Abstract
This study is aimed to investigate the pattern of CEBPA mutations and its clinical significance in Chinese non-M3 acute myeloid leukemia (AML) patients. The entire coding region of CEBPA gene was amplified by PCR and then sequenced in samples from 233 non-M3 AML patients. Fifty mutations were identified in 37 (15.8%) patients with eleven (4.7%) double mutated CEBPA (dmCEBPA) and twenty-six (11.1%) single mutated CEBPA (smCEBPA). dmCEBPA was exclusively observed in M1 and M2 subtypes of FAB classification (P = 0.008), whereas smCEBPA occurred in almost all subtypes (P = 0.401). Patients with dmCEBPA had significantly younger age and higher WBC counts than those with wtCEBPA (P = 0.016 and 0.043, respectively). Both dmCEBPA and smCEBPA were mainly present in cytogenetically normal patients. Patients with dmCEBPA achieved higher rate of complete (CR) than wtCEBPA patients (88% vs. 51%, P = 0.037), whereas smCEBPA and wtCEBPA groups are similar (47% vs. 51%, P = 0.810). Patients with dmCEBPA had a superior overall survival (OS) compared with patients with wtCEBPA (P = 0.033), whereas patients with smCEBPA had a similar OS as patients with wtCEBPA (P = 0.976). dmCEBPA but not smCEBPA was also associated with favorable outcome in patients with wild-type NPM1 and FLT3-ITD (NPM1wtFLT3-ITDwt). Our data confirm that dmCEBPA but not smCEBPA is prognostically favorable in NPM1wtFLT3-ITDwt AML, and suggest that the entity AML with mutated CEBPA should be definitely designated as AML with dmCEBPA in WHO classification and smCEBPA should be excluded from the favorable risk of molecular abnormalities.
Keywords: CEBPA, mutation, prognosis, acute myeloid leukemia
Introduction
The hallmark of acute myeloid leukemia (AML) is the differentiation arrest and neoplastic accumulation of myeloid precursor cells in the bone marrow. Researches on the pathogenesis of AML have identified the molecular changes caused by acquired cytogenetic abnormalities in leukemic patients [1,2]. Inappropriately activated transcription factors involved in these structural rearrangements disturb normal programs of myeloid cell proliferation, differentiation, and survival [1-3]. Other genetic and epigenetic lesions accumulate and act in concert with aberrant transcription factors in multiple pathways of leukemogenesis [4-6]. Recurrent cytogenetic abnormalities have been demonstrated as powerful predictors of the outcome in AML patients [7-9]. Aberrant molecular events have further refined the prognosis in AML [10].
CCAAT/enhancer binding protein alpha (CEBPA) gene, located on chromosome 19q13.1, encodes a protein of 358 amino acids which consists of a N-terminal transcriptional activation domain (TAD) and a C-terminal basic leucine zipper (bZIP) domain. The CEBPA transcription factor is widely expressed during the differentiation of myelopoiesis and is involved in cell cycle block, proliferation inhibition, and repression of self-renewal [11-13]. CEBPA mutations have been reported in approximately 5~14% of all AML patients among which the majority are cytogenetically normal (CN) [14-17]. Although CEBPA mutations can occur across the whole coding region, two types of mutations are predominant: (1) N-terminal frame-shift mutations that lead to loss of translation of the full-length 42-kDa CEBPA protein (p42 CEBPA) and to the overexpression of a truncated, dominant negative 30-kDa CEBPA isoform (p30 CEBPA); (2) C-terminal in-frame insertions/deletions that prevent homodimerization or hetero-dimerization of CEBPA [15-18]. These CEBPA mutation types can occur as mono- or bi-allelic mutations. More than half of CEBPA-mutated patients harbor bi-allelic mutations with a N-terminal frame-shift mutation on one allele and a C-terminal in-frame mutation on the other allele [19]. The clinical significance of CEBPA mutations has been extensively explored. AML with mutated CEBPA has recently been included in the current WHO classification as a provisional entity due to its prognostically favorable influence in normal karyotype [20]. However, more recent studies have identified that the favorable impact on AML outcome is predicted by double mutated CEBPA (dmCEBPA) rather than single mutated CEBPA (smCEBPA) [21-24]. In the present study, we evaluated the frequency, the main associated features, and the prognostic significance of CEBPA mutations in a cohort of Chinese de novo non-M3 AML patients.
Materials and methods
Patients and samples
This study was approved by the Ethics Committee Board of the Affiliated People’s Hospital of Jiangsu University. Bone marrow aspirates of 233 non-M3 AML patients were collected after informed consent written by patients or their guardians. The diagnosis and classification were conducted according to the French-American-British Cooperative Group Criteria and the 2008 World Health Organization (WHO) proposal [20,25]. Treatment protocol was described as reported previously [26]. The main clinical and laboratory features of the patient cohort were summarized in Table 1.
Table 1.
