Abstract
Periodontal diagnosis and treatment plan are based on the assessment of probing depth, clinical attachment level, plaque index, gingival index, bleeding on probing, suppuration, furcation involvement, mobility, and radiographic findings. However, these clinical parameters are not sufficiently sensitive and specific to identify disease activity in individual sites or to predict future attachment loss. Hence, attention is focused on the development of diagnostic tools that could screen and differentiate the active inflamed sites and predict future tissue destruction. Gingival crevicular fluid (GCF), has gained great interest on possible diagnostic value in periodontal disease. It contains a large number of proteins and peptides derived from inflamed host tissues. The analysis of the GCF components can reflect the disease status of individual sites and thus, identify potential biomarkers of periodontitis. A literature search was carried out to find out all the available tests that indicate periodontal disease markers in GCF. All major databases were searched to compile the information on published reports between 1999 and 2014. The list of GCF-biomarkers available to date is compiled and presented in a table format. Based on the available literature on GCF biomarkers, it can be concluded that several sensitive and reliable markers are present to detect the presence, severity, and response to treatment. Further studies are warranted to analyze the sensitivity and reliability of these indicators which might help in developing noninvasive tests that could help in the diagnosis of periodontal disease.
Keywords: Biological markers, gingival crevicular fluid, periodontal disease
Introduction
Periodontitis is characterized by the destruction of connective tissue, loss of periodontal attachment, and resorption of alveolar bone. The tissue destruction in periodontal disease appears as a result from the interplay between the pathogenic bacteria and the host’s immune and inflammatory responses. The immune system is activated in order to protect against local microbial attack and their damaging products from spreading or invading the gingival tissues. This defense mechanism might be harmful to the host, by destroying surrounding cells and connective tissue structures.1 Diagnosis of the diseases affecting the periodontium and assessing its outcomes are based on clinical signs such as tissue color and contour, the presence or absence of bleeding on probing, gingival recession, probing pocket depths, attachment levels, suppuration, and tooth mobility.2 Radiographs are used as an additional tool to visualize the loss of periodontal tissue, by determining the amount of bone loss around the teeth.3 However, these methods are only useful to assess the past disease activity. Reliable diagnostic methods are essential to assess the active disease status and for monitoring the response to periodontal therapy.4
Gingival crevicular fluid (GCF) is a complex mixture of substances derived from serum, host inflammatory cells, structural cells of the periodontium, and oral bacteria. GCF originates from the vessels of the gingival plexus of blood vessels and flows through the external basement membrane and the junctional epithelium to reach the gingival sulcus. GCF can be isolated from healthy sulcus, although only in small amounts. In the healthy periodontium, GCF represents the transudate of gingival tissue interstitial fluid produced by an osmotic gradient.5 The products of the inflammatory response which occur during the disease process can be found in the GCF. Monitoring of the presence of such components can be of potential value in evaluating periodontal disease status or outcomes of periodontal therapy.6
Current understanding of the pathogenesis of periodontal disease showed a wide variation in the magnitude of the inflammatory response suggesting a high risk subgroup of periodontitis with rapid progression. Factors such as smoking, diabetes, psychological stress, reduced serum antibodies, or biochemical mediators of inflammation may also contribute to disease progression. Hence, the severity and progression of diseases have been linked to a combination of genetic, host response, microbial challenge, and the local environmental factors.
Biomarkers of disease have gained considerable attention during the past decade. These markers generally fall into three categories:
Indicators of current disease activity;
Predictors of future disease progression;
Predictors of future disease initiation at currently healthy sites.
The potential biomarkers in the GCF have been grouped into three general categories (Table 1):
Table 1.
Host-derived enzymes in GCF.
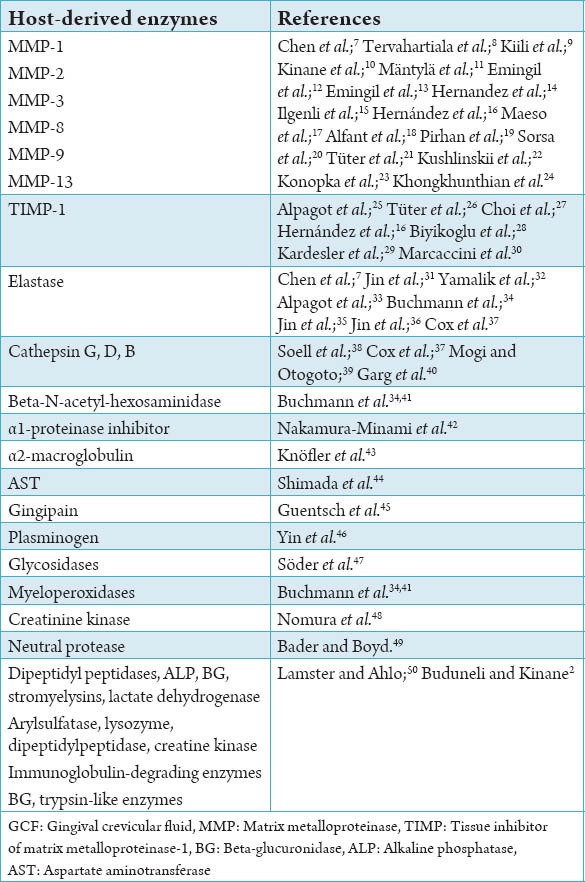
Host-derived enzymes
Inflammatory mediators and products
Tissue-breakdown products.
Since the GCF accumulates at the gingival margin, it contains potential markers derived not only from the host tissues and serum, but also from the subgingival microbial plaque. The changes in the GCF constituents could be used as a potential marker in the periodontitis progression.
The objective of the current review is to critically analyze the current understanding of the various constituents in the GCF that are used as biomarkers and the future developments that could help to establish noninvasive diagnostic aid in this area.
Materials and Methods
The review was conducted in January 2014. All relevant studies published between, January 1999 to January 2014 were identified and included in the article. Two authors independently searched the Medline, EMBASE, Cochrane Library, Web of Science, Google Scholar, and Scopus databases for relevant studies. The search was carried out using a combined text and the MeSH search strategies: Using the key words; “periodontitis” and “GCF,” “biomarkers” and “early detection of periodontitis.” We also examined the bibliographies from identified studies, reviews, and gray literature. The last search was conducted on January 31, 2014. Studies reporting the use of any biomarkers in the GCF for diagnostic or prognostic aspect of periodontitis is included and summarized in the article. The scope of using these biomarkers as chair side test is critically analyzed.
Discussion
Host-derived enzymes in GCF
Enzymes, especially proteinases, play a central part in the control of periodontal tissue turnover in health and tissue destruction in periodontitis.
Aspartate aminotransferase (AST)
AST is a soluble enzyme that is released to the extracellular environment upon cell death.51 The level of AST is elevated at sites with active periodontitis.52 Clinical attachment loss and inflammation have shown a marked elevation of AST in GCF.53
Alkaline phosphatase (ALP)
ALP is a membrane-bound glycoprotein produced by many cells, such as leukocytes, osteoblasts, macrophages, and fibroblasts. Bacteria present in the sulcus or pocket also produce ALP and contribute to ALP levels in GCF. ALP in GCF has been suggested as a potential diagnostic marker for periodontitis.54,55
Nakashima et al.54 found a positive correlation between crevicular fluid ALP levels from active sites than in the inactive sites with periodontitis. However, ALP levels in GCF as a marker of periodontal disease diagnosis are limited.4
Beta-glucuronidase (BG)
BG is one of the enzymes involved in the destruction of noncollagenous components of the extracellular matrix and is considered as an indicator or predictor of periodontal disease activity.56 BG contributes to noncollagenous matrix degradation in periodontal disease, and its activity might be a good indicator or predictor of periodontal disease.57,58
Elastase
Elastase is released from polymorphonuclears (PMNs) to the gingival crevice as a result of host-microbial interactions. It is considered as a risk factor for the development of periodontitis. Elevated levels of GCF elastase enzyme have been reported in periodontitis.33
Cathepsin B
Cathepsin B is a cysteine proteinases enzyme and in GCF, it originates specifically from macrophages. The level of cathepsin B in the GCF was found to be elevated in patients with periodontitis.59 It has shown a direct correlation to the severity of periodontitis.60 The level of cathepsin in the GCF can be used as an indicator of the attachment loss and also as a prognostic indicator in periodontal disease.61
Matrix metalloproteinases (MMPs)
MMPs are a family of enzymes that are responsible for the degradation of extracellular matrix components such as collagen, proteoglycans, laminin, elastin, and fibronectin. They play a central role in the periodontal ligament (PDL) remodeling, both in physiological and pathological conditions. MMP-8, in conjunction with MMP-9 and functional granulocyte elastase, is involved in tissue destruction in subjects with periodontal disease.47 The bacterial plaque induces the initial infiltrate of inflammatory cells in the gingival crevice including macrophages and lymphocytes.
