Abstract
Objective:
C-reactive protein (CRP) is an acute-phase reactant and has been proved to be a significant predictor of future cardiovascular events. Recent studies have demonstrated a correlation between periodontitis and elevated CRP levels. However, most of the studies have focused on chronic periodontitis and very few studies are done in patients with aggressive periodontitis. The aim of this study was to determine and compare the relative levels of serum CRP in aggressive and chronic periodontitis patients.
Materials and Methods:
A total of 75 systemically healthy subjects were divided into three groups: Group I, nonperiodontitis subjects; group II, chronic generalized periodontitis patients and group III, generalized aggressive periodontitis patients. All participants were subjected to quantitative CRP analysis using enzyme-linked immunosorbent assay.
Results:
Mean CRP levels were significantly greater in both group II and III as compared to group I and group III having greater level than group II. Furthermore, CRP levels positively correlated with the amount of periodontal destruction as measured by probing depth and clinical attachment loss.
Conclusion:
The present study indicates a positive correlation between CRP and periodontal disease severity with particular concern in younger individuals that could be a possible underlying pathway in the association between periodontal disease and the observed higher risk for cardiovascular disease in periodontitis patients.
Keywords: Aggressive periodontitis, chronic periodontitis, C-reactive protein, periodontitis
Introduction
Growing interest in association between periodontal disease and systemic inflammation has led to convergence in oral and medical care. It has been widely accepted that periodontal infections are leading culprits for cardiovascular disease (CVD). This association could partly be explained by C-reactive protein (CRP), which is a systemic marker of inflammation. It is receiving the most attention as it best describes the inflammatory status of an individual due of its kinetics.[1] CRP is an acute-phase reactant produced by the liver,[2] which is nonspecific and produced in response to various stimuli. CRP possesses the ability to reveal inflammation at an early stage as it rises in serum within 48 h.[3] Its long plasma half-life of 12-18 h is constant under most of the conditions and hence that the sole determinant of circulating CRP is the synthesis rate, which directly reflects the intensity of the pathological process stimulating CRP production.[4] This property is useful for early detection of patients who are at risk for inflammatory disease. Moreover, it can upregulate proinflammatory mediator production.[5] According to the Centers for Disease Control and Prevention/American Heart Association, CRP levels >3 mg/L indicates a higher risk for CVDs, whereas CRP levels of 1-3 mg/L suggests medium risk, and CRP levels <1 mg/L suggests lower risk.[6] A number of studies have demonstrated an association between periodontal disease and the risk of CVD.[7,8] CRP possess the ability to predict future cardiovascular events in apparently healthy individuals. But, it is not clear whether this association is casual or definite as both the diseases share so many risk factors.
There is strong evidence that CRP is increased in otherwise healthy adults with poor periodontal status.[9] However, the disparity among them occurs in terms of methods used, criteria of patient selection, confounding of risk factors and moreover some authors denied this association.[10]
Most studies to date have included patients with chronic periodontitis without correlating serum CRP levels with severity of inflammation, and also limited information is available whether systemic inflammation differs in different types of periodontitis as there is scarcity of literature regarding CRP levels in subjects with aggressive periodontitis.[11,12,13,14,15,16] Since both forms of periodontitis show disparity in the rate of progression, the effect of chronic and aggressive periodontitis on CRP levels seems to be an appealing area of research. Thus, the present study was undertaken to determine the relative levels of serum CRP and compare them in aggressive and chronic periodontitis patients and correlating the serum CRP levels with severity of disease.
Materials and Methods
Following complete medical and dental examination, 75 individuals were selected for the study from Department of Periodontics, Dr. Ziauddin Ahmad Dental College, Aligarh. The study was approved by Internal Review Board. A total of seventy-five systemically healthy subjects were divided into three groups: Group I, nonperiodontitis subjects; group II, chronic generalized periodontitis (CGP) patients and group III, generalized aggressive periodontitis (GAP) patients. Informed consent was obtained from each individual.
