Abstract
Although adults with autism spectrum disorder are an increasingly identified patient population, few treatment options are available. This preliminary randomized controlled open trial with a parallel design developed two group interventions for adults with autism spectrum disorders and intelligence within the normal range: cognitive behavioural therapy and recreational activity. Both interventions comprised 36 weekly 3-h sessions led by two therapists in groups of 6–8 patients. A total of 68 psychiatric patients with autism spectrum disorders participated in the study. Outcome measures were Quality of Life Inventory, Sense of Coherence Scale, Rosenberg Self-Esteem Scale and an exploratory analysis on measures of psychiatric health. Participants in both treatment conditions reported an increased quality of life at post-treatment (d = 0.39, p < 0.001), with no difference between interventions. No amelioration of psychiatric symptoms was observed. The dropout rate was lower with cognitive behavioural therapy than with recreational activity, and participants in cognitive behavioural therapy rated themselves as more generally improved, as well as more improved regarding expression of needs and understanding of difficulties. Both interventions appear to be promising treatment options for adults with autism spectrum disorder. The interventions’ similar efficacy may be due to the common elements, structure and group setting. Cognitive behavioural therapy may be additionally beneficial in terms of increasing specific skills and minimizing dropout.
Keywords: adult, Asperger disorder, autism, cognitive behaviour therapy, group, randomized controlled trial
Introduction
The main characteristics of autism spectrum disorder (ASD; i.e. Asperger syndrome, autistic disorder or pervasive developmental disorder–not otherwise specified) are qualitative impairment of social interaction, qualitative impairments in communication and restricted and repetitive stereotyped patterns of behaviour, interests and activities (American Psychiatric Association, 2000). Individuals with ASDs also seem to be vulnerable to a number of psychiatric and neurological disorders, such as depression, obsessive-compulsive disorder, attention deficit disorder, developmental coordination disorder, epilepsy, sleep disturbances and anxiety (Kopp et al., 2010; Myers and Plauché Johnson, 2007; Wink et al., 2010). Moreover, hyper- or hyposensitivity to pain, touch, movement, sound, smell and light is often reported (Minshew and Hobson, 2008).
In addition to psychiatric and neurological vulnerabilities, adults with ASDs also face a number of social challenges such as having low self-esteem (Tantam, 2000) and being bullied during the school years (Bejerot and Humble, 2013; Cappadocia et al., 2012; Vlachou et al., 2011). As adults, they are single to a much greater extent than psychiatric controls (Rydén and Bejerot, 2008), and less than 16% report having friends (Shattuck et al., 2007). Although the educational level in this population is comparable to that of other psychiatric populations, patients with ASDs have significantly lower employment rates (Rydén and Bejerot, 2008). In addition, unfulfilled needs regarding privacy, choice making and independency may affect quality of life negatively (Gaus, 2011). Due to severe executive problems, daily life activities can be experienced as chaotic (Frith, 2004). As a result of these psychiatric and social difficulties, quality of life is often impaired in patients with ASDs (Jennes-Coussens et al., 2006).
Although the prevalence of ASDs among psychiatric patients is reported to be low (Nylander and Gillberg, 2001), these patients are not uncommon at specialized psychiatric outpatient settings. The intensity of care needed and the relative difficulty in treating this group lead to a high frequency of office visits, evaluations and therapeutic contacts. Knowledge and recognition of ASDs have increased enormously in recent years. According to the Stockholm psychiatric patient registry, during the last 20 years, less than 20 adults were diagnosed with Asperger syndrome each year until 2004. In 2008, almost 500 were diagnosed, and in 2010, the number of new cases reached almost 700. As this new patient population has emerged in clinical practice during the last decade, there is an urgent need to identify suitable treatment options.
Available treatment options for adults with ASDs
The Stockholm municipality guideline for treatment of adults with ASDs lists housing support or professional advice, psycho-education, cognitive aides and financial support as suitable interventions (Axén et al., 2010). Psychotherapeutic and social interventions are not mentioned, possibly due to lack of clinical studies investigating their efficacy. Psychological methods designed to treat children with ASDs are difficult to adapt to adult patients because they either involve parental participation or are too time-consuming and authoritative, for example, applied behaviour analysis (Virués-Ortega, 2010). Alternative treatment options to psycho-therapeutical interventions are social training programmes. These target peer relationships and provide instruction and rehearsal of social skills (Frankel et al., 2010; Hillier et al., 2011). Recently, a brief social training programme was adapted to suit young adults, and a pilot study showed promising results (Gantman et al., 2012). Another treatment option is training in planning and engaging in recreational activities (Palmen et al., 2011). In adults with ASDs and intellectual disability, quality of life has been positively associated with engagement in regular recreational activities (Billstedt et al., 2011). Furthermore, for children with ASDs, recreational activity has been shown to be equally influential as cognitive behavioural therapy (CBT) in reducing anxiety (Sung et al., 2011). Social training or recreational programmes do not, however, target the psychiatric symptoms often linked to ASDs, or the multitude of social difficulties common in this group.
To date, apart from social training and symptom-specific programmes, such as CBT treatment of anxiety for individuals with ASDs (Lang et al., 2010), there are very limited treatment options for adults with ASDs. Much of the published literature is clinical or anecdotal, or purely based on theory. A few publications target the specific difficulties of providing psychotherapy for this patient population (Gaus, 2007, 2011; Munro, 2010; Weiss and Lunsky, 2010). There are a number of challenges, some of which include social withdrawal making it difficult for patients to enter psychotherapy (Munro, 2010), a sense of being misunderstood leading to low expectations of getting help (Gaus, 2007; Munro, 2010) and insufficiently trained and experienced therapists (Attwood, 2007; Gaus, 2011; Munro, 2010).
There is undoubtedly a need for the development of treatment options for adult psychiatric patients with ASDs. Group settings enable social interaction and sharing experiences with others, thereby reducing social isolation (Attwood, 2007; Munro, 2010; Weiss and Lunsky, 2010). In addition, the need for structure and predictability makes CBT an attractive treatment option (Gaus, 2007, 2011). Within CBT, psycho-education on ASDs and related psychiatric symptoms and social training are recommended (Gantman et al., 2012; Gerhardt and Lainer, 2010). Specific CBT techniques that are suitable include setting goals, home assignments and practising social skills for everyday life (Gaus, 2007). In summary, five elements of interventions that seem beneficial to adults with ASDs are group setting, structure and predictability, psycho-education, social training and ASD-suitable CBT techniques. It is, however, unclear whether the positive effects of CBT extend beyond the influence of social interaction gained by any type of group intervention.