Patient characteristics according to CEBPA mutation status in non-M3 AML
| Variables | Total (n = 233) | wtCEBPA (n = 196) | smCEBPA (n = 26) | P | dmCEBPA (n = 11) | P |
|---|---|---|---|---|---|---|
| Sex, male/female | 135/98 | 114/82 | 16/10 | 0.834 | 5/6 | 0.534 |
| Median age, years (range) | 53 (15-93) | 54 (15-93) | 52 (17-85) | 0.489 | 35 (15-61) | 0.016 |
| Median WBC, × 109/L (range) | 16.1 (0.6-528.0) | 14.5 (0.8-528.0) | 35.5 (1.3-528.0) | 0.072 | 44.7 (2.4-507.0) | 0.043 |
| Median hemoglobin, g/L (range) | 73 (32-147) | 72 (32-142) | 74 (45-147) | 0.220 | 85 (56-108) | 0.168 |
| Median platelets, × 109/L (range) | 40 (3-447) | 37 (3-447) | 53 (4-203) | 0.137 | 21 (3-76) | 0.084 |
| FAB | 0.158 | 0.022 | ||||
| M0 | 1 | 1 | 0 | 0 | ||
| M1 | 27 | 18 | 6 | 3 | ||
| M2 | 115 | 95 | 12 | 8 | ||
| M4 | 51 | 49 | 2 | 0 | ||
| M5 | 28 | 24 | 4 | 0 | ||
| M6 | 11 | 9 | 2 | 0 | ||
| WHO | 0.005 | 0.007 | ||||
| AML with t (8; 21) | 37 | 37 | 0 | 0 | ||
| AML with inv (16) | 1 | 1 | 0 | 0 | ||
| AML with 11q23 | 4 | 3 | 0 | 1 | ||
| AML without maturation | 23 | 15 | 6 | 2 | ||
| AML with maturation | 82 | 62 | 12 | 8 | ||
| Acute myelomonocytic leukemia | 50 | 48 | 2 | 0 | ||
| Acute monoblastic and monocytic leukemia | 25 | 21 | 4 | 0 | ||
| Acute erythroid leukemia | 11 | 9 | 2 | 0 | ||
| Karyotype classification | 0.005 | 0.099 | ||||
| Favorable | 39 | 39 | 0 | 0 | ||
| Intermediate | 153 | 121 | 23 | 9 | ||
| Poor | 29 | 25 | 2 | 2 | ||
| No data | 12 | 11 | 1 | 0 | ||
| Karyotype | 0.021 | 0.180 | ||||
| normal | 119 | 91 | 20 | 8 | ||
| t (8;21) | 38 | 38 | 0 | 0 | ||
| inv (16) | 1 | 1 | 0 | 0 | ||
| 11q23 | 4 | 3 | 0 | 1 | ||
| complex | 23 | 20 | 2 | 1 | ||
| others | 36 | 32 | 3 | 1 | ||
| No data | 12 | 11 | 1 | 0 | ||
| Gene Mutation | ||||||
| NPM1 (+/-) | 26/203 | 23/169 | 3/23 | 1.000 | 0/11 | 0.618 |
| FLT3 ITD (+/-) | 22/207 | 19/173 | 2/24 | 1.000 | 1/10 | 1.000 |
| C-KIT (+/-) | 15/214 | 15/177 | 0/26 | 0.226 | 0/11 | 1.000 |
| IDH1/2 | 14/207 | 13/171 | 1/25 | 1.000 | 0/11 | 1.000 |
| DNMT3A | 17/204 | 14/170 | 2/24 | 1.000 | 1/10 | 0.595 |
| N/K-RAS | 20/201 | 15/169 | 4/22 | 0.266 | 1/10 | 1.000 |
| CR (+/-) | 83/74 | 66/63 | 9/10 | 0.810 | 8/1 | 0.037 |
Cytogenetic analysis
Conventional cytogenetic analysis was performed in the cytogenetics laboratory of our hospital. Chromosomes were prepared routinely by the direct method or 24h short-term culture of bone marrow cells. Karyotypes were analyzed on R-banded metaphases. The definition of a cytogenetic clone and descriptions of karyotypes followed the International System for Human Cytogenetic Nomenclature [27]. Karyotypes were classified according to the revised MRC prognostic classification [9].
Cell separation and DNA isolation
The mononuclear cells were separated by density-gradient centrifugation using Ficoll. Subseq-uently, genomic DNA was extracted using the Genomic DNA Purification Kit (Gentra, Minneapolis, MN, USA) according to the manufacturer’s instructions.
Gene mutation detection
Mutation of the CEBPA gene was detected in genomic DNA by PCR and direct sequencing. Two overlapping primer pairs were used to amplify the entire coding region of CEBPA (NM_004364.3): P1 (477 bp) 5’-TGCCGGGAGAACTCTAACT-3’ (sense) and 5’-CCCGACGCGCTCGTACA-3’ (antisense), P2 (688 bp) 5’-CTGGACGGCAGGC TGGA-3’ (sense) and 5’-CAGGGCGGTCCCACAGC-3’ (antisense). The total PCR reaction volume of 25 μL contained 1× PCR buffer for KOD FX, 0.4 μM of primer set 1 or 0.2 μM of primer set 2, 0.4 μM of each dNTP, and 0.5U KOD FX polymerase (Toyobo, Osaka, Japan). The following conditions were performed: 98°C for 2 minutes; 35 cycles of 98°C for 10 seconds, 60°C (P1) or 68°C (P2) for 30 seconds, and 68°C for 3 minutes; then 72°C for 7 minutes. PCR products were electrophoresed on 2% agarose gels, purified using Axygen AP-GS500 kit (Axygen, CA, USA) and then sequenced in both directions with PCR primers on an ABI 3730 Prism Sequencer (Applied Biosystems, CA, USA). In samples with a CEBPA sequence variation, the entire coding region was amplified with primers P1F and P2R under the previously described PCR conditions except for annealing at 65°C and was cloned into the pMD19-T vector (TaKaRa, Japan). 5 to 10 clones were sequenced in each patient with the primers used to amplify the entire coding region of CEBPA.
