Abstract
Two cases of brown tumor of the humerus caused by ectopic parathyroid adenomas were presented, which to our knowledge has not been previously documented in the international literature. There are two highlights in these two cases. First, brown tumors of the long bones may commonly involve femur and tibia, rarely involve humerus in association with primary hyperparathyroidism. Second, ectopic parathyroid adenomas of our patient had an unusual location of this disorder. We explored the role of ultrasound, MIBI scintigraphy as well as FNAB (fine needle aspiration biopsy) in diagnosis of brown tumor especially simultaneously occurrence of ectopic parathyroid adenomas and the importance of a thorough diagnostic work-up. The contemporary diagnosis and treatment options will be emphasized.
Keywords: Brown tumor, ectopic parathyroid adenomas, hyperparathyroidism, humerus
Introduction
Primary hyperparathyroidism (Primary HPT) is defined as hypercalcemia resulting from the overproduction of parathyroid hormone (PTH) by one or more hyperfunctioning parathyroid glands, which may lead to abnormal bone metabolism and cause brown tumors [1,2]. Brown tum ors derive their name from their characteristic reddish brown color. They are essentially cellular reparative processes and are non-neoplastic [3,4]. The term “tumor” is an impropriety. It is most commonly found in the trabecular portion of the long bones, pelvis, ribs, clavicle and jaw [1-4]. Ectopic parathyroid adenoma especially inside the thyroid and mandible are quite exceptional and give rise to certain diagnostic difficulties. Pre-surgery localization of parathyroid adenomas in the context of primary HPT is significant. We report two cases of primary hyperparathyroidism, with the first presentation of brown tumor of the humerus, caused by ectopic parathyroid adenomas, and, subsequently, review the literature.
Case reports
Case 1
An 18-year-old male patient was transferred from another hospital with a six-month history of progressive pain in his right shoulder with limitation of motion obviously. Physical examination was unremarkable. Plain X-rays showed space-occupying lesions and the ultrasound showed a hypoechoic mass in the right upper humeral shaft with a pathological fracture (Figure 1A, 1B). Biopsy did not show any malignancy and further diagnostic work out revealed elevated PTH of 148 pg/ml (normal values between 15 and 65 pg/ml), elevated calcium level of 3.15 mmol/L (normal values between 2.15 and 2.55 mmol/L) and low phosphate level of 0.79 mmol/L (normal values between 0.8 and 1.45 mmol/L) in a blood sample. The diagnosis of hyperparathyroidism was definitive. In order to find out of the pathogeny, both CT and ultrasonography of neck were done (Figure 1C, 1D). We did not see the parathyroid gland in the normal place but a nodule intrathyroid was noticed, which guided the suspicion of ectopic parathyroid. Sestamibi scan of the parathyroid glands demonstrated the focal accumulation of radiotracer uptake in the left lower lobe thyroid (Figure 1E). In order to confirm the nodule inside the thyroid was the reliable ectopic parathyroid adenoma, we performed FNAB with 22G needle and the pathological result certified our diagnosis (Figure 1F). He was advised to receive the ectopic parathyroid adenoma resection and an intrathyroidal parathyroid adenoma was confirmed in the final histopathological examination (Figure 1G). A follow up at 8 months revealed satisfactory clinical recovery with normal calcium, phosphorus, alkaline phosphatase, and PTH levels.
Figure 1.
