Abstract
The gastrointestinal tract is the most common site for extranodal involvement by non-Hodgkin’s lymphoma. However, primary appendiceal lymphomas presenting as perforated acute appendicitis are very rare: they occur in only 0.015% of all gastrointestinal lymphoma cases. The management of this condition is still controversial, and a multimodality approach (e.g., surgery, radiation therapy, and chemotherapy) is the optimal treatment. In these cases, appendiceal non-Hodgkin’s lymphomas typically manifest with acute symptoms in patients with no prior lymphoma history. Additionally, we treated our patient with a right hemicolectomy and postoperative multiagent chemotherapy.
Keywords: Appendix, non-Hodgkin, lymphoma
Introduction
The “2008 WHO Classification” specification of non-Hodgkin lymphoma (NHL) is based on recent progress in immunohistochemical and genetic analyses and clinical findings, including prognostic data [1]. Among extranodal NHLs, the alimentary tract is the most frequently affected site [2,3]. However, appendiceal lymphomas are exceedingly rare and often diagnosed postoperatively. Moreover, the clinical findings are nonspecific. Lymphomatous infiltration of the appendix is also rare, and it is even rarer when acute appendicitis is the initial manifestation. To the best of our knowledge, computed tomography (CT) scans play a very important role in appendiceal neoplasm evaluations and appear to be the modality of choice whenever an appendiceal mass is suspected.
Case report
A 43-year-old female was referred to our hospital complaining of severe, dull lower abdominal pain for 20 hours. One week before the referral, the patient initially complained of epigastric distress, nausea and vomiting, and during the following days, the pain increased. The pain was not radiating, related to meals or urination and was not associated with fever, weight loss or bowel habit changes. Additionally, it was occasionally associated with nausea and vomiting. Moreover, there was no history of renal diseases or stones.
A physical examination helped determine that there was significant lower abdominal tenderness, with more tenderness occurring in the right quadrant. Rebounding pain was also noted.
Following a lab examination, blood tests revealed an elevated white cell count of 14.3×109/L (range 3.5-10×109/L), with an associated N% of 80.5% (range 50%-70%). A gynecologic examination was negative; however, an abdominal ultrasonography revealed a mixed mass in the right lower abdomen (Figure 1). An abdominal CT scan showed a low-density mass in the cecum, which was distended to 3 cm in diameter, with the lumen measuring approximately 50 H in density. No other masses or enlarged lymph nodes were present in the abdomen or pelvis (Figure 2).
Figure 1.

Abdominal ultrasonography shows a mixed mass in the right pelvis, which measured 72×66 cm2. The mass shape was irregular, and the borders were not normal. Additionally, no obvious blood flow was observed within the display.
Figure 2.

Axial images from an unenhanced CT scan showed a large tubular structure extending posteriorly into pelvis from the cecal region. The appendix measured 3 cm in diameter and coiled in and out of transverse axial plane. The appendiceal density was approximately 50 H.
The patient was prepared for and consented to a laparoscopic exploration, which revealed a large appendicular mass that was approximately 7×6 cm and had invaded into the cecum. Because of extensive adhesions in the right iliac fossa, the procedure was converted into a laparotomy through a paramidline incision. The appendicular mass was hard in consistency and had invaded into the cecum. The appendix was 10×3 cm in size and was gangrenous and perforated. The appendiceal wall, which measured more than 1 cm in length, was distinguishable from the lumen. Additionally, the appendiceal base protruded slightly into the cecal lumen. No additional masses or enlarged lymph nodes were discovered in the abdomen or pelvis. Moreover, there was no evidence of tumors. Thus, we proceeded with an appendicectomy. After one week, the final histologic examination revealed a large and diffuse appendiceal B-cell NHL (DLBCL), and the tumor had infiltrated through the muscularis propria into the subserosa (Figure 3). Ten days later, the patient underwent a right hemicolectomy and an ilieotransverse anastomosis. The mesenteric lymph nodes along the right colic artery were excised, and a pathological examination showed that the proximal and distal resection margins were malignancy free. Additionally, all 18 examined lymph nodes were malignancy free. An immunohistochemical analysis revealed that the typical tumor cells were CD20, CD10, and Bcl-6 positive and were CD3, CD4, and Bcl-2 negative.
Figure 3.
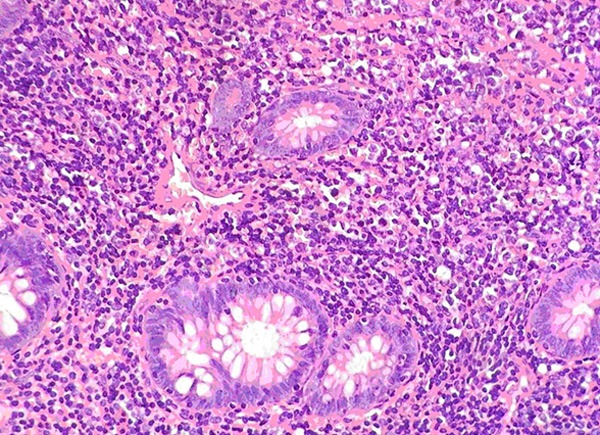
Intraepithelial lymphocytes were not increased, and abnormal tumor cell invasion was not prominent in the mucosal layer. Large atypical lymphocytes with small distinct nuclei diffusely infiltrated the area, and some reactive histiocytes were observed (H&E stain, ×100).
