reported that recurrent NAFLD (predominantly NASH) was histologically found in 39% of recipients transplanted for NAFLD related or cryptogenic cirrhosis associated with the metabolic syndrome. While survival was not affected by NAFLD recurrence, a high frequency of cardiovascular disease and of infection-related morbidity and mortality was noted in patients with NAFLD recurrence.
Collectively, NAFLD seems to recur in at least 1/3 of patients transplanted for NASH cirrhosis. While, NAFLD recurrence does not seem to affect overall graft and patient survival up to 10 years, CV and infection related morbidity and mortality seem to be increased in these patients.
At least 30% of liver transplant recipients for non NAFLD related indications develop IR and/or other risk factors for NAFLD typically within 1-3 years post LT[35-38]. There is therefore growing interest in the de novo occurrence of post-LT NAFLD in recipients transplanted for non-NAFLD indications[39,40]. Dumortier et al[41] studied retrospectively the prevalence of NAFLD in post-LT liver biopsy specimens obtained by protocol biopsies in a population of recipients transplanted for non-NAFLD/CC cirrhosis and assessed the risk factors for NAFLD development. They found that de novo liver steatosis developed in 30% and steatohepatitis in 5% of the recipients. Analysis of data revealed that obesity, hyperlipidemia, diabetes mellitus, arterial hypertension, tacrolimus treatment, alcoholic cirrhosis as an indication for transplantation, and pre-transplant liver graft steatosis, were risk factors for the de novo development of post-LT NAFLD. The more of these factors were present, the higher was the prevalence of steatosis.
Recent data suggest that the genetic predisposition plays role in the post-LT recurrence of NAFLD. It is well established that the patatin-like phospholipase domain-containing protein 3 (PNPLA3) rs738409-G allele is associated with an increased fat accumulation in the liver, and is a risk factor for developing more advanced liver disease in NAFLD patients[42]. A recent study showed that the presence of the rs738409-G allele of the PNPLA3 in the recipients, but not in the donors, is an independent risk factor for post-LT steatosis[43]. These findings are in keeping with a previous study demonstrating that the presence of the PNPLA-3 rs738409 G- allele was associated with the development of post-LT obesity and diabetes mellitus[44].
MANAGEMENT OF NAFLD AFTER LIVER TRANSPLANTATION
Many drugs have been evaluated for treating NAFLD/NASH in the non-transplant setting (e.g., pioglitazone, metformin, vitamin E, pentoxyphylline, ursodeoxycholic acid). Suffice it to say that no drug intervention trial was able to demonstrate a benefit that would justify the wide spread use of the drug in NAFLD/NASH[45-47]. We are not aware of solid data on the effects on post liver transplant outcomes of treatment of insulin-resistance prior to liver transplantation in patients with NAFLD. Thus, beyond life style measures and the control of risk factors[48], there is currently no universally accepted medical therapy with proven efficacy available for NAFLD/NASH. Dietary modifications could affect the progression of NAFLD. In a recent study, Kontogianni et al[49] found that patients with NAFLD adhering to a Mediterranean diet had less severe liver disease and lower degree of IR[49]. Additionally, the role of bariatric surgery at time of LT in patients with obesity and NASH related cirrhosis remains to be defined[50].
CONCLUSION
NAFLD is expected to become the most common indication for liver transplantation within the next 1-2 decades. Despite the fact that recent studies have shed some light on the prevalence of NAFLD in patients awaiting LT and on the outcomes of recipients transplanted for NASH related cirrhosis, many aspects remain ill defined. The latter include, but are not limited to, the proportion of patients with NASH cirrhosis that is a priori excluded from liver transplantation because of co-morbidities, as well as strategies allowing to prevent the increased CV and infection related morbidity and mortality in recipients transplanted for NASH. The latter include bariatric surgery at the time of LT and attempt to tailor immunosuppressive regimens to the risk factor profile in NASH recipients. To address these and other issues, adequately powered, prospective, and whenever possible controlled trials will be required.