The purpose of this study was to develop and compare two group interventions for psychiatric patients with ASDs and normal intellectual ability. The first intervention was CBT developed to suit adults with ASDs, and the second intervention was recreational activity enabling social interaction. The recreational activity was designed to control for social interaction effects. We hypothesized that both interventions would lead to improvement in primary measures of quality of life, sense of coherence and self-esteem, as well as in the exploratory analysis of the secondary measures of psychiatric symptoms. A greater effect in the CBT intervention compared to recreational activity was also expected, due to patients in the CBT intervention receiving a wider range of psychotherapeutic techniques.
Methods
This study was an open randomized controlled trial, of parallel design, comparing group CBT with group recreational activity, in adult psychiatric patients with ASDs. It was carried out between August 2005 and September 2011, at an outpatient tertiary psychiatric clinic situated in Stockholm. The unit specialized in assessment of ASDs and attention deficit hyperactivity disorder (ADHD) in difficult-to-treat psychiatric patients. The regional ethics committee in Stockholm approved the study, and informed consent was obtained from all participants. Both interventions were provided at a low cost for the patients (£7 per session)
Patients and recruitment
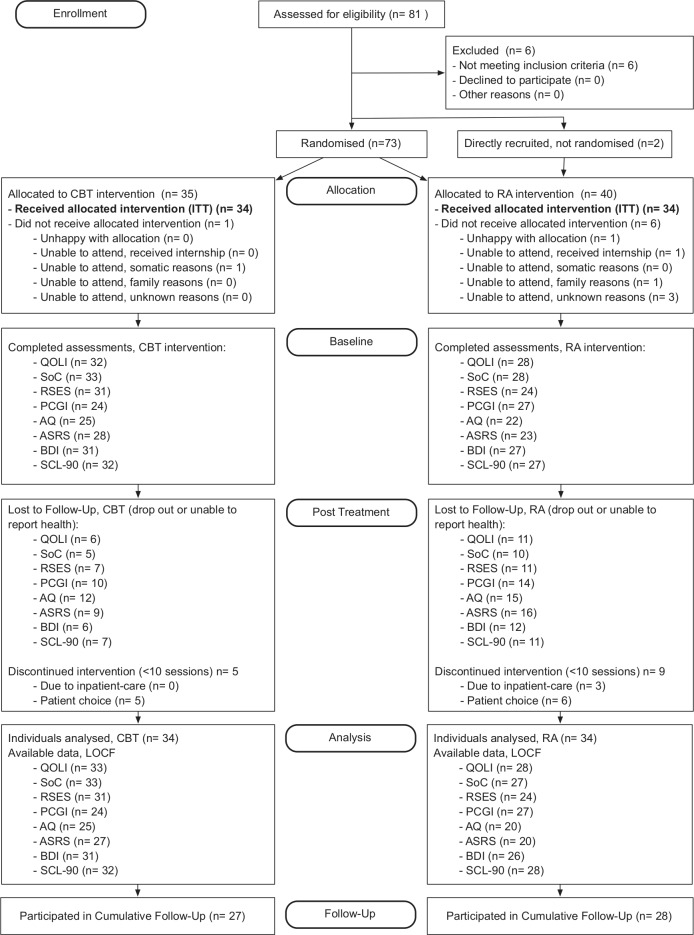
Participants were recruited through referrals from psychiatric clinics and advertisements in patient organizations and publications. All participants had been clinically diagnosed with ASD, confirmed by medical records, the Autism Diagnostic Observational Schedule (ADOS; Lord et al., 2000) and clinical interviews. After inclusion, 73 patients were stratified by gender and blindly randomized to one of the two treatment conditions. A team member uninvolved in the study made the random allocation manually with the use of a paper-based lottery. Two additional patients were included without being randomized during the last year of the study to compensate for the greater attrition in the recreational intervention. Overall, 7 patients chose not to begin intervention, resulting in 68 participants. A total of 14 participants who attended less than 10 sessions were defined as dropouts resulting in 54 completers (see Figure 1).
Figure 1.
Study flowchart.
CBT: cognitive behavioural therapy; RA: recreational activity group; QOLI: Quality of Life Inventory; SoC: Sense of Coherence Scale; PCGI-S: Patient Rated Clinical Global Improvement–Severity; SCL-90 (mean): Symptom Checklist 90; AQ: Autism Quotient; BDI: Beck Depression Index; ASRS: Adult ADHD Self-Report Scale; RSES: Rosenberg Scale of Self-Esteem; CI: confidence interval; LOCF: last observation carried forward.
In addition to having an ASD diagnosis, inclusion criteria were age 18 years or above and having normal intellectual ability as indicated by mainstream schooling and absence of an intellectual disability diagnosis. All forms of psychiatric co-morbidity were accepted except current substance abuse, current psychosis, high suicide risk and being an inpatient. From the second year, suicidality and inpatient care were no longer exclusion criteria since the group setting was considered to be beneficial to these patients. Exclusion criteria were kept at a minimum to ensure clinical validity.
Baseline patient characteristics
The mean age of patients at recruitment was 31.8 years (standard deviation (SD) = 9.03, range = 19–53 years, n = 75). A total of 83% were single, and 26% were in part-or full-time employment or studies. The mean ADOS score was 11.2 (SD = 3.86, n = 50). With a mean of 10.3 psychiatric inpatient days in the year prior to treatment (SD = 36.0, range = 0–164, n = 67; missing data n = 8), the participants constituted a severely ill population. More than one-third of the participants had previously attempted suicide, 85% had at least one co-existing psychiatric condition and 79% were treated with psychotropic medication. There were no significant differences in demographics or psychiatric health data between intervention groups after randomization, except that current diagnoses of depression and anxiety disorders were more common in the CBT group (p < 0.05), see Table 1.
Table 1.
Patient demographics and psychiatric health data.
