Abstract
Introduction. An outpatient transoral endoscopic procedure for gastroesophageal reflux disease (GERD) and obesity would be appealing if safe, effective, and durable. We present the first in human experience with a new system. Methods. Eight patients with GERD (3) and obesity (5) were selected according to a preapproved study protocol. All GERD patients had preprocedure manometry and pH monitoring to document GERD as well as quality of life and symptom questionnaires. Obese patients (body mass index >35) underwent a psychological evaluation and tests for comorbidities. Under general anesthesia, a procedure was performed at the gastroesophageal junction including mucosal excision, suturing of the excision beds for apposition, and suture knotting. Results. One patient with micrognathia could not undergo the required preprocedural passage of a 60 F dilator and was excluded. The first 2 GERD patients had incomplete procedures due to instrument malfunction. The subsequent 5 subjects had a successfully completed procedure. Four patients were treated for obesity and had an average excess weight loss of 30.3% at 2-year follow-up. Of these patients, one had an 8-mm outlet at the end of the procedure recognized on video review—a correctable error—and another vomited multiple times postoperatively and loosened the gastroplasty sutures. The treated GERD patient had resolution of reflux-related symptoms and is off all antisecretory medications at 2-year follow-up. Her DeMeester score was 8.9 at 24 months. Conclusion. The initial human clinical experience showed promising results for effective and safe GERD and obesity therapy.
Keywords: esophageal surgery, flexible endoscopy, gastric surgery, NOTES, interventional endoscopy
Introduction
GERD
Gastroesophageal reflux disease (GERD) affects an estimated 19 million people in the United States, which results in a direct cost of $9.3 billion for treatments per year.1 (1) The management of GERD has gained increasing attention during the past 2 decades due to a high prevalence in Western societies, a better understanding of the pathophysiology, new potent antisecretory drug therapies, the advent of minimally invasive surgery, and new transoral endoscopic procedures. Patients with early disease normally experience episodes of esophageal acid exposure shortly after meals.
An outpatient endoscopic procedure that would alter the gastroesophageal junction (GEJ) barrier to prevent acid reflux would be appealing to patients and physicians alike. In this study, an endoluminal gastroplication procedure was studied, with the intent to demonstrate safety, symptom relief, increased lower esophageal sphincter pressure, and normalization of pH monitoring results.
Obesity
Approximately two thirds of individuals living in the United States are overweight, and of those, almost half are obese.2 Obesity is associated with increases in the prevalence of type 2 diabetes, hyperlipidemia, hypertension, obstructive sleep apnea, heart disease, stroke, asthma, back and lower extremity weight-bearing degenerative joint problems, several forms of cancer, and depression. For example, obese men have a 5.5 times greater risk of becoming diabetic.3 In comparison with a normal-weight individual, a 25-year-old morbidly obese man has a 22% reduction in lifespan, representing a loss of 12 years of life.4
However, as with all operative procedures, bariatric surgery is associated with morbidity and mortality. Operative mortality (30 days) is approximately 0.1% for restrictive procedures, 0.5% for gastric bypass, and 1.1% for biliopancreatic diversion or duodenal switch.5 In addition, increasing cost, postoperative pain, hospital stay, and other morbidities associated with surgery make this a difficult choice. Hence, effective endosurgical therapy for the treatment of obesity would be both cost-effective and highly beneficial.
Excision of mucosa followed by apposition of the excision beds will result in a durable plication. In an abstract this was demonstrated, and it is evident from open and laparoscopic surgery that raw or open gastric edges do fuse with suture reinforcement, as in anastomoses. We have demonstrated in canines that sufficient and durable fibrosis is placed to alter GEJ compliance and to create a durable 6 mm in diameter outlet along the lesser curvature.6 The gastroplasty line must also remain intact as any opening will increase and remove the restrictive nature of the procedure. In addition, a distal 1 cm opening must be secure to provide a relative obstruction to the rapid intake of food. We have demonstrated in the animal laboratory that this is possible.7 The purpose of this pilot project was to demonstrate feasibility and safety of the procedure and if possible preliminary effectiveness.
Methods
After hospital ethics committee and National Regulatory Agency protocol approval, patients were screened for study eligibility, and then GERD patients were administered a symptom scoring questionnaire, the GERD-HRQL (health-related quality of life). They underwent upper endoscopy to rule out a hiatal hernia larger than 2 cm and other contraindicating pathology before manometry and pH monitoring testing. The DeMeester score was determined and patients with a normal score or a score more than 50 were excluded. The schedule of tests is shown in Table 1.