These activated inflammatory cells produce inflammatory mediators which stimulate the production of MMPs from fibroblasts, epithelial cells, and PMNs.
Leptin
Leptin is involved in the host response, which stimulates the immune system by enhancing pro inflammatory cytokine production and phagocytosis by macrophages. Hence, during infection and inflammation, leptin expression is modulated in a manner similar to the cytokine response to infection and injury.62 During gingival inflammation, the concentration of leptin is decreased as a result of the expansion of the vascular network caused by vascular endothelial growth factor, which may increase the net rate of leptin removal from the gingival tissues.63 Studies have shown that the leptin levels in GCF decreased with the progression of periodontal disease and could be used as an indicator.64,65
Hepatocyte growth factor (HGF)
HGF is known to be a multi-functional cytokine involved in a variety of physiological processes, including tissue development, regeneration, and wound healing.66 HGF plays an important role in the progression of periodontitis, by stimulating intense growth of epithelial cells and preventing regeneration of the connective tissue attachment. HGF is well-known as a serum marker indicating disease activity in various diseases, including periodontitis.67 An association between HGF and periodontitis has been reported earlier.68,69 A higher level of HGF in GCF was expressed at periodontally compromised sites.70,71
Inflammatory mediators and host response modifiers (Table 2)
Table 2.
Inflammatory mediators and host response modifiers.
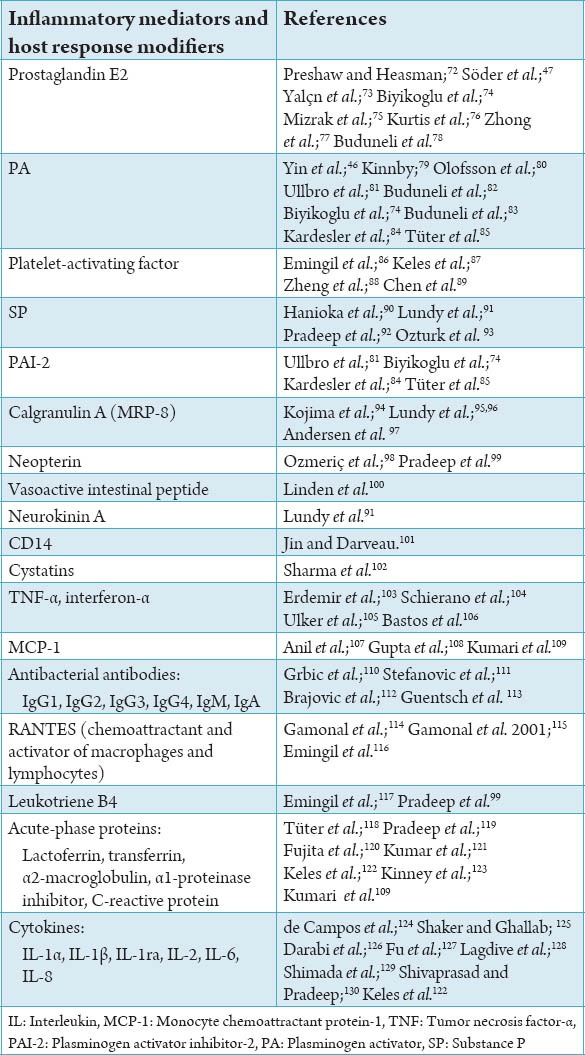
Cytokines
Cytokines are important modulators of both normal and pathologic processes within the periodontium. The analysis of cytokine production levels has been also used as a tool for studying the local host response to bacterial challenge.
Cytokines present in the GCF have been proposed as potentially useful diagnostic or prognostic markers of periodontal destruction. Of these, interleukin-1b (IL-1b), IL-4, and IL-8 have been shown to function in concert with other members of the cytokine network to regulate the cellular inflammatory response in the periodontium.
Substance P (SP)
SP is localized in sensory nerves that innervate blood vessels. SP is a member of the tachykinin family of these neuropeptides, and it is stored in the secretory granules of sensory neurons and their peripheral branches. Release of SP in human gingiva was related to periodontal inflammation. The SP level in GCF is correlated with the degree of periodontal inflammation, and it has been shown that a reduction in inflammation as a result of effective periodontal treatment is associated with a reduction in the levels of undecapeptide SP in GCF.90-92
Tumor necrosis factor-a (TNF-a)
TNF-α is a proinflammatory cytokine that is often over expressed in periodontitis and is responsible for alveolar bone resorption during periodontitis.131
Monocyte chemo-attractant protein (MCP)
MCP-1, a potent mediator of both monocyte recruitment and activation. MCP-1 is expressed by monocytes, endothelial cells, fibroblasts, and T-cells, primarily on the basal layer of epithelial tissues. MCP-1 is related to the stages of oral infection by means of its monocyte chemotactic ability, which has been known to increase with increasing inflammation. High levels of MCP-1 have been reported in the GCF of both aggressive and chronic periodontitis patients.107,116,132
The MCP activity in GCF increases with the advancement of periodontitis and could be involved in the mechanism of monocyte recruitment from the circulating pool into periodontal tissues.
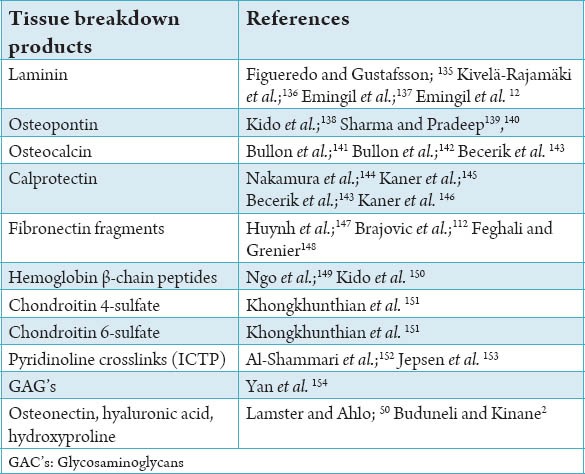
Tissue breakdown products (Table 3)
Table 3.
Tissue breakdown products.
Laminin
In the oral cavity, laminin is expressed mainly in epithelial cells which stimulates the migration of epithelial cells and, in the formation of periodontal pockets in the progression of periodontitis, is believed to be one of the key factors in the apical migration of epithelial cells.133 PDL fibroblasts demonstrate enhanced expression of some other laminin isoforms.134 Several laminin isoforms are involved in the procession of periodontal inflammatory diseases and tissue remodeling.135
Osteopontin (OPN)
OPN is a major glycosylated phosphoprotein in bone matrix and is produced by several cells including osteoblasts, osteoclasts, and macrophages. Studies have reported an increased level of GCF OPN in periodontitis and its reduction after periodontal therapy.138-140
Osteocalcin (OC)
OC is a noncollagenous matrix protein of calcifying and calcified tissue.155 It is produced by osteoblasts and has been described as the most specific marker of osteoblast function.156 Structurally, it binds to both major bone components (collagen and apatite) and is believed to play a role in both bone resorption and mineralization.
OC has been found in GCF from patients with periodontal disease, and increases in GCF OC concentration were associated with high rates of bone turnover.
Raised levels of GCF OC are reported in adult periodontitis may be related to the severity of breakdown and/or repair of alveolar bone. During active bone resorption, OC and OC fragments are likely to be released from the extracellular matrix into the GCF. Nakashima et al.54 reported the mean concentration of OC in GCF was ten-fold than that found in serum and speculated that OC was produced locally by periodontal tissues. Several investigations on OC levels in GCF from patients with periodontitis have been reported, suggesting that OC levels in GCF may reflect inflammation at diseased sites and there has been recent interest in OC as a potential marker of bone turnover in periodontal disease.141,142
Conclusion
GCF, which is an exudate that can be harvested from the sulcus or periodontal pocket, has been regarded as a promising medium for the detection of periodontal disease activity. The composition of this fluid resembles that of serum, and the intensity of its flow has been shown to vary as a function of gingival inflammation. GCF has been used as a medium to measure a variety of molecules and bacteria present in both the oral cavity and the PDL space. GCF contains a variety of substances including immunoglobulins, microorganisms, toxins, cells, and lysosomal enzymes and markers the immune and inflammatory reactions arising from periodontitis.
