Abstract
Exophytic growth of the oral cavity often presents a diagnostic challenge because a diverse group of the pathologic process can produce such lesions. Inflammatory hyperplasia is one of the important etiology behind the exophytic growths of the oral cavity. The pyogenic granuloma (PG) is the most common type of inflammatory hyperplasia found in the oral cavity especially in the gingiva. Extragingival occurrence of PG is very rare. This case report has described an extragingival PG which occurred on the lower labial mucosa in a 54-year-old male patient.
Keywords: Inflammatory hyperplasia, lobular capillary hemangioma, pyogenic granuloma
Introduction
Pyogenic granuloma (PG) is a well-known and common benign mucocutaneous lesion that occurs as a reactive inflammatory hyperplasia due to exuberant tissue response to local irritation or trauma. It is important to note here that this condition is neither associated with pus nor does it represent a granuloma histologically.[1] In fact, on the basis of the histopathological picture alone, it is invariably called lobular capillary hemangioma.[2] Clinically, these lesions usually present as single nodule or sessile papule with smooth or lobulated surface and are red, elevated and usually ulcerated.[3,4] The peak prevalence is in teenagers and young adults, with a female predilection of 2:16.[4,5] PGs of the oral cavity are known to involve the gingiva commonly. Uncommonly it can occur on the lips, tongue, buccal mucosa and palate.[4,5,6] This paper presents an unusual presentation of PG of the lower lip where many lesions of the oral mucosa with similar clinical characteristics were considered before arriving at a final diagnosis through biopsy.
Case Report
A 54-year-old male patient reported to the Department of Oral Medicine and Radiology, with a chief complaint of a growth on his lower lip causing hindrance in speech and mastication since 2 months. The growth was initially of a peanut size, which had gradually grown and had attained the present size. Patient is a smoker and gutka chewer since 15 years.
Examination revealed a pedunculated, exophytic growth on the mucosal surface of the lower lip measuring about 3 cm × 3 cm in diameter, the surface was lobulated and covered by a yellowish white pseudomembrane with some areas of ulceration [Figures 1 and 2]. The growth was firm in consistency and nontender. Intraorally, Grade III mobility was present i.r.t 31 and 41 with severe attrition and moderate amounts of stains and calculus. Based on the duration, considering the patient's age and clinical features a working diagnosis of benign minor salivary gland tumor was given. A differential diagnosis of traumatic fibroma and PG were also considered.
Figure 1.

A lobulated exophytic growth on the mucosal surface of the lower lip
Figure 2.

Exophytic growth showing the pedunculation
An excisional biopsy was carried out under antibiotic coverage along with the extraction of lower anterior root stumps. Biopsy results showed areas of ulcerated stratified squamous keratinized epithelium with underlying granulation tissue. Numerous varied caliber of blood vessels arranged in lobular pattern were seen in the connective tissue [Figures 3 and 4] suggestive of lobular capillary hemangioma, a histological terminology for PG.
Figure 3.
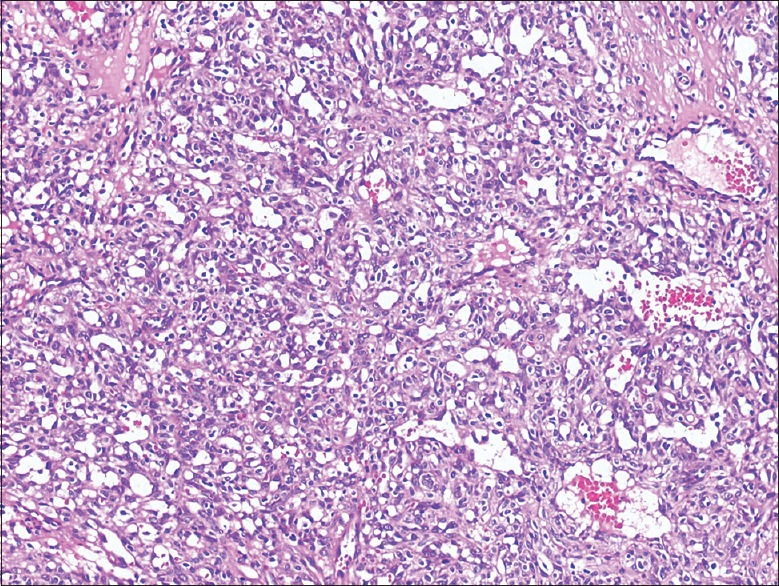
H and E stained micropictograph shows ulcerated stratified squamous keratinized epithelium with underlying granulation tissue. Numerous varied caliber of blood vessels arranged in lobular pattern is seen in the connective tissue
Figure 4.