Table 1.
Schedule of Tests.
| Form Name | Baseline | Procedure | Day 1 Postop Phone Call | 2 Weeks ± 4 Days | 1 Month ± 1 Week | 3 Months ± 2 Weeks | 6 Months ± 1 Month | 12 Months ± 1 Month | 24 Months ± 1 Month |
|---|---|---|---|---|---|---|---|---|---|
| GERD symptoms | X | X | X | X | X | X | |||
| GERD medications | X | X | X | X | X | X | |||
| Quality of life (GERD-HRQL) | X | X | X | X | X | X | |||
| Esophageal assessment | |||||||||
| Endoscopy | X | X | X | X | |||||
| Manometry | X | X | X | X | |||||
| pH monitoring | X | X | X | X | |||||
| Procedure | X | ||||||||
| Adverse event | X | ||||||||
| Postprocedure adverse events | X | X | X | X | X | X | X | ||
Abbreviations: GERD, gastroesophageal reflux disease; HRQL, health-related quality of life.
For obesity patients, the following tests were performed: Impact of Weight on Quality of Life Questionnaire (IWQOL), a symptom questionnaire, medication usage, a psychological evaluation, body weight and height, a Helicobacter pylori test, a UGI series, assessment of comorbidities including an A1c level, blood pressure, a sleep apnea questionnaire, and serum lipids. This was followed by upper endoscopy. Table 2 shows the scheduled tests.
Table 2.
Schedule of Tests.
| Form Name | Baseline | Procedure | 2 Weeks | 1 Month | 3 Months | 6 Months | 12 Months | 24 Months |
|---|---|---|---|---|---|---|---|---|
| H&P | X | |||||||
| Medications | X | X | X | X | X | X | X | |
| UGI symptoms | X | X | X | X | X | X | X | |
| Body weight | X | X | X | X | X | X | X | |
| Stool guiac | X | |||||||
| UGI series | X | X | X | |||||
| Assessment of comorbidities | ||||||||
| Blood pressure | X | X | X | X | X | X | X | X |
| Fasting blood glucose | X | X | X | X | X | X | X | |
| Hb A1C | X | X | X | X | X | X | X | |
| Helicobacter pylori breath test | X | |||||||
| Lipid profile | X | X | X | X | X | |||
| IWQOL questionnaire | X | X | X | X | X | X | ||
| Procedure | X | |||||||
| Endoscopy | X | X | X | X | ||||
| Adverse events | X | |||||||
| Postprocedure adverse events | X | X | X | X | X | X | ||
| Standard psychological evaluation | X | |||||||
Abbreviation: IWQOL, Impact of Weight on Quality of Life Questionnaire.
Safety was evaluated by monitoring the incidence of adverse events. The following is a list of possible adverse events: esophageal perforation, gastrointestinal bleeding requiring transfusion, gastric perforation, aspiration, cardiac events, pneumothorax, or bacteremia.
Operative Technique
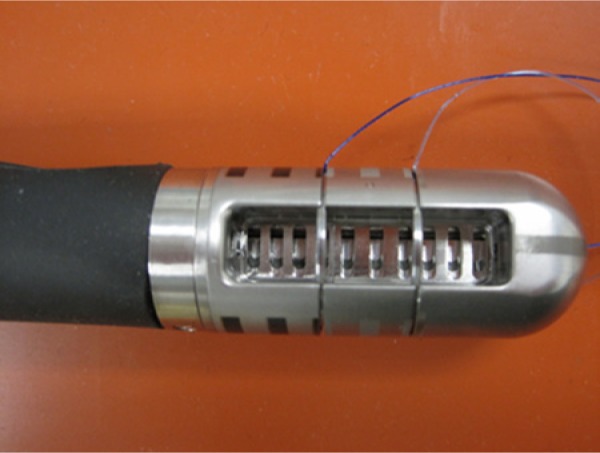
Initially, the patients were placed in the supine position after intubation and initiation of general anesthesia. Upper endoscopy was performed followed by Savary guidewire esophageal dilation with a 60 F Savary dilator. Instrument insertion of the excision device (Figure 1) was difficult but possible in the first patient; however, the device and other malfunctions occurred.
Figure 1.

The excision device with the blade.
