Abstract
Background
Physical activity (PA) has previously been suggested to attenuate the risk of atrial fibrillation (AF) conferred by excess body weight and weight gain. We prospectively examined the relationship between body size, weight change and level of PA in a biracial cohort of middle-aged men and women.
Methods and Results
Baseline characteristics on risk factor levels were obtained on 14,219 participants from the Atherosclerosis Risk in Communities Study. AF incidence was ascertained from 1987–2009. Adjusted Cox proportional hazards models were utilized to estimate the associations between body mass index (BMI), waist circumference (WC), relative weight change, and PA level with incident AF. During follow-up, there were 1775 cases of incident AF. BMI and WC were positively associated with AF, as was weight loss/gain of >5% initial body weight. An ideal level of PA had a small protective effect on AF risk and partially attenuated the risk of AF associated with excess weight in men but not women: compared with men with a normal BMI, the risk of AF in obese men with an ideal, intermediate and poor level of PA at baseline was increased by 37%, 129% and 156% (Pinteraction=0.04). During follow-up, PA did not modify the association between weight gain and risk of AF.
Conclusions
Obesity and extreme weight change are risk factors for incident AF whereas being physically active is associated with a small reduction in risk. In men only, being physically active offset some, but not all, of the risk incurred with excess body weight.
Keywords: atrial fibrillation, obesity, physical activity
Introduction
Atrial fibrillation (AF) is one of the most commonly diagnosed cardiac arrhythmias in clinical practice, affecting 2.3 million people in the United States (US) alone1. AF is responsible for one-third of all hospitalizations for cardiac rhythm disturbances and consequently is associated with significant health care costs that in the US alone exceed $6 billion annually2.
Excess body weight is an established risk factor for cardiovascular diseases (CVD) including AF3. But, for physical activity, which also has cardioprotective properties, the shape of the relationship with incident AF appears to be more variable and largely dependent upon the age and fitness level of the population under investigation4,5. Moreover, a recent study reported that physical fitness could ameliorate the adverse effect of excess body weight and weight gain on AF risk in men6. These findings have yet to be replicated, and it is unknown whether the observed relationship is generalizable to women. Given that population-based interventions that increase and maintain physical activity levels may be more successful than those aimed at long-term weight loss7, the possibility that physical activity may obviate the increased risk of AF associated with weight gain and obesity warrants further investigation. We therefore examined the interplay between body size, weight change and physical activity on risk of AF in a large biracial cohort of men and women.
Methods
The Atherosclerosis Risk in Communities (ARIC) Study is a prospective cohort study of atherosclerotic diseases within four communities in the United States: Forsyth County, North Carolina; Jackson, Mississippi; Washington County, Maryland; and the northwest suburbs of Minneapolis, Minnesota. The recruitment of study participants is described in detail elsewhere8. Briefly, the cohort comprised at baseline in 1987–89, 15,792 men and women aged 45–64 years who were selected by list of area probability sampling. The baseline home interview and clinic examination measured various risk factors and cardiovascular conditions. Three triennial study visits occurred subsequently in with the last visit in 1996–98. Additionally, participants or their proxy were contacted annually by telephone to ascertain hospitalizations and death. In addition, active surveillance of the ARIC community hospitals was conducted. The ARIC Study protocol was approved by the institutional review board of each participating university, and informed consent was obtained from each study participant.
Body mass index (BMI: kg/m2) was calculated from measurements of weight to the nearest pound (which was subsequently converted into kilograms) and height to the nearest centimeter, with the participants wearing a scrub suit and no shoes. Participants were classified as normal weight (18.5 – 24.9 kg/m2), overweight (25 – 29.9 kg/m2), and obese (≥30 kg/m2). Underweight individuals (BMI < 18.5 kg/m2) were excluded from the analysis (n = 138). Waist circumference was measured at the umbilical level. As there are no set criteria to define increasing severity of central obesity in men and women, we categorized individuals by sex-specific quartiles of waist circumference. The inter-technician reliability coefficient for waist circumference was r > 0.949. The percent weight change through Visit 4 was calculated using the weight at Visit 1 as the denominator.
PA was measured using the modified Baecke questionnaire which defines 3 semi-continuous indices ranging from 1 (low) to 5 (high) for physical activity in sports, during leisure time, and at work10,11. The questions were converted to “minutes per week” of moderate or vigorous exercise based on metabolic equivalents (MET) values, using an updated version of the Compendium of Physical Activities as a guide, and incorporating number of months annually a participant partook in the activity12. We used the American Heart Association’s definition for “poor” (no moderate or vigorous), “intermediate” (1–149min/week moderate or 1–74min/week vigorous) or “ideal” (1–149min/week moderate + vigorous)13.