The patient was discharged after 40 days with an oncological referral. Postoperative treatment with chemotherapy was carried out. Two months later, a follow-up CT of the abdomen and pelvis revealed no evidence of any tumor remnants.
Discussion
Primary appendiceal lymphomas are rarely limited. As far as we know, only approximately 50 appendiceal NHL cases have been previously reported, with few of these case reports occurring in Asia. In the previous cases, the median age at diagnosis for gastrointestinal tract NHLs was 55 years, and the disease was more common in men [4]. Appendix NHLs typically manifested with acute symptoms in patients who had no prior lymphoma history. Further, most of these patients had no relevant medical history and were believed to be immunocompetent. Patients with this disease always present clinically with signs and symptoms that are suggestive of acute appendicitis. Acute appendicitis from a luminal obstruction is the most common manifestation of many appendicular tumors [5]. Other clinical manifestations include asymptomatic palpable masses, incidental imaging findings, intussusception, gastrointestinal bleeding, ureteral obstructions or hematuria, and increasing abdominal girth from a malignant mucocele rupture, which results in pseudomyxoma peritonei.
Detection of these neoplasms with preoperative imaging is important because it may change the surgical approach and obviate additional surgeries [5]. The ultrasonography showed a mixed mass in the right pelvis. Following a CT scan, a lymphomatous infiltration of the appendix that had produced a markedly diffuse mural soft-tissue thickening was observed (range of diameters, 2.5-4.0 cm; mean diameter, 3.2 cm). A vermiform morphology is usually maintained in the appendix, and aneurysmal dilatation of the lumen is occasionally observed. No evidence of mural thickening or intraluminal masses suggested the involvement of other gastrointestinal sites, such as the stomach, small bowel, or colon; however, the solid abdominal organs were normal. Although the CT scan image appearance was not pathognomonic, as can occasionally be observed with other primary appendiceal neoplasms, NHL was the lead differential diagnosis. The specificity for lymphoma is increased in the settings of abdominal lymphadenopathy or aneurysmal dilatation of the appendiceal lumen [4]. What was lacking, however, were sufficient data regarding the upper diameter limit, above which one should consider infiltrative neoplasms in addition to standard, non-tumoral appendicitis. Because an inflamed appendix without a neoplasm will usually not exceed 15 mm in diameter on a CT scan [6], an enlargement beyond this size should be viewed with suspicion. Although it is quite uncommon, appendix mucoceles are less rare than appendiceal lymphomas and should be considered in the differential diagnoses of appendiceal masses.
It is difficult to establish guidelines for appendiceal lymphoma therapies because of its rarity. A primary surgical resection followed by postoperative CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone) chemotherapy showed a high efficacy in intestinal diffuse large B cell lymphoma (DLBL) patients [7]. The efficacy of a surgery/chemotherapy combination in obtaining a good remission rate for localized early primary intestinal lymphomas indicates that this combination represents the only means for managing these complications [8]. Additionally, close follow-up examinations are certainly recommended.
Conclusion
We present a rare case of a large, B-cell type lymphoma of the appendix. Although appendiceal lymphomas are rare, a characteristic CT scan appearance may lead to preoperative diagnoses. Additionally, our case illustrates that this cancer type must be included in differential acute appendicitis diagnoses and that physicians and surgeons have to be aware of these conditions.
Disclosure of conflict of interest
None.
References
- 1.Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: International Agency for Research on Cancer; 2008. [Google Scholar]
- 2.Gustafsson BI, Siddique L, Chan A, Dong M, Dorozdov I, Kidd M, Modlin IM. Uncommon cancers of the small intestine, appendix and colon. An analysis of SEER 1973-2004, and current diagnosis and therapy. Int J Oncol. 2008;33:1121–1131. [PubMed] [Google Scholar]
- 3.O’Donnell ME, Badger SA, Beattie GC, Carson J, Garstin WIH. Malignant neoplasms of the appendix. Int J Colorectal Dis. 2007;22:1239–1248. doi: 10.1007/s00384-007-0304-0. [DOI] [PubMed] [Google Scholar]
- 4.Pickhardt PJ, Levy AD, Rohrmann CA, Abbondanzo SL, Kende AI. Non-Hodgkin lymphoma of the appendix: Clinical and CT findings with pathologic correlation. AJR Am J Roentgenol. 2002;187:1123–1127. doi: 10.2214/ajr.178.5.1781123. [DOI] [PubMed] [Google Scholar]
- 5.Pickhardt PJ. Primary Neoplasms of the Appendix: Radiologic Spectrum of Disease with Pathologic Correlation. Radiographics. 2003;23:645–662. doi: 10.1148/rg.233025134. [DOI] [PubMed] [Google Scholar]
- 6.Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology. 2000;215:337–348. doi: 10.1148/radiology.215.2.r00ma24337. [DOI] [PubMed] [Google Scholar]
- 7.Lee J, Kim WS, Kim K, Ahn JS, Jung CW, Lim HY, Kang WK, Park K, Ko YH, Kim YH, Park C, Yoon SH, Lee WY, Chun HK. Prospective clinical study of surgical resection followed by CHOP in localized intestinal diffuse large B cell lymphoma. Leuk Res. 2007;31:359–64. doi: 10.1016/j.leukres.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 8.Zinzani PL. Primary intestinal lymphoma: clinical and therapeutic features of 32 patients. Haematologica. 1997;82:305–308. [PubMed] [Google Scholar]


