Abstract
The accountable care organization (ACO) model of health care delivery is rapidly being implemented under government and private-sector initiatives. The model requires that each ACO have a defined patient population for which the ACO will be held accountable for both total cost of care and quality performance. However, there is no empirical evidence about the best way to define how patients are assigned to these groups of doctors, hospitals, and other health care providers. We examined the two major methods of defining, or attributing, patient populations to ACOs: the prospective method and the performance year method. The prospective method uses data from one year to assign patients to an ACO for the following performance year. The performance year method assigns patients to an ACO at the end of the performance year based on the population served during the performance year. We used Medicare fee-for-service claims data from 2008 and 2009 to simulate a set of ACOs to compare the two methods. Although both methods have benefits and drawbacks, we found that attributing patients using the performance year method yielded greater overlap of attributed patients and patients treated during the performance year and resulted in a higher proportion of care concentrated within an accountable care organization. Together, these results suggest that performance year attribution may more fully and accurately reflect an ACO’s patient population and may better position an ACO to achieve shared savings.
New models of health care delivery are moving toward holding providers accountable for the health, quality of care, and costs of a defined patient population. In particular, implementation of accountable care organizations (ACOs) is rapidly moving forward. Medicare began three accountable care organization programs in 2012. The Pioneer ACO program began contracts with 32 advanced organizations in January 2012, and the Medicare Shared Savings Program—Medicare’s larger program, with a much broader set of participating organizations—started contracts with 115 participant organizations in 2012 and another 106 in January 2013. In addition, the Advance Payment Program provides eligible Shared Savings Program participants with advances on anticipated shared savings. The program aims to help small or underresourced ACOs build infrastructure and capacity to achieve cost and quality benchmarks.
At the same time, several states are implementing Medicaid accountable care organizations. Private-sector accountable care organizations are also proliferating, with more than 160 initiatives under way.
As accountable care organizations are implemented, a key concern for stakeholders is defining the timing and methodology for assigning patients to the accountable care organization.1–5 ACO contracts require an attribution methodology to define the population for which providers will be held accountable for quality and cost.6,7 There are several methods of attributing a population to an accountable care organization, each with benefits and drawbacks.8–11
The release of the proposed and final rules for the Medicare Shared Savings Program and regulations for the Pioneer ACO program alongside widespread growth in commercial ACO contracts sparked strong debate among stakeholders—including physicians, payers, and patient advocates—about what methodology provides the fairest and most accurate way to assign patients to accountable care organizations. Two primary approaches for attribution are possible.
The first method is to assign patients to an accountable care organization for the coming performance year based on each patient’s use of services in the prior year—a method known as prospective attribution. The second method is to wait until the end of the performance year and then assign patients to an accountable care organization based on their use of services in the completed performance year—a method known as retrospective or performance year attribution.
We used 2008 and 2009 Medicare claims data to simulate potential Medicare accountable care organizations. We then examined prospective attribution and performance year attribution to evaluate how the two methods compare across a set of outcome measures. In particular, we examined how the two methods compared on the alignment of assigned patients with patients cared for during the performance year, the extent to which patient care was concentrated within a given network, and whether or not ACOs could realistically identify their assigned patient populations. Overall, our data suggest that performance year attribution offers advantages on several of these counts.
Attribution Methods
PROSPECTIVE ATTRIBUTION
Some providers favor a prospective method of attribution, in which at the beginning of a performance year accountable care organizations are given a list of patients for whom they will be responsible; this list is based on data from the patients’ use of services in the previous year.1,2,10,12 When given a choice between prospective or performance year attribution, all thirty-two of Medicare’s Pioneer ACO program participants selected prospective attribution.
The most prominent benefit of this method is that providers can reach out to assigned patients proactively to coordinate care and develop tailored care management programs.1,3–5,10,12–14 Since physicians know exactly which patients will be included for performance evaluation, they can actively coordinate with patients, such as by encouraging preventive care and routine exams, in an effort to improve quality and reduce costs. In addition, prospective attribution initially prevents providers from selectively avoiding patients that providers perceive as difficult or likely to negatively affect their performance. Of course, since prospective attribution is updated yearly, providers could selectively avoid patients to favorably alter attribution moving forward.