Methods used for ascertainment of blood pressure (BP), hypertension, education and income have been reported elsewhere14. Smoking status was obtained from the interview. Prevalent coronary heart disease (CHD) included individuals with a history of myocardial infarction (MI), MI adjudicated from the baseline electrocardiogram (ECG), or history of coronary bypass, heart failure (HF) or angioplasty.
Individuals with evidence of AF or atrial flutter on an ECG at study baseline were excluded from this analysis. Diagnoses of incident AF and atrial flutter were obtained through the end of 2009 from three sources: ECGs done at study visits (visits 2–4), presence of an International Classification of Disease (ICD9) code for AF (427.31 or 427.32) in a hospital discharge, or AF listed as any cause of death on a death certificate. Hospitalizations with AF associated with open cardiac surgery were not considered events. Date of AF incidence was the earliest of any AF diagnosis. All ARIC examination ECGs were recorded using MAC PC Personal Cardiographs (Marquette Electronics, Inc., Milwaukee, WI). A standard supine 12-lead resting ECG was recorded at each clinic visit and was transmitted by modem to the ARIC ECG Reading Center for automatic reading and coding. All AF cases that were automatically detected from the study ECGs were visually rechecked by a cardiologist. Prior analysis within the ARIC cohort to determine the validity of hospital discharge diagnoses for AF reported 84% sensitivity and 98% specificity in the ascertainment of AF events15.
Means and standard deviations (SD) for the baseline continuous variables and percentages for the categorical variables were calculated separately in men and women. Cox proportional hazards models with time to AF as the dependent variable were utilized to estimate the associations between BMI, waist circumference, relative weight change, and physical activity level with AF. Follow-up time was defined as the time between the baseline visit and the date of AF incidence, death, loss to follow-up, or December 31, 2009. For the analysis of weight change, the analysis was restricted to those participants who had weight information at visits 1 and 4 and were free of AF at visit 4 (n=10,239, 1026 AF cases). This analysis was adjusted for visit 1 covariates (education, income and level of PA) and visit 4 covariates (prevalent cardiovascular disease, alcohol consumption, age, smoking status and height). Restricted cubic splines adjusted for age, race, and sex were used to explore the shape of the association of BMI, waist circumference, relative weight change, and physical activity level with risk of incident AF.
Where there was a significant sex interaction (p-values < 0.05), separate analyses for men and women were conducted and the results shown separately by sex; models were adjusted for age, race, study site, education, income, prevalent CVD, cigarette smoking, height, physical activity level (where appropriate), and alcohol consumption. Continuous exposures were analyzed categorically (using where possible established clinical cut-points) given that these associations have more relevance in clinical practice than measures of the continuous associations. Chi-square tests for trend were conducted across categorical levels of BMI, waist circumference, and physical activity level. There was no significant interaction between race, body size and PA level. We explored the assumption of proportional hazards by computation of Schoenfeld residuals, inspection of log(−log[survival function]) curves, and an interaction term between each exposure variable and follow-up time; the proportional hazards assumption was found to be satisfied in all instances.
Additional sensitivity analyses were performed to examine the associations between waist circumference and BMI with AF in more detail. Sex-specific tertiles of the MET-minutes score were generated, and separate analyses by sex and MET-minutes tertile for both BMI and waist circumference as categories with AF risk were examined. To further examine the effect of possible mediators such as SBP, DBP, antihypertensive medication, diabetes, and incident CVD on the BMI-AF association, an additional model adjusting for these mediators as time-varying covariates based on measurements at other ARIC study exam visits was performed. All statistical analyses were performed using SAS v 9.2 (SAS Inc., Cary, NC).
Results
Overall, 14,219 study participants contributed to this analysis following exclusion of 1573 individuals for reasons specified in Web-figure 1. The response rates between visits were 93% (visit 1–2), 86% (visit 2–3) and 81% (visit 3–4). Only 455 participants (3%) were lost to follow-up before developing AF, death, or administrative censoring. At study baseline, the mean age of the study participants was 54.2 years (SD 5.7). Overall, 39.9% of the study population was overweight and 27.4% were obese; the mean values for height, weight, BMI and waist circumference at baseline are shown in Table 1. Baseline level of physical activity varied by sex: 34% of men and 40% of women had a poor level of physical activity (Table 1). Within the intermediate and ideal categories of physical activity, men tended to have slightly higher MET-minute values within each of the four weight categories than women (Web-table 1). The most common forms of physical activity were walking and gardening (Web-table 2).