| CBT (n = 35) | RA (n = 40) | |
|---|---|---|
| Age, years (SD) | 31.9 (8.5) | 31.8 (9.6) |
| ADOS, total score (SD) (⦰ = 25) | 11.4 (4.6) | 11.1 (3.2) |
| Gender, n (%) | ||
| Male | 17 (49) | 24 (60) |
| Civil status, n (%) | ||
| Married or co-habiting (⦰ = 3) | 4 (12) | 4 (11) |
| Children, n (%) (⦰ = 4) | ||
| Yes | 3 (9) | 5 (14) |
| Occupational status, n (%) (⦰ = 15) | ||
| Employed or student | 6 (22) | 11 (35) |
| Living condition, n (%) (⦰ = 6) | ||
| Independent | 28 (82) | 24 (69) |
| Education, n (%) (⦰ = 7) | ||
| 9 years | 3 (9) | 4 (12) |
| 11 years | 3 (9) | 1 (3) |
| 12–13 years | 15 (43) | 15 (45) |
| >13–15 years | 14 (40) | 13 (39) |
| ASD-adapted school,a n (%) (⦰ = 25) | ||
| Yes | 5 (18) | 6 (27) |
| Previous suicide attempt, n (%) (⦰ = 9) | ||
| Yes | 14 (41) | 9 (28) |
| Previous inpatient care, n (%) (⦰ = 8) | ||
| Yes | 9 (23) | 12 (34) |
| Co-existing psychiatric symptoms, n (%) (⦰ = 9) | ||
| Current depression* | 22 (67) | 13 (39) |
| Lifetime depression | 29 (88) | 24 (73) |
| Current anxiety disorderb* | 12 (36) | 5 (15) |
| ADHD or ADD | 15 (45) | 10 (30) |
| Lifetime OCD | 6 (18) | 8 (24) |
| Borderline personality disorder | 5 (15) | 2 (6) |
| Other psychiatric conditionsc | 13 (38) | 15 (45) |
| Any current co-existing condition | 29 (88) | 27 (82) |
| Current use of psychotropic medication, n (%) (⦰ = 13) | ||
| Antidepressants | 20 (67) | 18 (56) |
| Benzodiazepines | 13 (43) | 7 (22) |
| Antihistamines | 10 (23) | 10 (31) |
| Hypnotics | 10 (33) | 8 (25) |
| Antipsychotics | 8 (27) | 8 (25) |
| Central stimulants | 6 (20) | 5 (16) |
| Antiepileptics | 7 (23) | 6 (19) |
| Other psychotropic medication | 7 (23) | 3 (9) |
| Any psychotropic medication | 24 (80) | 25 (78) |
CBT = cognitive behavioural therapy; RA = recreational activity; ⦰: missing data.
Adaptations within mainstream schooling, such as small group setting or assistant teachers.
Current diagnosis of social phobia, panic syndrome or other anxiety disorder.
Lifetime diagnosis of one or more of the following: psychosis, personality disorder, eating disorder, bipolar disorder or dissociative disorder.
Significant difference between groups (p < 0.05).
Intervention procedures
The interventions were labelled ‘course group’ (CBT) and ‘social group’ (recreational activity) in all materials, to reduce expectancy effects. Each intervention group was divided into five subgroups consisting of 6–8 patients and two therapists. All subgroups were provided with the same frequency and number of sessions: 36 weekly 3-h sessions during the course of two semesters. In both conditions, subgroups were lead by two collaborating therapists. All therapists received qualified supervision once or twice monthly by trained supervisors during the first 3 years of the project.
A psychiatrist and a clinical psychologist, both trained in CBT, led the CBT intervention. They treated 30 and 26 patients, respectively, corresponding to 86% and 74% of allocated patients. The co-therapists were four licensed psychologists, three of whom had special training in CBT.
A psychiatric nurse assistant and a social worker, both with more than 20 years of experience in the field, led the recreational activity intervention. They treated 31 and 27 patients corresponding to 78% and 68% of allocated patients, respectively. The occupations of the four co-therapists were occupational therapist, special education teacher, social worker and psychiatric nurse assistant.
The CBT intervention
This was specifically designed for psychiatric patients with ASDs. The setting was tailored to accommodate patients’ poor executive functioning and minimize the requirement of social skills. All psychotherapeutic interventions aim at inducing change. However, if symptoms are longstanding, pervasive change tends to be more difficult to achieve (Garety et al., 2008). Thus, acceptance of and insight into the dysfunction is essential for severely ill patients to gain improvements. Techniques for introducing acceptance and change to participants were drawn from psychotherapeutic techniques developed to treat psychiatric patients with severe symptoms, such as Dialectical Behaviour Therapy (DBT; Linehan, 1984). However, some DBT-techniques, such as metaphors, exposure and limit setting, poorly suited adults with ASDs and so were only partially used in this study. Generally, the therapists focused on being clear, sincere and open to the impairments associated with ASDs, with the goal to keep patients in treatment.
Based on available literature, the CBT intervention consisted of five elements: (a) structure, (b) group setting, (c) psycho-education (e.g. lectures and discussions on ASD and psychiatric symptoms, including learning to identify and reappraise maladaptive thoughts), (d) social training (e.g. skill building such as practising phone calls and asking for help) and (e) cognitive behavioural techniques (e.g. setting goals, role-playing, exposure exercises and conducting behaviour analysis). Furthermore, the treatment was divided into three thematic modules: (a) self-esteem and ASD awareness, (b) social contacts and everyday life and (c) psychological and physical health. A manual describing the 36 individual sessions was created prior to starting the treatment (Bejerot and Björnstierna, 2011), see Appendix 1 for full session plan.
Each session followed a strict agenda: (a) introduction and presentation of the agenda of the day, (b) review of homework assignments from the previous session, (c) psycho-educative lecture and discussions on the session topic, (d) coffee break with buns or sandwiches and social interaction, (e) relaxation or mindfulness exercise, (f) discussions and exercises on the session topic, (g) distribution of homework and (h) evaluation and end of session. A written contract regarding confidentiality and respect for other participants was signed prior to treatment. In each subgroup, 3–4 community support-workers participated in the group as a part of their professional training. This provided an opportunity for both patients and support-workers to exchange experiences by taking on roles of peer tutors in the social training segments of the CBT intervention (White et al., 2010). The support-workers were not previously known to the participants.
Recreational activity intervention
The purpose of the recreational activity intervention was to facilitate social interaction and to break social isolation. The therapists did not provide any deliberate techniques, such as psycho-education, social training or CBT. Instead, this intervention relied on structure and group setting only. During the first session, participants were asked to write down group activities they would like to engage in. The therapists created a list of the suggested activities, such as visiting museums, playing board games, cooking, restaurant visits, boating, cinema and taking walks. Each week, participants voted for the next session’s activity. All entrance fees and additional costs were paid for by the project, with a budget for each session of £45.
Assessments and gathering of data
Demographic data were collected during the intake interview. Then, psychiatric diagnoses of ASDs were collected from medical records, as were data on co-morbidities and use of psychotropic medications. Baseline assessment was made after randomization, hence not blinded to intervention type. The post-treatment assessment was completed during the last intervention session.
In the baseline and post-treatment assessments, many patients showed difficulty in completing assessments, which resulted in missing data. Reasons for not completing assessment included fear of being misinterpreted, difficulty with responding to questions, difficulty with quantifying experience (e.g. choosing between a ‘3’ and a ‘4’), procrastination and lack of motivation.
A long-term follow-up was conducted, regardless of patient participation year, between July and September 2011 (ranging from 8 to 57 months after treatment termination). To minimize missing data, the follow-up survey was shortened in consideration of patients’ limited capabilities. In order to encourage involvement, participants could complete either a paper- or web-based questionnaire, and a telephone interview was performed with those who did not respond to the questionnaire. Participation was gratified with two cinema tickets.