PERFORMANCE YEAR ATTRIBUTION
Other stakeholders support retrospective or performance year attribution, which assigns patients to an accountable care organization at the end of the year based on patients’ use of care during the actual performance year. Performance year attribution is thought to provide two major benefits to providers.15
First, performance year attribution removes patients who no longer receive care from the organization, including those who have moved or sought care from other providers. Providers are then responsible for the cost and quality of care of only those patients for whom they provided care in the performance year. Second, performance year attribution ensures that accountable care organizations are credited for the care of patients who initiated care during the performance year, such as those aging into Medicare upon turning sixty-five or those choosing a new doctor for any one of a variety of reasons.16
MEDICARE’S HYBRID APPROACH
In the final rule for the Medicare Shared Savings Program, the Centers for Medicare and Medicaid Services elected a third, hybrid approach that it termed a “preliminary prospective assignment methodology with final retrospective reconciliation.”1(p67864) The hybrid approach begins with prospective attribution; each quarter, program participants receive a list of patients prospectively attributed to their accountable care organizations based on the most recent twelve months of data.
In effect, these are lists of patients who are likely to be attributed to a given accountable care organization. Assignment is regularly updated to include new patients in practices and to remove patients who are no longer receiving care from the ACO’s providers—a process referred to as retrospective reconciliation.6 The final reconciliation takes place at the end of the performance year based solely on patients’ use of services in that performance year. As a result of the reconciliation, the final attributed population under the hybrid method is identical to a purely retrospective attributed population.
To date, the two basic attribution methods, prospective and performance year, have not been compared empirically. Although the arguments laid out above for and against each method have been based on logic, direct data have not been used to examine which arguments are most accurate.
For the purposes of this article, we examined the differences between prospective attribution and performance year attribution in terms of the alignment of patients attributed and those cared for during a performance year and the concentration of care within the accountable care organization. We also reflect on whether it is possible for accountable care organizations to identify probable assigned patients independent of prospective attribution lists provided by a payer, such as Medicare.
Study Data And Methods
SIMULATED ACCOUNTABLE CARE ORGANIZATIONS
Using 100 percent Medicare fee-for-service claims data from 2008 and 2009, we created empirically defined, simulated accountable care organizations caring for at least 5,000 Medicare beneficiaries—the minimum threshold for organizations to take part in Medicare’s ACO programs. We simulated these accountable care organizations based on the established methodology of naturally occurring physician-hospital networks.17,18
We derived our simulated ACOs directly from the Medicare claims data, as explained in the Appendix, Part A.19 We began with all physicians billing Medicare. Physicians were linked to the hospital where they performed the plurality of their work during the calendar year. If a physician did not bill for any inpatient care, he or she was linked to the hospital where the plurality of his or her patients were referred and admitted. This linkage created a naturally occurring network of physicians around each hospital. We referred to each of these natural networks as a simulated accountable care organization.
Beneficiaries were then attributed to one of these physician networks, or simulated accountable care organizations. Beneficiaries were attributed to the physician from whom they received the plurality of their evaluation and management outpatient care. The specific methodology is explained in the Appendix, Part B.19
We used a two-step attribution process matching the attribution methodology of Medicare’s largest and ongoing ACO program, the Medicare Shared Savings Program. We first attributed patients to their predominant primary care physician. For patients without any visits to primary care physicians, we attributed them to the specialist, nurse practitioner, physician assistant, or clinical nurse specialist who provided the plurality of the patient’s outpatient evaluation and management care.
PROSPECTIVE AND PERFORMANCE YEAR ATTRIBUTION
For prospective attribution, we used 2008 data on patients’ use of services to attribute patients for a hypothetical 2009 performance year. For performance year attribution, we attributed patients using 2009 data on patients’ use of services for a hypothetical 2009 performance year.
We tried several alternative specifications of our attribution methodology, including methods such as shifting which physicians were eligible for attribution (that is, attributing patients only through a primary care physician and excluding specialists), using a subset of all possible simulated accountable care organizations rather than the entire set of possible accountable care organizations, and changing the minimum number of beneficiaries required to be considered an ACO. Our substantive results were the same regardless of how we altered the specifications.
