Abstract
Objective
Patient activation questions from a major national Medicare survey are used to highlight characteristics of Medicare beneficiaries with low activation. We demonstrate that Medicare Current Beneficiary Survey (MCBS) data is an untapped resource for further research on patient activation within Medicare beneficiaries and programs.
Data source
Data are from the 2012 MCBS Access to Care file and include 10,650 beneficiaries.
Methods
Patient Activation levels were derived by taking the weighted average responses to the Patient Activation Supplement. Cut points for high, moderate, and low activation were assigned at +/– ½ standard deviation of the mean. Data were analyzed using SAS survey procedures. Within group comparisons were tested using chi-square tests with post hoc pairwise comparisons. Logistic regression identified predictors of low patient engagement.
Results
In a multiple logistic regression, beneficiary characteristics associated with low activation included Hispanic origin, being widowed or never married, select age groups, male gender, fair or poor health, difficulty with an IADL or ADLs, and having no usual source of care, with failure to complete high school as the strongest predictor (OR=2.22, p<.001). Utilization and costs were also examined in descriptive analyses
Discussion
Overall, findings on the characteristics of low activation patients in the Medicare population resemble previous research. In a regression analysis, less education and no usual source of care are the strongest predictors of low activation levels in Medicare beneficiaries. The MCBS Patient Activation Supplement is a rich resource for examining patient activation in the Medicare population, and can be used for a wide range of analyses.
Keywords: Medicare, access, demand, utilization of services, aging, elderly, geriatrics, health care costs
Introduction
Patient-centered care, including an emphasis on patient engagement and activation, is being pushed to the forefront of health policy in part due to the Affordable Care Act (Millenson & Macri, 2012). Patient engagement is characterized as actions that individuals must take to obtain the greatest benefit from the health care services available to them (Center for Advancing Health, 2010) or, more generally, the relationship between patients and health care providers as active patient involvement in healthcare is promoted (Coulter, 2011). Patient activation is a component of patient engagement, focusing specifically on the patient’s understanding of his or her role in the care process and empowering the patient with the knowledge, skills, and confidence to manage his or her care (Hibbard, Stockard, Mahoney, & Tusler, 2004; Carman et al., 2013; Hibbard, Greene, & Overton, 2013; Cunningham, Hibbard, & Gibbons, 2011; Hibbard & Greene, 2013; Hibbard & Mahoney, 2010).
In today’s health care environment, it may be insufficient for a patient to be discharged from outpatient surgery with instructions for recovery and prescription medications. The patient should (a) have confidence in their ability to understand their doctor’s instructions and to know when they should seek further medical care, (b) feel they can effectively communicate with their doctor, and (c) have the ability and motivation to educate themselves or seek more information on health care (such as medical conditions, symptoms, treatments, and test results), all of which would indicate high patient activation. The success of health care reform-related programs and initiatives in Medicare, such as patient centered care, the Chronic Care Model (Wagner et al., 2001), and medical homes, may ride on how involved patients are in their own health care. The usefulness of public reporting initiatives comparing quality of health plans, hospitals, and other health facilities depends on a patient’s ability and motivation to interact with health care as a more involved and educated consumer.
Studies in the adult population have linked high patient activation levels to better health outcomes, better patient experiences, and lower costs (Hibbard et al., 2004; Nease, Frazee, Zarin, & Miller, 2013; Hibbard et al., 2013; Greene & Hibbard, 2012). Patient activation tends to be higher among those with higher educational attainment, private health insurance, better overall health, and in younger age groups (Hibbard & Cunningham, 2008), but increasing activation is a potential mechanism to reduce racial and ethnic disparities in health outcomes (Cunningham et al., 2011; Hibbard et al., 2008) as well as improve self-management health behaviors (Hibbard, Mahoney, Stock, & Tusler, 2007). Growing literature on the topic of patient activation has demonstrated the association between high activation with both a higher quality of care and reduced health care costs (Greene & Hibbard, 2012). If interventions can be targeted to increase patient activation, the U.S. health care system may move towards achieving the “Triple Aim” of improved experience of care, improved health of populations, and reduced health care costs (Berwick, Nolan, & Whittington, 2008).
Many studies of patient activation have included the chronically ill community (Maeng, Martsolf, Scanlon, & Christianson, 2012; Alexander, Hearld, Mittler, & Harvey, 2012; Wong, Peterson, & Black, 2011), and most studies of patient activation among the elderly focus on small samples of older adults managing multiple comorbidities (Chubak et al., 2012; Skolasky et al., 2011; Ryvicker, Peng, & Feldman, 2012; Allen et al., 2012). However, focused studies and reporting on patient activation among Medicare-covered beneficiaries1 has been limited. The Patient Activation Supplement of the Medicare Current Beneficiary Survey (MCBS) serves as a rich resource for exploring patient activation via a nationally representative survey of Medicare beneficiaries, but only a few studies have utilized this resource (Tarn, Young, & Craig, 2012; Butler, Farley, Sleath, Murray, & Maciejewski, 2012). This data brief is intended to highlight a few of the potential research uses of the MCBS Patient Activation Supplement.