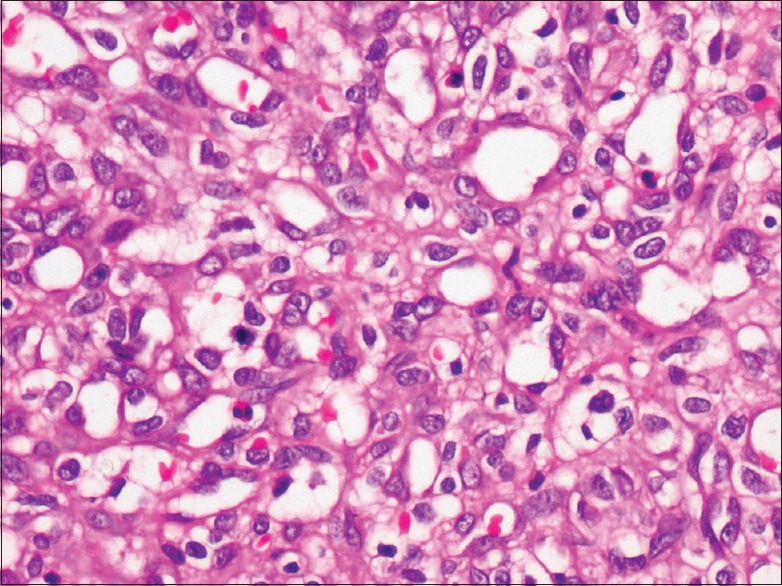
H and E stained section shows numerous blood vessels of varying size lined by endothelial cells. Few dilated blood vessels are also seen (×40). There is endothelial cell proliferation admixed with mixed inflammatory cell infiltrate
Postexcision period was uneventful with a regular follow-up of 1 month interval, which showed no evidence of recurrence for a period of 1-year.
Discussion
Pyogenic granuloma of the oral cavity is a relatively common entity first described by Poncet and Dor in 1897 as human botryomycosis. Hullihen's description in 1844 was most likely the first PG reported in English literature, but the term “PG” or “granuloma pyogenicum” was introduced by Hartzell in 1904.[7] The incidence of PG has been described to be between 26.8% and 32% of all the reactive lesions.[7] PG occurs most commonly in the gingiva. Other sites include extragingival areas such as lips, tongue, and buccal mucosa. Jafarzadeh et al., defined PG as an inflammatory overgrowth of the oral mucosa, which was caused by minor trauma or irritation.[7] According to Nevill et al., these injuries may be caused in the mouth by a gingival inflammation, which was caused due to a poor oral hygiene, trauma, or a local infection.[3] In the present case, consistent trauma inflicted by the lip biting, as a result of mobility in lower teeth may be the cause for the lesion in this location.
Originally, PGs were believed to be botryomycotic infection, which was transmitted from horse to man. Subsequently, it was proposed that these lesions are caused due to some pyogenic bacteria like streptococci and staphylococci. However, there is no evidence of any infectious organisms isolated from the lesions confirming the unlikely relation to any infection and hence the name is a misnomer.[1] The tissues react in a characteristic manner resulting in overzealous proliferation of the vascular type of connective tissue. The reason attributed to such connective tissue proliferation varies from trauma to hormonal factors, which along with poor oral hygiene cause tissue irritation and inflammation and contribute to the lesion development.[8] The increased incidence of these lesions during pregnancy may be related to the increased levels of estrogen and progesterone. The hormonal imbalance coincident with pregnancy heightens the organism's response to irritation; however, bacterial plaque and gingival inflammation are necessary for subclinical hormone alterations leading to gingivitis and PG formation. The pathogenesis of PG at the molecular level may be considered as the imbalance of the angiogenesis enhancers and inhibitors. There is over production of the vascular endothelial growth factor; the basic fibroblast growth factor and decreased amounts of angiostatin, thrombopsondin-1, and the estrogen receptors lead to the formation of PG.[9]
Clinically, the lesion typically appears as red to pink nodular growth depending upon the duration and vascularity of the lesion.[4] The surface of the lesion can show areas of erythema and ulceration as was seen in the present case, which indicate impingement of the lesion during functions like speech and mastication.
