Abstract
Objective
The purpose of this study was to compare the effects of mechanical polishing (MP) and chemical polishing (CP) on the average surface roughness (Ra) of heat-cured (HC) and light-cured (LC) denture base acrylic resins.
Methods
A total of 120 specimens (30 × 15 × 3 mm) were prepared from one HC and one LC acrylic resin. To remove nodules and gross surface irregularities, all specimens were finished with a lathe-mounted small acrylic bur and 360-grit sandpaper. Ten finished specimens of each acrylic resin were randomly assigned to each of six polishing techniques: Resilit High-luster Polishing Liquid (RHPL), Universal Polishing Paste, Abraso-star K50, pumice, Jet Seal Liquid, or Acrypoint. MP was performed with an automatic polishing machine for 2 min, under 50 rpm and 500 g of load. CP was performed by immersing the HC and LC specimens in preheated methyl methacrylate at 75 ± 1 °C for 10 s. The surface roughness of the acrylic resin specimens was measured with a contact profilometer. The Ra values were analyzed by two-way analysis of variance, post hoc Scheffe's test, and paired t-test (p ⩽ 0.05). Polished and tested acrylic resin surfaces were evaluated by scanning electron microscopy.
Results
MP was more effective than CP. The smoothest surface was obtained with the use of the RHPL on the LC (0.05 ± 0.01 μm) or HC (0.07 ± 0.01 μm) acrylic resin. Two-way ANOVA showed a statistically significant difference between MP and CP.
Conclusions
MP produced the smoothest surface of denture base acrylic resin. The mean surface roughness values after MP and CP were not influenced by the type of acrylic resin.
Keywords: Surface roughness, Mechanical polishing, Chemical polishing, Contact profilometer, Acrylic resin
1. Introduction
Acrylic resins and resin-based direct and indirect restorative materials have been used widely in dentistry, specifically in the field of prosthodontics, to fabricate different types of prostheses, including complete and partial dentures, temporary fixed partial dentures, implant-supported overdentures, and maxillofacial prostheses (Kuhar et al., 2005). Acrylic resins may be heat-cured (HC), autocured, or microwave-cured (Hong et al., 2009; Rached et al., 2004; Yunus et al., 1994). Conventional resins that are used in dentistry are based on poly-methyl methacrylate (poly-MMA) (Danesh et al., 2012; Hong et al., 2009).
A major breakthrough in the application of acrylic resins in the field of dentistry occurred with the introduction of visible light-cured (LC) acrylic resins, which are urethane dimethylacrylate-based (Danesh et al., 2012; Jorge et al., 2003; Kedjarune et al., 1999; Leggat and Kedjarune, 2003). LC acrylic resins are activated by light in the wavelength range of 460–470 nm. They include larger molecular weight methacrylates and dimethacrylates (Haselden et al., 1998). LC resins have a lower elution rate (0.06 wt%) than MMA-based acrylic resins (0.13–0.054 wt%) (Danesh et al., 2012; Ferracane, 1994). LC resins elicit less soft-tissue irritation, produce less heat during polymerization, and have a relatively pleasant odor compared to MMAs (Al Rifaiy, 2012; Haywood et al., 2003).
The surface finish of any dental prosthesis is an important factor that determines patient’s comfort, prosthesis longevity, and esthetics (Rahal et al., 2004; Ulusoy et al., 1986). High values for the free energy (hydrophilicity) (Busscher et al., 1986) and roughness of the prosthesis surface will increase the chances of microbial adhesion and plaque retention, respectively, and reduce patient’s oral hygiene (Kagermeier-Callaway et al., 2000; Rahal et al., 2004; Ulusoy et al., 1986). Studies have shown a direct correlation between surface roughness and plaque retention, plaque maturation, Candida albicans colonization, and associated denture stomatitis (Barbeau et al., 2003; Berger et al., 2006; Radford et al., 1997).