In our analysis we compared the set of patients attributed to a simulated accountable care organization and the set of patients who received care at the ACO during the hypothetical performance year. We defined receiving care during a performance year as a patient having an out-patient evaluation and management visit at a given accountable care organization. We focused on these outpatient evaluation and management visits—as opposed to inpatient hospital stays, for example—because the visits represented on-going clinician contacts through which the advantages of having a prospective patient list for care coordination would be borne out. For the same reason, we paid particular attention to primary care throughout the analyses. For all results, we report the average value for all simulated accountable care organizations with more than 5,000 attributed Medicare beneficiaries.
LIMITATIONS
This analysis has limitations, including the use of Medicare data that represent only a subset of the total population. Although this would be a serious limitation for certain research questions, it is unlikely that the two attribution methods would be systematically different or interpretation reversed in a commercially insured patient population.
Another important limitation is that our data examined hypothetical accountable care organizations based on naturally occurring networks using observational data. These networks were based on flow of patients to physicians and hospitals, using the hospital as the link between the physicians. It is unknown how our observed networks relate to actual ACOs, which are more likely to arise from corporate relationships between providers than from relationships derived from work at or referrals to the same hospital. As more information on new accountable care organizations becomes available, empirical research could examine this question.
We are reassured that the nature of the provider group would make little difference in our main findings, based on our examination of how results varied across types of simulated accountable care organizations presented in the following section.
Study Results
We derived 1,642 simulated ACOs for 2009, each with at least 5,000 Medicare beneficiaries. Medicare attribution rules place priority on attributing patients to primary care providers, and patients are assigned based on specialist visits only if they visit no primary care physicians; this methodology is likely to be similar in commercial ACO contracts. We found that 81–82 percent of patients were assigned through a primary care physician, while only 18–19 percent were attributed through specialist care (Exhibit 1).
EXHIBIT 1.
Comparison Of Prospective Attribution And Performance Year Attribution To Simulated Accountable Care Organizations (ACOs)
| Prospective attribution |
Performance year attribution |
|
|---|---|---|
| SIMULATED ACOS AND ATTRIBUTION | ||
| Number of ACOs with >5,000 patients | 1,642 | 1,642 |
| Mean number of assigned patients | 10,668 | 11,437 |
| Patients assigned through primary care physician | 82% | 81% |
| Patients assigned through specialists | 18% | 19% |
| ATTRIBUTED POPULATION | ||
| Percent visiting ACO during performance year | 83 | 100 |
| Percent visiting an ACO primary care physician during performance year |
69 | 81 |
| PATIENTS VISITING DURING PERFORMANCE YEAR | ||
| Percent attributed | 45 | 57 |
| Percent attributed to primary care physician | 36 | 49 |
| Percent attributed of those visiting a primary care physician |
62 | 86 |
| PATIENT LOYALTY | ||
| Percent of assigned patients’ performance year visits occurring within the ACO |
68 | 74 |
SOURCE Authors’ analysis of 100 percent Medicare fee-for-service claims data, 2008–09.
Our data showed several important differences between prospective attribution and performance year attribution that would have an impact on providers. We analyzed three topics of concern raised by stakeholders during the development of the Medicare attribution rules. It is likely that these topics are also of concern to organizations developing commercial and Medicaid accountable care contracts.
We began by examining the overlap between attributed patients and patients visiting the accountable care organization during the performance year. First, we examined assigned patients who did not receive care within the organization—an issue unique to prospective attribution, such as when patients move out of the area or switch providers. Second, we examined the extent to which patients who received care at an accountable care organization were not assigned to that organization; this occurs under both attribution models.
Third, we examined how the two methods differed in terms of the proportion of attributed patients’ total visits and costs that occurred within the accountable care organization during the performance year. This analysis assumed that providers would prefer to concentrate visits within an ACO in order to maximize their influence over quality and cost.