Table 1.
Baseline characteristics of study participants in the Atherosclerosis Risk in Communities (ARIC) Study, 1987–2009. Values correspond to means (SD) or % unless otherwise stated.
| Variable | Men (n=6445) |
Women (n=7774) |
|---|---|---|
| Age, years | 54.6 (5.8) | 53.8 (5.7) |
| Body height, cm | 176.1 (6.6) | 162.3 (6.0) |
| Body weight, kg | 85.2 (14.2) | 73.6 (16.6) |
| Body mass index, kg/m2 | 27.5 (4.2) | 28.0 (6.0) |
| Waist circumference, cm | 99.2 (10.9) | 95.6 (15.6) |
| Median physical activity MET-minutes (IQR) | 110.4 (248.4) | 63.0 (193.2) |
| African American | 20.8 | 28.7 |
| < High school graduate | 23.3 | 23.1 |
| < $35,000 per year income | 48.3 | 61.6 |
| Current drinker | 65.2 | 49.1 |
| Current smoker | 27.1 | 24.6 |
| Prior cardiovascular disease | 10.0 | 7.3 |
| Physical activity level | ||
| Poor | 34.4 | 40.0 |
| Intermediate | 22.0 | 26.5 |
| Ideal | 43.6 | 33.5 |
| Weight change through visit 4* | ||
| >5% loss | 12.1 | 12.2 |
| 0–5% loss | 19.2 | 15.5 |
| 0–4.9% gain | 33.6 | 25.5 |
| 5–9.9% gain | 21.3 | 21.3 |
| >10% gain | 13.8 | 25.5 |
Reduced sample size: men, n=4500 and women, n=5739.
SD=standard deviation; MET-minutes = metabolic equivalent; IQR =interquartile range
During follow-up there were 1775 cases of incident AF during 258,409 person-years (incidence rate: 6.9 events per 1,000 person-years): 98.7% were identified from hospitalizations, 6.5% from study ECGs, and 6.0% from death certificates (some cases were identified by more than one method).
Above BMI’s of 18.5 kg/m2, there was a positive linear association between BMI and risk of AF (Web-Figures 2, 3) that did not differ by sex (Psex-interaction = 0.34) or by race (Prace-interaction = 0.81). Compared to individuals of normal weight, the risk of AF was nearly doubled in those who were obese after adjustment for possible confounders (Table 2). Similarly, there was a positive linear association between sex-specific quartiles of waist circumference with incident AF (Web-Figures 4, 5) with no evidence of a sex-difference in the magnitude of the association (Psex-interaction = 0.76; Table 2) or of a race difference (Prace-interaction = 0.27). Compared with those in the lowest quartile, those in the highest quartile for waist circumference had 113% increased risk of AF after consideration of possible confounders.
Table 2.
Adjusted* hazard ratios (95% confidence intervals) for the association between categories of overweight and obesity with risk of incident atrial fibrillation (AF) in men and women in the Atherosclerosis Risk in Communities Study (ARIC), 1987 – 2009
| Body mass index (kg/m2) | |||||
| 18.5–24.9 (Ref) | 25–29.9 (Overweight) | ≥30 (Obese) | Ptrend** | ||
| n | 4650 | 5667 | 3902 | ||
| AF cases | 444 | 690 | 641 | ||
| HR (95% CI) | 1.00 | 1.20 (1.06–1.36) | 1.95 (1.72–2.21) | <0.0001 | |
| Waist circumference (quartiles) | |||||
| 1st (Ref) | 2nd | 3rd | 4th | Ptrend** | |
| n | 3696 | 3665 | 3441 | 3417 | |
| AF cases | 293 | 375 | 476 | 631 | |
| HR (95% CI) | 1.00 | 1.18 (1.01–1.37) | 1.52 (1.31–1.76) | 2.13 (1.85–2.46) | <0.0001 |
Adjusted for age, sex, race, study site, education, income, prior cardiovascular disease, cigarette smoking, height, physical activity and alcohol consumption.