In vivo studies have suggested that, to be clinically acceptable, prostheses and dental restorations should not have average (mean) surface roughness (Ra) values higher than 0.2 μm (Bollen et al., 1997; Quirynen et al., 1996; Seng-Kyun Kim et al., 2009). Below this value, no further reduction in plaque accumulation can be expected. Above this value, a proportional increase in plaque accumulation occurs (Abuzar et al., 2010; Bollen et al., 1996; Kuhar et al., 2005; Quirynen et al., 1996).
Polishing can be performed through mechanical or chemical methods (Goncalves et al., 2008). Mechanical polishing (MP) methods use abrasives to produce controlled wear of the surface material to reduce surface roughness (Abuzar et al., 2010). Materials used for MP include polishing wheels, felt cones, prophylactic pastes, rubber polishers, abrasive stones, aluminum oxide-based polishing pastes, silicone polishers, pumice, and lathe polishing (Braun et al., 2003; Sofou et al., 2001; Yamauchi et al., 1990).
As an alternative to the conventional method of MP, in 1969, Gotusso introduced a method called superficial chemical polishing (CP) (Al-Rifaiy, 2010; Braun et al., 2003; Gotusso, 1969; Rahal et al., 2004). In this technique, the finished acrylic resin denture is placed in a chemical polisher containing heated monomer at 75 °C for 10 s (Al-Rifaiy, 2010; Rahal et al., 2004). Subsequent studies have proven the biocompatibility of this technique (Nagem-Filho et al., 1973; Rahal et al., 2004).
Although some studies have evaluated the effects of MP and CP techniques on the surface roughness of HC, autocured, and microwave-cured acrylic resins, no study has examined the effects of polishing techniques on the surface roughness of LC denture base resins. Therefore, the aim of this study was to evaluate and compare the effects of MP and CP on the Ra of visible LC and HC denture base resins.
2. Materials and methods
2.1. Preparation of test specimens
In this study, 120 specimens (30 × 15 × 3 mm) were prepared from HC acrylic resin (Lucitone, Dentsply International, Inc., York, PA, USA) and LC acrylic resin (Eclipse, Dentsply International, Inc.). The HC acrylic resin specimens were prepared by investing the wax pattern (30 × 15 × 3 mm) in gypsum plaster by a conventional flasking procedure in dental flasks. After dewaxing the plaster molds, the acrylic material was packed and processed in accordance with manufacturers’ instructions.
A Perspex mold with a glass lid was designed to prepare the LC specimens. After applying petroleum jelly, the mold was preheated at 55 °C for 2 min in a special oven (Conditioning Oven, Dentsply Trubyte). The LC acrylic resins were compacted into the mold cavity by finger pressure. A glass slab was pressed on top to remove excess material and to obtain specimens of uniform thickness. An air-barrier coating (Eclipse ABC, Dentsply Trubyte, USA) was applied to the resin surface to prevent the inhibition of polymerization by oxygen. Polymerization was performed in an LC unit (Eclipse Processing Unit, Dentsply Trubyte) containing six Eclipse halogen lamps (41 V each; Dentsply Trubyte) by exposing the sample to visible light at 400 to 500 nm for 10 min.
Polymerized specimens were retrieved from the flask and finished to remove nodules and gross irregularities. Finishing was performed by using a small acrylic trimming bur mounted on a laboratory lathe. Final finishing was done with 360-grit sandpaper mounted on a lathe. After final finishing of all the specimens, 10 specimens of each acrylic resin were randomly assigned to one of the six polishing techniques shown in Table 1. MP was performed with an automatic polishing machine (The Wirtz, Jean Wirtz, Dusheldory W, Germany) for 2 min, under 50 rpm and 500 g of load with Resilit High-luster Polishing Liquid (RHPL), Universal Polishing Paste (UPP), Abraso-Star K50 (K50), pumice, Jet Seal Liquid (JSL), or AcryPoint, as recommended by the manufacturer. CP was performed by immersing the HC and LC specimens in preheated MMA (JSL) at 75 ± 1 °C for 10 s (Al-Rifaiy, 2010).
Table 1.