NPM1, FLT3 internal tandem duplication (ITD), C-KIT, DNMT3A, IDH1/IDH2, and N/K-RAS mutations were detected as described previously [28-30]. Briefly, genomic DNA was amplified using gene-specific primers. Mutation scanning was performed for PCR products of all genes except for FLT3-ITD using HRMA with the LightScannerTM platform (Idaho, Utah, USA). All positive samples were directly DNA sequenced to confirm the results of HRMA. FLT3 internal tandem duplication (ITD) was detected using direct DNA sequencing.
Statistical analysis
All statistical analyses were performed using the SPSS 17.0 software package (SPSS, Chicago, IL). Statistical significance of the difference between groups for continuous variables was determined by the Mann-Whitney test. Statistical significance of the difference between groups for categoric variables was determined by Fisher exact test or Chi-square analysis. Overall survival (OS) was estimated using the Kaplan-Meier method and were compared using the log-rank test. Multivariate analyses were performed using Cox proportional hazards regression. The significance of results was defined as a level of P<0.05 at both tails.
Results
Frequency and types of CEBPA mutations in Chinese AML patients
Fifty mutations were identified in 37 (15.8%) patient samples (Figure 1; Table S1). Eleven patients (4.7%) had dmCEBPA, whereas twenty-six (11.1%) had smCEBPA. We observed four CEBPA mutations in one patient. In all 11 patients with two CEBPA mutations, we identified one patient with two CEBPA mutations in one allele, while the distribution of the mutations was biallelic in other patients as determined by cloning analysis. 10 patients with double mutations had both a N-terminal frame-shift mutation resulting in premature truncation and a C-terminal mutation resulting in in-frame insertion/duplication/substitution/deletion or out-of-frame duplication/deletion. Among patients with a single CEBPA mutation, eight mutations were located in the N-terminal leading to premature truncation, the majority of mutations (15/26, 58%) were located in the C-terminal resulting in in-frame duplication/insertion/substitution, while three mutations were located in between TAD2 and DNA binding domain (DBD) regions resulting in frame-shift premature truncation.
Figure 1.
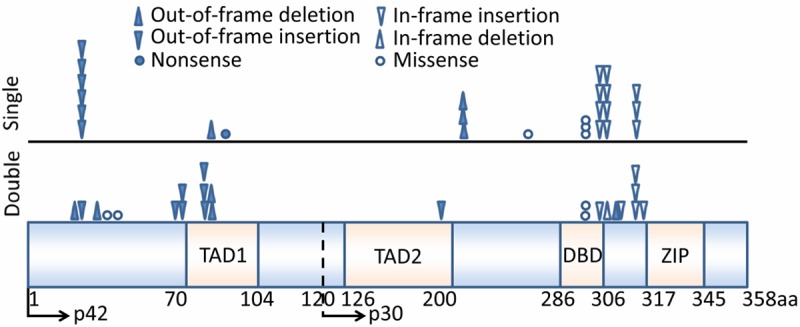
Schematic representation and location of the 50 CEBPA mutations. Functional regions of two transactivation domains (TAD1 and TAD2), DNA-binding domain (DBD), and the bZIP region are depicted. Amino acid (aa) numbering and the alternative translation start site at position 120aa are also depicted.
Patient characteristics related to CEBPA mutation status
Because double CEBAP mutations were considered as a prognostic factor according to previous studies, we divided our patient cohort into the following three groups: patients with dmCEBPA (n = 11), patients with smCEBPA (n = 26), and patients with wild-type CEBPA (wtCEBPA, n = 196). The comparison of the clinical and laboratory features between three groups is summarized in Table 1.
smCEBPA was distributed in almost all subtypes of FAB classification (Table 1). Although the majority of patients with smCEBPA had M1 or M2 subtypes (18/26, 69%), there was no difference in the distribution of smCEBPA in the whole cohort [18/142 (13%) patients with M1 or M2 versus 8/91 (9%) patients with other subtypes, P = 0.401]. There was a trend that the patients with smCEBPA had higher WBCs than those with wtCEBPA (P = 0.072). smCEBPA was predominantly present in cytogenetically normal patients (P = 0.005). Concurrent other molecular mutations including NPM1, FLT3, IDH1, N/K-RAS, and DNMT3A occurred in patients with wtCEBPA, but no correlation was observed (P > 0.05).
dmCEBPA was exclusively observed in M1 and M2 subtypes (Table 1). Overall, 11 (8%) out of 142 patients with M1 or M2 subtypes harbored dmCEBPA, while none of 91 patients with other subtypes who did so (P = 0.008). Patients with dmCEBPA had significantly younger age and higher WBC counts at diagnosis than those with wtCEBPA (P = 0.016 and 0.043, respectively). There was a trend that dmCEBPA group had lower platelet counts than wtCEBPA group (P = 0.084). dmCEBPA was mainly present in cytogenetically normal patients except for two patients harboring poor-risk karyotypes. Concurrent FLT3-ITD, N-RAS, and DNMT3A mutations occurred in two patients with dmCEBPA.