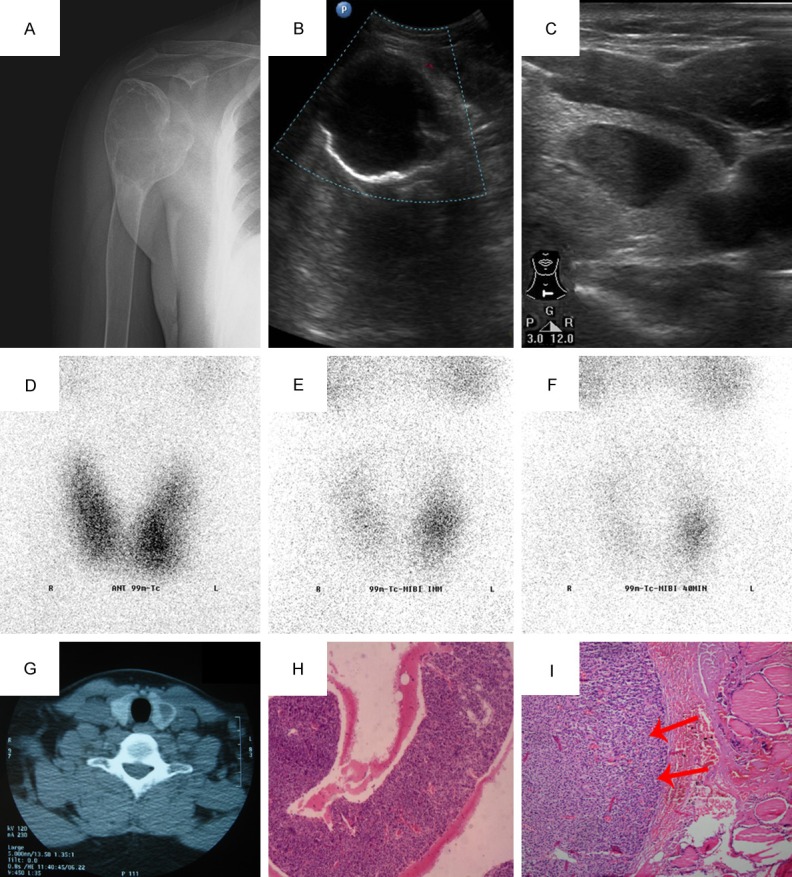
A. Round, radiolucent and osteolytic bone-expanding lesion was found in the right humeral head by X-ray; B. The ultrasound showed that there was a cystic mass in the right upper humeral shaft, which was irregular, well-demarcated and without any blood flow signals; C. Ultrasonography of neck showed there was a hypoechoic nodule (18 × 15 × 7 mm) inside the left lobe of his thyroid gland, which was of a standard shape, well-demarcated, homogeneous and a cystic area within; D. space-occupying effect can be seen in the thyroid static imaging; E&F. Dual-time point imaging showed the focal accumulation of radiotracer uptake in the left lower lobe thyroid; G. CT of the neck revealed a large low-density mass in the left lower lobe thyroid; H. Aspiration biopsy assumed that this intrathyroidal nodule was a ectopic parathyroid adenoma (HE, × 40); I. Ectopic parathyroid adenoma, chief cell type. The tumor cells had round or ovoid nuclei with densely stained chromatin. The tumor (left) was surrounded by a rim of normocellular thyroid gland (HE, × 100).
Case 2
A 26-year-old female patient was admitted to our hospital for the pain and swelling of the right upper limb for a period lasting 2 months without a history of trauma. Relevant examination from other hospitals revealed some lesion in both right upper humerus and left ribs with the formation of soft tissue mass, considered the possibility of tumors. The patient attended our clinic for further treatment. Physical examination showed a regional swelling without tenderness over the right upper limb. The diagnosis of primary HPT was confirmed when further diagnostic work out revealed elevated PTH of 263 pg/ml, elevated calcium level of 3.47 mmol/L and low phosphate level of 0.57 mmol/L in a blood sample. The assistant examination was summarized in Figure 2. Initially, we did not found the causation of the disease due to the non-existent of the normally located parathyroid adenomas. After image review we noticed the ectopic parathyroid adenomas inside the mandible in the 99mTc-Sestamibi Parathyroid Scan (Figure 2). The patient was referred elsewhere for parathyroidectomy. Further supersonic and radiological evaluation 3 years later, 30 months after parathyroidectomy, were showed in Figure 2. Brown tumors appeared spontaneous regression.
Figure 2.