Inclusion criteria
Subjects were placed into three groups according to the following definitions:
Group I: Nonperiodontitis (NP) group - clinically healthy periodontal status with probing depth (PD) ≤2 mm along with no evidence of attachment loss
Group II: CGP patients - probing depth (PD) of ≥5 mm and/or clinical attachment loss (CAL) >30% sites with varying degree of disease severity. Local factors concomitant with the amount of destruction and with moderate rate of progression
Group III: GAP - patients under age of 30 years having probing depth (PD) of ≥5 mm and/or CAL on 8 or more teeth, at least three of which were not first molars and incisors with varying degree of disease severity. Deposits being inconsistent with disease severity.
Exclusion criteria
Current smokers; pregnant and lactating women; individuals with acute or chronic medical disorders; patient under any medication for the past 3 months; patient undergone any dental treatment for the past 6 months were excluded from the study.
Periodontal assessment
Periodontal disease status was evaluated at 4 sites per tooth (mesiobuccal, buccal, distobuccal, lingual/palatal) by measuring the probing depth (PD), CAL, gingival index by Loe and Silness), plaque index (Silness and Loe) using the same periodontal probe (UNC-15 probes Hu-Friedy's, USA) and by same examiner to avoid bias. The probing depth was measured as the distance from the gingival margin to the base of the pocket in millimeters. The clinical attachment levels were calculated from the recession and probing depth measures and represented as the distance in millimeters from the cementoenamel junction to the base of the pocket.
Sample collection
Venous blood was withdrawn from the participants selected for the study. The subjects were informed, and consent was taken. They were made to tighten a fist so that vein was more palpable, and antecubital vein was selected for venipuncture. A tourniquet was applied about 1-2 inches above the antecubital fossa. After cleansing the puncture site with 10% isopropanol solution, blood was withdrawn using a syringe with 24 gauge needle. Tourniquet was released as the blood flow began. After drawing 3 mL of blood, sterile cotton ball was placed on the puncture site and needle was withdrawn. The subjects were instructed to apply mild finger pressure on the site for few minutes to avoid oozing out of blood.
C-reactive protein determination
Samples were centrifuged in the centrifuge machine at 3000 rpm for 10 min to separate the serum from blood. Separated serum was collected in eppendrof and stored in the deep freeze at - 20°. Quantitative determination of CRP in patient's serum was done by double antibody sandwich enzyme-linked immunosorbent assay (ELISA) method (ICLA, USA).
Principle of the assay
Quantitative determination of CRP in patient's serum was done by double antibody sandwich ELISA method. In this assay, the CRP present in sample reacts with anti-CRP antibodies, which had been adsorbed to the surface of polystyrene microtiter wells. After the removal of unbound sample proteins by washing, anti-CRP antibodies conjugated with horseradish peroxidise were added. These enzyme- labeled antibodies form complexes with the previously bound sample CRP. Following another washing step, the enzyme bound to the immunosorbent is assayed by the addition of a chromogenic substrate, 3, 3’, 5, 5’-tetramethylbenzidine. The quantity of bound enzyme varies directly with a concentration of CRP in the test sample.
The quantity of CRP in test sample can be interpolated from the standard curve constructed from standard and corrected for serum dilution.
Statistical analysis
Data were presented as mean, standard deviation and 95% confidence interval of the mean difference. Comparison of three groups (CGP, GAP, and NP) with respect to CRP values was done using one-way analysis of variance (ANOVA). Correlation between variables was found by using Pearson's correlation coefficient “r”, and all levels of significance were set at P < 0.05.
Results
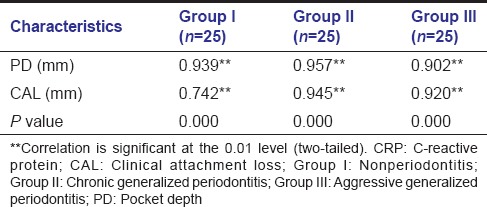
The demographic characteristics of the three groups were summarized in Table 1. Clinical parameters and mean CRP levels were summarized in Table 2. The mean CRP (mg/L) levels for the GAP, CGP and NP groups were 4.61 ± 0.58, 2.31 ± 0.56 and 0.96 ± 0.13, respectively. CRP values of the three patient groups were significantly different from each other, with CRP levels in the group III greater than those in the group II, which were in turn greater than those in the group I subjects. Furthermore, comparison of three groups (CGP, GAP, and NP) with respect to CRP values by one-way ANOVA showed statistical significance (P < 0.0001), as shown in Table 3a. Furthermore, multiple comparisons of all groups with respect to CRP values by ANOVA [Table 3b] illustrated statistical significance. Correlation coefficient between CRP and PD was 0.939, 0.957, 0.902 and with CAL 0.742, 0.945 and 0.920 in group I, II and III respectively, thus indicating a positive correlation [Table 4]. Again, they were significantly correlated, and all the parameters increased with increasing CRP levels, thus indicating a positive correlation.