Footnotes
Conflict of Interest: None
Source of Support: Nil
References
- 1.Madianos PN, Bobetsis YA, Kinane DF. Generation of inflammatory stimuli: How bacteria set up inflammatory responses in the gingiva. J Clin Periodontol. 2005;32(Suppl 6):57–71. doi: 10.1111/j.1600-051X.2005.00821.x. [DOI] [PubMed] [Google Scholar]
- 2.Buduneli N, Kinane DF. Host-derived diagnostic markers related to soft tissue destruction and bone degradation in periodontitis. J Clin Periodontol. 2011;38(Suppl 11):85–105. doi: 10.1111/j.1600-051X.2010.01670.x. [DOI] [PubMed] [Google Scholar]
- 3.Brägger U. Radiographic parameters: Biological significance and clinical use. Periodontol 2000. 2005;39:73–90. doi: 10.1111/j.1600-0757.2005.00128.x. [DOI] [PubMed] [Google Scholar]
- 4.Loos BG, Tjoa S. Host-derived diagnostic markers for periodontitis: Do they exist in gingival crevice fluid? Periodontol 2000. 2005;39:53–72. doi: 10.1111/j.1600-0757.2005.00129.x. [DOI] [PubMed] [Google Scholar]
- 5.Alfano MC. The origin of gingival fluid. J Theor Biol. 1974;47(1):127–36. doi: 10.1016/0022-5193(74)90103-9. [DOI] [PubMed] [Google Scholar]
- 6.Toker H, Marakoglu I, Poyraz O. Effect of meloxicam on gingival crevicular fluid IL-1beta and IL1 receptor antagonist levels in subjects with chronic periodontitis, and its effects on clinical parameters. Clin Oral Investig. 2006;10(4):305–10. doi: 10.1007/s00784-006-0062-3. [DOI] [PubMed] [Google Scholar]
- 7.Chen HY, Cox SW, Eley BM, Mäntylä P, Rönkä H, Sorsa T. Matrix metalloproteinase-8 levels and elastase activities in gingival crevicular fluid from chronic adult periodontitis patients. J Clin Periodontol. 2000;27(5):366–9. doi: 10.1034/j.1600-051x.2000.027005366.x. [DOI] [PubMed] [Google Scholar]
- 8.Tervahartiala T, Pirilä E, Ceponis A, Maisi P, Salo T, Tuter G, et al. The in vivo expression of the collagenolytic matrix metalloproteinases (MMP-2, -8, -13, and -14) and matrilysin (MMP-7) in adult and localized juvenile periodontitis. J Dent Res. 2000;79(12):1969–77. doi: 10.1177/00220345000790120801. [DOI] [PubMed] [Google Scholar]
- 9.Kiili M, Cox SW, Chen HY, Wahlgren J, Maisi P, Eley BM, et al. Collagenase-2 (MMP-8) and collagenase-3 (MMP-13) in adult periodontitis: Molecular forms and levels in gingival crevicular fluid and immunolocalisation in gingival tissue. J Clin Periodontol. 2002;29(3):224–32. doi: 10.1034/j.1600-051x.2002.290308.x. [DOI] [PubMed] [Google Scholar]
- 10.Kinane DF, Darby IB, Said S, Luoto H, Sorsa T, Tikanoja S, et al. Changes in gingival crevicular fluid matrix metalloproteinase-8 levels during periodontal treatment and maintenance. J Periodontal Res. 2003;38(4):400–4. doi: 10.1034/j.1600-0765.2003.00663.x. [DOI] [PubMed] [Google Scholar]
- 11.Mäntylä P, Stenman M, Kinane DF, Tikanoja S, Luoto H, Salo T, et al. Gingival crevicular fluid collagenase-2 (MMP-8) test stick for chair-side monitoring of periodontitis. J Periodontal Res. 2003;38(4):436–9. doi: 10.1034/j.1600-0765.2003.00677.x. [DOI] [PubMed] [Google Scholar]
- 12.Emingil G, Kuula H, Pirilä E, Atilla G, Sorsa T. Gingival crevicular fluid laminin-5 gamma2-chain levels in periodontal disease. J Clin Periodontol. 2006;33(7):462–8. doi: 10.1111/j.1600-051X.2006.00933.x. [DOI] [PubMed] [Google Scholar]
- 13.Emingil G, Kuula H, Sorsa T, Atilla G. Gingival crevicular fluid matrix metalloproteinase-25 and -26 levels in periodontal disease. J Periodontol. 2006;77(4):664–71. doi: 10.1902/jop.2006.050288. [DOI] [PubMed] [Google Scholar]
- 14.Hernandez M, Valenzuela MA, Lopez-Otin C, Alvarez J, Lopez JM, Vernal R, et al. Matrix metalloproteinase-13 is highly expressed in destructive periodontal disease activity. J Periodontol. 2006;77(11):1863–70. doi: 10.1902/jop.2006.050461. [DOI] [PubMed] [Google Scholar]
- 15.Ilgenli T, Vardar-Sengul S, Gürkan A, Sorsa T, Stackelberg S, Köse T, et al. Gingival crevicular fluid matrix metalloproteinase-13 levels and molecular forms in various types of periodontal diseases. Oral Dis. 2006;12(6):573–9. doi: 10.1111/j.1601-0825.2006.01244.x. [DOI] [PubMed] [Google Scholar]
- 16.Hernández M, Martínez B, Tejerina JM, Valenzuela MA, Gamonal J. MMP-13 and TIMP-1 determinations in progressive chronic periodontitis. J Clin Periodontol. 2007;34(9):729–35. doi: 10.1111/j.1600-051X.2007.01107.x. [DOI] [PubMed] [Google Scholar]
- 17.Maeso G, Bravo M, Bascones A. Levels of metalloproteinase-2 and -9 and tissue inhibitor of matrix metalloproteinase-1 in gingival crevicular fluid of patients with periodontitis, gingivitis, and healthy gingiva. Quintessence Int. 2007;38(3):247–52. [PubMed] [Google Scholar]
- 18.Alfant B, Shaddox LM, Tobler J, Magnusson I, Aukhil I, Walker C. Matrix metalloproteinase levels in children with aggressive periodontitis. J Periodontol. 2008;79(5):819–26. doi: 10.1902/jop.2008.070513. [DOI] [PubMed] [Google Scholar]
- 19.Pirhan D, Atilla G, Emingil G, Sorsa T, Tervahartiala T, Berdeli A. Effect of MMP-1 promoter polymorphisms on GCF MMP-1 levels and outcome of periodontal therapy in patients with severe chronic periodontitis. J Clin Periodontol. 2008;35(10):862–70. doi: 10.1111/j.1600-051X.2008.01302.x. [DOI] [PubMed] [Google Scholar]
- 20.Sorsa T, Hernández M, Leppilahti J, Munjal S, Netuschil L, Mäntylä P. Detection of gingival crevicular fluid MMP-8 levels with different laboratory and chair-side methods. Oral Dis. 2010;16(1):39–45. doi: 10.1111/j.1601-0825.2009.01603.x. [DOI] [PubMed] [Google Scholar]
- 21.Tüter G, Serdar M, Kurtis B, Walker SG, Atak A, Toyman U, et al. Effects of scaling and root planing and subantimicrobial dose doxycycline on gingival crevicular fluid levels of matrix metalloproteinase-8, -13 and serum levels of HsCRP in patients with chronic periodontitis. J Periodontol. 2010;81(8):1132–9. doi: 10.1902/jop.2010.090694. [DOI] [PubMed] [Google Scholar]
- 22.Kushlinskii NE, Solovykh EA, Karaoglanova TB, Bayar U, Gershtein ES, Troshin AA, et al. Content of matrix metalloproteinase-8 and matrix metalloproteinase-9 in oral fluid of patients with chronic generalized periodontitis. Bull Exp Biol Med. 2011;152(2):240–4. doi: 10.1007/s10517-011-1498-2. [DOI] [PubMed] [Google Scholar]
- 23.Konopka L, Pietrzak A, Brzezinska-Blaszczyk E. Effect of scaling and root planing on interleukin-1ß, interleukin-8 and MMP-8 levels in gingival crevicular fluid from chronic periodontitis patients. J Periodontal Res. 2012;47(6):681–8. doi: 10.1111/j.1600-0765.2012.01480.x. [DOI] [PubMed] [Google Scholar]
- 24.Khongkhunthian S, Techasatian P, Supanchart C, Bandhaya P, Montreekachon P, Thawanaphong S, et al. Elevated levels of a disintegrin and metalloproteinase 8 in gingival crevicular fluid of patients with periodontal diseases. J Periodontol. 2013;84(4):520–8. doi: 10.1902/jop.2012.120262. [DOI] [PubMed] [Google Scholar]
- 25.Alpagot T, Bell C, Lundergan W, Chambers DW, Rudin R. Longitudinal evaluation of GCF MMP-3 and TIMP-1 levels as prognostic factors for progression of periodontitis. J Clin Periodontol. 2001;28(4):353–9. doi: 10.1034/j.1600-051x.2001.028004353.x. [DOI] [PubMed] [Google Scholar]
- 26.Tüter G, Kurtis B, Serdar M. Effects of phase I periodontal treatment on gingival crevicular fluid levels of matrix metalloproteinase-1 and tissue inhibitor of metalloproteinase-1. J Periodontol. 2002;73(5):487–93. doi: 10.1902/jop.2002.73.5.487. [DOI] [PubMed] [Google Scholar]