Linear trend by body mass index group or waist circumference quartiles as an ordinal variable. Non-significant sex interaction between BMI categories and risk of atrial fibrillation (p = 0.34) and between waist circumference and risk of atrial fibrillation (p = 0.76). Sex specific quartiles for WC in men (women) were ≤ 92 (≤ 84) cm, 93 –98 (85 – 94) cm, 99 – 105 (95 – 105) and ≥ 106 (≥106) cm.
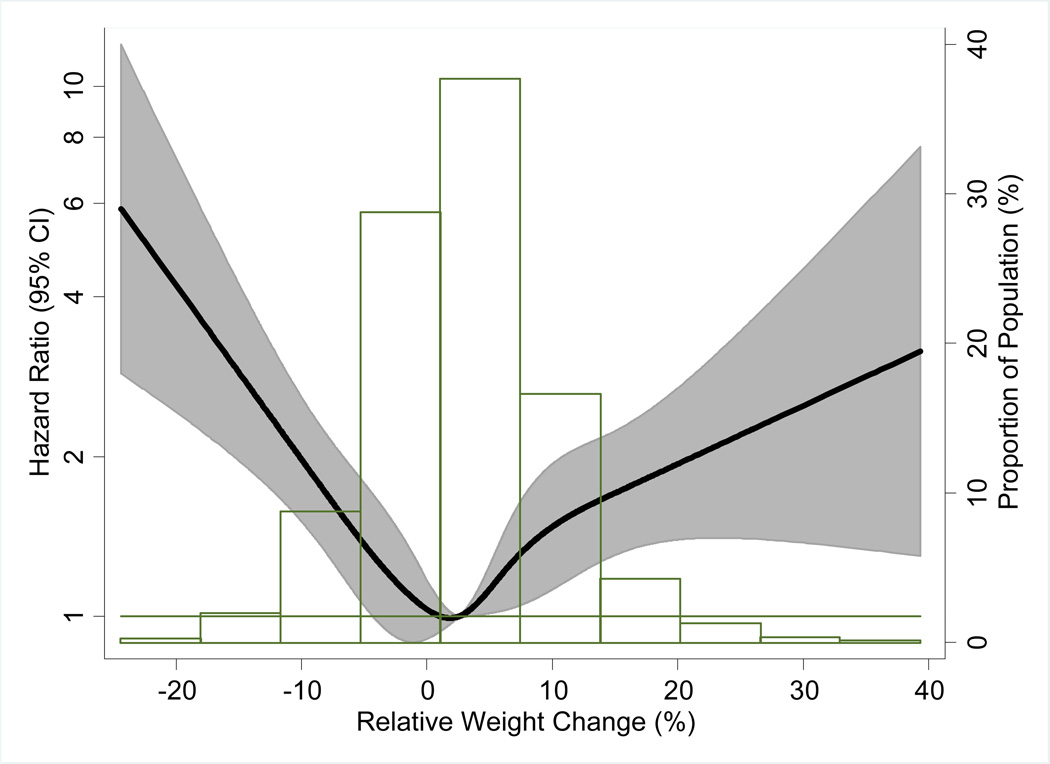
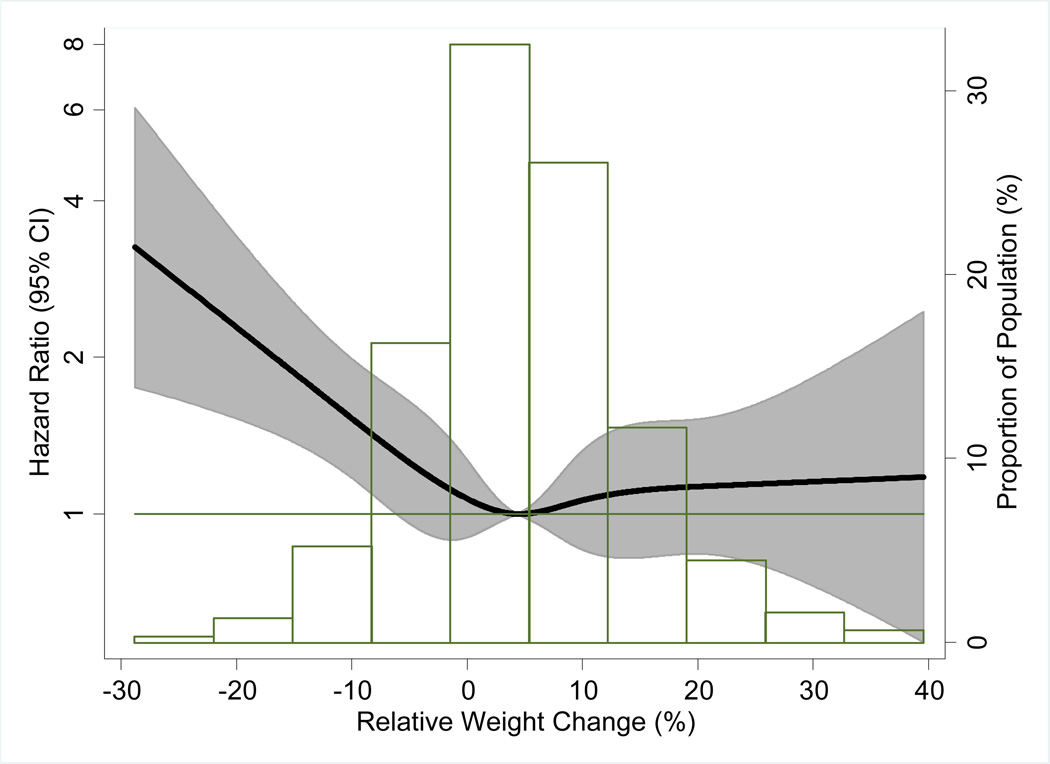
Between visits 1–4, the mean percent weight change was 4.0%. The relationship between relative weight change and subsequent risk of AF differed between men and women (Psex-interaction = 0.01; Web-table 3; Figures 1, 2). In adjusted analyses, compared with those who gained less than 5% body weight during follow up, men who gained more than 10% body weight had a 61% (95% CI: 24% to 111%) increased risk of AF whereas there was a non-significant 19% increase in risk of AF in women (95% CI: −10% to 55%). For those who lost more than 5% of body weight during follow up, the risk of AF was 52% higher in men and 45% in women (Web-table 3) compared with those who gained less than 5%.
Figure 1.
Association of relative weight change with incidence of atrial fibrillation in men presented as hazard ratio (solid line) and 95% confidence intervals (shaded area). Results from Cox proportional hazards model using restricted cubic splines, adjusted for age and race. Median value of relative weight change was considered the reference (HR=1). The histograms represent the frequency distribution of the relative weight change in the study sample.
Figure 2.
Association of relative weight change with incidence of atrial fibrillation in women. Conventions as in Figure 1.
There was a weak protective association of physical activity with risk of AF that was of a similar magnitude for both men and women (Psex-interaction = 0.29; Web-Figures 6,7). Compared with a poor level of physical activity, those who reported having an ideal level of physical activity at baseline had 11% (95% CI: 0% to 21%) lower risk of AF after adjusting for relevant confounders (Ptrend = 0.04). The association remained materially unchanged when using sex-specific tertiles of physical activity (Web-Table 4).