Although PG can be diagnosed clinically, atypical presentations lead to inappropriate diagnosis and should be further investigated by biopsy to rule out any other serious lesions. The histopathology of extragingival PG is similar to that occurring in the gingiva, showing proliferating vascular core in the connective tissue stroma with acute and chronic inflammatory infiltrates depending upon the etiology and duration of the lesion. Depending on its rate of proliferation and vascularity, there are two histological variants of PG called lobular capillary hemangioma (LCH type) and non-LCH type. Numerous small and larger endothelium-lined channels are formed; that are engorged with red blood cells. These vessels are sometimes organized in lobular aggregates and some pathologists look for this lobular arrangement to make a diagnosis of lobular capillary hemangioma.
In view of its clinical characteristics, the differential diagnosis of PG includes peripheral giant cell granuloma, peripheral ossifying fibroma, irritation or traumatic fibroma, benign salivary gland tumor, and non-Hodgkin's lymphoma. PG is treated conservatively by surgical excision. Surgical excision and removal of causative irritants are among the choice of treatment. Other forms of treatment include neodymium-doped yttrium aluminum garnet laser, flash lamp pulsed dye laser, cryosurgery, intralesional injection of ethanol or corticosteroid and sodium tetradecyl sulfate sclerotherapy have been produced.[10]
Conclusion
Although PG can be diagnosed clinically, atypical presentations lead to inappropriate diagnosis and should be further investigated by biopsy to rule any other serious lesions, before the final diagnosis is made, and adequate treatment is instituted.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Shafer WG, Hine MK, Levy BM. 5th ed. Amsterdam: Elsevier Health Sciences; 2006. Shafer's Textbook of Oral Pathology; pp. 459–61. [Google Scholar]
- 2.Wood NK, Goaz PW. Textbook of Differential Diagnosis of Oral and Maxillofacial Leions. 5th ed. USA: Mosby; 1997. pp. 32–4. [Google Scholar]
- 3.Neville BW, Damm DD, Allen CM, Bouquot JE. 2nd ed. Philadelphia: W.B. Saunders Co; 2004. Oral and Maxillofacial Pathology; pp. 444–9. [Google Scholar]
- 4.Regezi JA, Sciubba JJ, Jordan RC. 4th ed. Philadelphia: WB Saunders; 2003. Oral Pathology: Clinical Pathologic Considerations; pp. 115–6. [Google Scholar]
- 5.Eversole LR. 3rd ed. London: B C Decker, Hamilton; 2002. Clinical Outline of Oral Pathology: Diagnosis and Treatment; pp. 113–4. [Google Scholar]
- 6.Patil K, Mahima VG, Lahari K. Extragingival pyogenic granuloma. Indian J Dent Res. 2006;17:199–202. doi: 10.4103/0970-9290.29864. [DOI] [PubMed] [Google Scholar]
- 7.Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: A review. J Oral Sci. 2006;48:167–75. doi: 10.2334/josnusd.48.167. [DOI] [PubMed] [Google Scholar]
- 8.Shenoy SS, Dinkar AD. Pyogenic granuloma associated with bone loss in an eight year old child: A case report. J Indian Soc Pedod Prev Dent. 2006;24:201–3. doi: 10.4103/0970-4388.28078. [DOI] [PubMed] [Google Scholar]
- 9.Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: Various concepts of etiopathogenesis. J Oral Maxillofac Pathol. 2012;16:79–82. doi: 10.4103/0973-029X.92978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kamala KA, Ashok L, Sujatha GP. Pyogenic granuloma on the upper labial mucosa: A case report. J Clin Diagn Res. 2013;7:1244–6. doi: 10.7860/JCDR/2013/4539.3024. [DOI] [PMC free article] [PubMed] [Google Scholar]