Prognostic impact of CEBPA mutation status
Survival data were obtained for 157 AML patients with mean follow-up time of 14 months (range, 1-84 months). There was no significant difference in the rate of complete remission (CR) after induction chemotherapy between smCEBPA and wtCEBPA groups (47% vs 51%, P = 0.810), however, more patients with dmCEBPA achieved CR than wtCEBPA patients (88% vs 51%, P = 0.037, Table 1). Patients with dmCEBPA had a superior overall survival (OS) compared with patients with wtCEBPA (estimated median 25 vs 8 months, respectively, P = 0.033; Figure 2A), whereas smCEBPA patients had a similar OS as wtCEBPA patients (estimated median 8 vs 8 months, respectively, P = 0.976; Figure 2A). Furthermore, in multivariate analysis that included sex, age (≤60 yrs vs >60 yrs), WBC count (≤30 vs >30 × 109/L), karyotype risk group, and mutational status of seven genes as covariates, the presence of a dmCEBPA mutation remained an independent favorable prognostic factor for OS (Table 2). Because of the small size of CEBPA mutations, patients with dmCEBPA, compared with patients with smCEBPA, showed the trend towards longer OS (P = 0.115, Figure 2A).
Figure 2.
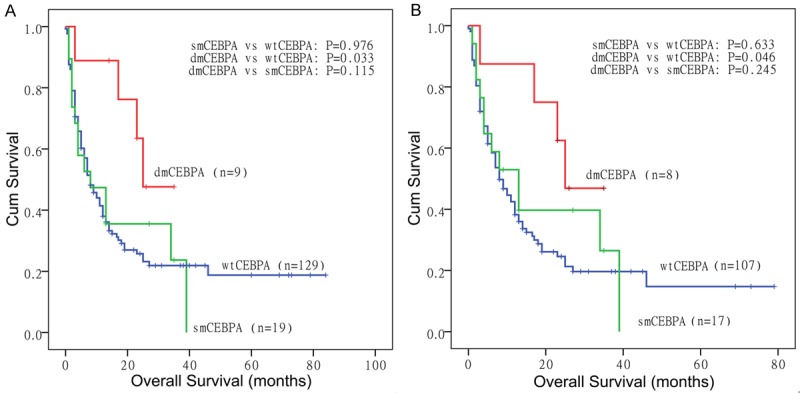
Kaplan-Meier survival curves for OS in non-M3 AML patients. A: All patients; B: NPM1wtFLT3-ITDwt patients.
Table 2.
Multivariate analyses of prognostic factors for OS in non-M3 AML
| All patients | NPM1wtFLT3-ITDwtpatients | |||
|---|---|---|---|---|
|
| ||||
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Sex | 0.922 (0.56-1.497) | 0.743 | 0.891 (0.560-1.418) | 0.628 |
| Age | 1.938 (1.270-2.958) | 0.002 | 2.073 (1.326-3.242) | 0.001 |
| WBC | 1.555 (1.026-2.354) | 0.037 | 1.140 (0.723-1.797) | 0.573 |
| Karyotype risk | 1.979 (1.467-2.669) | < 0.001 | 1.953 (1.422-2.682) | <0.001 |
| dmCEBPA vs wtCEBPA | 0.596 (0.358-0.992) | 0.047 | 0.650 (0.431-0.980) | 0.040 |
| smCEBPA vs wtCEBPA | 0.869 (0.458-1.650) | 0.669 | 0.763 (0.387-1.503) | 0.434 |
| FLT3 | 0.606 (0.304-1.208) | 0.155 | - | - |
| NPM1 | 0.852 (0.338-2.145) | 0.734 | - | - |
| C-KIT | 0.906 (0.319-2.576) | 0.853 | 0.842 (0.296-2.398) | 0.748 |
| N/K-RAS | 1.695 (0.825-3.483) | 0.151 | 1.576 (0.797-3.116) | 0.191 |
| IDH1/2 | 1.354 (0.643-2.850) | 0.425 | 2.321 (1.037-5.197) | 0.041 |
| DNMT3A | 1.061 (0.417-2.698) | 0.901 | 1.848 (0.443-7.703) | 0.399 |
HR: hazard ratio; CI: confidence interval; -: not included.
The impact of CEBPA mutations was also evaluated in patients with wild-type NPM1 and FLT3-ITD (NPM1wtFLT3-ITDwt), dmCEBPA but not smCEBPA was associated with favorable outcome (Figure 2B). Estimated median OS in dmCEBPA, smCEBPA, and wtCEBPA groups was 25, 13 and 8 months, respectively. Multivariate analysis also confirmed dmCEBPA only as an independent favorable factor in NPM1wtFLT3-ITDwt patients (Table 2).
Discussion
A total of 37 (15.8%) out of 233 Chinese non-3 AML patients were identified to carry 50 CEBPA mutations after excluding all known CEBPA polymorphisms (data not shown). The frequency of CEBPA mutations detected in our study is in good accordance with previous studies [24,31]. Three mutational hot spots were identified, one 5’ of the TAD1 region, the other in bZIP and the third in the DBD of the CEBPA gene, which was comparable with previous studies [22-24,32]. The proportion of smCEBPA and dmCEBPA was different from previous studies in which the percentage of dmCEBPA was more than that of smCEBPA [22-24]. However, a recent large-scale study has identified dmCEBPA in 104 (42.6%) out 2296 AML patient [33].