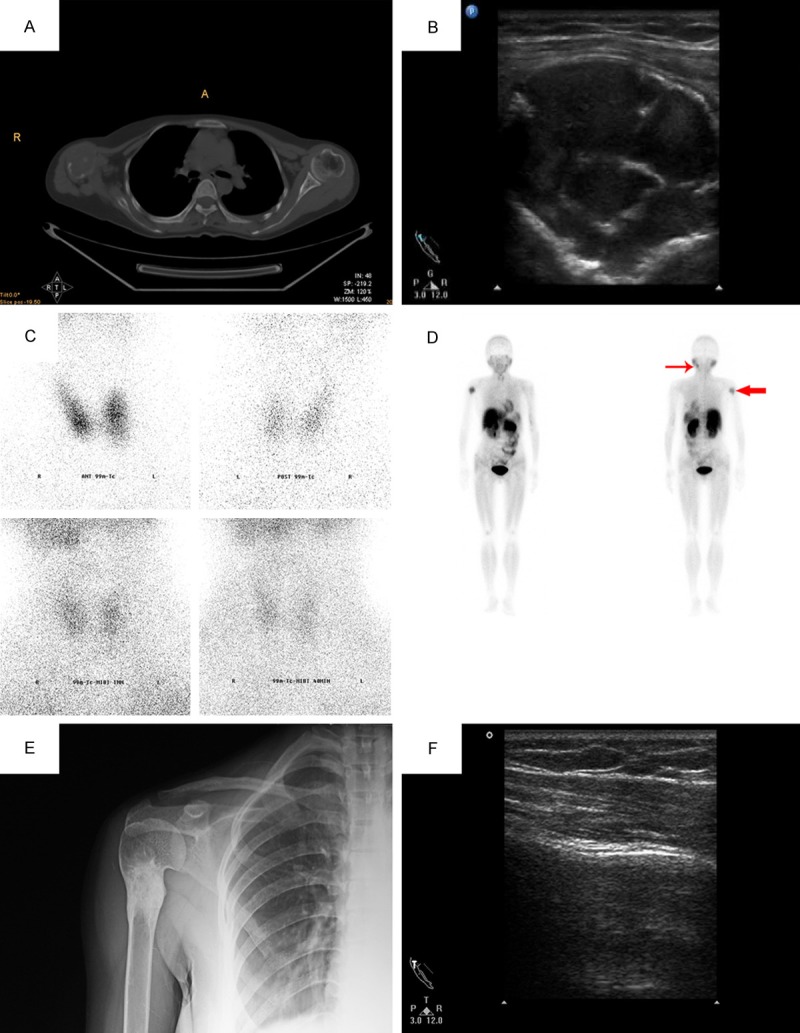
A. CT demonstrated a well-circumscribed large mass in the right humeral head, with bony expansion; B. The ultrasound showed that there was a cystic-solid mass in the right humerus. The tumor was of an irregular shape, with clear margins, and hyperechoic ribbons within; C. None focal accumulation of radiotracer uptaked in the normal position of parathyroid; D. focal accumulation of radiotracer uptaked in the right upper humeral shaft (brown tumor) and the left mandible (ectopic parathyroid adenomas); E. 30 months after parathyroidectomy, X-ray revealed reactive sclerosis on the original diseased region; F. The ultrasound showed well bony cortex and the mass on the original diseased region of the right humerus was disappeared.
Discussion
With the improvements in routine biochemical tests and radiological procedures, hyperparathyroidism is nowadays diagnosed much earlier and mainly in the asymptomatic stage [1]. Brown tumor, as one of the bony complications of HPT, is characterized by high osteoclastic activity and bone resorption [1]. In our two cases, the patients suffered from primary HPT, with the first symptom of brown tumor being in the humerus. Although the long bone is one of the common sites for the detection of brown tumors, rare cases of the involvement of the humerus were reported [5,6].
The most common cause of primary HPT is a solitary adenoma (90%), followed by hyperplasia (9%) and carcinoma (1%) [7]. Whether the normally located parathyroid adenomas or ectopic parathyroid adenomas may cause primary HPT and lead to similar radiologic and pathologic features in the bones. Ectopic parathyroid adenoma can be explained by abnormalities during embryonic migration of the parathyroid glands and it is extremely rare that the parathyroid adenoma is inside the thyroid or mandible. The incidence of intrathyroid parathyroid adenoma has been variously reported between 1.4% and 6% [8], while the mandible location is quite exceptional and has never been reported.
There is no standard guideline on those cases [9]. A variety of techniques, including ultrasonography, computed tomography, Technetium-99 (99mTc) and FNAB can be used in investigating the disease. We also summarized several critical clinical points that are easily missed and should be kept in mind.