- 27.Choi DH, Moon IS, Choi BK, Paik JW, Kim YS, Choi SH, et al. Effects of sub-antimicrobial dose doxycycline therapy on crevicular fluid MMP-8, and gingival tissue MMP-9, TIMP-1 and IL-6 levels in chronic periodontitis. J Periodontal Res. 2004;39(1):20–6. doi: 10.1111/j.1600-0765.2004.00696.x. [DOI] [PubMed] [Google Scholar]
- 28.Biyikoglu B, Buduneli N, Kardesler L, Aksu K, Pitkala M, Sorsa T. Gingival crevicular fluid MMP-8 and -13 and TIMP-1 levels in patients with rheumatoid arthritis and inflammatory periodontal disease. J Periodontol. 2009;80(8):1307–14. doi: 10.1902/jop.2009.090130. [DOI] [PubMed] [Google Scholar]
- 29.Kardesler L, Biyikoglu B, Cetinkalp S, Pitkala M, Sorsa T, Buduneli N. Crevicular fluid matrix metalloproteinase-8, -13, and TIMP-1 levels in type 2 diabetics. Oral Dis. 2010;16(5):476–81. doi: 10.1111/j.1601-0825.2010.01659.x. [DOI] [PubMed] [Google Scholar]
- 30.Marcaccini AM, Meschiari CA, Zuardi LR, de Sousa TS, Taba M, Jr, Teofilo JM, et al. Gingival crevicular fluid levels of MMP-8, MMP-9, TIMP-2, and MPO decrease after periodontal therapy. J Clin Periodontol. 2010;37(2):180–90. doi: 10.1111/j.1600-051X.2009.01512.x. [DOI] [PubMed] [Google Scholar]
- 31.Jin L, Söder B, Corbet EF. Interleukin-8 and granulocyte elastase in gingival crevicular fluid in relation to periodontopathogens in untreated adult periodontitis. J Periodontol. 2000;71(6):929–39. doi: 10.1902/jop.2000.71.6.929. [DOI] [PubMed] [Google Scholar]
- 32.Yamalik N, Caglayan F, Kilinç K, Kilinç A, Tümer C. The importance of data presentation regarding gingival crevicular fluid myeloperoxidase and elastase-like activity in periodontal disease and health status. J Periodontol. 2000;71(3):460–7. doi: 10.1902/jop.2000.71.3.460. [DOI] [PubMed] [Google Scholar]
- 33.Alpagot T, Silverman S, Lundergan W, Bell C, Chambers DW. Crevicular fluid elastase levels in relation to periodontitis and metabolic control of diabetes. J Periodontal Res. 2001;36(3):169–74. doi: 10.1034/j.1600-0765.2001.360305.x. [DOI] [PubMed] [Google Scholar]
- 34.Buchmann R, Hasilik A, Van Dyke TE, Lange DE. Amplified crevicular leukocyte activity in aggressive periodontal disease. J Dent Res. 2002;81(10):716–21. doi: 10.1177/154405910208101012. [DOI] [PubMed] [Google Scholar]
- 35.Jin LJ, Leung WK, Corbet EF, Söder B. Relationship of changes in interleukin-8 levels and granulocyte elastase activity in gingival crevicular fluid to subgingival periodontopathogens following non-surgical periodontal therapy in subjects with chronic periodontitis. J Clin Periodontol. 2002;29(7):604–14. doi: 10.1034/j.1600-051x.2002.290704.x. [DOI] [PubMed] [Google Scholar]
- 36.Jin L, Yu C, Corbet EF. Granulocyte elastase activity in static and flow gingival crevicular fluid. J Periodontal Res. 2003;38(3):303–10. doi: 10.1034/j.1600-0765.2003.00606.x. [DOI] [PubMed] [Google Scholar]
- 37.Cox SW, Rodriguez-Gonzalez EM, Booth V, Eley BM. Secretory leukocyte protease inhibitor and its potential interactions with elastase and cathepsin B in gingival crevicular fluid and saliva from patients with chronic periodontitis. J Periodontal Res. 2006;41(5):477–85. doi: 10.1111/j.1600-0765.2006.00891.x. [DOI] [PubMed] [Google Scholar]
- 38.Soell M, Elkaim R, Tenenbaum H. Cathepsin C, matrix metalloproteinases, and their tissue inhibitors in gingiva and gingival crevicular fluid from periodontitis-affected patients. J Dent Res. 2002;81(3):174–8. [PubMed] [Google Scholar]
- 39.Mogi M, Otogoto J. Expression of cathepsin-K in gingival crevicular fluid of patients with periodontitis. Arch Oral Biol. 2007;52(9):894–8. doi: 10.1016/j.archoralbio.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 40.Garg G, Pradeep AR, Thorat MK. Effect of nonsurgical periodontal therapy on crevicular fluid levels of Cathepsin K in periodontitis. Arch Oral Biol. 2009;54(11):1046–51. doi: 10.1016/j.archoralbio.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 41.Buchmann R, Hasilik A, Van Dyke TE, Lange DE. Resolution of crevicular fluid leukocyte activity in patients treated for aggressive periodontal disease. J Periodontol. 2002;73(9):995–1002. doi: 10.1902/jop.2002.73.9.995. [DOI] [PubMed] [Google Scholar]
- 42.Nakamura-Minami M, Furuichi Y, Ishikawa K, Mitsuzono-Tofuku Y, Izumi Y. Changes of alpha1-protease inhibitor and secretory leukocyte protease inhibitor levels in gingival crevicular fluid before and after non-surgical periodontal treatment. Oral Dis. 2003;9(5):249–54. doi: 10.1034/j.1601-0825.2003.02884.x. [DOI] [PubMed] [Google Scholar]
- 43.Knöfler G, Purschwitz R, Jentsch H, Birkenmeier G, Schmidt H. Gingival crevicular fluid levels of aspartate aminotransferase and alpha2-macroglobulin before and after topical application of metronidazole or scaling and root planing. Quintessence Int. 2008;39(5):381–9. [PubMed] [Google Scholar]
- 44.Shimada K, Mizuno T, Ohshio K, Kamaga M, Murai S, Ito K. Analysis of aspartate aminotransferase in gingival crevicular fluid assessed by using PocketWatch: A longitudinal study with initial therapy. J Clin Periodontol. 2000;27(11):819–23. doi: 10.1034/j.1600-051x.2000.027011819.x. [DOI] [PubMed] [Google Scholar]
- 45.Guentsch A, Kramesberger M, Sroka A, Pfister W, Potempa J, Eick S. Comparison of gingival crevicular fluid sampling methods in patients with severe chronic periodontitis. J Periodontol. 2011;82(7):1051–60. doi: 10.1902/jop.2011.100565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yin X, Bunn CL, Bartold PM. Detection of tissue plasminogen activator (t-PA) and plasminogen activator inhibitor 2(PAI-2) in gingival crevicular fluid from healthy, gingivitis and periodontitis patients. J Clin Periodontol. 2000;27(3):149–56. doi: 10.1034/j.1600-051x.2000.027003149.x. [DOI] [PubMed] [Google Scholar]
- 47.Söder B, Jin LJ, Wickholm S. Granulocyte elastase, matrix metalloproteinase-8 and prostaglandin E2 in gingival crevicular fluid in matched clinical sites in smokers and non-smokers with persistent periodontitis. J Clin Periodontol. 2002;29(5):384–91. doi: 10.1034/j.1600-051x.2002.290502.x. [DOI] [PubMed] [Google Scholar]
- 48.Nomura Y, Tamaki Y, Tanaka T, Arakawa H, Tsurumoto A, Kirimura K, et al. Screening of periodontitis with salivary enzyme tests. J Oral Sci. 2006;48(4):177–83. doi: 10.2334/josnusd.48.177. [DOI] [PubMed] [Google Scholar]
- 49.Bader HI, Boyd RL. Neutral proteases in crevicular fluid as an indicator for periodontal treatment intervention. Am J Dent. 2001;14(5):314–8. [PubMed] [Google Scholar]
- 50.Lamster IB, Ahlo JK. Analysis of gingival crevicular fluid as applied to the diagnosis of oral and systemic diseases. Ann N Y Acad Sci. 2007;1098:216–29. doi: 10.1196/annals.1384.027. [DOI] [PubMed] [Google Scholar]
- 51.Chambers DA, Crawford JM, Mukherjee S, Cohen RL. Aspartate aminotransferase increases in crevicular fluid during experimental periodontitis in beagle dogs. J Periodontol. 1984;55(9):526–30. doi: 10.1902/jop.1984.55.9.526. [DOI] [PubMed] [Google Scholar]
- 52.Paolantonio M, Di Placido G, Tumini V, Di Stilio M, Contento A, Spoto G. Aspartate aminotransferase activity in crevicular fluid from dental implants. J Periodontol. 2000;71(7):1151–7. doi: 10.1902/jop.2000.71.7.1151. [DOI] [PubMed] [Google Scholar]