Polishing procedures and products used in the study.
| Polishing procedure | Polishing products | Composition | Manufacturer |
|---|---|---|---|
| Mechanical | Resilit High-luster Polishing Liquid | Loose abrasives (aluminum oxide-Al2O3) in liquid | Renfert, GmbH |
| Mechanical | Universal Polishing Paste | Loose abrasives (aluminum oxide-Al2O3) in paste | Ivoclar Vivadent, Schaan, Liechtenstein |
| Mechanical | Abraso-Star K50 | Mixture of waxes and abrasives | Bredent GmbH & Co. KG |
| Mechanical | Pumice | Pumice (coarse CL-60), amorphous silica and quartz | WhipMix Corporation, Kentucky, USA. |
| Mechanical | AcryPoint | Bonded abrasives (silicon carbide in silicon matrix) | Shofu Inc., Kyoto, Japan |
| Chemical | Jet Seal Liquid | Methyl methacrylate | Lang Dental Mfg. Co., USA. |
2.2. Surface roughness measurements
The surface roughness of the acrylic resin specimens was determined with a contact profilometer (Tylor Hobson Ltd., series No. 339, Leicester, UK). The instrument’s diamond stylus was moved across the specimen surface under constant pressure. Three measurements were made for each specimen, with a cutoff value of 5 mm. The average of three readings for each specimen was considered as the final Ra value of the particular specimen. To test for significant differences in Ra of the two acrylic resins, six polishing techniques and their interactions were compared. Paired and unpaired Student’s t-tests and two-way ANOVA followed by a post hoc Scheffe's test for multiple comparisons were performed (p < 0.05).
2.3. Scanning electron microscopy (SEM)
Polished samples were subjected to SEM analysis (JSM 6360, JEOL Ltd., Japan) at a magnification of 50× under a high-vacuum condition. Specimens were air dried in desiccators, cleaned with 70% alcohol in an ultrasonic cleaner, and sputter-coated with gold for up to 200 Å (Polaron E-5200 Energy Beam Sciences, Agawan, MA, USA).
3. Results
Table 2 and Table 3 shows the Ra values and standard deviations (SDs). The Ra values varied depending on the polishing technique (p < 0.000 by two-way ANOVA). There was no significant difference in the Ra between the HC and LC acrylic resins (p < 0.2) (Table 2). There was a significant interaction between the material and the polishing technique, indicating that the effect of one factor was dependent on the other. Paired Student’s t-test revealed no significant difference between the materials after each polishing technique.
Table 2.
Two-way analysis of variance.
| Effect | Sum of squares | df | Mean-squared | F | p |
|---|---|---|---|---|---|
| Material | 0.005 | 1 | 0.005 | 1.690 | 0.200 |
| Technique | 0.514 | 5 | 0.103 | 34.963 | 0.000 |
| Material*Technique | 0.112 | 5 | 0.022 | 7.599 | 0.000 |
| Error | 0.141 | 48 | 0.003 |
Table 3.
Mean and standard deviations of roughness values for acrylic specimens polished with different systems (μm). The value with the same superscript letter indicates no significance.