The association between BMI with risk of incident AF differed by level of physical activity in men (Pinteraction = 0.04; Table 3) but not in women (Pinteraction = 0.98). In obese men, the risk of AF was significantly attenuated with increasing level of physical activity physical activity after adjustment for confounders. These estimates remained largely unchanged when using sex-specific tertiles of MET-score (Web-table 5). Much of the effect of an increase in BMI on AF risk was mediated through increases in blood pressure, diabetes and prior heart disease as further adjustment for these covariates substantially attenuated the risk of AF (Table 3). However, even after adjustment for these explanatory variables, obese men with a poor level of physical activity at baseline still had significantly increased risk of AF compared with lean men with a similar level of physical activity.
Table 3.
Hazard ratios (95% confidence intervals) adjusted for confounders and by potential mediators for the impact of level of physical activity on the association between overweight and obesity with risk of incident atrial fibrillation (AF) in men in the Atherosclerosis Risk in Communities Study (ARIC), 1987 – 2009
| Body mass index (kg/m2) | ||||
|---|---|---|---|---|
| N (AF cases) |
25–29.9 (Overweight) |
≥30 (Obesity) |
Pinteraction | |
| Model 1 (adjusted for confounders)* | ||||
| Poor | 2218 (342) | 1.45 (1.07–1.97) | 2.56 (1.86–3.50) | |
| Intermediate | 1420 (210) | 1.39 (0.96–2.00) | 2.29 (1.54–3.40) | |
| Ideal | 2807 (435) | 1.14 (0.91–1.43) | 1.37 (1.04–1.81) | 0.04 |
| Model 2 (adjusted for confounders and potential mediators)** | ||||
| Poor | 2218 (342) | 1.23 (0.90–1.67) | 1.59 (1.14–2.22) | |
| Intermediate | 1420 (210) | 1.12 (0.77–1.63) | 1.61 (1.05–2.46) | |
| Ideal | 2807 (435) | 1.03 (0.81–1.29) | 1.00 (0.75–1.34) | 0.05 |
Reference group = body mass index 18.5 – 24.9 kg/m2.