- 53.Persson GR, DeRouen TA, Page RC. Relationship between gingival crevicular fluid levels of aspartate aminotransferase and active tissue destruction in treated chronic periodontitis patients. J Periodontal Res. 1990;25(2):81–7. doi: 10.1111/j.1600-0765.1990.tb00896.x. [DOI] [PubMed] [Google Scholar]
- 54.Nakashima K, Roehrich N, Cimasoni G. Osteocalcin, prostaglandin E2 and alkaline phosphatase in gingival crevicular fluid: Their relations to periodontal status. J Clin Periodontol. 1994;21(5):327–33. doi: 10.1111/j.1600-051x.1994.tb00721.x. [DOI] [PubMed] [Google Scholar]
- 55.Daltaban O, Saygun I, Bal B, Balos K, Serdar M. Gingival crevicular fluid alkaline phosphatase levels in postmenopausal women: Effects of phase I periodontal treatment. J Periodontol. 2006;77(1):67–72. doi: 10.1902/jop.2006.77.1.67. [DOI] [PubMed] [Google Scholar]
- 56.Lamster IB, Holmes LG, Gross KB, Oshrain RL, Cohen DW, Rose LF, et al. The relationship of beta-glucuronidase activity in crevicular fluid to clinical parameters of periodontal disease. Findings from a multicenter study. J Clin Periodontol. 1994;21(2):118–27. doi: 10.1111/j.1600-051x.1994.tb00289.x. [DOI] [PubMed] [Google Scholar]
- 57.Lamster IB, Oshrain RL, Harper DS, Celenti RS, Hovliaras CA, Gordon JM. Enzyme activity in crevicular fluid for detection and prediction of clinical attachment loss in patients with chronic adult periodontitis. Six month results. J Periodontol. 1988;59(8):516–23. doi: 10.1902/jop.1988.59.8.516. [DOI] [PubMed] [Google Scholar]
- 58.Chung RM, Grbíc JT, Lamster IB. Interleukin-8 and beta-glucuronidase in gingival crevicular fluid. J Clin Periodontol. 1997;24(3):146–52. doi: 10.1111/j.1600-051x.1997.tb00483.x. [DOI] [PubMed] [Google Scholar]
- 59.Ichimaru E, Tanoue M, Tani M, Tani Y, Kaneko T, Iwasaki Y, et al. Cathepsin B in gingival crevicular fluid of adult periodontitis patients: Identification by immunological and enzymological methods. Inflamm Res. 1996;45(6):277–82. doi: 10.1007/BF02280991. [DOI] [PubMed] [Google Scholar]
- 60.Eley BM, Cox SW. The relationship between gingival crevicular fluid cathepsin B activity and periodontal attachment loss in chronic periodontitis patients: A 2-year longitudinal study. J Periodontal Res. 1996;31(6):381–92. doi: 10.1111/j.1600-0765.1996.tb00507.x. [DOI] [PubMed] [Google Scholar]
- 61.Chen HY, Cox SW, Eley BM. Cathepsin B, alpha2-macroglobulin and cystatin levels in gingival crevicular fluid from chronic periodontitis patients. J Clin Periodontol. 1998;25(1):34–41. doi: 10.1111/j.1600-051x.1998.tb02361.x. [DOI] [PubMed] [Google Scholar]
- 62.Ahima RS, Flier JS. Leptin. Annu Rev Physiol. 2000;62:413–37. doi: 10.1146/annurev.physiol.62.1.413. [DOI] [PubMed] [Google Scholar]
- 63.Johnson RB, Serio FG. Leptin within healthy and diseased human gingiva. J Periodontol. 2001;72(9):1254–7. doi: 10.1902/jop.2000.72.9.1254. [DOI] [PubMed] [Google Scholar]
- 64.Karthikeyan BV, Pradeep AR. Gingival crevicular fluid and serum leptin: Their relationship to periodontal health and disease. J Clin Periodontol. 2007;34(6):467–72. doi: 10.1111/j.1600-051X.2007.01078.x. [DOI] [PubMed] [Google Scholar]
- 65.Karthikeyan BV, Pradeep AR. Leptin levels in gingival crevicular fluid in periodontal health and disease. J Periodontal Res. 2007;42(4):300–4. doi: 10.1111/j.1600-0765.2006.00948.x. [DOI] [PubMed] [Google Scholar]
- 66.Skibinski G. The role of hepatocyte growth factor/c-met interactions in the immune system. Arch Immunol Ther Exp (Warsz) 2003;51(5):277–82. [PubMed] [Google Scholar]
- 67.Lönn J, Starkhammar Johansson C, Kälvegren H, Brudin L, Skoglund C, Garvin P, et al. Hepatocyte growth factor in patients with coronary artery disease and its relation to periodontal condition. Results Immunol. 2011;2:7–12. doi: 10.1016/j.rinim.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ohshima M, Noguchi Y, Ito M, Maeno M, Otsuka K. Hepatocyte growth factor secreted by periodontal ligament and gingival fibroblasts is a major chemoattractant for gingival epithelial cells. J Periodontal Res. 2001;36(6):377–83. doi: 10.1034/j.1600-0765.2001.360605.x. [DOI] [PubMed] [Google Scholar]
- 69.Ohshima M, Sakai A, Ito K, Otsuka K. Hepatocyte growth factor (HGF) in periodontal disease: Detection of HGF in gingival crevicular fluid. J Periodontal Res. 2002;37(1):8–14. doi: 10.1034/j.1600-0765.2002.00660.x. [DOI] [PubMed] [Google Scholar]
- 70.Nagaraja C, Pradeep AR. Hepatocyte growth factor levels in gingival crevicular fluid in health, disease, and after treatment. J Periodontol. 2007;78(4):742–7. doi: 10.1902/jop.2007.060249. [DOI] [PubMed] [Google Scholar]
- 71.Rudrakshi C, Srinivas N, Mehta DS. A comparative evaluation of hepatocyte growth factor levels in gingival crevicular fluid and saliva and its correlation with clinical parameters in patients with and without chronic periodontitis: A clinico-biochemical study. J Indian Soc Periodontol. 2011;15(2):147–51. doi: 10.4103/0972-124X.84384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Preshaw PM, Heasman PA. Prostaglandin E2 concentrations in gingival crevicular fluid: Observations in untreated chronic periodontitis. J Clin Periodontol. 2002;29(1):15–20. doi: 10.1034/j.1600-051x.2002.290103.x. [DOI] [PubMed] [Google Scholar]
- 73.Yalçn S, Basegmez C, Mijiritsky E, Yalçn F, Isik G, Onan U. Detection of implant crevicular fluid prostaglandin E2 levels for the assessment of peri-implant health: A pilot study. Implant Dent. 2005;14(2):194–200. [PubMed] [Google Scholar]
- 74.Biyikoglu B, Buduneli N, Kardesler L, Aksu K, Oder G, Kütükçüler N. Evaluation of t-PA, PAI-2, IL-1beta and PGE(2) in gingival crevicular fluid of rheumatoid arthritis patients with periodontal disease. J Clin Periodontol. 2006;33(9):605–11. doi: 10.1111/j.1600-051X.2006.00961.x. [DOI] [PubMed] [Google Scholar]
- 75.Mizrak T, Güncü GN, Caglayan F, Balci TA, Aktar GS, Ipek F. Effect of a controlled-release chlorhexidine chip on clinical and microbiological parameters and prostaglandin E2 levels in gingival crevicular fluid. J Periodontol. 2006;77(3):437–43. doi: 10.1902/jop.2006.050105. [DOI] [PubMed] [Google Scholar]
- 76.Kurtis B, Tüter G, Serdar M, Pinar S, Demirel I, Toyman U. Gingival crevicular fluid prostaglandin E(2) and thiobarbituric acid reactive substance levels in smokers and non-smokers with chronic periodontitis following phase I periodontal therapy and adjunctive use of flurbiprofen. J Periodontol. 2007;78(1):104–11. doi: 10.1902/jop.2007.060217. [DOI] [PubMed] [Google Scholar]
- 77.Zhong Y, Slade GD, Beck JD, Offenbacher S. Gingival crevicular fluid interleukin-1beta, prostaglandin E2 and periodontal status in a community population. J Clin Periodontol. 2007;34(4):285–93. doi: 10.1111/j.1600-051X.2007.01057.x. [DOI] [PubMed] [Google Scholar]
- 78.Buduneli N, Buduneli E, Cetin EO, Kirilmaz L, Kütükçüler N. Clinical findings and gingival crevicular fluid prostaglandin E2 and interleukin-1-beta levels following initial periodontal treatment and short-term meloxicam administration. Expert Opin Pharmacother. 2010;11(11):1805–12. doi: 10.1517/14656566.2010.490555. [DOI] [PubMed] [Google Scholar]