PATIENTS ASSIGNED TO BUT NOT VISITING AN ACO DURING PERFORMANCE YEAR
Under prospective attribution, some patients who are assigned to an accountable care organization may in fact not visit one of that organization’s providers during the performance year. The left-hand diagram in Exhibit 2 illustrates this gap: patients prospectively attributed to an accountable care organization are shown in red, and patients visiting accountable care organization providers during the performance year are shown in blue. On average, 17 percent of prospectively assigned patients did not receive care from their accountable care organization providers during the performance year, and 31 percent did not receive care from a primary care physician in an accountable care organization (Exhibit 1). This proportion varied little by region, academic medical center status, rural or urban status, or the size of the accountable care organization (Exhibit 3).
EXHIBIT 2. Comparison Of Prospective Attribution And Performance Year Attribution To Accountable Care Organizations (ACOs): Mean Population Receiving Primary Care Services From All ACO Providers.
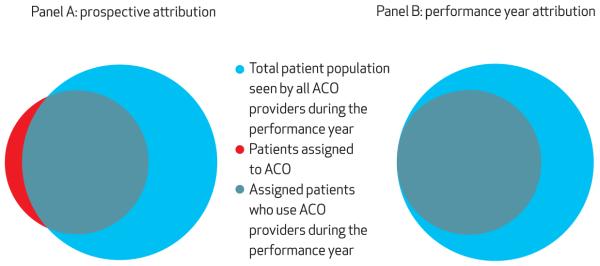
SOURCE Authors’ analysis of 100 percent Medicare fee-for-service claims data, 2008–09. NOTES “All ACO providers” includes primary care physicians, specialists, and other nonphysician providers. Sample sizes are as follows. Total patient population seen by ACO providers, Panel A: 21,231; Panel B: 21,231. Patients assigned to ACO, Panel A:11,511; Panel B: 11,437. Panel A overlap: 9,554.
EXHIBIT 3.
Variation In Key Measures Of Interest By Region, Academic Medical Center Status, Urbanicity, And Size Of Accountable Care Organization (ACO)
| Percent of those visiting during performance year attributed |
Percent of those visiting a PCP during performance year attributed |
Percent of visits occurring within ACO |
|||||
|---|---|---|---|---|---|---|---|
| Number | Prospective | Performance year |
Prospective | Performance year |
Prospective | Performance year |
|
| OVERALL | |||||||
| Mean | — a | 44.7 | 56.6 | 62.4 | 85.6 | 68.4 | 74.2 |
| 25th percentile | — a | 36.5 | 48.5 | 55.7 | 82.2 | 57.1 | 65.0 |
| 75th percentile | — a | 53.6 | 65.0 | 70.9 | 90.3 | 82.4 | 85.7 |
| REGION | |||||||
| Midwest | 399 | 45.6 | 57.2 | 64.6 | 86.2 | 70.4 | 75.5 |
| Northeast | 331 | 45.1 | 56.1 | 63.3 | 85.4 | 66.4 | 71.5 |
| South | 638 | 43.8 | 55.4 | 62.0 | 85.5 | 67.6 | 73.6 |
| West | 274 | 45.0 | 59.5 | 58.8 | 85.3 | 69.8 | 77.2 |
| ACADEMIC MEDICAL CENTER | |||||||
| Yes | 686 | 40.8 | 52.7 | 59.1 | 83.5 | 63.4 | 69.7 |
| No | 956 | 47.6 | 59.5 | 64.7 | 87.1 | 72.1 | 77.5 |
| URBANICITY | |||||||
| Rural | 259 | 54.6 | 66.4 | 70.0 | 89.5 | 81.0 | 84.9 |
| Urban | 1,383 | 42.9 | 54.8 | 60.9 | 84.9 | 66.1 | 72.2 |
| SIZE OF ACO (no. of BENEFICIARIES) | |||||||
| <10,000 | 877 | 45.1 | 57.2 | 62.6 | 85.7 | 68.9 | 74.8 |
| 10,000–15,000 | 412 | 44.0 | 55.6 | 62.1 | 85.4 | 68.0 | 73.5 |
| >15,000 | 353 | 44.7 | 56.3 | 62.2 | 85.6 | 67.8 | 73.6 |
SOURCE Authors’ analysis of 100 percent Medicare fee-for-service claims data, 2008–09. NOTES N= 1,642. PCP is primary care physician.