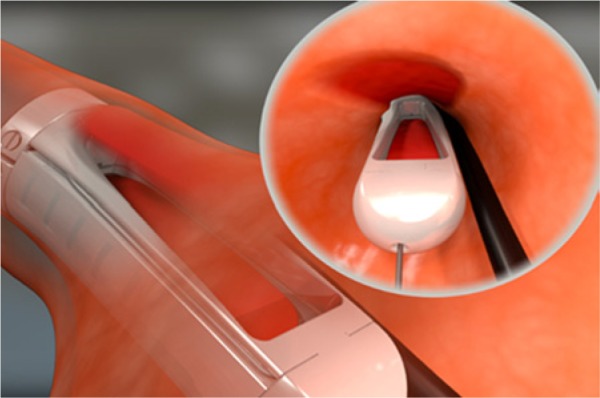
In the second patient, we found the supine and left lateral decubitus position difficult because the fundus of the stomach could not be captured correctly for excisions. We tried then used the right lateral decubitus position which allowed tissue capture of the proximal greater curvature such that injection and excision could be consistently performed. However, the suture device (Figure 2) malfunctioned and this procedure was terminated as well.
Figure 2.
The suture device with suture needles and attached sutures.
The following 5 patients all had a complete procedure although in the third patient the excisions were not in ideal position. With the subsequent patients the mucosal excisions were in satisfactory position and the procedure was performed as follows.
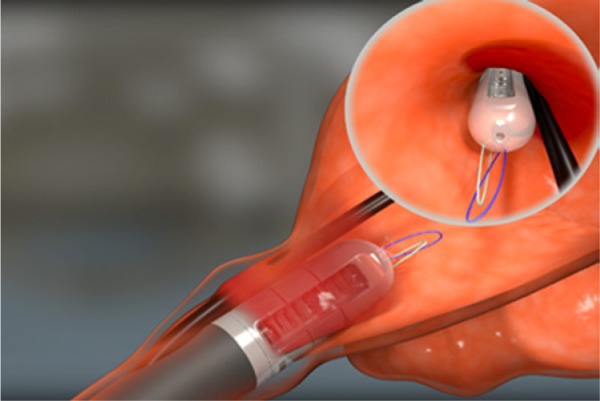
The excision device was introduced into the proximal stomach and the stomach was insufflated after a 6 mm endoscope was introduced through the device (Supplemental Data Figure S1; available online at http://SRI.sagepub.com/supplemental). After excision device positioning, a vacuum was applied and tissue was pulled into the excision device trough. A 4.2% hypertonic saline (HTS) and 1:100 000 adrenaline solution was injected and the vacuum was discontinued. The tissue escaped the capsule trough (Supplemental Data Figure S2) and the cushion was inspected for position, length, height, and width. If satisfactory the cushion was recaptured and again injected (Supplemental Data Figure S3). Excision was performed after a 60-second delay for adrenaline-mediated vasoconstriction. The vacuum was discontinued, the stomach was reinsufflated and the mucosa visualized in the bottom of the trough (Figure 3). A small elevating platform at the bottom of the trough was activated and the mucosal/submucosal strip was positioned (Supplemental Data Figure S4) so that it could be removed. A foreign body grasping forceps was introduced through the endoscope (Supplemental Data Figure S5) and the tissue was removed with the endoscope through the endoscope channel (Supplemental Data Figure S6). The tissue was pinned on a cork board for inspection and measurements. This same process was repeated 2 more times with the 3 excisions placed adjacent to each creating one confluent excision bed (Supplemental Data Figure S7). Blood clots were removed and then hypertonic saline was injected along the lesser curvature to form a restrictive fibrotic ring in obese patients only.
Figure 3.
The mucosa submucosal strip is seen with the through.