Footnotes
P- Reviewer: Abenavoli L, Mikolasevic I, Navarro-Jarabo JM S- Editor: Gou SX L- Editor: A E- Editor: Ma S
References
- 1.Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012;55:2005–2023. doi: 10.1002/hep.25762. [DOI] [PubMed] [Google Scholar]
- 2.Lazo M, Clark JM. The epidemiology of nonalcoholic fatty liver disease: a global perspective. Semin Liver Dis. 2008;28:339–350. doi: 10.1055/s-0028-1091978. [DOI] [PubMed] [Google Scholar]
- 3.Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology. 2006;43:S99–S112. doi: 10.1002/hep.20973. [DOI] [PubMed] [Google Scholar]
- 4.Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363:1341–1350. doi: 10.1056/NEJMra0912063. [DOI] [PubMed] [Google Scholar]
- 5.Rafiq N, Bai C, Fang Y, Srishord M, McCullough A, Gramlich T, Younossi ZM. Long-term follow-up of patients with nonalcoholic fatty liver. Clin Gastroenterol Hepatol. 2009;7:234–238. doi: 10.1016/j.cgh.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34:274–285. doi: 10.1111/j.1365-2036.2011.04724.x. [DOI] [PubMed] [Google Scholar]
- 7.McCullough AJ. Pathophysiology of nonalcoholic steatohepatitis. J Clin Gastroenterol. 2006;40 Suppl 1:S17–S29. doi: 10.1097/01.mcg.0000168645.86658.22. [DOI] [PubMed] [Google Scholar]
- 8.Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, Landt CL, Harrison SA. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140:124–131. doi: 10.1053/j.gastro.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 9.Charlton MR, Burns JM, Pedersen RA, Watt KD, Heimbach JK, Dierkhising RA. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology. 2011;141:1249–1253. doi: 10.1053/j.gastro.2011.06.061. [DOI] [PubMed] [Google Scholar]
- 10.Kemmer N, Neff GW, Franco E, Osman-Mohammed H, Leone J, Parkinson E, Cece E, Alsina A. Nonalcoholic fatty liver disease epidemic and its implications for liver transplantation. Transplantation. 2013;96:860–862. doi: 10.1097/01.TP.0000436723.59879.01. [DOI] [PubMed] [Google Scholar]
- 11.Caldwell SH, Oelsner DH, Iezzoni JC, Hespenheide EE, Battle EH, Driscoll CJ. Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease. Hepatology. 1999;29:664–669. doi: 10.1002/hep.510290347. [DOI] [PubMed] [Google Scholar]
- 12.Liou I, Kowdley KV. Natural history of nonalcoholic steatohepatitis. J Clin Gastroenterol. 2006;40 Suppl 1:S11–S16. doi: 10.1097/01.mcg.0000168644.23697.31. [DOI] [PubMed] [Google Scholar]
- 13.McCormack L, Dutkowski P, El-Badry AM, Clavien PA. Liver transplantation using fatty livers: always feasible? J Hepatol. 2011;54:1055–1062. doi: 10.1016/j.jhep.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Angulo P. Nonalcoholic fatty liver disease and liver transplantation. Liver Transpl. 2006;12:523–534. doi: 10.1002/lt.20738. [DOI] [PubMed] [Google Scholar]
- 15.de Graaf EL, Kench J, Dilworth P, Shackel NA, Strasser SI, Joseph D, Pleass H, Crawford M, McCaughan GW, Verran DJ. Grade of deceased donor liver macrovesicular steatosis impacts graft and recipient outcomes more than the Donor Risk Index. J Gastroenterol Hepatol. 2012;27:540–546. doi: 10.1111/j.1440-1746.2011.06844.x. [DOI] [PubMed] [Google Scholar]