Adjusted for age, race, study site, education, income, prior cardiovascular disease, cigarette smoking, height, and alcohol consumption.
Adjusted for age, race, study site, education, income, prior cardiovascular disease, cigarette smoking, height, alcohol consumption, and as time-varying covariates: systolic blood pressure, diastolic blood pressure, antihypertensive medications, diabetes, incident heart failure, and incident myocardial infarction. P for interaction = interaction between physical activity and BMI on risk of AF.
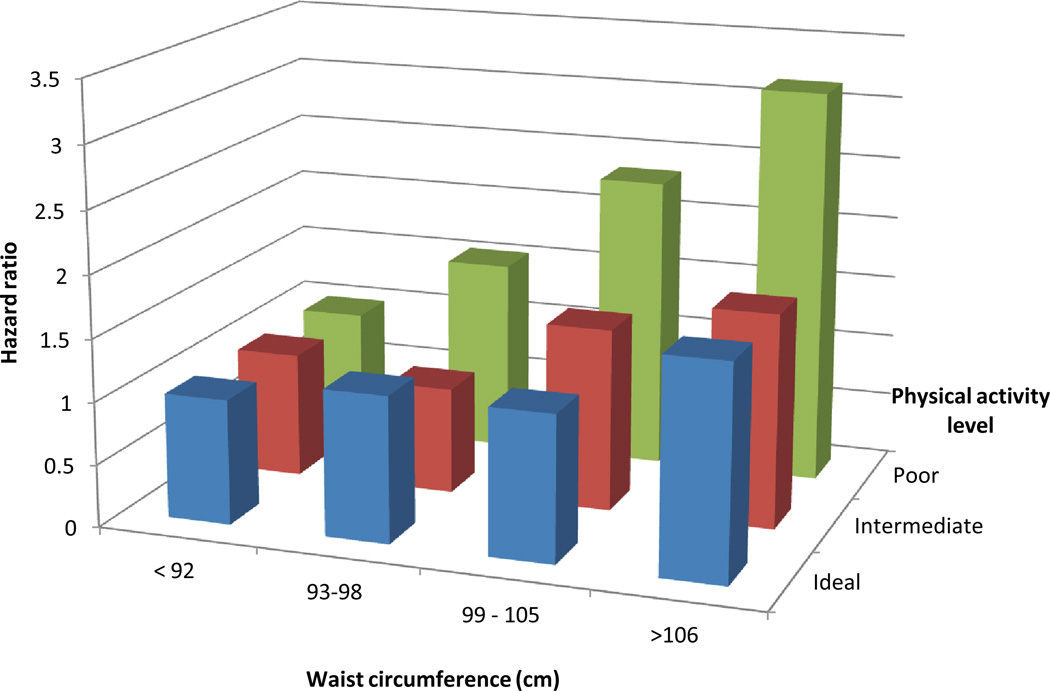
Similarly, there was some evidence of an attenuation of the impact of central obesity on risk of AF by physical activity level in men (Pinteraction = 0.08) but not in women (Pinteraction = 0.92) (Figure 3). These estimates remained unaltered when derived using sex-specific tertiles of MET-score (Web-table 6). Finally, there was no evidence of an interaction between level of physical activity with weight change in men (Pinteraction = 0.71) or women (Pinteraction = 0.96) (Web-Table 7).
Figure 3.
Hazard ratios for the impact of physical activity level on the association between waist circumference and risk of incident atrial fibrillation(AF) in men after adjustment for confounders. P for interaction between physical activity level and waist circumference on risk of AF = 0.08.
Discussion
Physical activity has previously been suggested to mitigate some of the cardiovascular hazards associated with excess body weight16, 17, but whether this may also be true for AF, which is the most frequently sustained cardiac arrhythmia, is unknown. In this middle-aged biracial cohort of men and women, excess body weight and weight change in excess of 5% were associated with increased risk of AF. Conversely, achieving an ideal level of physical activity at study baseline conferred a modicum of protection against future AF risk. But the most pertinent finding was that in men, but interestingly not women, an ideal level of physical activity partly attenuated the risk of AF associated with excess body weight.