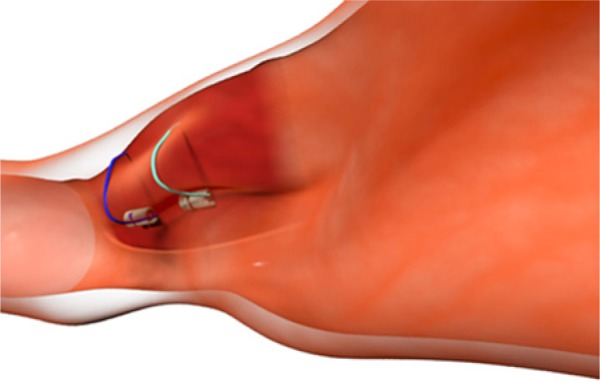
The suture device was introduced over a guidewire and positioned for suturing within excision #3 (Figure 4). The sutures are full thickness if placed within the excision bed and partially close the GEJ at the greater curvature side. A vacuum is applied and after suture application the position of the suture device is checked (Supplemental Data Figure S8). The device is then rotated to the first excision bed and the process is repeated (Supplemental Data Figure S9). The suction is discontinued, the sutures are inspected (Supplemental Data Figure S10) and the suture device is removed from the patient. The sutures are organized outside the patients’ mouth and the distal suture strands are placed into the knotter and between the plug and sleeve (Supplemental Data Figure S11). The knotter is run over the sutures under slight tension into the esophagus and the 6 mm endoscope is introduced for visualization (Figures 5 and Supplemental Data Figure S12). The endoscope is retroflexed in the stomach as the sutures are tightened to the tissue to assure tissue apposition (Supplemental Data Figure S13). This is repeated with the more proximal suture strands and the completed GERD (Figure 6) and obesity procedures (Figure 7) are shown.
Figure 4.
The suture device is positioned for the first suture cycle.
Figure 5.
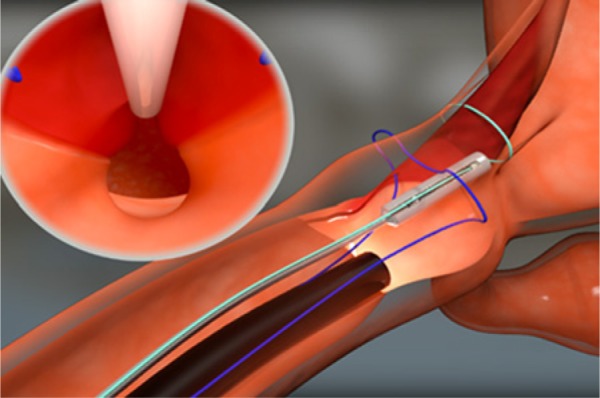
The endoscope monitoring tissue apposition.
Figure 6.
The GERD procedure with excisions more proximally located.
Figure 7.
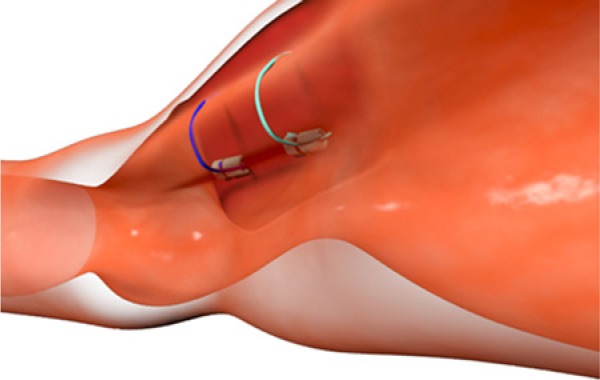
The obesity procedure.
The obesity and GERD procedures differed in 2 ways. The mucosal excisions were closer to the squamocolumnar junction for GERD, and the radial separation of the 2 sets of sutures was greater for the obesity procedure. Thus, the sutured in-folding at the angle of His was larger and more distal for the obesity procedure.
Patient Results
Five GERD patients were evaluated but 2 were excluded—one because of a falsely positive pH score and the other due to a hiatal hernia larger than 2 cm. One obesity patient was excluded due to psychological issues. The first 2 patients to have a GERD procedure experienced instrument malfunction making completion of the procedures not possible. The first patient made an uneventful recovery but the second had a wrist drop that resolved with time. This was due to improper patient positioning. The third patient had micrognathia and limited neck extension making 60 F upper esophageal sphincter dilation impossible. This patient was excluded. The remaining patients had a complete procedure. These patients had the procedure performed in the right lateral decubitus position, and the instrument introduction technique was simplified by a mouth opener that made it possible to deflect the instruments into the proper plane for esophageal introduction. The mucosal excisions were uneventful but only the last 4 patients had excisions placed in what was learned to be the ideal position. During the first three procedures the excisions were difficult to place in the correct position due to redundant folds, and excision site opposition sutures were under excessive tension when tied.