Table 1.
Subject characteristics
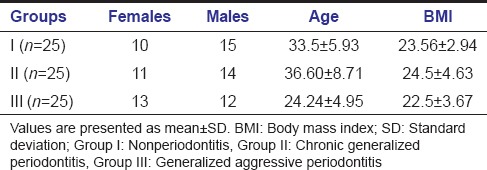
Table 2.
Clinical parameters and serum CRP levels in subjects
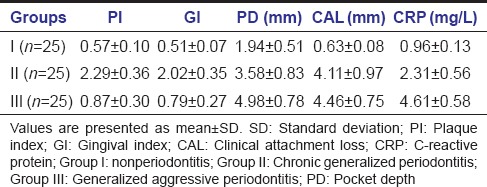
Table 3a.
One-way ANOVA showing comparison between and within groups
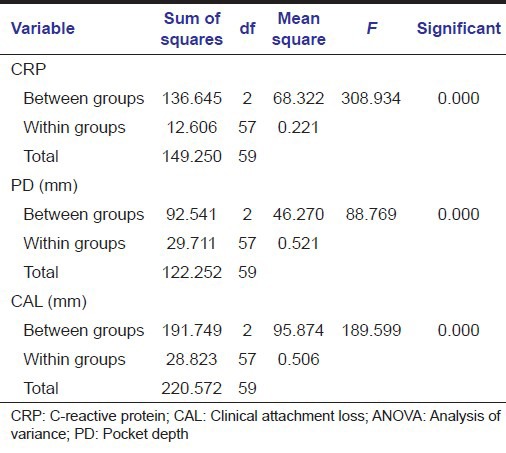
Table 3b.
Multiple comparison
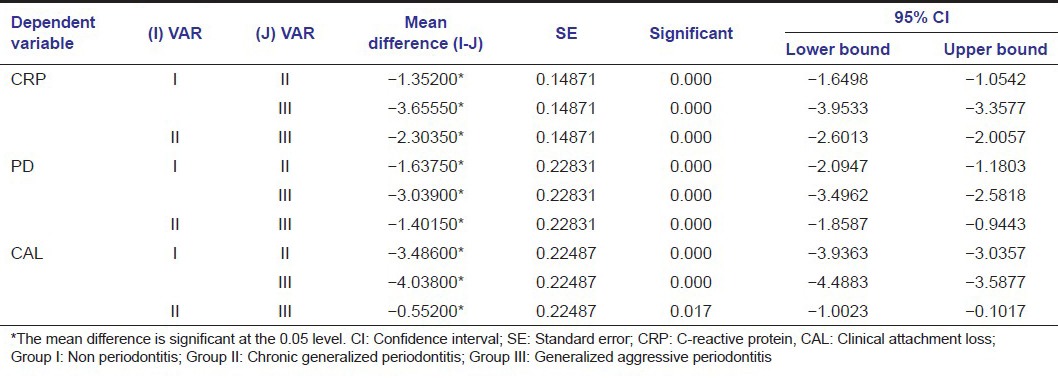
Table 4.
