Abstract
Treacher Collins syndrome (TCS) or Franceschetti syndrome is an autosomal dominant disorder of craniofacial development with variable phenotypic expression. It presents with characteristic facial appearance enabling it to be easily recognizable. A case of a 10-year-old girl having TCS is briefly described in this article. A review of the etiology, clinical features, differential diagnosis, and treatment options are also discussed.
Keywords: Berry's syndrome, mandibulofacial dysostosis, Treacher Collins syndrome
Introduction
Treacher Collins syndrome (TCS) otherwise known as mandibulofacial dysostosis is a congenital disorder of craniofacial development that occurs with an incidence of 1 in 50,000 live births.[1] Early descriptions were attributed to Berry (1889), Treacher Collins (1900) and Franceschetti and Klein (1949) and hence the names Berry's syndrome and Franceschetti–Zwahlen–Klein syndrome. From the structures affected and from studies in mice exposed to teratogenic cis or trans-retinoic acid, it has been deducted that the disease results from interference in the development of the first and second branchial arches (Gorlin et al. 1990).[2,3]
This syndrome may appear under different clinical types. Antimongoloid palpebral fissures, malar hypoplasia, mandibular hypoplasia, malformation of auricular pinna, coloboma of the lower eyelids, conductive deafness, and cleft palate are among the most frequent clinical presentations.[4]
Case Report
A 10-year-old girl reported to the Department of Pediatric Dentistry with the chief complaint of decayed teeth. Examination revealed downward slanting of eyes, depressed zygomatic arches, sunken cheekbones, deformed external ears, coloboma of lower eyelid and retruded chin giving a bird-like appearance. Nasal septum was deviated [Figure 1].
Figure 1.

Clinical features of Treacher Collins syndrome
Mouth opening was limited to 18 mm and the path of closure was deviated to the right side.
Intraoral examination revealed Class III molar relationship with anterior open bite, crowding of maxillary and mandibular anterior teeth, high arched palate with submucosal cleft and deep dentinal caries in relation to teeth 75 and 36 [Figure 1]. Habit of mouth breathing and tongue thrusting was present.
Low birth weight, frequent episodes of fever during childhood and delayed speech were elicited from a detailed case history.
Orthopantamogram showed underdeveloped condylar and coronoid processes, hypoplastic zygomatic arches and short rami [Figure 2].
Figure 2.
Short rami and anterior crowding
Functional abnormalities included difficulties in swallowing and hearing and impaired vision. A subsequent ENT consultation revealed absence of middle ear on the right side and conductive hearing loss. The child's father also had similar phenotypic features like antimongoloid palpebral fissures; deficient malar prominence and anterior open bite [Figures 3 and 4].
Figure 3.

Father with Treacher Collins syndrome, but in milder form
Figure 4.
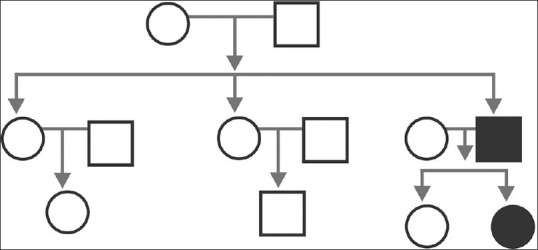
Pedigree analysis
Based on phenotypic and radiographic findings the diagnosis of TCS was made.
The cephalometric analysis showed reduced anterior cranial base length, decreased the ramal height and mandibular length. Extraction of 75, apexification of 36 and distraction osteogenesis followed by comprehensive orthodontic therapy were planned.
Discussion
Treacher Collins syndrome exhibits autosomal dominant inheritance with variable penetrance. It is caused by mutation of the TCOF1 gene, which exhibit linkage to human chromosome 5q32 locus. TCOF1 gene encodes a nuclear phosphoprotein “Treacle” that may serve as a link between rRNA gene transcription and pre-rRNA processing. Recently Dauwerse et al. detected mutations in genes encoding subunits of RNA polymerases I and III in Treacher Collins patients. More than 60% of TCS cases have no family history and arise, as a result of de novo mutation. In 40%, the mutation may be inherited from the parents.[5,6] The present case has shown the positive family history suggesting familial mutation transfer in TCOF1 gene, which is seen in 40% of cases.