- 16.Spitzer AL, Lao OB, Dick AA, Bakthavatsalam R, Halldorson JB, Yeh MM, Upton MP, Reyes JD, Perkins JD. The biopsied donor liver: incorporating macrosteatosis into high-risk donor assessment. Liver Transpl. 2010;16:874–884. doi: 10.1002/lt.22085. [DOI] [PubMed] [Google Scholar]
- 17.Selzner M, Rüdiger HA, Sindram D, Madden J, Clavien PA. Mechanisms of ischemic injury are different in the steatotic and normal rat liver. Hepatology. 2000;32:1280–1288. doi: 10.1053/jhep.2000.20528. [DOI] [PubMed] [Google Scholar]
- 18.Selzner M, Clavien PA. Failure of regeneration of the steatotic rat liver: disruption at two different levels in the regeneration pathway. Hepatology. 2000;31:35–42. doi: 10.1002/hep.510310108. [DOI] [PubMed] [Google Scholar]
- 19.Farrell GC, Teoh NC, McCuskey RS. Hepatic microcirculation in fatty liver disease. Anat Rec (Hoboken) 2008;291:684–692. doi: 10.1002/ar.20715. [DOI] [PubMed] [Google Scholar]
- 20.Selzner N, Selzner M, Jochum W, Amann-Vesti B, Graf R, Clavien PA. Mouse livers with macrosteatosis are more susceptible to normothermic ischemic injury than those with microsteatosis. J Hepatol. 2006;44:694–701. doi: 10.1016/j.jhep.2005.07.032. [DOI] [PubMed] [Google Scholar]
- 21.Dutkowski P, Schlegel A, Slankamenac K, Oberkofler CE, Adam R, Burroughs AK, Schadde E, Müllhaupt B, Clavien PA. The use of fatty liver grafts in modern allocation systems: risk assessment by the balance of risk (BAR) score. Ann Surg. 2012;256:861–868; discussion 868-869. doi: 10.1097/SLA.0b013e318272dea2. [DOI] [PubMed] [Google Scholar]
- 22.Kwon CH, Joh JW, Lee KW, Kim SJ, Han YS, Park JW, Kim DJ, Park JB, Lee SK. Safety of donors with fatty liver in liver transplantation. Transplant Proc. 2006;38:2106–2107. doi: 10.1016/j.transproceed.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 23.Cho JY, Suh KS, Kwon CH, Yi NJ, Lee KU. Mild hepatic steatosis is not a major risk factor for hepatectomy and regenerative power is not impaired. Surgery. 2006;139:508–515. doi: 10.1016/j.surg.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 24.Yamamoto K, Takada Y, Fujimoto Y, Haga H, Oike F, Kobayashi N, Tanaka K. Nonalcoholic steatohepatitis in donors for living donor liver transplantation. Transplantation. 2007;83:257–262. doi: 10.1097/01.tp.0000250671.06456.3f. [DOI] [PubMed] [Google Scholar]
- 25.Ahn JS, Sinn DH, Gwak GY, Kim JM, Kwon CH, Joh JW, Paik YH, Choi MS, Lee JH, Koh KC, et al. Steatosis among living liver donors without evidence of fatty liver on ultrasonography: potential implications for preoperative liver biopsy. Transplantation. 2013;95:1404–1409. doi: 10.1097/TP.0b013e31828d1588. [DOI] [PubMed] [Google Scholar]
- 26.Malik SM, deVera ME, Fontes P, Shaikh O, Ahmad J. Outcome after liver transplantation for NASH cirrhosis. Am J Transplant. 2009;9:782–793. doi: 10.1111/j.1600-6143.2009.02590.x. [DOI] [PubMed] [Google Scholar]
- 27.Bhagat V, Mindikoglu AL, Nudo CG, Schiff ER, Tzakis A, Regev A. Outcomes of liver transplantation in patients with cirrhosis due to nonalcoholic steatohepatitis versus patients with cirrhosis due to alcoholic liver disease. Liver Transpl. 2009;15:1814–1820. doi: 10.1002/lt.21927. [DOI] [PubMed] [Google Scholar]