Patient #4 (obese) had the excisions placed on the anterior greater curvature and the knotter was incorrectly used for the first anchor; therefore, she had only 1 of 2 anchors. Hypertonic saline was injected along the lesser curvature as described above, and although the anchor was not evident at 6 and 12 months she did have constriction of her 2 cm hiatal hernia and a 37% excess weight loss (EWL) plus normalization of her elevated baseline blood pressure at 1 year follow-up and 68% EWL at the 2-year follow-up. She had no other comorbidities.
Patient #5 (obese) had the excisions placed correctly on the posterior side of the greater curvature and the procedure was uncomplicated. However, on videotape review it was evident that the outlet was 8 mm in diameter (ideal is 6 mm). The patient at 24-month follow-up did lose weight and had an EBL% of 23%.
Patient #6 (obese) had a complete procedure with a satisfactory result. At 2-year follow-up she was experiencing dysphagia intermittently and had a 6 to 7 mm outlet, and her blood pressure had normalized. She had no other comorbidities. Her EWL% was 24 at 12 months and 30% at 24 months.
Patient #7 (obese) had a complete procedure but vomited repeatedly in the recovery room. Her initial chest X-ray was unremarkable but on the first postoperative day she had free air under both hemidiaphragms. Laparoscopy and simultaneous upper endoscopy showed no perforation. A nasogastric tube was left in place and she recovered and was discharged. However, on day 9 she developed vertigo with repeated vomiting and required rehospitalization. At 6-month endoscopy her gastroplasty was loose and she had no food restriction. The 12-month endoscopy showed no change and the patient had gained 9 lbs from baseline; however, the 24-month follow-up showed a return to the baseline weight. Tables 3 to 6 show the obesity patient cohort baseline information and study results.
Table 3.
Obesity Symptoms and IWQOL Table.
| Baseline |
6 Months |
12 Months |
24 Months |
||||
|---|---|---|---|---|---|---|---|
| Patient | GERD Symptoms | IWQOLa | GERD Symptoms | GERD Symptoms | IWQOL | GERD Symptoms | IWQOL |
| 4 | None | 68 | None | 81 | None | 91 | |
| 5 | None | 69 | None | None | 70 | ||
| 6 | None | 45 | Occasional dyspepsia | 73 | None | 92 | |
| 7 | None | 69 | Occasional regurgitation | 80 | |||
Abbreviation: GERD, gastroesophageal reflux disease; IWQOL, Impact of Weight on Quality of Life Questionnaire.
Higher IWQOL score is improvement.
Table 6.
Excess Weight Loss (% EWL).
| Patient | Baseline Weight, kg/lb/BMI | 3 Month %EWL | 6 Month %EWL | 12 Month %EWL | 24 Month %ELW |
|---|---|---|---|---|---|
| 4 | 185/16/61 | 18.5 | 25 | 37 | 68 |
| 5 | 116/256/42 | 2 | 4 | −0.06 | 23 |
| 6 | 154/337/61 | 19 | 20 | 24 | 30 |
| 7 | 98/216/39 | 14 | 9 | −0.08 | 0 |
Abbreviation: BMI, body mass index.
Table 4.
Obesity Comorbidities Table.
| Baseline |
6 Months |
12 Months |
24 Months |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Sleep Apnea | BP | A1C | Sleep Apnea | BP | A1C | Sleep Apnea | BP | A1C | Sleep Apnea | BP | A1C |
| 4 | No | 135/100 | 5.5 | No | 115/90 | 5.6 | No | 120/80 | 5.2 | |||
| 5 | No | 141/100 | 5.8 | >3× night | 135/95 | 5.7 | >3× night | 150/110 | 5.9 | |||
| 6 | >3× night | 142/98 | 5.6 | >3× night | 110/80 | 5.2 | >3× night | 120/82 | 5.1 | |||
| 7 | >3× night | 118/78 | 5.4 | >3× night | 110/70 | 5.6 | ||||||
Abbreviation: BP, blood pressure.
Table 5.
Endoscopy Results in Obesity Patientsa.
| Patient | Baseline Hill Classification | Operation Result | 6 Months; Gap in mm | 12 Months; Gap in mm | 24 Months; Gap in mm |
|---|---|---|---|---|---|
| 4 | Hill 3 | 2 | 0 | 0 | 0 |
| 5 | Hill 3 | 2 | 0 | ||
| 6 | Hill 3 | 2 | 0 | 0 | 0 |
| 7 | Hill 3 | 3 | 2-3 | 2 |
0, not performed; 1, excisions only; 2, suture and excision not optimal; 3, suture and excision satisfactory.