Not applicable.
In contrast, performance year attribution included only patients who used the accountable care organization during the performance year, meaning that 100 percent of assigned patients received care from accountable care organization providers during the performance year. In addition, 81 percent of patients assigned using performance year attribution received care from a primary care physician in an ACO.
The implications of these figures on the misalignment of patient populations are critical within a payment model emphasizing accountability. For prospective attribution, the proportion of attributed patients not visiting the ACO during the performance year was substantial, leaving the organizations responsible for both the cost and quality of care of patients for whom they had little or no impact.
It is unknown how difficult or easy it may be to reach such patients. For example, some patients might move out of state and become nearly impossible to reach, while for others a simple phone call might be all that is needed to prompt them to come in for care. Nevertheless, such patients would be an important consideration for providers under prospective attribution.
PATIENTS RECEIVING CARE DURING A PERFORMANCE YEAR BUT NOT ASSIGNED
Next we examined patients who visited an accountable care organization but were not attributed to the organization. Under prospective attribution, an average of 45 percent of patients who visited an accountable care organization’s providers during a performance year were prospectively attributed, leaving 55 percent of patients who visited such providers not attributed to the organization.
In contrast, under performance year attribution, 57 percent of patients visiting all accountable care organization providers were attributed, and only 43 percent were not. These numbers are high because they include visits to primary care physicians as well as to specialists and other providers. Many patients with visits to an accountable care organization’s specialists were not attributed to the organization because they saw primary care physicians in a different simulated ACO, and attribution methods favored primary care physicians for assignment.
When we focused on primary care physicians, these values were considerably smaller but had the same pattern. Under prospective attribution, 62 percent of patients visiting an accountable care organization’s primary care physicians during a performance year were attributed; under performance year attribution, 86 percent of patients visiting such physicians during the performance year were attributed.
The unattributed patients who received care at the accountable care organization during the performance year have different implications for the two attribution methods. Under prospective attribution, an ACO is aware that these patients are not on its assigned list, and therefore the organization need not expend specific resources on these patients. For example, they need not enroll these patients in new or developmental interventions that are designed to improve quality for patients and that in turn lead to shared savings. Instead, accountable care organizations can target only their assigned patients and conserve resources. At the same time, there is a potential risk that a prospective attribution methodology creates incentives to direct resources to assigned patients who are evaluated for cost and quality of care, possibly resulting in two standards of care—one for patients assigned to the ACO and one for the rest of an organization’s patients.
Performance year attribution also has inherent difficulties associated with patients who are treated by the accountable care organization but remain unassigned. Because patients are assigned at the end of the performance year, an ACO would not know which of the patients visiting its providers would ultimately be assigned to it and which would not. The organization must either make educated guesses about which patients will be assigned to it or treat all patients as if they were accountable care organization patients. For example, any new interventions, resources, or programs intended to enhance quality or cost performance would be likely to focus on all primary care patients, including the 14 percent who will ultimately not be assigned to the ACO.
These “free riders,” so to speak, may dilute the impact of accountable care organization programs on attributed beneficiaries and reduce the organization’s ability to achieve shared savings to support investments made in care redesign. Alternatively, these types of programs may result in a patient’s returning to the ACO and ultimately lead to greater attribution. Effective accountable care interventions could increase the proportion of treated patients that is ultimately assigned under performance year attribution and could close the gap between the population visiting the organization within a performance year and the population assigned to the accountable care organization.
CONCENTRATION OF CARE WITHIN THE ACO
Finally, we examined the proportion of assigned patients’ visits and costs that occur within the accountable care organization under the two attribution models. Providers will probably benefit the most from attribution models that result in a larger share of their patients’ visits taking place within the organization. Patient visits are the major avenue for affecting patient care, including initiating necessary care to meet quality benchmarks (such as encouraging a patient to complete preventive screenings like mammograms or colorectal cancer screening) and reducing avoidable high-cost care (such as unnecessary imaging). In addition, patient visits are a likely starting point for initiating care coordination or care management for chronic conditions such as diabetes—a concept fundamental to accountable care and other population-based health care delivery models.