| Comparison | Light-cured acrylic resin (mean ± SD) | Heat-cured acrylic resin (mean ± SD) |
|---|---|---|
| Resilit High-luster Polishing Liquid | 0.05a ± 0.01 | 0.07a ± 0.01 |
| Universal Polishing Paste | 0.06a ± 0.01 | 0.08a ± 0.02 |
| Abraso-Star K50 | 0.06a ± 0.00 | 0.10a ± 0.05 |
| Pumice | 0.11a ± 0.04 | 0.10a ± 0.01 |
| Jet Seal Liquid | 0.29b ± 0.04 | 0.29b ± 0.05 |
| AcryPoint | 0.23b ± 0.06 | 0.25b ± 0.05 |
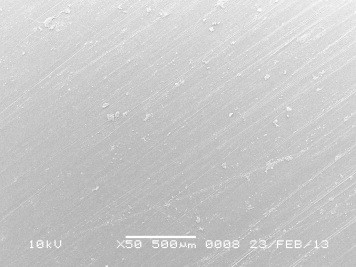
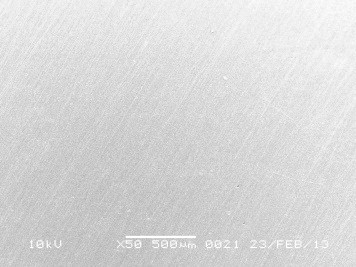
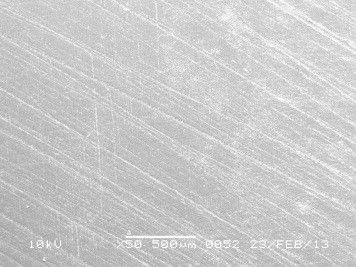
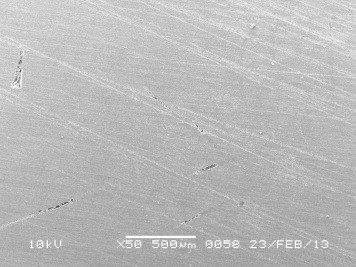
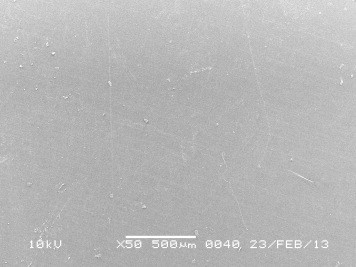
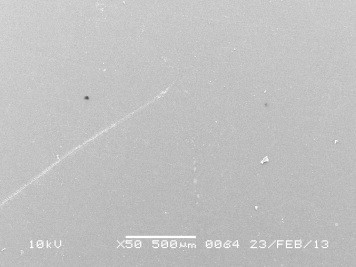
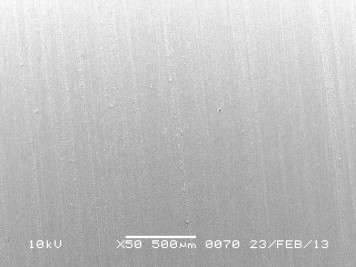
The post hoc Scheffe's test was used to compare the six polishing techniques for each type of acrylic resin (Table 3). The smoothest surface was obtained with the RHPL on the LC (0.05 ± 0.01 μm) or HC (0.07 ± 0.01 μm) acrylic resin (Figs. 1 and 6), with these values being well below the clinically accepted threshold value of 0.2 μm. The highest Ra value was obtained with AcryPoint on the HC (0.25 ± 0.05 μm) or LC (0.23 ± 0.06 μm) acrylic resin (Figs. 5 and 11), with these values being above the threshold value of 0.2 μm. After CP with JSL, the same Ra value was obtained for the HC and LC specimens (0.29 ± 0.04 and ± 0.05 μm, respectively), which significantly exceeded the threshold value of 0.2 μm (Figs. 6 and 12).
Figure 1.
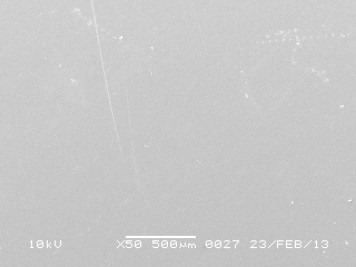
SEM image of heat-cured specimen after polishing using Resilit high luster polishing liquid.
Figure 6.
SEM image of heat-cured specimen after polishing using Jet Seal Liquid.
Figure 5.
SEM image of heat-cured specimen after polishing using acrypoint.
Figure 11.
SEM image of visible light cured specimen after polishing using acrypoint.
Figure 12.
SEM image of visible light cured specimen after polishing using Jet Seal Liquid.
The surface irregularities of the acrylic resins by SEM corresponded with the respective Ra values of the particular specimens (Figs. 1–12). SEM micrographs confirmed that highest roughness was found in with AcryPoint and Jet Seal Liquid polishing systems (Figs. 5, 6, 11 and 12).
Figure 2.