Patient #8 (GERD) had a complete procedure and made an uneventful recovery. At 12-month follow-up she remains asymptomatic and off all antisecretory medications. Her preoperative HRQOL was 19 and the DeMeester score was 44, compared with 24-month results, which were 6 and 8.9, respectively. Her 12-month endoscopy with a 6 mm endoscope and full insufflation is shown in figure 8. No esophagitis was evident.
Figure 8.

Patient 8’s 12-month follow-up endoscopy using a 6-mm endoscope.
Discussion
The new endoluminal gastroplasty was proven to be feasible, and initial patient outcomes show that it has the potential to effectively treat GERD and obesity. During the study, we learned the proper way to insert the devices, which was simplified by the use of a mouth-opener. The right lateral decubitus position facilitated capture of the proximal greater curvature tissues for excision and suturing. Initial device problems were resolved during the study. Patients who underwent a complete procedure with excisions and sutures in the corrected position had satisfactory results with significant excess weight loss, blood pressure normalization, and acid reflux control for the GERD patient.
A number of antireflux endoscopic procedures have been introduced but only one is based on scar tissue deposition, the Stretta (Mederi Therapeutics Inc, Greenwich, CT) procedure. During this procedure, radiofrequency energy is administered to the LES, inducing fibrosis, and or collagen deposition, which leads to a higher LES yield pressure and a decrease in transient LES relaxation.8 Long-term results proved that the Stretta procedure is effective in terms of GERD symptoms, health-related quality of life (HRQOL), and ongoing medical management.9-11 Noar and Lotfi-Emram9 showed heartburn scores decreased from a mean of 3.67 to 1.18 at 4-year follow-up. Medication usage also decreased significantly, and 85% of patients reduced their medication requirement by half or eliminated it completely. Reymunde and Santiago10 also reported 4-year results on the Stretta procedure. Their GERD symptom scores improved from a mean of 2.7 to 0.6, and 68.67% of patients showed complete resolution of symptoms. Four years after the procedure, 13.75% of the patients were on antisecretory medication. At 12-month EGD, 31.9% of the patients with grade A esophagitis at baseline healed and this remained at 4-year follow-up. The Stretta procedure demonstrates the role of fibrosis in altering the functionality of the LES. In the described gastroplasty procedure, injection of hypertonic saline and the infolding and sutured apposition of excision beds induce fibrosis as well.
Histological examinations showed that collagen deposition after Stretta takes place in the muscularis propria layer.12 The effect of fibrosis in the esophageal wall can be described in an inorganic material analogy. The normal gastric wall is similar to a water hose that has no reinforcements in its wall. In mechanical engineering terms, the lumen wall would be described as being composed of a viscoelastic material that has a low modulus of elasticity, medium yield strength, and limited creep resistance. If you were to maintain a high water pressure on this hose, similar to a pressure created on the gastric lumen repeatedly stretching it secondary to eating, stomach overfilling, vomiting, gagging, hiccough, and heavy lifting, the lumen will expand over time. In mechanical engineering, vernacular it is known as plastic deformation caused by creep and fatigue. In this analogy, fibrosis in the submucosal layer acts as a reinforcement layer to the wall of the garden hose making it less susceptible to expansion or plastic deformation over time. In mechanical engineering terms, the scarred gastric wall would be described as also having a higher modulus of elasticity, higher yield strength, and a higher creep resistance.
The Esophyx procedure is a transoral flexible endoscopic procedure that creates a Toupet fundoplication using proprietary H fasteners. The procedure has shown safety and efficacy in terms of symptom control and quality of life measures at 6-month follow-up.13,14 The Esophyx procedure (transoral incisionless fundoplication) is an endoscopic attempt at duplicating a Toupet fundoplication.
Endoscopic suturing techniques usually involve submucosal suture placement, which has limit procedure-related complications but has also lead to early suture dehiscence and loss of procedural efficacy. This problem may be solved by full-thickness suturing or stapling devices that include the use of pledgets. The NDO plicator was designed to apply a full thickness pledget-reinforced U stitch near the GEJ with serosa-to-serosa apposition. Results using one15 or two16 plications failed to demonstrate a change in LES pressure, or substantial normalization of pH scores. Thus, there is still no effective endoscopic method for the control of GERD. The mucosal excision sutured gastroplasty uses a different concept whereby larger volumes of scar tissue is strategically deposited to restore LES compliance for GERD patients or create an outlet restriction for the obese.