Data Source and Methods
The MCBS is a continuous, in-person, nationally representative survey of approximately 15,000 beneficiaries. Data can be used for either cross-sectional or longitudinal analyses, as rotating panels are followed for a period of four years. The findings reported in this brief were based on self-reported survey data collected in the 2012 Access to Care file (fielded in Fall 2012) and the Patient Activation Supplement2 (fielded in Summer 2013).
Inclusion criteria for the MCBS require that respondents be current Medicare beneficiaries residing in the United States at the time of the interview. While the MCBS does include an institutionalized population (in health care facilities) and allows proxy respondents for community respondents in poor health, the Patient Activation Supplement requires self-reported beneficiary responses.
The key analytic variables used in this study were derived from the MCBS Patient Activation Supplement of 16 questions (see Appendix A), completed by 10,680 survey participants. Patient activation is often measured via the Patient Activation Measure, or PAM (Hibbard et al., 2004). The MCBS Patient Activation Supplement does not use the PAM, but its items are conceptually similar. The items were designed to capture the following domains of patient activation: confidence, communication, and information seeking. An example of a confidence question is: “How confident are you that you can follow instructions to care for yourself at home?” The information seeking section contains questions such as: “Do you make sure you understand the results of any medical test or procedure?”
A composite activation level was derived for beneficiaries who responded to at least 50% of the questions. Thirty survey participants had “Don’t Know,” “Refused,” “Not Ascertained,” or “Inapplicable” responses for at least half of the scale items and were removed, resulting in 10,650 participants included in this analysis. Due to the exclusion of proxy respondents for the Patient Activation Supplement, adjusted survey weights were created to generalize estimates to the Medicare population.3 With the survey weights, this sample represents 40,729,409 Medicare beneficiaries.
Cut points for high, moderate, and low activation were assigned at +/– ½ standard deviation of the unweighted mean for each question set. The unweighted score was used to determine the cut points as the distribution did not differ from the weighted scores. Sensitivity analyses included altering the survey response thresholds and the activation cut points. For more details on how the scale was created, see Appendix B. Summary scores from the supplement have been used in other research to assign levels of patient activation (Butler et al., 2012), and our method of scale creation is similar to the method demonstrated by Hibbard and Cunningham (2008).
Data were analyzed using SAS survey procedures, which take into account the complex survey design of the MCBS in reporting standard errors. Activation levels were first described across sociodemographic characteristics. Next, exploratory data analysis for the model included univariate logistic regression for all variables under consideration for the model. Missing data on covariates was less than 1% for each variable and so an “all available” data analysis was utilized, resulting in 10,512 beneficiaries included in the model, representing 40.2 million beneficiaries with the use of the cross-sectional weights. The outcome of interest was low patient activation, defined by a patient activation score under ½ standard deviation of the mean. Multicollinearity among predictor variables was assessed by fitting a multiple linear regression model and obtaining the variance inflation factor. Several models were fit and assessed using Akaike’s Information Criteria (AIC). Final covariates in the weighted model included Medicaid eligibility, marital status, education level, race, sex, age, self-reported health status, number of functional limitations measured by self-reported difficulty with activities of daily living (ADLs), and usual place of health care. Influence diagnostics, including plots of Pearson residuals and leverage, were used to identify potential influential data points. Deletion of these observations resulted in no noticeable change to model coefficients; therefore, the observations were retained. Goodness of fit was assessed using the Hosmer-Lemeshow test and indicated good fit.
Lastly, mean service utilization and costs were compared across activation levels. Cost and utilization data was only available for the fee-for-service (FFS) population of 7,370 survey participants who completed the supplement, representing 28,326,423 Medicare beneficiaries. Within group comparisons of high activation and moderate activation versus low activation were tested using chi-square tests with post hoc pairwise comparisons, with a Dunnett adjustment.