- 79.Kinnby B. The plasminogen activating system in periodontal health and disease. Biol Chem. 2002;383(1):85–92. doi: 10.1515/BC.2002.008. [DOI] [PubMed] [Google Scholar]
- 80.Olofsson A, Matsson L, Kinnby B. Plasminogen activating capacity in gingival fluid from deteriorating and stable periodontal pockets. J Periodontal Res. 2002;37(1):60–5. doi: 10.1034/j.1600-0765.2002.00325.x. [DOI] [PubMed] [Google Scholar]
- 81.Ullbro C, Kinnby B, Lindberg P, Matsson L. Tissue plasminogen activator (t-PA) and placental plasminogen activator inhibitor (PAI-2) in gingival crevicular fluid from patients with Papillon-Lefèvre syndrome. J Clin Periodontol. 2004;31(9):708–12. doi: 10.1111/j.1600-051X.2004.00551.x. [DOI] [PubMed] [Google Scholar]
- 82.Buduneli N, Buduneli E, Kardesler L, Lappin D, Kinane DF. Plasminogen activator system in smokers and non-smokers with and without periodontal disease. J Clin Periodontol. 2005;32(4):417–24. doi: 10.1111/j.1600-051X.2005.00694.x. [DOI] [PubMed] [Google Scholar]
- 83.Buduneli N, Becerik S, Buduneli E, Baylas H, Kinnby B. Gingival status, crevicular fluid tissue-type plasminogen activator, plasminogen activator inhibitor-2 levels in pregnancy versus post-partum. Aust Dent J. 2010;55(3):292–7. doi: 10.1111/j.1834-7819.2010.01237.x. [DOI] [PubMed] [Google Scholar]
- 84.Kardeşler L, Buduneli N, Çetinkalp S, Lappin D, Kinane DF. Gingival crevicular fluid IL-6, tPA, PAI-2, albumin levels following initial periodontal treatment in chronic periodontitis patients with or without type 2 diabetes. Inflamm Res. 2011;60(2):143–51. doi: 10.1007/s00011-010-0248-7. [DOI] [PubMed] [Google Scholar]
- 85.Tüter G, Ozdemir B, Kurtis B, Serdar M, Yücel AA, Ayhan E. Short term effects of non-surgical periodontal treatment on gingival crevicular fluid levels of tissue plasminogen activator (t-PA) and plasminogen activator inhibitor 2 (PAI-2) in patients with chronic and aggressive periodontitis. Arch Oral Biol. 2013;58(4):391–6. doi: 10.1016/j.archoralbio.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 86.Emingil G, Cinarcik S, Baylas H, Hüseyinov A. Levels of platelet-activating factor in gingival crevicular fluid and gingival tissue in specific periodontal diseases. J Periodontol. 2001;72(8):1032–7. doi: 10.1902/jop.2001.72.8.1032. [DOI] [PubMed] [Google Scholar]
- 87.Keles GC, Cetinkaya BO, Isildak I, Koprulu H, Acikgoz G. Levels of platelet activating factor in gingival crevice fluid following periodontal surgical therapy. J Periodontal Res. 2006;41(6):513–8. doi: 10.1111/j.1600-0765.2006.00898.x. [DOI] [PubMed] [Google Scholar]
- 88.Zheng P, Chen H, Shi S, Jepsen S, Eberhard J. Periodontal parameters and platelet-activating factor levels in serum and gingival crevicular fluid in a Chinese population. J Clin Periodontol. 2006;33(11):797–802. doi: 10.1111/j.1600-051X.2006.00987.x. [DOI] [PubMed] [Google Scholar]
- 89.Chen H, Zheng P, Zhu H, Zhu J, Zhao L, El Mokhtari NE, et al. Platelet-activating factor levels of serum and gingival crevicular fluid in nonsmoking patients with periodontitis and/or coronary heart disease. Clin Oral Investig. 2010;14(6):629–36. doi: 10.1007/s00784-009-0346-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hanioka T, Takaya K, Matsumori Y, Matsuse R, Shizukuishi S. Relationship of the substance P to indicators of host response in human gingival crevicular fluid. J Clin Periodontol. 2000;27(4):262–6. doi: 10.1034/j.1600-051x.2000.027004262.x. [DOI] [PubMed] [Google Scholar]
- 91.Lundy FT, Mullally BH, Burden DJ, Lamey PJ, Shaw C, Linden GJ. Changes in substance P and neurokinin A in gingival crevicular fluid in response to periodontal treatment. J Clin Periodontol. 2000;27(7):526–30. doi: 10.1034/j.1600-051x.2000.027007526.x. [DOI] [PubMed] [Google Scholar]
- 92.Pradeep AR, Raj S, Aruna G, Chowdhry S. Gingival crevicular fluid and plasma levels of neuropeptide Substance-P in periodontal health, disease and after nonsurgical therapy. J Periodontal Res. 2009;44(2):232–7. doi: 10.1111/j.1600-0765.2008.01138.x. [DOI] [PubMed] [Google Scholar]
- 93.Ozturk A, Bilgici B, Odyakmaz S, Konas E. The relationship of periodontal disease severity to serum and GCF substance P levels in diabetics. Quintessence Int. 2012;43(7):587–96. [PubMed] [Google Scholar]
- 94.Kojima T, Andersen E, Sanchez JC, Wilkins MR, Hochstrasser DF, Pralong WF, et al. Human gingival crevicular fluid contains MRP8 (S100A8) and MRP14 (S100A9), two calcium-binding proteins of the S100 family. J Dent Res. 2000;79(2):740–7. doi: 10.1177/00220345000790020701. [DOI] [PubMed] [Google Scholar]
- 95.Lundy FT, Chalk R, Lamey PJ, Shaw C, Linden GJ. Identification of MRP-8 (calgranulin A) as a major responsive protein in chronic periodontitis. J Pathol. 2000;192(4):540–4. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH740>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 96.Lundy FT, Chalk R, Lamey PJ, Shaw C, Linden GJ. Quantitative analysis of MRP-8 in gingival crevicular fluid in periodontal health and disease using microbore HPLC. J Clin Periodontol. 2001;28(12):1172–7. doi: 10.1034/j.1600-051x.2001.281213.x. [DOI] [PubMed] [Google Scholar]
- 97.Andersen E, Dessaix IM, Perneger T, Mombelli A. Myeloid-related protein (MRP8/14) expression in gingival crevice fluid in periodontal health and disease and after treatment. J Periodontal Res. 2010;45(4):458–63. doi: 10.1111/j.1600-0765.2009.01257.x. [DOI] [PubMed] [Google Scholar]
- 98.Ozmeriç N, Baydar T, Bodur A, Engin AB, Uraz A, Eren K, et al. Level of neopterin, a marker of immune cell activation in gingival crevicular fluid, saliva, and urine in patients with aggressive periodontitis. J Periodontol. 2002;73(7):720–5. doi: 10.1902/jop.2002.73.7.720. [DOI] [PubMed] [Google Scholar]
- 99.Pradeep AR, Kumar MS, Ramachandraprasad MV, Shikha C. Gingival crevicular fluid levels of neopterin in healthy subjects and in patients with different periodontal diseases. J Periodontol. 2007;78(10):1962–7. doi: 10.1902/jop.2007.070096. [DOI] [PubMed] [Google Scholar]
- 100.Linden GJ, Mullally BH, Burden DJ, Lamey PJ, Shaw C, Ardill J, et al. Changes in vasoactive intestinal peptide in gingival crevicular fluid in response to periodontal treatment. J Clin Periodontol. 2002;29(6):484–9. doi: 10.1034/j.1600-051x.2002.290602.x. [DOI] [PubMed] [Google Scholar]
- 101.Jin L, Darveau RP. Soluble CD14 levels in gingival crevicular fluid of subjects with untreated adult periodontitis. J Periodontol. 2001;72(5):634–40. doi: 10.1902/jop.2001.72.5.634. [DOI] [PubMed] [Google Scholar]
- 102.Sharma A, Pradeep AR, Raghavendra NM, Arjun P, Kathariya R. Gingival crevicular fluid and serum cystatin c levels in periodontal health and disease. Dis Markers. 2012;32(2):101–7. doi: 10.3233/DMA-2011-0864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Erdemir EO, Duran I, Haliloglu S. Effects of smoking on clinical parameters and the gingival crevicular fluid levels of IL-6 and TNF-alpha in patients with chronic periodontitis. J Clin Periodontol. 2004;31(2):99–104. doi: 10.1111/j.0303-6979.2004.00454.x. [DOI] [PubMed] [Google Scholar]
- 104.Schierano G, Pejrone G, Brusco P, Trombetta A, Martinasso G, Preti G, et al. TNF-alpha TGF-beta2 and IL-1beta levels in gingival and peri-implant crevicular fluid before and after de novo plaque accumulation. J Clin Periodontol. 2008;35(6):532–8. doi: 10.1111/j.1600-051X.2008.01224.x. [DOI] [PubMed] [Google Scholar]