Correlation of CRP with PD and CAL
Discussion
Main finding of the study was that CRP levels were higher in the periodontitis group as compared with NP group and highest in subjects with aggressive periodontitis demonstrating that periodontitis can have impact on systemic markers of inflammation in a relatively younger subject group. CRP levels correlated positively with the severity of inflammation as it is biologically plausible that inflammatory cytokines interleukin-6 (IL-6), IL-1, and tumor necrosis factor-alpha in response to periodontal infection present the capacity to stimulate hepatocyte to produce CRP. Circulating CRP levels are markers of systemic inflammation and are associated with periodontal disease.[17] Also of significance are the results of prospective longitudinal trials which indicate that this marker appears to be a useful predictor for future cardiovascular events in a variety of population.[18] All the subjects included in the study were systemically healthy, and all the other risk factors for periodontitis were excluded. The aggressive periodontitis subject group displays younger age range than that seen in studies of chronic periodontitis. Strength of the study was that the quantitative determination of CRP was done by double antibody sandwich ELISA method which is very sensitive method for detecting CRP as compared to other methods with a detection limit of 0.0005-0.005 mg/L.[19] Another strength of the study was that the results of the present study indicate a significant correlation between attachment loss, probing depth and CRP, which is consistent with findings of Noack et al.[20] as some studies did not find a correlation with severity of disease.[21,22,23] In a study reported by Salzberg et al.[11] patients with GAP had increased levels of CRP (3.72 mg/L) compared to control (1.54 mg/L). Sun et al.[12] reported 1.87 and 0.52 mg/L in patients with GAP and control subjects, respectively. The mean CRP (mg/L) level for chronic periodontitis patients was 2.3 1 ± 0.56 mg/L and for aggressive periodontitis patients was 4.61 ± 0.58 mg/L, as compared to the NP group with 0.96 ± 0.13 mg/L. Comparison of three groups (CGP, GAP, and NP) with respect to CRP values by one-way ANOVA showed statistical significance (P < 0.0001) as observed in Table 3a, which confirms the results of the previous studies[11,12,13,14] but the controversy regarding the mechanism of linkage between periodontitis and elevated CRP remains. Our findings were in contrast with findings of Kanaparthy et al.[15] where mean levels of CRP were greater in chronic periodontitis subjects when compared to aggressive periodontitis, which could be attributed to long standing nature of the disease and its influence on systemic health. Moreover, there lies genetic susceptibility towards inflammatory hyperactivity, which is beyond the scope of this study.[9] The correlation coefficient between CRP levels and PD as well as CAL in CGP was found to be positive and significant. With increasing mean PD and CAL, we could observe an increase in CRP levels. These findings are at par with those of a study done by Beck and Offenbacher.[24] Thus, as the severity and extent of periodontal disease increase, the systemic component of inflammation also increases. This may be seen as increased production of CRP.[14] One more strength of the study was complete periodontal examination had been performed to classify the patients into two groups of periodontitis which ensures that there were less chances of diagnosing false positive cases of periodontitis. None of the subjects in this study had CRP levels >15 mg/L, indicating that it is relatively unlikely that the subjects were experiencing acute or chronic systemic diseases characterized by large increases in serum CRP. Similar results were found in another study, in which Lim et al. concluded that CRP was a significant predictor of sites with PD ≥5 mm and could be a potential risk marker in periodontal destruction.[25] CRP tends to increase with age but the elevation of CRP in relatively younger subjects of the present study may correlate with periodontal destruction rather than with age.[26] Thus, serum CRP levels can be a possible marker to depict active periodontal destruction and can differentiate progressive disease from a quiescent one. Recently, CRP has been proved to be the strongest and most significant predictor of future cardiovascular events.[27,28] The results of the present study suggest that elevated CRP levels in periodontitis patients can contribute at least in part to the increased risk for CVD. This may be of particular concern in younger individuals, as represented by GAP patients where elevated levels of CRP due to periodontitis may contribute to early or rapider CVD in susceptible individuals. This study shows an association between elevated serum CRP level, PD and CAL, but due to its cross-sectional nature, effect of each variable upon other can’t be determined. For better understanding, the nature of association long-term longitudinal studies is needed. Limited sample size, the role of genetics, oral health behaviors, nutrition, stress levels, which have been shown to affect the prevalence of periodontitis, were not considered in our study. From our study, we can conclude that periodontitis is related with the severity of inflammation, so it is empirical to treat the periodontal inflammation but recommending periodontal therapy solely for the purpose of preventing CVD is not supported by current evidence of literature. Recommendations by American Heart Association states that patients should be educated about oral health as no one is systemically healthy without possessing good oral health.