The nature of the relationship between physical activity and risk of AF remains somewhat contentious, but it appears to be related to both the intensity of physical exertion as well as the subtype of AF event incurred. Previous reports suggest that endurance athletes and those who participate in high intensity exercise are at substantially increased risk of paroxysmal or ‘lone’ AF5. In contrast, a meta-analysis of four population-based cohort studies –that combined had fewer AF events than the current study- regular exercise was not significantly associated with risk of AF (the pooled Odds Ratio of AF comparing the most physically active versus the least physically active groups was 1.08 [95% CI: 0.97 to 1.21; P = 0.1]18). Findings from the current study suggest that physical activity is associated with a small reduction in AF risk but more prospective data that can distinguish between subtypes of AF are required before any definitive conclusions can be reached.
That excess body weight is a risk factor for incident AF concurs with a meta-analysis of 16 studies that reported 50% greater risk of AF in obese compared with non-obese individuals with similar effects in men and women3. In contrast, the effect of weight change on risk of AF was significantly stronger among men than in women: those men who gained more than 10% body weight compared with less than 5% weight gain had a 61% greater risk of AF compared with 19% in women. Of interest was the marked increase in incident AF among individuals who lost more than 5% of their initial body weight during follow up. This rather paradoxical finding may be explained by the different physiological mechanisms that distinguish intentional from non-intentional weight loss. Whereas intentional weight loss tends to be associated with favorable cardiovascular outcomes19, unintentional weight loss (due to conditions associated with sarcopenia or some underlying disease) has been associated with higher mortality20. Although we had no information on the reasons for weight loss in ARIC we suggest that conditions associated with muscle-wasting may account for the increased risk of AF associated with weight loss that we observed in the present study.
The attenuation in the positive association between body size and risk of AF by physical activity level was marked and only apparent in men: obese men who were reported as having an ideal level of physical activity at baseline had 37% increased risk of AF compared with 156% in those with a poor level of physical activity. Interestingly, the increased risk of AF associated with being both obese and having a poor level of physical activity was not entirely explained by physiological mediators such as blood pressure, diabetes and prior cardiovascular disease. This sex-difference remained true even when using sex-specific tertiles of physical activity scores. An effect modification by physical activity has been previously been suggested in a small cohort of European men6. In that study, physically fit men had a reduced risk of incident AF that was similar across subgroups of BMI whilst in unfit men, the risk of AF increased with greater levels of obesity. But aside from this one study, no other study has reported on the possible interaction between body size, physical activity and risk of AF in either men or women. Our findings concur with what we currently understand about the modifying effect of physical activity on the relationship between BMI and other health outcomes. Although the sex difference that we observed may be plausible given earlier reports, it may also be a chance finding.
There are several significant limitations of this current study that warrant mention. First, we had no measure of aerobic fitness, which may be a better indicator of physical fitness than physical activity level, or an objective measure of physical activity. Neither did we have information on whether weight loss in this study population was intentional or non-intentional which have opposing relationships with cardiovascular and all-cause mortality. We also had no information regarding AF subtypes, and therefore we could not examine whether there were differences in the relationship between body weight, physical activity and AF subtype. Finally, cases of AF were mainly ascertained through hospital discharge codes, this may have led to under-ascertainment of asymptomatic events and those that, perhaps, were not severe enough to warrant hospitalization.
In summary, AF is amenable to lifestyle intervention: maintaining a healthy body weight, avoidance of weight gain, and being physically active constitute a coherent public health message for reducing the growing burden of AF. That physical activity may confer some degree of protection against future risk of AF in men is worthy of future investigation.
Supplementary Material
Acknowledgments
The authors thank the staff and participants of the ARIC study for their important contributions.
Funding Sources: The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C). This study was additionally funded by grant RC1 HL099452 from NHLBI and grant 09SDG2280087 from the American Heart Association.
Footnotes
Conflict of Interest Disclosures: None.