The clinical symptoms of brown tumors depend on the size and site of the lesion and are nonspecific. In these two cases, both the ectopic parathyroid adenoma and humeral brown tumor are so unusual of primary HPT that may raise diagnostic difficulties and compound the misdiagnosis.
As usual, brown tumor tends to be misdiagnosed as malignancy and the differential diagnosis of brown tumor, giant cell tumor, non-ossifying fibroma, fibrous dysplasia, giant cell reparative granuloma, aneurysmal bone cyst and metastatic disease must be considered [3,10], whereas radiographic features do not help to distinguish between these diagnoses, delayed diagnosis of the underlying hyperparathyroidism is common. Raised serum calcium and PTH and a decrease in bone mineral density must cause suspicion for the probable brown tumor.
Sonography revealed the features of the brown tumor to be internally homogenous oval or round hypoechoic masses with clear smooth margins [10]. The solid part of the lesion shows the color Doppler signal, marked vascularity was thought to be the reason for that [5].Ultrasound can help to scan the parathyroid gland at the same time especially explore whether they are normal located. If not, it is also useful to find out the possibility of intrathyroid parathyroid adenoma when there is a well-circumscribed, round or oval hypoechoic nodule inside the thyroid. Furthermore, as a convenient and non-radiative examination, ultrasound may help evaluate and monitor the evolution of lesions after parathyroidectomy [10]. The ultrasound appearance of a brown tumor after parathyroidectomy varies with the pathological type of lesion. The cystic transformed brown tumors will not show ossification after parathyroidectomy, but the non-cystic transformed brown tumors will. The appearance of these healing and healed brown tumors can easily be misdiagnosed as fibrous dysplasia or even metastatic lesions [11].
Etiological assessment as well as pre-surgery localization of parathyroid adenomas in the context of primary HPT is important to limit the extent of the surgical dissection and avoid missing an ectopic adenoma or multiple adenomas, necessary for successful surgery [12,13]. Because of the small-size and position-changing of parathyroid, there are fade zones for ultrasound. Sestamibi scanning even dual-tracer (iodine-123 and 99mTc-MIBI) subtraction scintigraphy is the most common and high-efficiency way to localize diseased parathyroid glands prior to surgery especially in the case of an ectopic parathyroid [14]. As a mild and safe radioactive agent, 99mTc is absorbed by the hyperactive parathyroid gland and detected when scanning, which demonstrates a persistent focus of activity location in the parathyroid scintigraphy [14]. In case 2 we did not catch sight of the ectopic parathyroid adenoma at the first time, but after image review we noticed it inside the mandible. It is a salutary warning that meticulous could never be overemphasis in our clinical work.
Ultrasound-guided FNAB can be a very useful diagnostic method both to make an accurate preoperative diagnosis in the evaluation of brown tumor and to conform the exit of ectopic parathyroid adenoma. As in case 1, we cannot ensure the nodule intrathyroid was the ectopic parathyroid adenoma without FNAB and may cause needless operation. FNAB represents the timeliest and the least invasive method for making a definite diagnosis.
The importance of different radiological evaluation methods and the consultation between the surgeons, endocrinologists, and radiologists are emphasized. Further longitudinal studies are required to establish a more normative procedure in the diagnosis of brown tumor caused by ectopic parathyroid adenomas. Surgical resection of brown tumors is generally not recommended. Sometimes, when brown tumors are large, symptomatic, or have a risk of pathological fracture, surgical resection should be considered. Parathyroidectomy is a standard method of treatment for brown tumors. However, minorities of brown tumors fail to heal after parathyroidectomy, thus curettage and bone graft could be considered for persistent symptoms after parathyroidectomy [15].
Acknowledgements
This work was supported by Grants from the National Natural Science Foundation of China (No. 30973040) and the Technology Foundation of Tianjin Public Health Bureau of China (No. 2012KZ104).
Disclosure of conflict of interest
None.