Conclusion
Thus, there is a complementary need to recognize that apparently healthy individuals may be having extensive periodontal disease, which might be adding to systemic inflammation. Hence, periodontal disease assessment and its treatment should be instituted in current health programs to improve the overall health status of an individual. It should be noted, however that an additional study in larger samples of patients might further investigate and confirm this idea.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.de Maat MP, Kluft C. Determinants of C-reactive protein concentration in blood. Ital Heart J. 2001;2:189–95. [PubMed] [Google Scholar]
- 2.Ablij H, Meinders A. C-reactive protein: history and revival. Eur J Intern Med. 2002;13:412. doi: 10.1016/s0953-6205(02)00132-2. [DOI] [PubMed] [Google Scholar]
- 3.Kushner I. C-reactive protein in rheumatology. Arthritis Rheum. 1991;34:1065–8. doi: 10.1002/art.1780340819. [DOI] [PubMed] [Google Scholar]
- 4.Ridker PM. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation. 2003;107:363–9. doi: 10.1161/01.cir.0000053730.47739.3c. [DOI] [PubMed] [Google Scholar]
- 5.Ridker PM. High-sensitivity C-reactive protein: Potential adjunct for global risk assessment in the primary prevention of cardiovascular disease. Circulation. 2001;103:1813–8. doi: 10.1161/01.cir.103.13.1813. [DOI] [PubMed] [Google Scholar]
- 6.Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, 3rd, Criqui M, et al. Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107:499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 7.Janket SJ, Baird AE, Chuang SK, Jones JA. Meta-analysis of periodontal disease and risk of coronary heart disease and stroke. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:559–69. doi: 10.1067/moe.2003.107. [DOI] [PubMed] [Google Scholar]
- 8.Meurman JH, Sanz M, Janket SJ. Oral health, atherosclerosis, and cardiovascular disease. Crit Rev Oral Biol Med. 2004;15:403–13. doi: 10.1177/154411130401500606. [DOI] [PubMed] [Google Scholar]
- 9.Slade GD, Offenbacher S, Beck JD, Heiss G, Pankow JS. Acute-phase inflammatory response to periodontal disease in the US population. J Dent Res. 2000;79:49–57. doi: 10.1177/00220345000790010701. [DOI] [PubMed] [Google Scholar]
- 10.Bretz WA, Weyant RJ, Corby PM, Ren D, Weissfeld L, Kritchevsky SB, et al. Systemic inflammatory markers, periodontal diseases, and periodontal infections in an elderly population. J Am Geriatr Soc. 2005;53:1532–7. doi: 10.1111/j.1532-5415.2005.53468.x. [DOI] [PubMed] [Google Scholar]
- 11.Salzberg TN, Overstreet BT, Rogers JD, Califano JV, Best AM, Schenkein HA. C-reactive protein levels in patients with aggressive periodontitis. J Periodontol. 2006;77:933–9. doi: 10.1902/jop.2006.050165. [DOI] [PubMed] [Google Scholar]
- 12.Sun XJ, Meng HX, Shi D, Xu L, Zhang L, Chen ZB, et al. Elevation of C-reactive protein and interleukin-6 in plasma of patients with aggressive periodontitis. J Periodontal Res. 2009;44:311–6. doi: 10.1111/j.1600-0765.2008.01131.x. [DOI] [PubMed] [Google Scholar]
- 13.Wohlfeil M, Scharf S, Siegelin Y, Schacher B, Oremek GM, Sauer-Eppel H, et al. Increased systemic elastase and C-reactive protein in aggressive periodontitis (CLOI-D-00160R2) Clin Oral Investig. 2012;16:1199–207. doi: 10.1007/s00784-011-0627-7. [DOI] [PubMed] [Google Scholar]
- 14.Chopra R, Patil SR, Mathur S. Comparison of cardiovascular disease risk in two main forms of periodontitis. Dent Res J (Isfahan) 2012;9:74–9. doi: 10.4103/1735-3327.92953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanaparthy A, Kanaparthy R, Niranjan N. Evaluation of serum C-reactive protein levels in subjects with aggressive and chronic periodontitis and comparison with healthy controls. Dent Res J (Isfahan) 2012;9:261–5. [PMC free article] [PubMed] [Google Scholar]