Our examination of the proportion of patients’ visits that took place within a given accountable care organization under both attribution methods showed that a lower proportion of visits were made to accountable care providers under prospective attribution (68 percent) compared to the proportion under performance year attribution (74 percent) (Exhibit 1).
IMPLICATIONS OF SIMULATED ACOS
The data used to simulate attribution in these accountable care organizations were based on fee-for-service care patterns in Medicare during a period when little was being done to coordinate care or hold large groups of providers accountable for costs and quality of care. We expect that as real ACOs implement interventions to affect quality and cost, the proportion of attributed patients who receive care and the proportion of services that occur within each organization’s network of providers will probably increase, regardless of the attribution methodology chosen.
These numbers will probably increase because the existence of formal networks within accountable care organizations will greatly increase referrals within the organization in two ways. First, ACOs may adopt care coordination programs to help patients obtain visits with specialists who work closely with referring primary care physicians. Second, the use of effective disease management programs may encourage patients who see a specialist but not a primary care physician within the accountable care organization to move their care to an affiliated primary care practice.
If these circumstances did arise, the effect might be to reduce the differences between the two attribution methods, but this narrowing would be unlikely to completely close the gaps. Thus, our estimates of care concentrated within a simulated accountable care organization may be conservative compared to what might be expected after an organization has been formally implemented.
Discussion
This study used empirical analyses to compare the benefits of prospective attribution and performance year attribution. The results indicate that performance year attribution may have several attractive qualities to provider groups.
First, performance year attribution ensures that providers are not held responsible for any patients who do not seek care at the accountable care organization during the performance year. In addition, it ensures that a larger share of an ACO’s patients are actually attributed to the organization. Finally, performance year attribution results in a somewhat larger share of assigned patients’ visits taking place with the patients’ ACO providers, perhaps making the accountable care organization better able to influence patient care for the purposes of both quality and cost performance.
Although our overall assessment is that performance year attribution is a more favorable methodology for providers participating in accountable care contracts, prospective attribution does have some potential benefits. As noted in the results, performance year attribution may result in some wasted effort on the part of organizations as a result of “free riders”—patients who receive care at an accountable care organization but are not ultimately attributed to that organization. Because final assignment happens at the end of a year under the performance year method, providers are unable to identify which patients will or will not be assigned to them and thus must apply accountable care initiatives to their entire patient population. This reality will probably result in some wasted effort on patients who are ultimately not assigned to the ACO. In contrast, prospective attribution avoids the problem of free riders and allows physicians to proactively reach out to assigned patients.
Our analysis also points to a broader underlying finding regarding the important role that primary care could play in identifying likely assigned patients in the absence of preliminary prospective attribution lists. Taking notice of the central role of primary care in attribution could allow providers to realize the advantages of prospective patient identification when using performance year attribution. Our analysis suggests that providers can identify a large portion of their assigned population: Nearly all patients visiting primary care physicians during the performance year are assigned under performance year attribution.
Conclusion
Overall, our results indicate several important findings. First, performance year attribution, compared to prospective attribution, ensures a larger overlap of the assigned patient population and the set of patients visiting an accountable care organization during a performance year. This increased overlap is critical because under accountable care, providers are held responsible for the quality and cost of care for their attributed patients, regardless of where those patients seek care. Removing from the attributed population those patients who do not use the ACO and including patients who have initiated care at the ACO ensures that physicians are held accountable for the costs and quality of care for patients they actively played a role in caring for during the performance year.
Second, performance year attribution results in a greater concentration of costs for attributed patients within the accountable care organization, increasing the organization’s ability to achieve shared savings. Third, although prospective attribution allows accountable care organizations to avoid the problems of free riders and wasted resources on patients who are ultimately not attributed to them, our results indicate that performance year attribution can also avoid these two problems. The data suggest that ACOs can largely identify their likely patients by focusing on their primary care patients, who overwhelmingly become attributed to them under a performance year methodology. These results indicate that performance year attribution holds promise as a beneficial methodology for future and developing accountable care organizations.