Outcome measures
Primary outcome measures
Primary outcomes consisted of the three following self-rated questionnaires. The Quality of Life Inventory (QOLI; Frisch et al., 1992), a 32-item measurement of life satisfaction assessing areas, such as health, relationships, employment and living conditions. The QOLI ranges from −6 to 6 and negative values correspond to being ‘unsatisfied’. Sense of Coherence (SoC) scale (Antonovsky, 1993) is a 29-item scale that measures perceived comprehensibility, manageability and meaningfulness in life. The Rosenberg Self-Esteem Scale (RSES; Rosenberg, 1962), a 10-item instrument, measures self-esteem. Both the SoC and RSES are scales on which high scores indicate good health. Participants completed QOLI at baseline, post-treatment and follow-up. SoC and RSES were completed at baseline and at post-treatment.
Secondary outcome measures
To explore whether autistic traits or psychiatric symptoms would be affected by the interventions, the following six self-rating instruments were used: the Symptom Checklist 90 (SCL-90; Derogatis and Cleary, 1977), a 90-item questionnaire assessing the presence and severity of various psychiatric symptoms; the Autism Quotient (AQ; Baron-Cohen et al., 2001), a 50-item screening instrument for measuring autistic traits; the Beck Depression Inventory (BDI; Beck et al., 1996), a 20-item questionnaire assessing depression and the Adult ADHD Self-Report Scale (ASRS; Kessler et al., 2005) for measuring inattention, hyperactivity and impulsivity. These outcomes were measured at baseline and at post-treatment. These instruments were chosen as part of the diagnostic procedure, and used as exploratory outcome measures.
To assess participants’ subjective global functioning, they completed the self-rated Clinical Global Impression Scale–Severity (CGI-S) and Clinical Global Impression Scale–Improvement (CGI-I) (Guy, 1976). General severity of impairment was assessed using CGI-S ranging from 1 = ‘not ill or dysfunctional’ to 7 = ‘extremely ill or dysfunctional’. Improvement of impairment was assessed with CGI-I, ranging from 7 = ‘very much worse’ to 1 = ‘very much improved’, 4 = ‘no change’. CGI-S was completed at baseline and post-treatment and CGI-I at post-treatment and at follow-up.
Follow-up assessment
In addition to the QOLI and CGI-I, a question on subjective improvement in well-being was included, Compared to before treatment, how do you feel today? (with response options of ‘worse’, ‘no change’ or ‘improved’). Five questions on changes in life were also presented. A priming question, Has anything in your life changed as a result of your participation in the group? was followed by five individual statements, each rated on a 5-point Likert scale ranging from ‘strongly agree’ to ‘disagree’, with no neutral option: (a) my ability to express my needs is improved, (b) I have a greater understanding of my own difficulties, (c) my self-acceptance has improved, (d) I feel happier and (e) I have more social contacts than before. The responses were dichotomized into ‘agree’ and ‘disagree’.
Statistical analysis
In order to reach adequate power, the study aimed to include 23 patients in each treatment condition reaching a power of 80% with a hypothesized effect size of d = 0.8. All statistical analyses were performed with SPSS version 19. Results were calculated for patients who participated in at least one treatment session (n = 68, 34 in each intervention) unless otherwise specified. All results presented used an intention-to-treat (ITT) principle, and missing data were substituted with last observation carried forward (LOCF).
Background characteristics, co-existing psychiatric conditions and dropout rates for the two intervention groups were compared using χ2 tests. Differences between intervention groups’ baseline measures were analysed using two-sided independent t tests, as were differences between completers and dropouts’ baseline assessment scores. Then, repeated-measures analyses of variance (ANOVAs) were used to calculate between- and within-group effects on all continuous variables, and were completed post hoc with dependent t tests to calculate Cohen’s d. Differences between the interventions in CGI-I were examined using a one-way ANOVA. Reported change in the follow-up survey was compared between the interventions using independent t tests. Treatment effect calculations (Cohen’s d) were performed using pooled SDs.
Results
Primary outcomes – quality of life and psychological well-being
The participants reported an increase in QOLI scores at post-treatment compared to baseline (F(1, 59) = 10.48, p = 0.002, d = 0.31, n = 60; missing data n = 8) reaching a medium effect size. A significant increase from baseline was also sustained at follow-up (F(2, 58) = 9.00, p < 0.001, d = 0.39, n = 60; missing data n = 8). However, no significant difference in ratings was found between the two interventions, see Table 2. These results were replicated in a complementary analysis using only completers (between-group effects: QOLI – p = 0.13, SoC – p = 0.07). There were no significant changes in SoC or RSES from baseline to post-treatment.
Table 2.
Treatment outcome measures.
| Effect size LOCF |
Effect size LOCF |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline |
Post-treatment |
Cumulative follow-up |
Between-group comparison |
p | All participants before–after comparison |
p | |||||||||
| n | Mean | SD | n | Mean | SD | n | Mean | SD | d | Mean difference (95% CI) | d | Mean difference (95% CI) | |||
| QOLI | |||||||||||||||
| CBT | 32 | −0.11 | 1.90 | 32 | 0.64 | 1.68 | 32 | 0.64 | 1.69 | 0.43 | 0.75 (0.20, 1.29) | 0.19 | 0.39 | 0.67 (0.30, 1.04) | <0.01 |
| RA | 28 | −0.28 | 1.62 | 28 | −0.01 | 1.59 | 28 | 0.30 | 1.72 | 0.35 | 0.58 (0.06, 1.09) | ||||
| SoC | |||||||||||||||
| CBT | 33 | 95.94 | 21.08 | 33 | 101.39 | 20.56 | – | – | – | 0.26 | 6.21 (−1.64, 14.05) | 0.09 | 0.05 | 1.25 (−5.2, 7.69) | 0.70 |
| RA | 27 | 100.48 | 22.78 | 27 | 96.26 | 29.27 | – | – | – | −0.16 | −4.75 (−15.51, 6.01) | ||||
| RSES | |||||||||||||||
| CBT | 31 | 12.52 | 6.38 | 31 | 13.90 | 6.80 | – | – | – | 0.21 | −1.39 (0.13, 2.65) | 0.17 | 0.12 | 0.13 (−1.83, 2.08) | 0.15 |