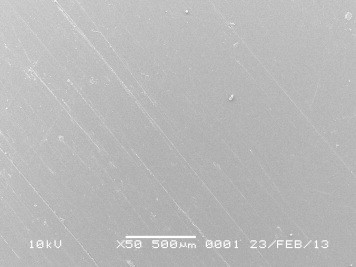
SEM image of heat-cured specimen after polishing using Universal Polishing Paste.
Figure 3.
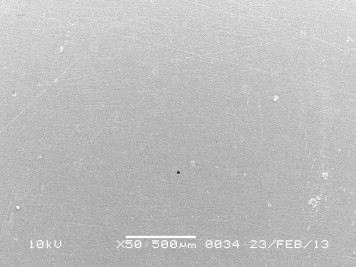
SEM image of heat-cured specimen after polishing using Abraso star K50.
Figure 4.
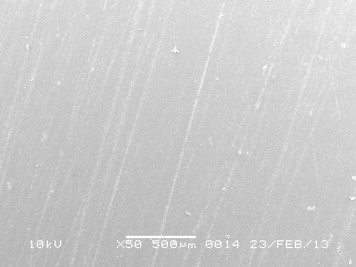
SEM image of heat-cured specimen after polishing using pumice.
Figure 7.
SEM image of visible light cured specimen after polishing using Resilit high luster polishing liquid.
Figure 8.
SEM image of visible light cured specimen after polishing using Universal Polishing Paste.
Figure 9.

SEM image of visible light cured specimen after polishing using Abraso star K50.
Figure 10.
SEM image of visible light cured specimen after polishing using pumice.
4. Discussion
Dentures and artificial acrylic teeth are hard surfaces that tend to attract food debris and to form plaque and calculus if not polished (Morgan and Wilson, 2001). A smooth surface is a prerequisite for denture base acrylics, to prevent plaque accumulation and further denture-induced stomatitis (Machado et al., 2011). To reduce the surface roughness, an acrylic prosthesis is finished and polished by various finishing and polishing techniques in a sequential manner. Sequential procedures are applied to remove gross irregularities and nodules from the rough superficial surface by using various lathe-mounted acrylic burs, felt cones, rubber wheels, and disks, followed by final finishing under light pressure. The ultimate smooth and glossy finish is achieved by polishing with different commercially available polishing agents.
In the present study, before the specimens were subjected to polishing, they were finished with a lathe-mounted acrylic bur to remove gross irregularities and surface nodules. Final finishing was performed with lathe-mounted 360-grit sandpaper with light pressure. After final finishing, the specimens were subjected to six polishing techniques.
Although manufacturers’ instructions and standard laboratory protocols were employed throughout the study, the study still has some limitations. First, the specimens were not fabricated to resemble dentures, because dentures do not have completely flat surfaces, as was the case for the specimens used in this study. Second, MP systems will have various degrees of abrasiveness. The abrasiveness of a polishing system and the resulting surface smoothness depend on the size of abrasive particles present in the polishing system.
In the present study, MP techniques were more effective than CP, producing surface roughness values that were less than the threshold value of 0.2 μm. This fact was especially true when the samples were polished using RHPL, UPP, K50, or pumice, which have been used routinely in the laboratory for quite some time. AcryPoint showed an Ra value that was very close to the threshold value. This finding could be due to the size of abrasive particles contained in that particular polishing system (Seng-Kyun Kim et al., 2009). The Ra values of the CP specimens were above the acceptable threshold (Table 3). Al-Rifaiy (2010); Rahal et al. (2004), and Alves et al. (2007) also found that CP produced a higher Ra in acrylic resins than MP.
A statistically significant difference in Ra was achieved in specimens treated by MP compared to CP. This difference could be attributed to the MMA molecules present in the polishing fluid, which penetrate the superficial polymeric chains of the acrylic resin, breaking the secondary bonds that join them and promoting a final plasticizing effect of the acrylic resin surface (Rahal et al., 2004). This effect may increase the surface roughness. Another reason for this difference could be related to the abrasive mechanical action, which decreases the surface roughness during polishing (Fionnuala O’Donnell et al., 2003). The MP agent may contain finer abrasive particles, which help to achieve a smooth surface (Phillips, 1982).