Conclusion
Twenty-four-month patient follow-up shows promising results for the excision gastroplasty. A larger study will be conducted to more accurately determine safety and effectiveness over time.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: SafeStitch Medical, soon to be called Transenterix, funded the research. Drs Filipi and Brandon Hunt were salaried by SafeStitch Medical at the time of the project. Dr Filipi also has partial ownership in SafeStitch Medical.
References
- 1. Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500-1511. [DOI] [PubMed] [Google Scholar]
- 2. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303:235-241. [DOI] [PubMed] [Google Scholar]
- 3. International Association for the Study of Obesity. Estimated relative risk of disease by BMI category: overweight and obesity. http://www.iaso.org/policy/eu-projects-copy/eu-projects/dynamohiaproject/estimatesrelativerisk/ Accessed October 14, 2013.
- 4. Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289:187-193. [DOI] [PubMed] [Google Scholar]
- 5. Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724-1737. [DOI] [PubMed] [Google Scholar]
- 6.Legner A, Tsuboi K, Stadlhuber R. Mucosal excision and suturing for obesity and GERD [published online February 18, 2013]. Surg Innov. 10.1177/1553350613475881. [DOI] [PubMed] [Google Scholar]
- 7. Filipi CJ, Stadlhuber RJ. Initial experience with new intraluminal devices for GERD, Barrett’s esophagus and obesity. J Gastrointest Surg. 2010;14:S121-S126. [DOI] [PubMed] [Google Scholar]
- 8. Kim MS, Holloway RH, Dent J, Utley DS. Radiofrequency energy delivery to the gastric cardia inhibits triggering of transient lower esophageal sphincter relaxation and gastroesophageal reflux in dogs. Gastrointest Endosc. 2003;57:17-22. [DOI] [PubMed] [Google Scholar]
- 9. Noar MD, Lotfi-Emram S. Sustained improvement in symptoms of GERD and antisecretory drug use: a 4-year follow-up of the Stretta procedure. Gastrointest Endosc. 2007;65:367-372. [DOI] [PubMed] [Google Scholar]
- 10. Reymunde A, Santiago N. Long-term results of radiofrequency energy delivery for the treatment of GERD: sustained improvement in symptoms, quality of life and drug use at 4-year follow-up. Gastrointest Endosc. 2007;65:361-366. [DOI] [PubMed] [Google Scholar]
- 11. Meier PN, Nietzschmann T, Akin I, Klose S, Manns MP. Improvement of objective GERD parameters after radiofrequency energy delivery: a European study. Scand J Gastroenterol. 2007;42:911-916. [DOI] [PubMed] [Google Scholar]
- 12. Herman RM, Wojtysiak D, Rys J, et al. Non-Ablative Radiofrequency (RF) Application to Smooth Muscle of Internal an al Sphincter (IAS) – A Tissue Study. http://www.sages.org/meetings/annual-meeting/abstracts-archive/non-ablative-radiofrequency-rf-application-to-smooth-muscle-of-internal-an-al-sphincter-ias-a-tissue-study/ Accessed October 28, 2013.
- 13. Barnes WE, Hoddinott KM, Mundy S, Williams M. Transoral incisionless fundoplication offers high patient satisfaction and relief of therapy-resistant typical and atypical symptoms of GERD in community practice. Surg Innov. 2011;18:119-129. [DOI] [PubMed] [Google Scholar]
- 14. Bell RCW, Mavrelis P, Barnes W, et al. A prospective multicenter registry of patients with chronic gastroesophageal reflux disease receiving transoral incisionless fundoplication. J Am Coll Surg. 2012;215:794-809. [DOI] [PubMed] [Google Scholar]
- 15. Rothstein R, Filipi C, Caca K, et al. Endoscopic full-thickness plication for the treatment of gastroesophageal reflux disease: a randomized, sham-controlled trial. Gastroenterology. 2006;131:704-712. [DOI] [PubMed] [Google Scholar]
- 16. Von Renteln D, Schiefke I, Fuchs KH, et al. Endoscopic full-thickness plication for the treatment of gastroesophageal reflux disease using multiple Plicator implants: 12-month multicenter study results. Surg Endosc. 2009;23:1866-1875. [DOI] [PubMed] [Google Scholar]