The observations are highly consistent across all studies: double CEBPA mutations occur mainly in M1/M2 subtypes and are highly associated with normal karyotypes. However, there is a discrepancy about clinical characteristics of AML with CEBPA mutations. Although the majority of studies did not find the correlation of CEBPA mutations with peripheral leukocytes in AML [22,23,32], two groups observed that CEBPA mutated patients had higher peripheral leukocytes than wild-type patients [34,35], which was consistent with our results. Moreover, similar to two previous reports [24,36], the present study found the association of double CEBPA mutation with younger age, whereas other studies did no find this correlation. However, a recent study on CEBPA mutations, the largest size of AML patients (a total of 2296 cases) till now, confirmed the association of dmCEBPA with younger age [33].
The impact of CEBPA mutations on outcome has been extensively evaluated. Earlier studies have led to the introduction of ‘AML with mutated CEBPA’, which includes both smCEBPA and smCEBPA, into the current WHO classification as a provisional entity among ‘AML with recurrent genetic abnormalities’ [20]. However, later studies have shown only dmCEBPA but not smCEBPA is a favorable prognostic factor. A recent study has confirmed that survival of AML with dmCEBPA is similar with those with PML-RARA [37]. Although in the present study patients with dmCEPA harbored higher peripheral leukocytes which also affected patients’ outcome, multivariate COX analysis verified dmCEBPA as an independent favorable predictor after adjusting for other covariates including peripheral leukocytes. Because of limited case numbers the difference in outcome was not significant between dmCEBPA and smCEBPA groups in this study. Initial study revealed that the presence of additional FLT3-ITD significantly worsen overall survival in the CEBPA-mutated group [38]. However, a subsequent study did not find the influence of FLT3-ITD on survival in the CEBPA-mutated group [34]. The aforementioned studies did not differentiate dmCEBPA from smCEBPA. Concurrent FLT3-ITD or NPM1 mutations are significantly less frequent in patients with dmCEBPA compared with those with smCEBPA, therefore, the impact of FLT3-ITD in AML with dmCEBP still needs to be determined. Further endeavor has been made to investigate the clinically relevant aspect of whether the favorable prognosis of dmCEBPA is influenced by other additional molecular markers. Concurrent TET2 mutations were adversely prognostic for OS [33,39], whereas GATA-2 mutations improved OS [39,40].
Although it has been shown that AML patients carrying single CEBPA mutation have similar outcome as those with wild-type CEBPA, further risk stratification has been tried in AML with single CEBPA mutation. Two studies revealed that FLT3-ITD significantly impaired the survival of AML patients with smCEBPA [24,33]. Furthermore, Fasan et al revealed that smCEBPA further decreased survival compared with wtCEBPA in patients with FLT3-ITD [33]. Moreover, two groups also observed that NPM1mt/CEBPAsm genotype showed a trend toward favorable outcome compared with NPM1wt/CEBPAsm [24,33]. Although smCEBPA was considered beneficial for outcome of AML with NPM1 mutation by Dufour et al [41], the later results from the same group did not confirm this observation [33]. As for the role of smCEBPA in NPM1wtFLT-ITDwt AML, it is also controversial. Park et al found smCEBPA subgroup had longer survival than wtCEBPA subgroup in NPM1wtFLT-ITDwt AML [42], however, similar with the results of the large-scale study of Fasan et al [33], we did not identify the difference.
In conclusion, the results of our present study confirm that AML with dmCEBPA but not smCEBPA is associated with a favorable outcome in NPM1wtFLT3-ITDwt non-M3 AML. Our data suggest that the entity AML with mutated CEBPA should be definitely designated as AML with dmCEBPA in WHO classification and smCEBPA should be excluded from the favorable risk of molecular abnormalities [10].
Acknowledgements
This study was supported by National Natural Science foundation of China (81270630, 81172592), Science and Technology Special Project in Clinical Medicine of Jiangsu Province (BL2012056), 333 Project of Jiangsu Province (BRA2011085, BRA2013136), Science and Technology Infrastructure Program of Zhenjiang (SS2012003), Social Development Foundation of Zhenjiang (SH2013042, SH2013082, SH2014044), Research and Development Foundation of Clinical Medicine of Jiangsu University (JLY20120013), Key Medical Talent Program of Zhenjiang City, and Jiangsu Government Scholarship for Overseas Studies.
Disclosure of conflict of interest
None.