- 28.Barritt AS, Dellon ES, Kozlowski T, Gerber DA, Hayashi PH. The influence of nonalcoholic fatty liver disease and its associated comorbidities on liver transplant outcomes. J Clin Gastroenterol. 2011;45:372–378. doi: 10.1097/MCG.0b013e3181eeaff0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Afzali A, Berry K, Ioannou GN. Excellent posttransplant survival for patients with nonalcoholic steatohepatitis in the United States. Liver Transpl. 2012;18:29–37. doi: 10.1002/lt.22435. [DOI] [PubMed] [Google Scholar]
- 30.Singal AK, Guturu P, Hmoud B, Kuo YF, Salameh H, Wiesner RH. Evolving frequency and outcomes of liver transplantation based on etiology of liver disease. Transplantation. 2013;95:755–760. doi: 10.1097/TP.0b013e31827afb3a. [DOI] [PubMed] [Google Scholar]
- 31.Wang X, Li J, Riaz DR, Shi G, Liu C, Dai Y. Outcomes of liver transplantation for nonalcoholic steatohepatitis: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2014;12:394–402.e1. doi: 10.1016/j.cgh.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 32.Vanwagner LB, Bhave M, Te HS, Feinglass J, Alvarez L, Rinella ME. Patients transplanted for nonalcoholic steatohepatitis are at increased risk for postoperative cardiovascular events. Hepatology. 2012;56:1741–1750. doi: 10.1002/hep.25855. [DOI] [PubMed] [Google Scholar]
- 33.Yalamanchili K, Saadeh S, Klintmalm GB, Jennings LW, Davis GL. Nonalcoholic fatty liver disease after liver transplantation for cryptogenic cirrhosis or nonalcoholic fatty liver disease. Liver Transpl. 2010;16:431–439. doi: 10.1002/lt.22004. [DOI] [PubMed] [Google Scholar]
- 34.Dureja P, Mellinger J, Agni R, Chang F, Avey G, Lucey M, Said A. NAFLD recurrence in liver transplant recipients. Transplantation. 2011;91:684–689. doi: 10.1097/TP.0b013e31820b6b84. [DOI] [PubMed] [Google Scholar]
- 35.Watt KD, Charlton MR. Metabolic syndrome and liver transplantation: a review and guide to management. J Hepatol. 2010;53:199–206. doi: 10.1016/j.jhep.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 36.Pagadala M, Dasarathy S, Eghtesad B, McCullough AJ. Posttransplant metabolic syndrome: an epidemic waiting to happen. Liver Transpl. 2009;15:1662–1670. doi: 10.1002/lt.21952. [DOI] [PubMed] [Google Scholar]
- 37.Laish I, Braun M, Mor E, Sulkes J, Harif Y, Ben Ari Z. Metabolic syndrome in liver transplant recipients: prevalence, risk factors, and association with cardiovascular events. Liver Transpl. 2011;17:15–22. doi: 10.1002/lt.22198. [DOI] [PubMed] [Google Scholar]
- 38.Sprinzl MF, Weinmann A, Lohse N, Tönissen H, Koch S, Schattenberg J, Hoppe-Lotichius M, Zimmermann T, Galle PR, Hansen T, et al. Metabolic syndrome and its association with fatty liver disease after orthotopic liver transplantation. Transpl Int. 2013;26:67–74. doi: 10.1111/j.1432-2277.2012.01576.x. [DOI] [PubMed] [Google Scholar]
- 39.Seo S, Maganti K, Khehra M, Ramsamooj R, Tsodikov A, Bowlus C, McVicar J, Zern M, Torok N. De novo nonalcoholic fatty liver disease after liver transplantation. Liver Transpl. 2007;13:844–847. doi: 10.1002/lt.20932. [DOI] [PubMed] [Google Scholar]