| RA | 24 | 13.50 | 5.96 | 24 | 13.46 | 6.38 | – | – | – | −0.01 | 0.04 (−1.85, 1.76) | ||||
| PCGI-S | |||||||||||||||
| CBT | 24 | 3.25 | 0.94 | 24 | 3.29 | 0.91 | – | – | – | 0.04 | 0.05 (−0.29, 0.38) | 0.98 | 0.04 | 0.05 (−0.19, 0.3) | 0.69 |
| RA | 27 | 3.37 | 0.88 | 27 | 3.41 | 1.12 | – | – | – | 0.04 | 0.05 (−0.34, 0.44) | ||||
| SCL-90 (mean) | |||||||||||||||
| CBT | 32 | 1.45 | 0.64 | 32 | 1.41 | 0.61 | – | – | – | −0.07 | −0.04 (−0.21, 0.13) | 0.88 | −0.07 | 1.03 (0.52, 1.53) | 0.37 |
| RA | 28 | 1.42 | 0.85 | 28 | 1.36 | 0.77 | – | – | – | −0.07 | −0.06 (−0.21, 0.09) | ||||
| AQ | |||||||||||||||
| CBT | 25 | 30.60 | 7.01 | 25 | 30.96 | 6.99 | – | – | – | 0.05 | 0.36 (−1.89, 2.61) | 0.32 | −0.05 | −0.05 (−0.16, 0.06) | 0.62 |
| RA | 20 | 30.05 | 9.94 | 20 | 28.60 | 10.28 | – | – | – | −0.14 | −1.45 (−4.53, 1.63) | ||||
| BDI | |||||||||||||||
| CBT | 31 | 15.13 | 7.56 | 31 | 15.48 | 8.77 | – | – | – | 0.04 | 0.35 (−2.28, 2.99) | 0.76 | 0.08 | −0.44 (−2.24, 1.35) | 0.58 |
| RA | 26 | 18.85 | 9.21 | 26 | 20.00 | 11.70 | – | – | – | 0.11 | 1.15 (−3.87, 6.18) | ||||
| ASRS | |||||||||||||||
| CBT | 27 | 38.67 | 11.51 | 27 | 39.63 | 10.57 | – | – | – | 0.09 | 0.96 (−2.10, 4.03) | 0.32 | 0.01 | 0.72 (−1.89, 3.33) | 0.90 |
| RA | 20 | 36.85 | 12.11 | 20 | 35.85 | 12.68 | – | – | – | −0.08 | −1.00 (−3.25, 1.25) | ||||
CBT: cognitive behavioural therapy; RA: recreational activity group; QOLI: Quality of Life Inventory; SoC: Sense of Coherence Scale; PCGI-S: Patient Rated Clinical Global Improvement–Severity; SCL-90 (mean): Symptom Checklist 90; AQ: Autism Quotient; BDI: Beck Depression Index; ASRS: Adult ADHD Self-Report Scale; RSES: Rosenberg Scale of Self-Esteem; CI: confidence interval; d: Cohen’s d calculated with pooled SD; SD: standard deviation; LOCF: last observation carried forward.
Secondary outcomes – psychiatric symptoms
As shown in Table 2, there were no changes in any measures of psychiatric health (i.e. SCL-90, AQ, BDI or ASRS) or CGI-S between baseline and post-treatment. Despite this, nearly two-thirds of the patients rated themselves as improved according to CGI-I (mean = 3.10, SD = 0.97; improvement n = 24; no change n = 14; deterioration n = 1), with a difference between groups favouring CBT (F(1, 37) = 7.11, p = 0.01, d = 0.6, n = 39; missing data n = 29). However, at follow-up, the majority of participants reported ‘no change’ in CGI-I, and no significant difference between intervention groups was observed (mean = 3.63, SD = 0.77; improvement n = 16; no change n = 31; deterioration n = 1; F(1, 46) = 0, p = 1.00, n = 48; missing data n = 20).
Follow-up outcomes
At follow-up, 67% (n = 16) of patients participating in CBT reported improved well-being compared to 27% (n = 7) of patients in recreational activity (χ2 = 8.72, df = 2, p = 0.013, n = 50; missing data n = 18). Moreover, as shown in Table 3, 56% of patients reported improved expression of needs with significantly higher rates of positive responses in the CBT intervention (χ2 = 5.66, df = 1, p = 0.02, n = 46; missing data n = 22). Similarly, 76% reported improved understanding of own difficulties with significantly higher rates of positive responses in the CBT intervention (χ2 = 3.95, df = 1, p < 0.05, n = 50; missing data n = 18). Across both interventions, 62% of participants reported improved self-acceptance, 49% reported that they felt happier than prior to treatment and 28% reported more social contacts (n = 50; missing data n = 18). However, there were no differences between interventions regarding improvements in self-acceptance, happiness or social contacts.
Table 3.
Follow-up questionnaire.
| Has anything in your life changed because of your participation in the group? | n | CBT |
RA |
χ 2 | df | p | ||
|---|---|---|---|---|---|---|---|---|
| Yes, n (%) | No, n (%) | Yes, n (%) | No, n (%) | |||||
| I have more social contacts than before | 50 | 7 (28) | 18 (72) | 7 (28) | 18 (72) | 0.00 | 1 | 0.62 |
| I have a better understanding of my own difficulties* | 50 | 22 (88) | 3 (12) | 16 (64) | 9 (36) | 3.947 | 1 | 0.05 |
| My self-acceptance has improved | 50 | 18 (72) | 7 (28) | 13 (52) | 12 (48) | 2.122 | 1 | 0.12 |
| My ability to express my needs is improved* | 46 | 17 (74) | 6 (26) | 9 (39) | 14 (61) | 5.662 | 1 | 0.02 |
| I feel happier | 47 | 12 (52) | 11 (48) | 11 (46) | 13 (54) | 0.189 | 1 | 0.44 |
CBT: cognitive behavioural therapy group; RA: recreational activity group.
p < 0.05.
Dropout rates and session attendance
Of patients allocated to the CBT intervention, 17% (n = 6) dropped out from treatment compared to 38% (n = 15) allocated to the recreational activity intervention (χ2 = 3.84, p = 0.05, n = 75). The completers participated in a mean of 28 (SD = 6.8) sessions of the CBT intervention and 25 sessions (SD = 5.9) of the recreational activity intervention (t(58) = 1.837, p = 0.07). Dropouts (n = 21) and completers (n = 54) differed in SoC at baseline (t(62) = 2.63, p = 0.01), with dropouts (mean = 80.5, SD = 29.3) showing lower scores than completers (mean = 100.2, SD = 21.9). Completers and dropouts did not significantly differ on any other baseline measures.
Discussion
This study successfully developed and compared two group interventions for adult psychiatric patients with ASDs. The hypotheses that both interventions would lead to improvements and that CBT would have a stronger effect were both partially supported. The group CBT and group recreational activity interventions were equally beneficial to participants in increasing their quality of life. Psychiatric symptoms, SoC and self-esteem were not affected by either intervention. CBT resulted in less attrition than recreational activity, and in addition, participants who received CBT rated themselves as more improved at post-treatment. At follow-up, CBT participants reported better well-being, greater understanding of their own difficulties and improved ability to express needs, compared to participants in the recreational activity intervention. However, findings should be considered preliminary, due to the small sample size and the lack of a non-treated control group.