Supporting Information
References
- 1.Look AT. Oncogenic transcription factors in the human acute leukemias. Science. 1997;278:1059–64. doi: 10.1126/science.278.5340.1059. [DOI] [PubMed] [Google Scholar]
- 2.Rowley JD. Chromosomal translocations: revisited yet again. Blood. 2008;112:2183–9. doi: 10.1182/blood-2008-04-097931. [DOI] [PubMed] [Google Scholar]
- 3.Tenen DG, Hromas R, Licht JD, Zhang DE. Transcription factors, normal myeloid development, and leukemia. Blood. 1997;90:489–519. [PubMed] [Google Scholar]
- 4.Renneville A, Roumier C, Biggio V, Nibourel O, Boissel N, Fenaux P, Preudhomme C. Cooperating gene mutations in acute myeloid leukemia: a review of the literature. Leukemia. 2008;22:915–31. doi: 10.1038/leu.2008.19. [DOI] [PubMed] [Google Scholar]
- 5.Shih AH, Abdel-Wahab O, Patel JP, Levine RL. The role of mutations in epigenetic regulators in myeloid malignancies. Nat Rev Cancer. 2012;12:599–612. doi: 10.1038/nrc3343. [DOI] [PubMed] [Google Scholar]
- 6.Chen J, Odenike O, Rowley JD. Leukaemogenesis: more than mutant genes. Nat Rev Cancer. 2010;10:23–36. doi: 10.1038/nrc2765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A, Paietta E, Willman CL, Head DR, Rowe JM, Forman SJ, Appelbaum FR. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood. 2000;96:4075–83. [PubMed] [Google Scholar]
- 8.Byrd JC, Mrózek K, Dodge RK, Carroll AJ, Edwards CG, Arthur DC, Pettenati MJ, Patil SR, Rao KW, Watson MS, Koduru PR, Moore JO, Stone RM, Mayer RJ, Feldman EJ, Davey FR, Schiffer CA, Larson RA, Bloomfield CD Cancer and Leukemia Group B (CALGB 8461) Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461) Blood. 2002;100:4325–36. doi: 10.1182/blood-2002-03-0772. [DOI] [PubMed] [Google Scholar]
- 9.Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH, Wheatley K, Harrison CJ, Burnett AK National Cancer Research Institute Adult Leukaemia Working Group. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116:354–65. doi: 10.1182/blood-2009-11-254441. [DOI] [PubMed] [Google Scholar]
- 10.Döhner H, Estey EH, Amadori S, Appelbaum FR, Büchner T, Burnett AK, Dombret H, Fenaux P, Grimwade D, Larson RA, Lo-Coco F, Naoe T, Niederwieser D, Ossenkoppele GJ, Sanz MA, Sierra J, Tallman MS, Löwenberg B, Bloomfield CD European LeukemiaNet. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010;115:453–74. doi: 10.1182/blood-2009-07-235358. [DOI] [PubMed] [Google Scholar]
- 11.Scott LM, Civin CI, Rorth P, Friedman AD. A novel temporal expression pattern of three C/EBP family members in differentiating myelomonocytic cells. Blood. 1992;80:1725–35. [PubMed] [Google Scholar]
- 12.Wang X, Scott E, Sawyers CL, Friedman AD. C/EBPα bypasses granulocyte colony-stimulating factor signals to rapidly induce PU. 1 gene expression, stimulate granulocytic differentiation, and limit proliferation in 32D cl3 myeloblasts. Blood. 1999;94:560–71. [PubMed] [Google Scholar]
- 13.Zhang P, Iwasaki-Arai J, Iwasaki H, Fenyus ML, Dayaram T, Owens BM, Shigematsu H, Levantini E, Huettner CS, Lekstrom-Himes JA, Akashi K, Tenen DG. Enhancement of hematopoietic stem cell repopulating capacity and self-renewal in the absence of the transcription factor C/EBPα. Immunity. 2004;21:853–63. doi: 10.1016/j.immuni.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Pabst T, Mueller BU, Zhang P, Radomska HS, Narravula S, Schnittger S, Behre G, Hiddemann W, Tenen DG. Dominant-negative mutations of CEBPA, encoding CCAAT/enhancer binding protein-alpha (C/EBPalpha), in acute myeloid leukemia. Nat Genet. 2001;27:263–70. doi: 10.1038/85820. [DOI] [PubMed] [Google Scholar]
- 15.Snaddon J, Smith ML, Neat M, Cambal-Parrales M, Dixon-McIver A, Arch R, Amess JA, Rohatiner AZ, Lister TA, Fitzgibbon J. Mutations of CEBPA in acute myeloid leukemia FAB types M1 and M2. Genes Chromosomes Cancer. 2003;37:72–8. doi: 10.1002/gcc.10185. [DOI] [PubMed] [Google Scholar]
- 16.Gombart AF, Hofmann WK, Kawano S, Takeuchi S, Krug U, Kwok SH, Larsen RJ, Asou H, Miller CW, Hoelzer D, Koeffler HP. Mutations in the gene encoding the transcription factor CCAAT/enhancer binding protein alpha in myelodysplastic syndromes and acute myeloid leukemias. Blood. 2002;99:1332–40. doi: 10.1182/blood.v99.4.1332. [DOI] [PubMed] [Google Scholar]