- 40.Lim LG, Cheng CL, Wee A, Lim SG, Lee YM, Sutedja DS, Da Costa M, Prabhakaran K, Wai CT. Prevalence and clinical associations of posttransplant fatty liver disease. Liver Int. 2007;27:76–80. doi: 10.1111/j.1478-3231.2006.01396.x. [DOI] [PubMed] [Google Scholar]
- 41.Dumortier J, Giostra E, Belbouab S, Morard I, Guillaud O, Spahr L, Boillot O, Rubbia-Brandt L, Scoazec JY, Hadengue A. Non-alcoholic fatty liver disease in liver transplant recipients: another story of “seed and soil”. Am J Gastroenterol. 2010;105:613–620. doi: 10.1038/ajg.2009.717. [DOI] [PubMed] [Google Scholar]
- 42.Rotman Y, Koh C, Zmuda JM, Kleiner DE, Liang TJ. The association of genetic variability in patatin-like phospholipase domain-containing protein 3 (PNPLA3) with histological severity of nonalcoholic fatty liver disease. Hepatology. 2010;52:894–903. doi: 10.1002/hep.23759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Finkenstedt A, Auer C, Glodny B, Posch U, Steitzer H, Lanzer G, Pratschke J, Biebl M, Steurer M, Graziadei I, et al. Patatin-like phospholipase domain-containing protein 3 rs738409-G in recipients of liver transplants is a risk factor for graft steatosis. Clin Gastroenterol Hepatol. 2013;11:1667–1672. doi: 10.1016/j.cgh.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 44.Watt KD, Dierkhising R, Fan C, Heimbach JK, Tillman H, Goldstein D, Thompson A, Krishnan A, Charlton MR. Investigation of PNPLA3 and IL28B genotypes on diabetes and obesity after liver transplantation: insight into mechanisms of disease. Am J Transplant. 2013;13:2450–2457. doi: 10.1111/ajt.12355. [DOI] [PubMed] [Google Scholar]
- 45.Charlton M. Evolving aspects of liver transplantation for nonalcoholic steatohepatitis. Curr Opin Organ Transplant. 2013;18:251–258. doi: 10.1097/MOT.0b013e3283615d30. [DOI] [PubMed] [Google Scholar]
- 46.Van Wagner LB, Rinella ME. The role of insulin-sensitizing agents in the treatment of nonalcoholic steatohepatitis. Therap Adv Gastroenterol. 2011;4:249–263. doi: 10.1177/1756283X11403809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Satapathy SK, Nair S, Vanatta JM. Nonalcoholic fatty liver disease following liver transplantation. Hepatol Int. 2013;7:400–412. doi: 10.1007/s12072-013-9434-3. [DOI] [PubMed] [Google Scholar]
- 48.Newsome PN, Allison ME, Andrews PA, Auzinger G, Day CP, Ferguson JW, Henriksen PA, Hubscher SG, Manley H, McKiernan PJ, et al. Guidelines for liver transplantation for patients with non-alcoholic steatohepatitis. Gut. 2012;61:484–500. doi: 10.1136/gutjnl-2011-300886. [DOI] [PubMed] [Google Scholar]
- 49.Kontogianni MD, Tileli N, Margariti A, Georgoulis M, Deutsch M, Tiniakos D, Fragopoulou E, Zafiropoulou R, Manios Y, Papatheodoridis G. Adherence to the Mediterranean diet is associated with the severity of non-alcoholic fatty liver disease. Clin Nutr. 2014;33:678–683. doi: 10.1016/j.clnu.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 50.Heimbach JK, Watt KD, Poterucha JJ, Ziller NF, Cecco SD, Charlton MR, Hay JE, Wiesner RH, Sanchez W, Rosen CB, et al. Combined liver transplantation and gastric sleeve resection for patients with medically complicated obesity and end-stage liver disease. Am J Transplant. 2013;13:363–368. doi: 10.1111/j.1600-6143.2012.04318.x. [DOI] [PubMed] [Google Scholar]