The value of the group setting
The group setting of both interventions enabled social interaction and sharing experiences. This may have promoted participants’ self-acceptance by allowing them to gain insight into both the impairments and the strengths that characterize the disorder, and to recognize that others share similar challenges. As increases in self-acceptance and quality of life were observed for both intervention groups, such benefits may be due to the group setting itself as opposed to the specific treatment techniques. Although people with ASDs often have social anxiety and may be reluctant to participate in group settings, the current findings indicate that group settings may be beneficial for their quality of life and self-acceptance. However, the range in time passed between treatment termination and follow-up (8–57 months) means that the specific long-term effect on quality of life is unclear. Future research could apply standardized point of assessments for follow-up investigation of longitudinal treatment effects on quality of life in more detail.
Strengths of the CBT intervention
The recreation activity involved only the intervention elements of structure and group setting, whereas the CBT intervention also included the elements of psycho-education, social training and CBT techniques. Thus, participants in CBT may have developed greater understanding of their own difficulties and improved ability to express needs and receive support because the aim of psycho-education and social training is to enhance these capacities. Plausibly, the difference in well-being scores at follow-up also represents greater insight gained from CBT rather than recreational activity. However, as no group differences were observed in other indicators of well-being (such as the QOLI), the links between CBT, greater insight and increased well-being need further investigation. The inclusion of support-workers was not specifically evaluated. Although the support-workers were active in the social training segments of the CBT intervention, they are not necessary to conduct social training. Therefore, the effects of support-workers are probably negligible.
Quality of life of participants
At baseline, participants’ ratings of quality of life (mean = −0.19, SD = 1.8) indicated a general dissatisfaction of life, which is similar to scores of untreated post-traumatic stress disorder (PTSD) patients (mean = 0.3, SD = 3.2) and very low when compared to findings with non-clinical controls (mean = 2.8, SD = 2.3) observed in other studies (Paunović and Öst, 2004). Although the change in QOLI at follow-up was moderate (d = 0.48) and scores at follow-up were still very low (mean = 0.43, SD = 1.73), responses progressed into the ‘satisfied’ range of QOLI. This may indicate an important positive clinical change in quality of life.
As neither of the interventions resulted in improvement of psychiatric symptoms or autistic traits, two observations were made. First, the increase in quality of life probably reflects a meaningful change. It is possible that the increase in quality of life represents spontaneous remission where patients seeking help at crisis point tend to inevitably improve to some extent because they cannot become worse. However, as there was no change in measures of psychiatric health, this explanation is unlikely. In addition, given the different longitudinal findings for the psychiatric measures and the QOLI, improvement in quality of life may not necessarily be connected to a reduction of psychiatric symptoms in patients with ASDs. It is also possible that the lack of effect on psychiatric measures could be caused by low power due to multiple co-morbidities, since not all patients received high scores on each measure. The patient group with a specific psychiatric problem (e.g. depressed, with high scores on BDI) was most likely too small for obtaining satisfactory statistical power. Future studies on treatment of psychiatric symptoms in ASDs should include larger samples to differentiate between patients with specific psychiatric problems in order to increase detectability of treatment effects. Notably, previous studies aimed at specific anxiety symptoms have succeeded in reducing psychiatric symptoms in children and young adults with ASDs with the use of CBT (Lang et al., 2010; Woods et al., 2009).
Factors related to dropout
The total attrition rate (28%) in this study was low, especially considering the length of the treatment (Villeneuve et al., 2010). Lower SoC was associated with a greater likelihood of dropout in both interventions, which is consistent with findings in other patient populations (Andersen and Berg, 2001). Interestingly, the CBT intervention had significantly less dropouts than recreational activity. The requirement of the recreational activity intervention to visit public places may have been perceived as stressful by participants and thereby contributed to the higher attrition rate in this group. When participants needed inpatient care, they could continue attending CBT sessions at the clinic, whereas recreational activities in public were not practical. This was an unexpected advantage of the CBT intervention, which may have lessened the risk of dropout further. In light of this, it is advisable in clinical practice to consider a patients’ likely need for inpatient care when selecting appropriate interventions.
Generalizability of the results
The psychiatric vulnerability of adult psychiatric patients with ASDs was illustrated in this sample by the high prevalence of previous suicide attempts (35%), current psychotropic medication (79%) and previous need of inpatient care (31%). These rates are high when compared to prevalence rates in the general ASD population (Lugnegård et al., 2011). Due to participants’ psychiatric co-morbidities, these findings may not be generalizable to a general ASD population. It is, however, unclear whether adults with ASDs with better general psychiatric health than this sample would benefit less from the interventions. Furthermore, in order for a participant to enter treatment, he or she had to agree to a group setting, possibly excluding those disinterested in social contact (Wing, 1981). Nevertheless, the current sample represents an important psychiatric population who require high-quality, flexible and frequent care.
The limited significant differences observed between the two interventions may have several explanations. Factors common to both treatment conditions (e.g. structure and group setting) are presumed to be beneficial to adults with ASDs. The initial power calculation proved to be too optimistic, since the observed effect sizes were much lower than expected. Thus, there may be differences between groups not detected in this study. To increase power of between-group effects, an untreated waiting-list group or larger sample could have been used. However, waiting-list design was considered unsuitable because the treatment length (two semesters) meant that severely ill patients would be left untreated for too long. Sample size was defined at the beginning of the study based on the initial power calculation and could not be altered in retrospect.
The use of manual randomization and primary assessment not being blind to randomization may have increased the risk of falsely identifying between group effects. However, no difference was found between groups regarding baseline measures or demographic data, hence a type I error is unlikely.
Methodological discussion
This study’s main strength is the development and evaluation of two interventions suitable for a patient group who have very few treatment options, and yet have a great need for diverse and high-quality interventions. The study’s limitations were largely due to the naturalistic setting and the specific difficulties of measuring psychiatric health in patients with multiple and complex symptoms.
The exclusive use of self-reports as outcome measures is a limitation. However, alternative methods to self-reports were not used because they were considered unsuitable for the current study. For example, therapist ratings were unsuitable because tone of voice, facial expression or body language may not provide any clues of how a person with ASD feels (Wing, 1981). Another approach for assessing intervention effects could have been to collect information from family members or caregivers. However, for adults living independently and suffering from social impairment, family members or caregivers are not always available, and furthermore, adult participants could view such involvement as intrusive. Using multiple outcome methods, such as blind clinician raters, would strengthen future research.
The ability to complete self-assessments was not a requirement for inclusion, which resulted in a considerable amount of missing data. Also, the measurements at baseline and post-treatment were not adapted to the patient population. In consideration of these limitations, the follow-up questionnaire was constructed to reduce the likelihood of missing data and better suit the ASD population, with fewer items to answer and more direct questions. As a result of the follow-up questionnaire being constructed and distributed after intervention termination, there is a possibility that question-bias may have affected the validity of the follow-up. However, due to participants’ impairment in communication and need for direct questions, rather than lengthy questionnaires, this was deemed appropriate.