- 105.Ulker AE, Tulunoglu O, Ozmeric N, Can M, Demirtas S. The evaluation of cystatin C, IL-1beta, and TNF-alpha levels in total saliva and gingival crevicular fluid from 11- to 16-year-old children. J Periodontol. 2008;79(5):854–60. doi: 10.1902/jop.2008.070422. [DOI] [PubMed] [Google Scholar]
- 106.Bastos MF, Lima JA, Vieira PM, Mestnik MJ, Faveri M, Duarte PM. TNF-alpha and IL-4 levels in generalized aggressive periodontitis subjects. Oral Dis. 2009;15(1):82–7. doi: 10.1111/j.1601-0825.2008.01491.x. [DOI] [PubMed] [Google Scholar]
- 107.Anil S, Preethanath RS, Alasqah M, Mokeem SA, Anand PS. Increased levels of serum and gingival crevicular fluid monocyte chemoattractant protein-1 in smokers with periodontitis. J Periodontol. 2013;84(9):e23–8. doi: 10.1902/jop.2013.120666. [DOI] [PubMed] [Google Scholar]
- 108.Gupta M, Chaturvedi R, Jain A. Role of monocyte chemoattractant protein-1 (MCP-1) as an immune-diagnostic biomarker in the pathogenesis of chronic periodontal disease. Cytokine. 2013;61(3):892–7. doi: 10.1016/j.cyto.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 109.Kumari M, Pradeep AR, Priyanka N, Kalra N, Naik SB. Crevicular and serum levels of monocyte chemoattractant protein-4 and high-sensitivity C-reactive protein in periodontal health and disease. Arch Oral Biol. 2014;59(6):645–53. doi: 10.1016/j.archoralbio.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 110.Grbic JT, Lamster IB, Fine JB, Lam KS, Celenti RS, Herrera-Abreu M, et al. Changes in gingival crevicular fluid levels of immunoglobulin A following therapy: Association with attachment loss. J Periodontol. 1999;70(10):1221–7. doi: 10.1902/jop.1999.70.10.1221. [DOI] [PubMed] [Google Scholar]
- 111.Stefanovic G, Markovic D, Ilic V, Brajovic G, Petrovic S, Milosevic-Jovcic N. Hypogalactosylation of salivary and gingival fluid immunoglobulin G in patients with advanced periodontitis. J Periodontol. 2006;77(11):1887–93. doi: 10.1902/jop.2006.060049. [DOI] [PubMed] [Google Scholar]
- 112.Brajovic G, Stefanovic G, Ilic V, Petrovic S, Stefanovic N, Nikolic-Jakoba N, et al. Association of fibronectin with hypogalactosylated immunoglobulin G in gingival crevicular fluid in periodontitis. J Periodontol. 2010;81(10):1472–80. doi: 10.1902/jop.2010.100053. [DOI] [PubMed] [Google Scholar]
- 113.Guentsch A, Hirsch C, Pfister W, Vincents B, Abrahamson M, Sroka A, et al. Cleavage of IgG1 in gingival crevicular fluid is associated with the presence of Porphyromonas gingivalis. J Periodontal Res. 2013;48(4):458–65. doi: 10.1111/jre.12027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Gamonal J, Acevedo A, Bascones A, Jorge O, Silva A. Levels of interleukin-1 beta, -8, and -10 and RANTES in gingival crevicular fluid and cell populations in adult periodontitis patients and the effect of periodontal treatment. J Periodontol. 2000;71(10):1535–45. doi: 10.1902/jop.2000.71.10.1535. [DOI] [PubMed] [Google Scholar]
- 115.Gamonal J, Acevedo A, Bascones A, Jorge O, Silva A. Characterization of cellular infiltrate, detection of chemokine receptor CCR5 and interleukin-8 and RANTES chemokines in adult periodontitis. J Periodontal Res. 2001;36(3):194–203. doi: 10.1034/j.1600-0765.2001.360309.x. [DOI] [PubMed] [Google Scholar]
- 116.Emingil G, Atilla G, Hüseyinov A. Gingival crevicular fluid monocyte chemoattractant protein-1 and RANTES levels in patients with generalized aggressive periodontitis. J Clin Periodontol. 2004;31(10):829–34. doi: 10.1111/j.1600-051X.2004.00584.x. [DOI] [PubMed] [Google Scholar]
- 117.Emingil G, Cinarcik S, Baylas H, Coker I, Hüseyinov A. Levels of leukotriene B4 in gingival crevicular fluid and gingival tissue in specific periodontal diseases. J Periodontol. 2001;72(8):1025–31. doi: 10.1902/jop.2001.72.8.1025. [DOI] [PubMed] [Google Scholar]
- 118.Tüter G, Kurtis B, Serdar M. Evaluation of gingival crevicular fluid and serum levels of high-sensitivity C-reactive protein in chronic periodontitis patients with or without coronary artery disease. J Periodontol. 2007;78(12):2319–24. doi: 10.1902/jop.2007.070150. [DOI] [PubMed] [Google Scholar]
- 119.Pradeep AR, Kathariya R, Raghavendra NM, Sharma A. Levels of pentraxin-3 in gingival crevicular fluid and plasma in periodontal health and disease. J Periodontol. 2011;82(5):734–41. doi: 10.1902/jop.2010.100526. [DOI] [PubMed] [Google Scholar]
- 120.Fujita Y, Ito H, Sekino S, Numabe Y. Correlations between pentraxin 3 or cytokine levels in gingival crevicular fluid and clinical parameters of chronic periodontitis. Odontology. 2012;100(2):215–21. doi: 10.1007/s10266-011-0042-1. [DOI] [PubMed] [Google Scholar]
- 121.Kumar S, Shah S, Budhiraja S, Desai K, Shah C, Mehta D. The effect of periodontal treatment on C-reactive protein: A clinical study. J Nat Sci Biol Med. 2013;4(2):379–82. doi: 10.4103/0976-9668.116991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Keles ZP, Keles GC, Avci B, Cetinkaya BO, Emingil G. Analysis of YKL-40 Acute-Phase Protein and Interleukin-6 Levels in Periodontal Disease. J Periodontol. 2014;85(9):1240–6. doi: 10.1902/jop.2014.130631. [DOI] [PubMed] [Google Scholar]
- 123.Kinney JS, Morelli T, Oh M, Braun TM, Ramseier CA, Sugai JV, et al. Crevicular fluid biomarkers and periodontal disease progression. J Clin Periodontol. 2014;41(2):113–20. doi: 10.1111/jcpe.12194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.de Campos BO, Fischer RG, Gustafsson A, Figueredo CM. Effectiveness of non-surgical treatment to reduce il-18 levels in the gingival crevicular fluid of patients with periodontal disease. Braz Dent J. 2012;23(4):428–32. doi: 10.1590/s0103-64402012000400020. [DOI] [PubMed] [Google Scholar]
- 125.Shaker OG, Ghallab NA. IL-17 and IL-11 GCF levels in aggressive and chronic periodontitis patients: Relation to PCR bacterial detection. Mediators Inflamm. 2012;2012:174764. doi: 10.1155/2012/174764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Darabi E, Kadkhoda Z, Amirzargar A. Comparison of the levels of tumor necrosis factor-a and interleukin-17 in gingival crevicular fluid of patients with peri-implantitis and a control group with healthy implants. Iran J Allergy Asthma Immunol. 2013;12(1):75–80. [PubMed] [Google Scholar]
- 127.Fu QY, Zhang L, Duan L, Qian SY, Pang HX. Correlation of chronic periodontitis in tropical area and IFN-?, IL-10, IL-17 levels. Asian Pac J Trop Med. 2013;6(6):489–92. doi: 10.1016/S1995-7645(13)60080-2. [DOI] [PubMed] [Google Scholar]
- 128.Lagdive SS, Marawar PP, Byakod G, Lagdive SB. Evaluation and comparison of interleukin-8 (IL-8) level in gingival crevicular fluid in health and severity of periodontal disease: A clinico-biochemical study. Indian J Dent Res. 2013;24(2):188–92. doi: 10.4103/0970-9290.116675. [DOI] [PubMed] [Google Scholar]