References
- 1.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: National implications for rhythm management and stroke prevention: The AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 2.Coyne KS, Paramore C, Grandy S, Mercader M, Reynolds MR, Zimetbaum P. Assessing the direct costs of treating nonvalvular atrial fibrillation in the United States. Value Health. 2006;9:348–356. doi: 10.1111/j.1524-4733.2006.00124.x. [DOI] [PubMed] [Google Scholar]
- 3.Wanahita N, Messerli FH, Bangalore S, Gami AS, Somers VK, Steinberg JS. Atrial fibrillation and obesity: results of a meta-analysis. Am Heart J. 2008;155:310–315. doi: 10.1016/j.ahj.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Williams PT, Franklin BA. Reduced incidence of cardiac arrhythmias in walkers and runners. PLoS One. 2013;8:e65302. doi: 10.1371/journal.pone.0065302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thelle DS, Selmer R, Gjesdal K, Sakshaug S, Jugessur A, Graff-Iversen S, Tverdal A. Nystad W Resting heart rate and physical activity as risk factors for lone atrial fibrillation: a prospective study of 309 540 men and women. Heart. 2013;99:1755–1760. doi: 10.1136/heartjnl-2013-303825. [DOI] [PubMed] [Google Scholar]
- 6.Grundvold I, Skretteberg PT, Liestøl K, Gjesdal K, Erikssen G, Kjeldsen SE, Arnesen H, Erikssen J, Bodegard J. Importance of physical fitness on predictive effect of body mass index and weight gain on incident atrial fibrillation in healthy middle-age men. Am J Cardiol. 2012;110:425–432. doi: 10.1016/j.amjcard.2012.03.043. [DOI] [PubMed] [Google Scholar]
- 7.Fjeldsoe B, Neuhaus M, Winkler E, Eakin E. Systematic review of maintenance of behavior change following physical activity and dietary interventions. Health Psychol. 2011;30:99–109. doi: 10.1037/a0021974. [DOI] [PubMed] [Google Scholar]
- 8.The ARIC Investigators. The Atherosclerosis Risk in Communities (ARIC) Study: Design and objectives. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 9.Ferrario M, Carpenter MA, Chambless LE. Reliability of body fat distribution measurements. The ARIC Study baseline cohort results. Atherosclerosis Risk in Communities Study. Int J Obes Relat Metab Disord. 1995;19:449–457. [PubMed] [Google Scholar]
- 10.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Amer J Clin Nutr. 1982;36:936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 11.Folsom AR, Arnett DK, Hutchinson RG, Liao F, Clegg LX, Cooper LS. Physical activity and incidence of coronary heart disease in middle-aged women and men. Med Sci Sports Exerc. 1997;29:901–909. doi: 10.1097/00005768-199707000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swart AM, Strath SJ, O’Brien WL, Bassett DR, Jr, Schmitz KH, Emplaincourt PO, Jacobs DR, Jr, Leon AS. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sport Exer. 2000;32:S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 13.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atherosclerosis Risk In Communities (ARIC) manuals, forms and data collection. [Accessed September 2013]; http://www.cscc.unc.edu/aric/displaydatatree.php. [Google Scholar]
- 15.Alonso A, Agarwal SK, Soliman EZ, Ambrose M, Chamberlain AM, Prineas RJ, Folsom AR. Incidence of atrial fibrillation in whites and African-Americans: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2009;158:111–117. doi: 10.1016/j.ahj.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Church TS, LaMonte MJ, Barlow CE, Blair SN. Cardiorespiratory fitness and body mass index as predictors of cardiovascular disease mortality among men with diabetes. Arch Intern Med. 2005;165:2114–2120. doi: 10.1001/archinte.165.18.2114. [DOI] [PubMed] [Google Scholar]
- 17.Stevens J, Cai J, Evenson KR, Thomas R. Fitness and fatness as predictors of mortality from all causes and from cardiovascular disease in men and women in the Lipid Research Clinics Study. Am J Epidemiol. 2002;156:832–841. doi: 10.1093/aje/kwf114. [DOI] [PubMed] [Google Scholar]
- 18.Ofman P, Khawaja O, Rahilly-Tierney CR, Peralta A, Hoffmeister P, Reynolds MR, Gaziano JM, Djousse L. Regular physical activity and risk of atrial fibrillation: a systematic review and meta-analysis. Circ Arrhythm Electrophysiol. 2013;6:252–256. doi: 10.1161/CIRCEP.113.000147. [DOI] [PubMed] [Google Scholar]
- 19.Eilat-Adar S, Eldar M, Goldbourt U. Association of intentional coronary heart disease event rates in overweight subjects who have an additional coronary risk factor. Am J Epidemiol. 2005;161:352–358. doi: 10.1093/aje/kwi045. [DOI] [PubMed] [Google Scholar]
- 20.Myers J, Lata K, Chowdhury S, McAuley P, Jain N, Froelicher V. The obesity paradox and weight loss. Am J Med. 2011;124:924–930. doi: 10.1016/j.amjmed.2011.04.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.