Acknowledgments
The study was supported in part by a grant from the Commonwealth Fund.
Biographies
Valerie A. Lewis is an assistant professor at the Dartmouth Institute for Health Policy and Clinical Practice.

In this month’s Health Affairs, Valerie Lewis and coauthors examine the two primary methods for attributing patients to accountable care organizations (ACOs): the prospective method and the performance year method, both described in the article. Using Medicare fee-for-service claims data to simulate a set of ACOs, they found that attributing patients using the performance year method creates a much larger overlap between an ACO’s attributed population and the patients an ACO saw during a hypothetical performance year. These results suggest that performance year attribution may more fully and accurately reflect an ACO’s patient population and may better position an ACO to achieve shared savings.
Lewis is an assistant professor at the Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine, Dartmouth College. Her work focuses on the impact of delivery system reform on disadvantaged groups. Lewis earned doctoral and master’s degrees in sociology from Princeton University.
Asha Belle McClurg is a medical student at the Geisel School of Medicine at Dartmouth.

Asha McClurg is a former health policy fellow at the Dartmouth Institute, where she studied accountable care organizations and payment reform. She is now a medical student and Urban Health Scholar at the Geisel School of Medicine at Dartmouth. She received a bachelor’s degree in biology and integrative physiology from the University of Colorado.
Jeremy Smith is a statistical research analyst at the Dartmouth Institute.

Jeremy Smith is a statistical research analyst at the Dartmouth Institute for Health Policy and Clinical Practice, where his numerous responsibilities include conducting observational pharmacoepidemiologic studies using Medicare claims data and participating in health policy research relating to ACOs and other payment and care reform initiatives. Smith earned a master’s degree in public health from the University of Minnesota.
Elliott S. Fisher is the director of the Center for Population Health at the Dartmouth Institute.
Elliott Fisher is the director of the Center for Population Health at the Dartmouth Institute for Health Policy and Clinical Practice. He is a professor of medicine and of community and family medicine at the Geisel School of Medicine at Dartmouth. He is also the co–principal investigator for the Dartmouth Atlas of Health Care. His research has focused on exploring the causes of the twofold differences in spending observed across US regions and health care systems, understanding the consequences of these variations on health, and developing and testing approaches to performance measurement and payment reform that can support improvement. Fisher received a master’s degree in public health from the University of Washington and a medical degree from Harvard University.
Julie P.W. Bynum is an associate professor of medicine and associate director of the Center for Health Policy Research, Dartmouth Institute.

Julie Bynum is an associate professor of medicine and associate director of the Center for Health Policy Research at the Dartmouth Institute for Health Policy and Clinical Practice. Her research focuses on the assessment of health system performance in the quality and costs of care for the elderly served by Medicare. She holds a master’s degree in public health from the Johns Hopkins University, where she also received a medical degree and specialty training in geriatrics.
Footnotes
A version of this article was presented at the AcademyHealth Annual Research Meeting in Orlando, Florida, June 24, 2012.
To access the Appendix, click on the Appendix link in the box to the right of the article online.
Contributor Information
Valerie A. Lewis, Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth, in Hanover, New Hampshire.
Asha Belle McClurg, Geisel School of Medicine at Dartmouth.
Jeremy Smith, Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth.
Elliott S. Fisher, Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth.
Julie P.W. Bynum, Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth.