- 17.Barjesteh van Waalwijk van Doorn-Khosrovani S, Erpelinck C, Meijer J, van Oosterhoud S, van Putten WL, Valk PJ, Berna Beverloo H, Tenen DG, Löwenberg B, Delwel R. Biallelic mutations in the CEBPA gene and low CEBPA expression levels as prognostic markers in intermediate-risk AML. Hematol J. 2003;4:31–40. doi: 10.1038/sj.thj.6200216. [DOI] [PubMed] [Google Scholar]
- 18.Schwieger M, Löhler J, Fischer M, Herwig U, Tenen DG, Stocking C. A dominant-negative mutant of C/EBPalpha, associated with acute myeloid leukemias, inhibits differentiation of myeloid and erythroid progenitors of man but not mouse. Blood. 2004;103:2744–52. doi: 10.1182/blood-2003-07-2280. [DOI] [PubMed] [Google Scholar]
- 19.Mueller BU, Pabst T. C/EBPalpha and the pathophysiology of acute myeloid leukemia. Curr Opin Hematol. 2006;13:7–14. doi: 10.1097/01.moh.0000190110.08156.96. [DOI] [PubMed] [Google Scholar]
- 20.Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon, France: IARC Press; 2008. [Google Scholar]
- 21.Wouters BJ, Lowenberg B, Erpelinck-Verschueren CA, van Putten WL, Valk PJ, Delwel R. Double CEBPA mutations but not single CEBPA mutations, define a subgroup of acute myeloid leukemia with a distinctive gene expression profile that is uniquely associated with a favorable outcome. Blood. 2009;113:3088–91. doi: 10.1182/blood-2008-09-179895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pabst T, Eyholzer M, Fos J, Mueller BU. Heterogeneity within AML with CEBPA mutations: Only CEBPA double mutations, but not single CEBPA mutations are associated with favourable prognosis. Br J Cancer. 2009;100:1343–6. doi: 10.1038/sj.bjc.6604977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dufour A, Schneider F, Metzeler KH, Hoster E, Schneider S, Zellmeier E, Benthaus T, Sauerland MC, Berdel WE, Büchner T, Wörmann B, Braess J, Hiddemann W, Bohlander SK, Spiekermann K. Acute myeloid leukemia with biallelic CEBPA gene mutations and normal karyotype represents a distinct genetic entity associated with a favorable clinical outcome. J. Clin. Oncol. 2010;28:570–7. doi: 10.1200/JCO.2008.21.6010. [DOI] [PubMed] [Google Scholar]
- 24.Taskesen E, Bullinger L, Corbacioglu A, Sanders MA, Erpelinck CA, Wouters BJ, van der Poel-van de Luytgaarde SC, Damm F, Krauter J, Ganser A, Schlenk RF, Löwenberg B, Delwel R, Döhner H, Valk PJ, Döhner K. Prognostic impact, concurrent genetic mutations, and gene expression features of AML with CEBPA mutations in a cohort of 1182 cytogenetically normal AML patients: further evidence for CEBPA double mutant AML as a distinctive disease entity. Blood. 2011;117:2469–75. doi: 10.1182/blood-2010-09-307280. [DOI] [PubMed] [Google Scholar]
- 25.Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, Sultan C. Proposed revised criteria for the classification of acute myeloid leukaemia. A report of the French-American-British Cooperative Group. Ann Intern Med. 1985;103:620–5. doi: 10.7326/0003-4819-103-4-620. [DOI] [PubMed] [Google Scholar]
- 26.Li Y, Lin J, Yang J, Qian J, Qian W, Yao DM, Deng ZQ, Liu Q, Chen XX, Xie D, An C, Tang CY. Overexpressed let-7a-3 is associated with poor outcome in acute myeloid leukemia. Leuk Res. 2013;37:1642–7. doi: 10.1016/j.leukres.2013.09.022. [DOI] [PubMed] [Google Scholar]
- 27.Mitelman F. In: An International system for human cytogenetic nomenclature. ISCN, editor. Basel: Karger; 1995. [Google Scholar]
- 28.Lin J, Yao DM, Qian J, Chen Q, Qian W, Li Y, Yang J, Wang CZ, Chai HY, Qian Z, Xiao GF, Xu WR. Recurrent DNMT3A R882 mutations in Chinese patients with acute myeloid leukemia and myelodysplastic syndrome. PLoS One. 2011;6:e26906. doi: 10.1371/journal.pone.0026906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin J, Yao DM, Qian J, Chen Q, Qian W, Li Y, Yang J, Wang CZ, Chai HY, Qian Z, Xiao GF, Xu WR. IDH1 and IDH2 mutation analysis in Chinese patients with acute myeloid leukemia and myelodysplastic syndrome. Ann Hematol. 2012;91:519–25. doi: 10.1007/s00277-011-1352-7. [DOI] [PubMed] [Google Scholar]
- 30.Yang X, Qian J, Sun A, Lin J, Xiao G, Yin J, Chen S, Wu D. RAS mutation analysis in a large cohort of Chinese patients with acute myeloid leukemia. Clin Biochem. 2013;46:579–83. doi: 10.1016/j.clinbiochem.2012.12.022. [DOI] [PubMed] [Google Scholar]