Interestingly, there were significant differences in the Ra values between MP and CP, except for polishing with AcryPoint, in both types of acrylic resin. The type of acrylic resin did not influence the Ra after MP or CP. MP rather than CP is indicated because it yields lower Ra values (Rahal et al., 2004).
The visual comparison of SEM images with Ra values showed that after polishing, the LC and HC acrylic resin specimens polished using AcryPoint (Figs. 5 and 11) and JSL (Figs. 6 and 12) contained large pores compared to the surface textures of specimens polished by other polishing systems. These specimens showed a similar pattern, with very minute debris at the surface. Kuhar et al. (2005) reported that pores, similar to surface roughness, enhance the accumulation of denture plaque and staining on some parts of dentures.
5. Conclusion
Within the limitations of this study, the following conclusions can be made:
-
(1)
The RHPL, UPP, and K50 agents produced superior surface smoothness for all acrylic resin specimens and a mean Ra significantly below the threshold Ra of 0.2 μm (p < 0.0017).
-
(2)
Ra values after MP and CP were not influenced by the type of acrylic resin.
-
(3)
MP was the most effective polishing technique.
Ethical statement
This research did not involve human subjects or where human subjects were involved was conducted in full accordance with ethics principles, including the World Medical Association Declaration of Helsinki.
Conflict of interest
The author has no conflicts of interest to declare.
Acknowledgement
The authors would like to extend their appreciation to the Research Centre, College of Applied Medical Sciences and the Deanship of Scientific Research at King Saud University for funding this research.
Footnotes
Peer review under responsibility of King Saud University.
References
- Abuzar M.A., Bellur S., Duong N., Kim B.B., Lu P., Palfreyman N. Evaluating surface roughness of a polyamide denture base material in comparison with poly (methyl methacrylate) J. Oral Sci. 2010;52:577–581. doi: 10.2334/josnusd.52.577. [DOI] [PubMed] [Google Scholar]
- Al Rifaiy M.Q. Shear bond strength between light polymerized hard reline resin and denture base resin subjected to long term water immersion. Saudi Dental J. 2012;24:23–27. doi: 10.1016/j.sdentj.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Rifaiy M.Q. The effect of mechanical and chemical polishing techniques on the surface roughness of denture base acrylic resins. Saudi Dental J. 2010;22:13–17. doi: 10.1016/j.sdentj.2009.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves P.V.M., Lima Filho Roberto M.A., Telles E. Surface roughness of acrylic resins after different curing and polishing techniques. Angle Orthodontist. 2007;77(3) doi: 10.2319/0003-3219(2007)077[0528:SROARA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Barbeau J., Seguin J., Goulet J.P., de Koninck L., Avon S.L., Lalonde B. Reassessing the presence of Candida albicans in denture-related stomatitis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003;95:51–59. doi: 10.1067/moe.2003.44. [DOI] [PubMed] [Google Scholar]
- Berger J.C., Driscoll C.F., Romberg E., Luo Q., Thompson G. Surface roughness of denture base acrylic resins after processing and after polishing. J. Prosthodont. 2006;15:180–186. doi: 10.1111/j.1532-849X.2006.00098.x. [DOI] [PubMed] [Google Scholar]
- Bollen C.M., Papaioanno W., Van Eldere J., Schepers E., Quirynen M., van Steenberghe D. The influence of abutment surface roughness on plaque accumulation and peri-implant mucositis. Clin. Oral Implants Res. 1996;7:201–211. doi: 10.1034/j.1600-0501.1996.070302.x. [DOI] [PubMed] [Google Scholar]
- Bollen C.M., Lambrechts P., Quirynen M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: a review of the literature. Dent. Mater. 1997;13:258–269. doi: 10.1016/s0109-5641(97)80038-3. [DOI] [PubMed] [Google Scholar]
- Braun K.O., Mello J.A.N., Rached R.N., Del Bel Cury A.A. Surface texture and some properties of acrylic resins submitted to chemical polishing. J. Oral Rehabil. 2003;30:91–98. doi: 10.1046/j.1365-2842.2003.00997.x. [DOI] [PubMed] [Google Scholar]