NOTES
- 1.Centers for Medicare and Medicaid Services Medicare Shared Savings Program: accountable care organizations, final rule. Fed Regist. 2011;76(212):67801–990. [PubMed] [Google Scholar]
- 2.Lieberman S. Proposed CMS regulation kills ACOs softly. Health Affairs Blog [blog on the Internet] 2011 Apr 6; [cited 2011 Dec 13]. Available from: http://healthaffairs.org/blog/2011/04/06/proposed-cms-regulation-kills-acos-softly/
- 3.Klar R. The importance of the shared-savings ACO model. Health Affairs Blog [blog on the Internet] 2011 Jan 25; [cited 2011 Dec 13]. Available from: http://healthaffairs.org/blog/2011/01/25/the-importance-of-the-shared-savings-aco-model/
- 4.Maves MD. American Medical Association CMS ACO comment letter. AMA; Chicago (IL): 2010. [Google Scholar]
- 5.Ginsburg PB. Spending to save—ACOs and the Medicare Shared Savings Program. N Engl J Med. 2011;364(22):2085–6. doi: 10.1056/NEJMp1103604. [DOI] [PubMed] [Google Scholar]
- 6.Higgins A, Stewart K, Dawson K, Bocchino C. Early lessons from accountable care models in the private sector: partnerships between health plans and providers. Health Aff (Millwood) 2011;30(9):1718–27. doi: 10.1377/hlthaff.2011.0561. [DOI] [PubMed] [Google Scholar]
- 7.Luft HS. Becoming accountable—opportunities and obstacles for ACOs. N Engl J Med. 2010;363(15):1389–91. doi: 10.1056/NEJMp1009380. [DOI] [PubMed] [Google Scholar]
- 8.Larson BK, van Citters AD, Kreindler SA, Carluzzo KL, Gbemudu JN, Wu FM, et al. Insights from transformations under way at four Brookings-Dartmouth accountable care organization pilot sites. Health Aff (Millwood) 2012;31(11):2395–406. doi: 10.1377/hlthaff.2011.1219. [DOI] [PubMed] [Google Scholar]
- 9.Mehrotra A, Adams JL, Thomas JW, McGlynn EA. The effect of different attribution rules on individual physician cost profiles. Ann Intern Med. 2010;152(10):649–54. doi: 10.1059/0003-4819-152-10-201005180-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pantely SE. Whose patient is it? Patient attribution in ACOs. Milliman; Seattle (WA): 2011. pp. 1–3. [Google Scholar]
- 11.McClellan M, McKethan AN, Lewis JL, Roski J, Fisher ES. A national strategy to put accountable care into practice. Health Aff (Millwood) 2010;29(5):982–90. doi: 10.1377/hlthaff.2010.0194. [DOI] [PubMed] [Google Scholar]
- 12.Lieberman SM, Bertko JM. Building regulatory and operational flexibility into accountable care organizations and “shared savings. Health Aff (Millwood) 2011;30(1):23–31. doi: 10.1377/hlthaff.2010.0928. [DOI] [PubMed] [Google Scholar]
- 13.Hastings D. Value-based payment, accountable care, and the ACO final rule: are we making progress? Health Affairs Blog [blog on the Internet] 2011 Oct 22; [cited 2011 Dec 9]. Available from: http://healthaffairs.org/blog/2011/10/22/value-based-payment-accountable-care-and-the-aco-final-rule-are-we-making-progress/
- 14.Casalino L, Shortell S. The ACO race is on: navigating the terrain. Health Affairs Blog [blog on the Internet] 2011 Oct 24; [cited 2011 Dec 9]. Available from: http://healthaffairs.org/blog/2011/10/24/the-aco-race-is-on-navigating-the-terrain/
- 15.McClellan M, Fisher E. The ACO final rule: progress toward better care at lower cost. Health Affairs Blog [blog on the Internet] 2011 Oct 21; [cited 2011 Dec 9]. Available from: http://healthaffairs.org/blog/2011/10/21/the-aco-final-rule-progress-toward-better-care-at-lower-cost/
- 16.Berenson RA. Shared Savings Program for accountable care organizations: a bridge to nowhere? Am J Manag Care. 2010;16(10):721–6. [PubMed] [Google Scholar]
- 17.Fisher ES, Staiger DO, Bynum JPW, Gottlieb DJ. Creating accountable care organizations: the extended hospital medical staff. Health Aff (Millwood) 2007;26(1):w44–57. doi: 10.1377/hlthaff.26.1.w44. DOI: 10.1377/hlthaff.26.1.w44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bynum JPW, Bernal-Delgado E, Gottlieb DJ, Fisher ES. Assigning ambulatory patients and their physicians to hospitals: a method for obtaining population-based provider performance measurements. Health Serv Res. 2007;42(1):45–62. doi: 10.1111/j.1475-6773.2006.00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