- 16.Chopra R, Patil SR, Kalburgi NB, Mathur S. Association between alveolar bone loss and serum C-reactive protein levels in aggressive and chronic periodontitis patients. J Indian Soc Periodontol. 2012;16:28–31. doi: 10.4103/0972-124X.94600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pitiphat W, Joshipura KJ, Rich-Edwards JW, Williams PL, Douglass CW, Gillman MW. Periodontitis and plasma C-reactive protein during pregnancy. J Periodontol. 2006;77:821–5. doi: 10.1902/jop.2006.050193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saito T, Shimazaki Y, Kiyohara Y, Kato I, Kubo M, Iida M, et al. Relationship between obesity, glucose tolerance, and periodontal disease in Japanese women: The Hisayama study. J Periodontal Res. 2005;40:346–53. doi: 10.1111/j.1600-0765.2005.00813.x. [DOI] [PubMed] [Google Scholar]
- 19.Hokama Y, Nobuhara WK, Munemasa K, Young PM, Kimura LH. Comparative sensitivity of an enzyme immunoassay (EIA) and other routine immunological methods for C-reactive protein (CRP) analysis in plasma: EIA examination of cancer plasma. Am Assoc Cancer Res Proc. 1984;25:285. [Google Scholar]
- 20.Noack B, Genco RJ, Trevisan M, Grossi S, Zambon JJ, De Nardin E. Periodontal infections contribute to elevated systemic C-reactive protein level. J Periodontol. 2001;72:1221–7. doi: 10.1902/jop.2000.72.9.1221. [DOI] [PubMed] [Google Scholar]
- 21.Yamazaki K, Honda T, Oda T, Ueki-Maruyama K, Nakajima T, Yoshie H, et al. Effect of periodontal treatment on the C-reactive protein and proinflammatory cytokine levels in Japanese periodontitis patients. J Periodontal Res. 2005;40:53–8. doi: 10.1111/j.1600-0765.2004.00772.x. [DOI] [PubMed] [Google Scholar]
- 22.Mattila K, Vesanen M, Valtonen V, Nieminen M, Palosuo T, Rasi V, et al. Effect of treating periodontitis on C-reactive protein levels: A pilot study. BMC Infect Dis. 2002;2:30. doi: 10.1186/1471-2334-2-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Loos BG, Craandijk J, Hoek FJ, Wertheim-van Dillen PM, van der Velden U. Elevation of systemic markers related to cardiovascular diseases in the peripheral blood of periodontitis patients. J Periodontol. 2000;71:1528–34. doi: 10.1902/jop.2000.71.10.1528. [DOI] [PubMed] [Google Scholar]
- 24.Beck JD, Offenbacher S. Relationships among clinical measures of periodontal disease and their associations with systemic markers. Ann Periodontol. 2002;7:79–89. doi: 10.1902/annals.2002.7.1.79. [DOI] [PubMed] [Google Scholar]
- 25.Lim LP, Tay FB, Sum CF, Thai AC. Relationship between markers of metabolic control and inflammation on severity of periodontal disease in patients with diabetes mellitus. J Clin Periodontol. 2007;34:118–23. doi: 10.1111/j.1600-051X.2006.01032.x. [DOI] [PubMed] [Google Scholar]
- 26.Tobe K, Ogura T, Tsukamoto C, Inoue H, Arata J, Matsuura K. Effect of change in body mass index on morbidity in non-obese university graduates. Acta Med Okayama. 2002;56:149–58. doi: 10.18926/AMO/31718. [DOI] [PubMed] [Google Scholar]
- 27.Joshipura KJ, Rimm EB, Douglass CW, Trichopoulos D, Ascherio A, Willett WC. Poor oral health and coronary heart disease. J Dent Res. 1996;75:1631–6. doi: 10.1177/00220345960750090301. [DOI] [PubMed] [Google Scholar]
- 28.Persson GR, Pettersson T, Ohlsson O, Renvert S. High-sensitivity serum C-reactive protein levels in subjects with or without myocardial infarction or periodontitis. J Clin Periodontol. 2005;32:219–24. doi: 10.1111/j.1600-051X.2005.00648.x. [DOI] [PubMed] [Google Scholar]