- 129.Shimada Y, Tabeta K, Sugita N, Yoshie H. Profiling biomarkers in gingival crevicular fluid using multiplex bead immunoassay. Arch Oral Biol. 2013;58(6):724–30. doi: 10.1016/j.archoralbio.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 130.Shivaprasad BM, Pradeep AR. Effect of non-surgical periodontal therapy on interleukin-29 levels in gingival crevicular fluid of chronic periodontitis and aggressive periodontitis patients. Dis Markers. 2013;34(1):1–7. doi: 10.3233/DMA-2012-120944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Stashenko P, Van Dyke T, Tully P, Kent R, Sonis S, Tanner AC. Inflammation and genetic risk indicators for early periodontitis in adults. J Periodontol. 2011;82(4):588–96. doi: 10.1902/jop.2010.100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kurtis B, Tüter G, Serdar M, Akdemir P, Uygur C, Firatli E, et al. Gingival crevicular fluid levels of monocyte chemoattractant protein-1 and tumor necrosis factor-alpha in patients with chronic and aggressive periodontitis. J Periodontol. 2005;76(11):1849–55. doi: 10.1902/jop.2005.76.11.1849. [DOI] [PubMed] [Google Scholar]
- 133.Pöllänen MT, Salonen JI, Uitto VJ. Structure and function of the tooth-epithelial interface in health and disease. Periodontol 2000. 2003;31:12–31. doi: 10.1034/j.1600-0757.2003.03102.x. [DOI] [PubMed] [Google Scholar]
- 134.Ohshima M, Yamaguchi Y, Otsuka K, Sato M, Ishikawa M. Laminin expression by human periodontal ligament fibroblasts. Connect Tissue Res. 2006;47(3):149–56. doi: 10.1080/03008200600685475. [DOI] [PubMed] [Google Scholar]
- 135.Figueredo CM, Gustafsson A. Increased amounts of laminin in GCF from untreated patients with periodontitis. J Clin Periodontol. 2000;27(5):313–8. doi: 10.1034/j.1600-051x.2000.027005313.x. [DOI] [PubMed] [Google Scholar]
- 136.Kivelä-Rajamäki MJ, Teronen OP, Maisi P, Husa V, Tervahartiala TI, Pirilä EM, et al. Laminin-5 gamma2-chain and collagenase-2 (MMP-8) in human peri-implant sulcular fluid. Clin Oral Implants Res. 2003;14(2):158–65. doi: 10.1034/j.1600-0501.2003.140204.x. [DOI] [PubMed] [Google Scholar]
- 137.Emingil G, Atilla G, Sorsa T, Savolainen P, Baylas H. Effectiveness of adjunctive low-dose doxycycline therapy on clinical parameters and gingival crevicular fluid laminin-5 gamma2 chain levels in chronic periodontitis. J Periodontol. 2004;75(10):1387–96. doi: 10.1902/jop.2004.75.10.1387. [DOI] [PubMed] [Google Scholar]
- 138.Kido J, Nakamura T, Asahara Y, Sawa T, Kohri K, Nagata T. Osteopontin in gingival crevicular fluid. J Periodontal Res. 2001;36(5):328–33. doi: 10.1034/j.1600-0765.2001.360509.x. [DOI] [PubMed] [Google Scholar]
- 139.Sharma CG, Pradeep AR. Gingival crevicular fluid osteopontin levels in periodontal health and disease. J Periodontol. 2006;77(10):1674–80. doi: 10.1902/jop.2006.060016. [DOI] [PubMed] [Google Scholar]
- 140.Sharma CG, Pradeep AR. Plasma and crevicular fluid osteopontin levels in periodontal health and disease. J Periodontal Res. 2007;42(5):450–5. doi: 10.1111/j.1600-0765.2007.00968.x. [DOI] [PubMed] [Google Scholar]
- 141.Bullon P, Goberna B, Guerrero JM, Segura JJ, Perez-Cano R, Martinez-Sahuquillo A. Serum, saliva, and gingival crevicular fluid osteocalcin: Their relation to periodontal status and bone mineral density in postmenopausal women. J Periodontol. 2005;76(4):513–9. doi: 10.1902/jop.2005.76.4.513. [DOI] [PubMed] [Google Scholar]
- 142.Bullon P, Chandler L, Segura Egea JJ, Perez Cano R, Martinez Sahuquillo A. Osteocalcin in serum, saliva and gingival crevicular fluid: Their relation with periodontal treatment outcome in postmenopausal women. Med Oral Patol Oral Cir Bucal. 2007;12(3):E193–7. [PubMed] [Google Scholar]
- 143.Becerik S, Afacan B, Oztürk VÖ, Atmaca H, Emingil G. Gingival crevicular fluid calprotectin, osteocalcin and cross-linked N-terminal telopeptid levels in health and different periodontal diseases. Dis Markers. 2011;31(6):343–52. doi: 10.3233/DMA-2011-0849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Nakamura T, Kido J, Kido R, Ohishi K, Yamauchi N, Kataoka M, et al. The association of calprotectin level in gingival crevicular fluid with gingival index and the activities of collagenase and aspartate aminotransferase in adult periodontitis patients. J Periodontol. 2000;71(3):361–7. doi: 10.1902/jop.2000.71.3.361. [DOI] [PubMed] [Google Scholar]
- 145.Kaner D, Bernimoulin JP, Kleber BM, Heizmann WR, Friedmann A. Gingival crevicular fluid levels of calprotectin and myeloperoxidase during therapy for generalized aggressive periodontitis. J Periodontal Res. 2006;41(2):132–9. doi: 10.1111/j.1600-0765.2005.00849.x. [DOI] [PubMed] [Google Scholar]
- 146.Kaner D, Bernimoulin JP, Dietrich T, Kleber BM, Friedmann A. Calprotectin levels in gingival crevicular fluid predict disease activity in patients treated for generalized aggressive periodontitis. J Periodontal Res. 2011;46(4):417–26. doi: 10.1111/j.1600-0765.2011.01355.x. [DOI] [PubMed] [Google Scholar]
- 147.Huynh QN, Wang S, Tafolla E, Gansky SA, Kapila S, Armitage GC, et al. Specific fibronectin fragments as markers of periodontal disease status. J Periodontol. 2002;73(10):1101–10. doi: 10.1902/jop.2002.73.10.1101. [DOI] [PubMed] [Google Scholar]
- 148.Feghali K, Grenier D. Priming effect of fibronectin fragments on the macrophage inflammatory response: Potential contribution to periodontitis. Inflammation. 2012;35(5):1696–705. doi: 10.1007/s10753-012-9487-9. [DOI] [PubMed] [Google Scholar]
- 149.Ngo LH, Veith PD, Chen YY, Chen D, Darby IB, Reynolds EC. Mass spectrometric analyses of peptides and proteins in human gingival crevicular fluid. J Proteome Res. 2010;9(4):1683–93. doi: 10.1021/pr900775s. [DOI] [PubMed] [Google Scholar]
- 150.Kido J, Bando M, Hiroshima Y, Iwasaka H, Yamada K, Ohgami N, et al. Analysis of proteins in human gingival crevicular fluid by mass spectrometry. J Periodontal Res. 2012;47(4):488–99. doi: 10.1111/j.1600-0765.2011.01458.x. [DOI] [PubMed] [Google Scholar]
- 151.Khongkhunthian S, Srimueang N, Krisanaprakornkit S, Pattanaporn K, Ong-Chai S, Kongtawelert P. Raised chondroitin sulphate WF6 epitope levels in gingival crevicular fluid in chronic periodontitis. J Clin Periodontol. 2008;35(10):871–6. doi: 10.1111/j.1600-051X.2008.01312.x. [DOI] [PubMed] [Google Scholar]
- 152.Al-Shammari KF, Giannobile WV, Aldredge WA, Iacono VJ, Eber RM, Wang HL, et al. Effect of non-surgical periodontal therapy on C-telopeptide pyridinoline cross-links (ICTP) and interleukin-1 levels. J Periodontol. 2001;72(8):1045–51. doi: 10.1902/jop.2001.72.8.1045. [DOI] [PubMed] [Google Scholar]
- 153.Jepsen S, Springer IN, Buschmann A, Hedderich J, Açil Y. Elevated levels of collagen cross-link residues in gingival tissues and crevicular fluid of teeth with periodontal disease. Eur J Oral Sci. 2003;111(3):198–202. doi: 10.1034/j.1600-0722.2003.00019.x. [DOI] [PubMed] [Google Scholar]
- 154.Yan F, Marshall R, Wynne S, Xiao Y, Bartold PM. Glycosaminoglycans in gingival crevicular fluid of patients with periodontal class II furcation involvement before and after guided tissue regeneration. A pilot study. J Periodontol. 2000;71(1):1–7. doi: 10.1902/jop.2000.71.1.1. [DOI] [PubMed] [Google Scholar]
- 155.Knepper-Nicolai B, Reinstorf A, Hofinger I, Flade K, Wenz R, Pompe W. Influence of osteocalcin and collagen I on the mechanical and biological properties of Biocement D. Biomol Eng. 2002;19(2-6):227–31. doi: 10.1016/s1389-0344(02)00036-9. [DOI] [PubMed] [Google Scholar]
- 156.Fassbender WJ, Steinhauer B, Stracke H, Schumm-Draeger PM, Usadel KH. Validation of a new automated immunoassay for measurement of intact osteocalcin. Clin Lab. 2002;48(1-2):31–8. [PubMed] [Google Scholar]