- Busscher H.J., Uyen M.H.M.J.C., Weerkamp A.H., Postma W.J., Arends J. Reversibility of adhesion of oral streptococci to solids. FEMS Microbiol. Lett. 1986;35:303–306. [Google Scholar]
- Danesh G., Hellak T., Reinhardt K.J., Vegh A., Schafer E., Lippold C. Elution characteristics of residual monomers in different light- and auto-curing resins. Exp. Toxicol. Pathol. 2012;64:867–872. doi: 10.1016/j.etp.2011.03.008. [DOI] [PubMed] [Google Scholar]
- Ferracane J.L. Elution of leachable components from composites. J. Oral Rehabil. 1994;21:441–452. doi: 10.1111/j.1365-2842.1994.tb01158.x. [DOI] [PubMed] [Google Scholar]
- Fionnuala O’Donnell E., Radford David R., Sinclair Gary F., Clark Robert K.F. Chairside polishing of heat-cured acrylic resin: an SEM and EDA study. Intern J. Prosth. 2003;16(3):233–238. [PubMed] [Google Scholar]
- Goncalves T.S., Spohr A.M., de Souza R.M., Macedo de Menezes L. Surface roughness of auto polymerized acrylic resin according to different manipulation and polishing methods: an in situ evaluation. Angle Orthod. 2008;78:931–934. doi: 10.2319/080307-363.1. [DOI] [PubMed] [Google Scholar]
- Gotusso M.J. Chemical surface treatment of acrylic resins. Rev. Asoc. Odonto.l Argent. 1969;57:359–361. [PubMed] [Google Scholar]
- Haselden C.A., Hobkirk J.A., Pearson G.J., Davies E.H. A comparison between the wear resistance of three types of denture resin to three different dentifrices. J. Oral Rehabil. 1998;25:335–339. doi: 10.1046/j.1365-2842.1998.00250.x. [DOI] [PubMed] [Google Scholar]
- Haywood J., Basker R.M., Watson C.J., Wood D.J. A comparison of three hard chairside denture reline materials. Part I. clinical evaluation. Eur. J. Prosthodont Restor. Dent. 2003;11:157–163. [PubMed] [Google Scholar]
- Hong G., Murata H., Li Y., Sadamori S., Hamada T. Influence of denture cleansers on the color stability of three types of denture base acrylic resin. J. Prosthet. Dent. 2009;101:205–213. doi: 10.1016/S0022-3913(09)60032-9. [DOI] [PubMed] [Google Scholar]
- Jorge J.H., Giampaolo E.T., Machado A.L., Vergani C.E. Cytotoxicity of denture base acrylic resins: a literature review. J. Prosthet. Dent. 2003;90:190–193. doi: 10.1016/s0022-3913(03)00349-4. [DOI] [PubMed] [Google Scholar]
- Kagermeier-Callaway A.S., Willershausen B., Frank T., Stender E. In vitro colonisation of acrylic resin denture base materials by Streptococcus oralis and Actinomyces viscosus. Int. Dent. J. 2000;50:79–85. doi: 10.1002/j.1875-595x.2000.tb00803.x. [DOI] [PubMed] [Google Scholar]
- Kedjarune U., Charoenworaluk N., Koontongkaew S. Release of methyl methacrylate from heat-curved and autopolymerized resins: cytotoxicity testing related to residual monomer. Aust. Dent. J. 1999;44:25–30. doi: 10.1111/j.1834-7819.1999.tb00532.x. [DOI] [PubMed] [Google Scholar]
- Kuhar M., Funduk N. Effects of polishing techniques on the surface roughness of acrylic denture base resins. J. Prosthet. Dent. 2005;93:76–85. doi: 10.1016/j.prosdent.2004.10.002. [DOI] [PubMed] [Google Scholar]
- Leggat P.A., Kedjarune U. Toxicity of methyl methacrylate in dentistry. Int. Dent. J. 2003;53:126–131. doi: 10.1111/j.1875-595x.2003.tb00736.x. [DOI] [PubMed] [Google Scholar]
- Machado A.L., Giampaolo E.T., Vergani C.E., Souza J.F., Jorge J.H. Changes in roughness of denture base and reline materials by chemical disinfection or microwave irradiation: surface roughness of denture base and reline materials. J. Appl. Oral Sci. 2011;19(5):521–528. doi: 10.1590/S1678-77572011000500015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan T.D., Wilson M. The effects of surface roughness and type of denture acrylic on biofilm formation by Streptococcus oralis in a constant depth film fermentor. J. Appl. Microbiol. 2001;19:47–53. doi: 10.1046/j.1365-2672.2001.01338.x. [DOI] [PubMed] [Google Scholar]
- Nagem-Filho H., Chiodi-Netto J., De Araujo P.A. Biocompatibility of acrylic resins implants in connective tissue. Estomatol. Cultura. 1973;7:120–123. [PubMed] [Google Scholar]
- Ralph W. Phillips., 1982 science of dental materials, eighth ed, Philadelphia, PA.