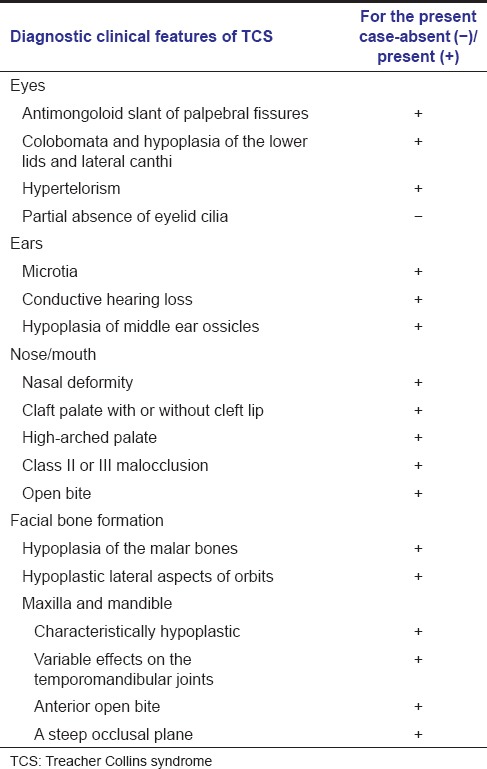
Diagnostic features of TCS include abnormalities in eyes, ears, nose/mouth, and facial bone. Vast majority [Table 1] of these features were present in this case. Based on these clinical features five clinical forms of TCS have been identified by Franceshetti and Klein.[7] They are the complete form (having all known features), an incomplete form (presenting with less severe ear, eye, zygoma, and mandibular abnormalities), the abortive form (only the lower lid pseudo coloboma and zygoma hypoplasia are present), the unilateral form (anomalies limited to only one side of the face) and the atypical form (combined with other abnormalities not usually part of this syndrome). In our case, the patient presented the incomplete form of this syndrome. Kasat and Baldawa in their article on TCS describes the obligatory features of TCS given by Axelsson et al. in 1963 which include antimongoloid palpebral fissures, anomaly of the lower eyelid, hypoplasia of malar bones and hypoplasia of mandible.[8] All these obligatory features were also seen in our case.
Table 1.
Features of TCS
Differential diagnosis of TCS includes acrofacial dysostosis (Nager and Miller syndrome) and oculoauriculovertebral spectrum (hemifacial microsomia and Goldenhar syndrome). Nager syndrome has similar facial features of TCS. In addition, thumbs may be hypoplastic, aplastic or duplicated, and the radius and ulna may be fused. Miller syndrome also has features in common with TCS, with the additional diagnostic feature of ectropion or out turning of the lower lids. The cleft lip, with or without cleft palate is more common than in TCS.[1,7]
Hemifacial microsomia primarily affects the development of the ear, mouth, and mandible. Goldenhar syndrome shows vertebral abnormalities, epibulbar dermoids and facial deformities.[2,9,10] Since this case had all the features of TCS and no additional features like hypoplastic thumb, fusion of radius and ulna, ectropion of lower lids, cleft lip, vertebral anomalies, etc., we came up with the diagnosis of TCS.
There is no cure for TCS. Treatment is aimed at the specific needs of each individual. Many children require a multidisciplinary approach involving a craniofacial team, comprising of a pediatric otolaryngologist, audiologist, plastic surgeon, geneticist, psychologist, dental surgeons, and other healthcare professionals. Genetic counseling is highly recommended for affected individuals and their families.
Conclusion
Every case of TCS is unique and needs to be assessed individually. Many features of the disease can be improved by surgery and other supportive treatments. A well-planned treatment can produce excellent results for complete restoration of the form and function of the patient. When confirmed with TCS, it is important to pay particular attention to the psychological needs too. This would in turn help to build self-esteem in a child, thereby enabling him to lead a normal life.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Marszalek B, Wójcicki P, Kobus K, Trzeciak WH. Clinical features, treatment and genetic background of Treacher Collins syndrome. J Appl Genet. 2002;43:223–33. [PubMed] [Google Scholar]
- 2.Gorlin RJ, Cohen MM, Jr, Levin LS. 3rd ed. New York: Oxford University Press; 1990. Syndromes of the Head and Neck; pp. 649–52. [Google Scholar]
- 3.Posnick JC, Ruiz RL. Treacher Collins syndrome: Current evaluation, treatment, and future directions. Cleft Palate Craniofac J. 2000;37:434. doi: 10.1597/1545-1569(2000)037<0434:TCSCET>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Andrade EC, Júnior VS, Didoni AL, Freitas PZ, Carneiro AF, Yoshimoto FR. Treacher Collins Syndrome with choanal atresia: A case report and review of disease features. Braz J Otorhinolaryngol. 2005;71:107–10. doi: 10.1016/S1808-8694(15)31296-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dauwerse JG, Dixon J, Seland S, Ruivenkamp CA, van Haeringen A, Hoefsloot LH, et al. Mutations in genes encoding subunits of RNA polymerases I and III cause Treacher Collins syndrome. Nat Genet. 2011;43:20–2. doi: 10.1038/ng.724. [DOI] [PubMed] [Google Scholar]
- 6.Conte C, D’Apice MR, Rinaldi F, Gambardella S, Sangiuolo F, Novelli G. Novel mutations of TCOF1 gene in European patients with Treacher Collins syndrome. BMC Med Genet. 2011;12:125. doi: 10.1186/1471-2350-12-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kothari P. Treacher Collins syndrome – A case report. Webmed Central Dent. 2012;3:WMC002902. [Google Scholar]
- 8.Kasat V, Baldawa R. Treacher Collins syndrome – A case report and review of literature. J Clin Exp Dent. 2011;3:E395–9. [Google Scholar]
- 9.Shete P, Tupkari J, Benjamin T, Singh A. Treacher Collins syndrome. J Oral Maxillofac Pathol. 2011;15:348–51. doi: 10.4103/0973-029X.86722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trainor PA, Dixon J, Dixon MJ. Treacher Collins syndrome: Etiology, pathogenesis and prevention. Eur J Hum Genet. 2009;17:275–83. doi: 10.1038/ejhg.2008.221. [DOI] [PMC free article] [PubMed] [Google Scholar]