- 31.Kihara R, Nagata Y, Kiyoi H, Kato T, Yamamoto E, Suzuki K, Chen F, Asou N, Ohtake S, Miyawaki S, Miyazaki Y, Sakura T, Ozawa Y, Usui N, Kanamori H, Kiguchi T, Imai K, Uike N, Kimura F, Kitamura K, Nakaseko C, Onizuka M, Takeshita A, Ishida F, Suzushima H, Kato Y, Miwa H, Shiraishi Y, Chiba K, Tanaka H, Miyano S, Ogawa S, Naoe T. Comprehensive analysis of genetic alterations and their prognostic impacts in adult acute myeloid leukemia patients. Leukemia. 2014;28:1586–95. doi: 10.1038/leu.2014.55. [DOI] [PubMed] [Google Scholar]
- 32.Lin LI, Chen CY, Lin DT, Tsay W, Tang JL, Yeh YC, Shen HL, Su FH, Yao M, Huang SY, Tien HF. Characterization of CEBPA mutations in acute myeloid leukemia: most patients with CEBPA mutations have biallelic mutations and show a distinct immunophenotype of the leukemic cells. Clin Cancer Res. 2005;11:1372–9. doi: 10.1158/1078-0432.CCR-04-1816. [DOI] [PubMed] [Google Scholar]
- 33.Fasan A, Haferlach C, Alpermann T, Jeromin S, Grossmann V, Eder C, Weissmann S, Dicker F, Kohlmann A, Schindela S, Kern W, Haferlach T, Schnittger S. The role of different genetic subtypes of CEBPA mutated AML. Leukemia. 2014;28:794–803. doi: 10.1038/leu.2013.273. [DOI] [PubMed] [Google Scholar]
- 34.Fröhling S, Schlenk RF, Stolze I, Bihlmayr J, Benner A, Kreitmeier S, Tobis K, Döhner H, Döhner K. CEBPA mutations in younger adults with acute myeloid leukemia and normal cytogenetics: prognostic relevance and analysis of cooperating mutations. J. Clin. Oncol. 2004;22:624–33. doi: 10.1200/JCO.2004.06.060. [DOI] [PubMed] [Google Scholar]
- 35.Shen Y, Zhu YM, Fan X, Shi JY, Wang QR, Yan XJ, Gu ZH, Wang YY, Chen B, Jiang CL, Yan H, Chen FF, Chen HM, Chen Z, Jin J, Chen SJ. Gene mutation patterns and their prognostic impact in a cohort of 1185 patients with acute myeloid leukemia. Blood. 2011;118:5593–603. doi: 10.1182/blood-2011-03-343988. [DOI] [PubMed] [Google Scholar]
- 36.Green CL, Koo KK, Hills RK, Burnett AK, Linch DC, Gale RE. Prognostic significance of CEBPA mutations in a large cohort of younger adult patients with acute myeloid leukemia: impact of double CEBPA mutations and the interaction with FLT3 and NPM1 mutations. J. Clin. Oncol. 2010;28:2739–47. doi: 10.1200/JCO.2009.26.2501. [DOI] [PubMed] [Google Scholar]
- 37.Grossmann V, Schnittger S, Kohlmann A, Eder C, Roller A, Dicker F, Schmid C, Wendtner CM, Staib P, Serve H, Kreuzer KA, Kern W, Haferlach T, Haferlach C. A novel hierarchical prognostic model of AML solely based on molecular mutations. Blood. 2012;120:2963–72. doi: 10.1182/blood-2012-03-419622. [DOI] [PubMed] [Google Scholar]
- 38.Preudhomme C, Sagot C, Boissel N, Cayuela JM, Tigaud I, de Botton S, Thomas X, Raffoux E, Lamandin C, Castaigne S, Fenaux P, Dombret H ALFA Group. Favorable prognostic significance of CEBPA mutations in patients with de novo acute myeloid leukemia: a study from the Acute Leukemia French Association (ALFA) Blood. 2002;100:2717–23. doi: 10.1182/blood-2002-03-0990. [DOI] [PubMed] [Google Scholar]
- 39.Grossmann V, Haferlach C, Nadarajah N, Fasan A, Weissmann S, Roller A, Eder C, Stopp E, Kern W, Haferlach T, Kohlmann A, Schnittger S. CEBPA double-mutated acute myeloid leukaemia harbours concomitant molecular mutations in 76·8% of cases with TET2 and GATA2 alterations impacting prognosis. Br J Haematol. 2013;161:649–58. doi: 10.1111/bjh.12297. [DOI] [PubMed] [Google Scholar]
- 40.Fasan A, Eder C, Haferlach C, Grossmann V, Kohlmann A, Dicker F, Kern W, Haferlach T, Schnittger S. GATA2 mutations are frequent in intermediate-risk karyotype AML with biallelic CEBPA mutations and are associated with favorable prognosis. Leukemia. 2013;27:482–5. doi: 10.1038/leu.2012.174. [DOI] [PubMed] [Google Scholar]
- 41.Dufour A, Schneider F, Hoster E, Benthaus T, Ksienzyk B, Schneider S, Kakadia PM, Sauerland MC, Berdel WE, Büchner T, Wörmann B, Braess J, Subklewe M, Hiddemann W, Bohlander SK, Spiekermann K AML CG study group. Monoallelic CEBPA mutations in normal karyotype acute myeloid leukemia: independent favorable prognostic factor within NPM1 mutated patients. Ann Hematol. 2012;91:1051–63. doi: 10.1007/s00277-012-1423-4. [DOI] [PubMed] [Google Scholar]
- 42.Park SH, Chi HS, Cho YU, Jang S, Park CJ. CEBPA single mutation can be a possible favorable prognostic indicator in NPM1 and FLT3-ITD wild-type acute myeloid leukemia patients with intermediate cytogenetic risk. Leuk Res. 2013;37:1488–94. doi: 10.1016/j.leukres.2013.08.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