References
- 1.Selvi F, Cakarer S, Tanakol R, Guler SD, Keskin C. Brown tumour of the maxilla and mandible: a rare complication of tertiary hyperparathyroidism. Dentomaxillofac Radiol. 2009;38:53–8. doi: 10.1259/dmfr/81694583. [DOI] [PubMed] [Google Scholar]
- 2.Sun C, Xu X, Wang X, Sheng W, Wen S, Han J. Thymic carcinoma with tumor thrombus protruding into the superior vena cava and the right atrium. Thoracic Cancer. 2013;4:333–334. doi: 10.1111/1759-7714.12012. [DOI] [PubMed] [Google Scholar]
- 3.Takeshita T, Takeshita K, Abe S, Takami H, Furui S. Brown tumor with fluid-fluid levels in a patient with primary hyperparathyroidism: radiological findings. Radiat Med. 2006;24:631–4. doi: 10.1007/s11604-006-0068-4. [DOI] [PubMed] [Google Scholar]
- 4.Jebasingh F, Jacob JJ, Shah A, Paul TV, Seshadri MS. Bilateral maxillary brown tumors as the first presentation of primary hyperparathyroidism. Oral Maxillofac Surg. 2008;12:97–100. doi: 10.1007/s10006-008-0105-9. [DOI] [PubMed] [Google Scholar]
- 5.Davies AM, Evans N, Mangham DC, Grimer RJ. MR imaging of brown tumour with fluid-fluid levels: a report of three cases. Eur Radiol. 2001;11:1445–9. doi: 10.1007/s003300100860. [DOI] [PubMed] [Google Scholar]
- 6.Hong WS, Sung MS, Chun KA, Kim JY, Park SW, Lee KH, Lim SY, Yoo WJ, Chung MH. Emphasis on the MR imaging findings of brown tumor: a report of five cases. Skeletal Radiol. 2011;40:205–13. doi: 10.1007/s00256-010-0979-0. [DOI] [PubMed] [Google Scholar]
- 7.Dimitri A, Kluyskens FF, Koenraad L, Verstraete Multiple healed brown tumors after resection of a parathyroid adenoma in primary hyperparathyroidism. Eur J Radiol. 2009 Extra. 03. [Google Scholar]
- 8.Bahar G, Feinmesser R, Joshua BZ, Shiptzer T, Morgenstein S, Popovtzer A, Shvero J. Hyperfunctioning intrathyroid parathyroid gland: a potential cause of failure in parathyroidectomy. Surgery. 2006;139:821–6. doi: 10.1016/j.surg.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 9.Cook MI, Qureshi YA, Todd CE, Cummins RS. An unusual ectopic location of a parathyroid carcinoma arising within the thyroid gland. J Clin Endocrinol Metab. 2012;97:1829–33. doi: 10.1210/jc.2011-3115. [DOI] [PubMed] [Google Scholar]
- 10.Jie Z, Hao W, Weijun T. Brown tumor of the rib as a first presentation of primary hyperparathyroidism: Report of three cases and literature review. Thoracic Cancer. 2013;4:474–478. doi: 10.1111/1759-7714.12045. [DOI] [PubMed] [Google Scholar]
- 11.Franco M, Bendini JC, Albano L, Barrilion D, Cassuto E, Bracco J. Radiographic follow-up of a phalangeal brown tumor. Joint Bone Spine. 2002;69:506–10. doi: 10.1016/s1297-319x(02)00439-6. [DOI] [PubMed] [Google Scholar]
- 12.Lumachi F, Zucchetta P, Varotto S, Polistina F, Favia G, D’Amico D. Noninvasive localization procedures in ectopic hyperfunctioning parathyroid tumors. Endocr Relat Cancer. 1999;6:123–5. doi: 10.1677/erc.0.0060123. [DOI] [PubMed] [Google Scholar]
- 13.Loevner LA. Imaging of the parathyroid glands. Semin Ultrasound CT MR. 1996;17:563–75. doi: 10.1016/s0887-2171(96)90004-9. [DOI] [PubMed] [Google Scholar]
- 14.Yan ST, Tian H. Senile parathyroid dysfunction: Characteristics of its diagnosis and treatment. J Transl Int Med. 2013;1:32–35. [Google Scholar]
- 15.Iwasaki N, Minami A. Brown tumour of the wrist with primary hyperparathyroidism. J Hand Surg Eur Vol. 2010;35:71–2. doi: 10.1177/1753193409344530. [DOI] [PubMed] [Google Scholar]