- Quirynen M., Bollen C.M., Papaioannou W., Van Eldere J., van Steenberghe D. The influence of titanium abutment surface roughness on plaque accumulation and gingivitis: short-term observations. Int. J. Oral Maxillofac. Implants. 1996;11:169–178. [PubMed] [Google Scholar]
- Rached R.N., Powers J.M., Del Bel Cury A.A. Repair strength of autopolymerizing, microwave, and conventional heat-polymerized acrylic resins. J. Prosthet. Dent. 2004;92:79–82. doi: 10.1016/j.prosdent.2004.04.005. [DOI] [PubMed] [Google Scholar]
- Radford D.R., Watson T.F., Walter J.D., Challacombe S.J. The effects of surface machining on heat cured acrylic resin and two soft denture base materials: a scanning electron microscope and confocal microscope evaluation. J. Prosthet. Dent. 1997;78:200–208. doi: 10.1016/s0022-3913(97)70126-4. [DOI] [PubMed] [Google Scholar]
- Rahal J.S., Mesquita M.F., Henriques G.E., Nobilo M.A. Surface roughness of acrylic resins submitted to mechanical and chemical polishing. J. Oral Rehabil. 2004;31:1075–1079. doi: 10.1111/j.1365-2842.2004.01344.x. [DOI] [PubMed] [Google Scholar]
- Seng-Kyun Kim, Ju-Mi Park, Min-Ho Lee, Jae-Youn Jung, Shipu Li, Xinyu Wang. Effects of Chairside Polishing and brushing on Surface Roughness of Acrylic Denture Base Resins. J. Wuhan Univ. Tech-Mater. Sci. Ed. 2009;24:1:100–105.
- Sofou A., Emmanouil J., Peutzfeldt A., Owall B. The effect of different polishing techniques on the surface roughness of acrylic resin materials. Eur. J. Prosthodont. Restor. Dent. 2001;9:117–122. [PubMed] [Google Scholar]
- Ulusoy M., Ulusoy N., Aydin A.K. An evaluation of polishing techniques on surface roughness of acrylic resins. J. Prosthet. Dent. 1986;56:107–112. doi: 10.1016/0022-3913(86)90292-1. [DOI] [PubMed] [Google Scholar]
- Yamauchi M., Yamamoto K., Wakabayashi M., Kawano J. In vitro adherence of microorganisms to denture base resin with different surface texture. Dent. Mater. J. 1990;9:19–24. doi: 10.4012/dmj.9.19. [DOI] [PubMed] [Google Scholar]
- Yunus N., Harrison A., Huggett R. Effect of microwave irradiation on the flexural strength and residual monomer levels of an acrylic resin repair material. J. Oral Rehabil. 1994;21:641–648. doi: 10.1111/j.1365-2842.1994.tb01179.x. [DOI] [PubMed] [Google Scholar]