In order to ensure intervention adherence and quality, this study used professional supervision and overlapping therapists. Furthermore, the CBT intervention was defined by a very detailed treatment manual. The recreational activity intervention was designed to be a low impact and easily organized intervention, and minimal instructions were given to therapists. Although this study lacks a general measurement of treatment adherence, the above measures were taken to maximize treatment quality and adherence.
Conclusion
This study addressed the shortage of treatment options for adults with ASDs, showing that group CBT and group recreational activity interventions are beneficial treatment options. Both interventions are suggested to be beneficial for this patient group because each intervention was associated with a sustained improvement in quality of life. This highlights the benefits of structure and group setting in treating this population. Due to the range of ASD-suitable techniques available in CBT, this method may be additionally beneficial in terms of increasing specific skills and minimizing dropout. Clinicians may find a combination of these interventions useful, depending on individual patients’ preferences and challenges. Social isolation is common in this population, and for patients reluctant to enter psychotherapy, a recreational activity group may be a possible treatment option.
In conclusion, this study demonstrates that adults with ASDs can attend group interventions and that this may improve their self-perceived quality of life and psychological well-being. It contributes towards the development of treatment options for adults with ASD, widening the range of appropriate treatment alternatives currently available to clinicians and patients. Further research using larger population samples and multi-method outcome measures are needed to further assess the validity and efficacy of both methods presented in this preliminary study.
Acknowledgments
Collaborators responsible for the content in the treatment sessions were Susanne Bejerot, Eva Björnstjerna, Susanna Bitter, Anna Martin, Maritta Reijonen and Gunilla Björk. The authors wish to express their gratitude towards the patients who participated in the study. We also warmly thank Mia Fahlén and Erik Truedsson for assistance.
Appendix 1
Session plan
Introduction and pre-treatment measurements
Presentation of participants and curriculum
What is autism?
How does your autism affect you?
Change and individual goals I
Ethics, boundaries and acceptance
Behaviour change
Problem-solving
Coping with stress and sleeping disturbances
Applied relaxation and mindfulness
Diet and exercise
Living situation and cognitive aids
Legislation and rights
Non-governmental organizations (NGOs) and patient organizations for people with autism
Different experiences of sensation
Compulsions, obsessions and rituals
Depression and social anxiety I
Depression and social anxiety II
Work and occupation I – what does it take and what does it give?
Work and occupation II – social skills
Living and housing support I
Living and housing support II – difficult situations
Change and individual goals II
Social stories I
Mentalisation and central coherence I
Mentalisation and central coherence II
Social stories II
Relationships with friends and family
Affect, emotion and body language
Love and romantic relationships
Mind traps and cognitive distortions
Change and individual goals III – telephone and e-mail
Social interaction I
Social interaction II
Social interaction III
Final session – closing remarks and post-treatment measurement
Footnotes
Funding: This work was supported by L.J. Boëthius’ Foundation, The Swedish National Board of Health and Welfare, Swedish Research Council (grant number 523-2011-3646) and the regional agreement on medical training and clinical research (ALF) between the Stockholm County Council and the Karolinska Institutet.
References
- American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). 4th ed., text rev. Washington, DC: American Psychiatric Association. [Google Scholar]
- Andersen S, Berg JE. (2001) The use of a sense of coherence test to predict drop-out and mortality after residential treatment of substance abuse. Addiction Research & Theory 9(3): 239–251. [Google Scholar]
- Antonovsky A. (1993) The structure and properties of the Sense of Coherence Scale. Social Science & Medicine 36(6): 725–733. [DOI] [PubMed] [Google Scholar]
- Attwood T. (2007) The Complete Guide to Asperger’s Syndrome. London: Jessica Kingsley Publishers. [Google Scholar]
- Axén M, Brar A, Huslid E, et al. (2010) Regionalt vårdprogram, ADHD, lindrig utvecklingsstörning och autismspektrumtillstånd hos barn, ungdomar och vuxna. Stockholm: Medicinskt Kunskapscentrum, Stockholms Läns Landsting. [Google Scholar]
- Baron-Cohen S, Wheelwright S, Skinner R, et al. (2001) The autism-spectrum quotient (AQ): evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. Journal of Autism and Developmental Disorders 31(1): 5–17. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Ball R, et al. (1996) Comparison of Beck Depression Inventories IA and II in psychiatric outpatients. Journal of Personality Assessment 67(3): 588–597. [DOI] [PubMed] [Google Scholar]
- Bejerot S, Björnstierna E. (2011) Psykopedagogisk behandling för personer med autismspektrumtillstånd och utbildning för boendestödjare. Unpublished manual.
- Bejerot S, Humble MB. (2013) Childhood clumsiness and peer victimization: a case-control study of psychiatric patients. BMC Psychiatry 13: 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billstedt E, Gillberg IC, Gillberg C. (2011) Aspects of quality of life in adults diagnosed with autism in childhood: a population-based study. Autism 15(1): 7–20. [DOI] [PubMed] [Google Scholar]
- Cappadocia MC, Weiss JA, Pepler D. (2012) Bullying experiences among children and youth with autism spectrum disorders. Journal of Autism and Developmental Disorders 42(2): 266–277. [DOI] [PubMed] [Google Scholar]
- Derogatis LB, Cleary PA. (1977) Confirmation of the dimensional structure of the SCL-90: a study in construct validation. Journal of Clinical Psychology 33(4): 981–990. [Google Scholar]
- Frankel F, Myatt R, Sugar C, et al. (2010) A randomized controlled study of parent-assisted children’s friendship training with children having autism spectrum disorders. Journal of Autism and Developmental Disorders 40(7): 827–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisch MB, Cornell J, Villanueva M, et al. (1992) Clinical validation of the Quality of Life Inventory. A measure of life satisfaction for use in treatment planning and outcome assessment. Psychological Assessment 4(1): 92–101. [Google Scholar]
- Frith U. (2004) Emanuel Miller lecture: confusions and controversies about Asperger syndrome. Journal of Child Psychology and Psychiatry and Allied Disciplines 45(4): 672–686. [DOI] [PubMed] [Google Scholar]
- Gantman A, Kapp SK, Orenski K, et al. (2012) Social skills training for young adults with high-functioning autism spectrum disorders: a randomized controlled pilot study. Journal of Autism and Developmental Disorders 42(6): 1094–1103. [DOI] [PubMed] [Google Scholar]
- Garety PA, Fowler DG, Freeman D, et al. (2008) Cognitive–behavioural therapy and family intervention for relapse prevention and symptom reduction in psychosis: randomised controlled trial. British Journal of Psychiatry 192(6): 412–423. [DOI] [PubMed] [Google Scholar]
- Gaus VL. (2007) Cognitive–Behavioral Therapy for Adult Asperger Syndrome. New York: Guilford Press. [Google Scholar]
- Gaus VL. (2011) Adult Asperger syndrome and the utility of cognitive-behavioral therapy. Journal of Contemporary Psychotherapy 41: 47–56. [Google Scholar]
- Gerhardt PF, Lainer I. (2010) Addressing the needs of adolescents and adults with autism: a crisis on the horizon. Journal of Contemporary Psychotherapy 41(1): 37–45. [Google Scholar]
- Guy W. (1976) ECDEU Assessment Manual for Psychopharmacology–Revised (DHEW Publ No. ADM 76-338). Rockville, MD: US Department of Health, Education, and Welfare, pp.218–222. [Google Scholar]
- Hillier AJ, Fish T, Siegel JH, et al. (2011) Social and vocational skills training reduces self-reported anxiety and depression among young adults on the autism spectrum. Journal of Developmental and Physical Disabilities 23(3): 267–276. [Google Scholar]
- Jennes-Coussens M, Magill-Evans J, Koning C. (2006) The quality of life of young men with Asperger syndrome: a brief report. Autism 10(4): 403–414. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Ames M, et al. (2005) The World Health Organization adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychological Medicine 35(2): 245–256. [DOI] [PubMed] [Google Scholar]
- Kopp S, Beckung E, Gillberg C. (2010) Developmental coordination disorder and other motor control problems in girls with autism spectrum disorder and/or attention-deficit/hyperactivity disorder. Research in Developmental Disabilities 31(2): 350–361. [DOI] [PubMed] [Google Scholar]
- Lang R, Regester A, Lauderdale S, et al. (2010) Treatment of anxiety in autism spectrum disorders using cognitive behaviour therapy: a systematic review. Developmental Neurorehabilitation 13(1): 53–63. [DOI] [PubMed] [Google Scholar]
- Linehan M. (1984) Dialectical Behavior Therapy for Treatment of Parasuicidal Women: Treatment Manual. Seattle, WA: University of Washington. [Google Scholar]
- Lord C, Risi S, Lambrecht L, et al. (2000) The Autism Diagnostic Observation Schedule–Generic: a standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders 30(3): 205–223. [PubMed] [Google Scholar]
- Lugnegård T, Hallerbäck MU, Gillberg C. (2011) Psychiatric comorbidity in young adults with a clinical diagnosis of Asperger syndrome. Research in Developmental Disabilities 32(5): 1910–1917. [DOI] [PubMed] [Google Scholar]
- Minshew NJ, Hobson JA. (2008) Sensory sensitivities and performance on sensory perceptual tasks in high-functioning individuals with autism. Journal of Autism and Developmental Disorders 38(8): 1485–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munro JD. (2010) An integrated model of psychotherapy for teens and adults with Asperger syndrome. Journal of Systemic Therapies 29(3): 82–96. [Google Scholar]
- Myers SM, Plauché Johnson C. (2007) Management of children with autism spectrum disorders. Pediatrics 120(5): 1162–1182. [DOI] [PubMed] [Google Scholar]
- Nylander L, Gillberg C. (2001) Screening for autism spectrum disorders in adult psychiatric out-patients: a preliminary report. Acta Psychiatrica Scandinavica 103(6): 428–434. [DOI] [PubMed] [Google Scholar]
- Palmen A, Didden R, Korzilius H. (2011) An outpatient group training programme for improving leisure lifestyle in high-functioning young adults with ASD: a pilot study. Developmental Neurorehabilitation 14(5): 297–309. [DOI] [PubMed] [Google Scholar]
- Paunović N, Öst L-G. (2004) Clinical validation of the Swedish version of the Quality of Life Inventory in crime victims with posttraumatic stress disorder and a nonclinical sample. Journal of Psychopathology and Behavioral Assessment 26(1): 15–21. [Google Scholar]
- Rosenberg M. (1962) The association between self-esteem and anxiety. Journal of Psychiatric Research 1: 135–152. [DOI] [PubMed] [Google Scholar]
- Rydén E, Bejerot S. (2008) Autism spectrum disorders in an adult psychiatric population. A naturalistic cross-sectional controlled study. Clinical Neuropsychiatry 5(1): 13–21. [Google Scholar]
- Shattuck PT, Seltzer MM, Greenberg JS, et al. (2007) Change in autism symptoms and maladaptive behaviors in adolescents and adults with an autism spectrum disorder. Journal of Autism and Developmental Disorders 37(9): 1735–1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung M, Ooi YP, Goh TJ, et al. (2011) Effects of cognitive-behavioral therapy on anxiety in children with autism spectrum disorders: a randomized controlled trial. Child Psychiatry & Human Development 42(6): 634–649. [DOI] [PubMed] [Google Scholar]
- Tantam D. (2000) Psychological disorder in adolescents and adults with Asperger syndrome. Autism 4(1): 47–62. [Google Scholar]
- Villeneuve K, Potvin S, Lesage A, et al. (2010) Meta-analysis of rates of drop-out from psychosocial treatment among persons with schizophrenia spectrum disorder. Schizophrenia Research 121(1–3): 266–270. [DOI] [PubMed] [Google Scholar]
- Virués-Ortega J. (2010) Applied behavior analytic intervention for autism in early childhood: meta-analysis, meta-regression and dose-response meta-analysis of multiple outcomes. Clinical Psychology Review 30(4): 387–399. [DOI] [PubMed] [Google Scholar]
- Vlachou M, Andreou E, Botsoglou K, et al. (2011) Bully/victim problems among preschool children: a review of current research evidence. Educational Psychology Review 23(3): 329–358. [Google Scholar]
- Weiss JA, Lunsky Y. (2010) Report behaviour therapy for adults with Asperger syndrome and anxiety or mood disorder: a case series. Clinical Psychology 446(May): 438–446. [DOI] [PubMed] [Google Scholar]
- White SW, Koenig K, Scahill L. (2010) Group social skills instruction for adolescents with high-functioning autism spectrum disorders. Focus on Autism and Other Developmental Disabilities 25(4): 209–219. [Google Scholar]
- Wing L. (1981) Asperger’s syndrome: a clinical account. Psychological Medicine 11: 115–129. [DOI] [PubMed] [Google Scholar]
- Wink LK, Erickson CA, McDougle CJ. (2010) Pharmacologic treatment of behavioral symptoms associated with autism and other pervasive developmental disorders. Current Treatment Options in Neurology 12(6): 529–538. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Drahota A, Sze K, et al. (2009) Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: a randomized, controlled trial. Journal of Child Psychology and Psychiatry 50(3): 224–234. [DOI] [PMC free article] [PubMed] [Google Scholar]