Results
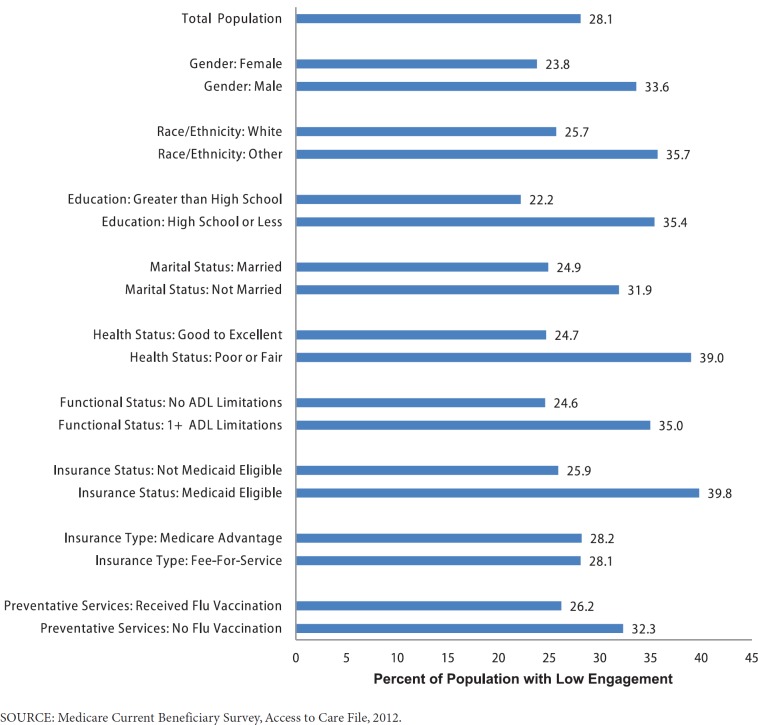
Exhibit 1 displays levels of activation in the 2012 Medicare population,4 as defined by our data-driven, post hoc cut points. The smallest group was the low activation group (28.1%), with 33.8% of beneficiaries at high activation levels.
Exhibit 1. Distribution of Overall Patient Activation Composite Scores.
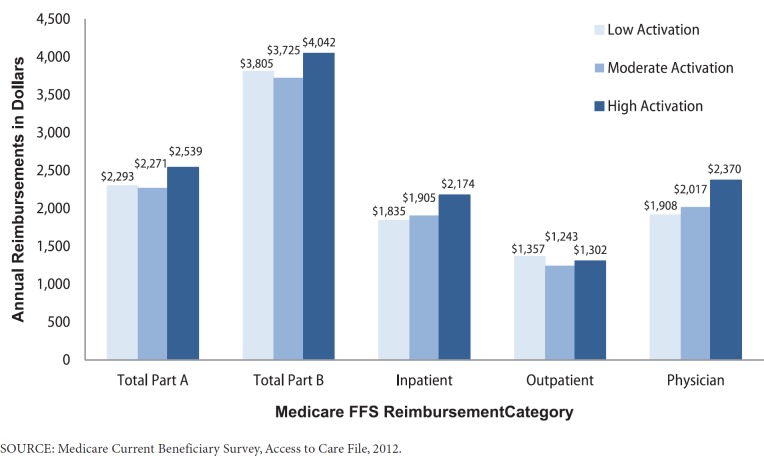
MCBS data shows that certain demographic characteristics are associated with low activation (Exhibit 2). The prevalence of lower activation was higher among beneficiaries who were male (33.6%), minority race (35.7%), had a high school education or less (35.4%), unmarried status (31.9%), fair or poor health (39.0%), low functional status demonstrated through difficulty with ADLs (35.0%), were Medicaid eligible (39.8%), or did not get the flu vaccine (32.3%). There was no notable difference in the prevalence of low activation between beneficiaries in Medicare Advantage compared to those in FFS.
Exhibit 2. Levels of Low Activation by Select Demographic Characteristics.
Similar relationships were found in a logistic regression predicting low patient activation by beneficiary characteristics (Exhibit 3). A marital status of never married (adjusted OR=1.71, p<.001) or widowed (adjusted OR=1.24, p<.001) was associated with low activation, compared to those who were married. Beneficiaries with less than a high school education were more than two times as likely (adjusted OR=2.22, p<.001) as those with a college degree to have low activation, while those with a high school degree were nearly twice as likely (adjusted OR=1.72, p<.001). Race was associated with low activation when comparing Hispanics to Non-Hispanic Whites (adjusted OR=1.63, p<.001), but it was not a statistically significant factor when comparing Non-Hispanic Blacks to Non-Hispanic Whites.
Exhibit 3. Adjusted Odds Ratios for Low Patient Activation.
| OR | 95% CI | p-value | |||
|---|---|---|---|---|---|
| Medicaid Eligible | |||||
| No (ref.) | 1.00 | — | — | ||
| Yes | 1.12 | (0.99, 1.27) | .083 | ||
| Marital Status | |||||
| Married (ref.) | 1.00 | — | — | ||
| Divorced/Separated | 1.11 | (0.97, 1.26) | .125 | ||
| Never Married | 1.71 | (1.44, 2.02) | <.001 | ||
| Widowed | 1.24 | (1.13, 1.36) | <.001 | ||
| Education | |||||
| College Degree or Greater (ref.) | 1.00 | — | — | ||
| Less than High School | 2.22 | (1.97, 2.50) | <.001 | ||
| High School Degree | 1.72 | (1.53, 1.93) | <.001 | ||
| Some College or Vocational Degree | 1.25 | (1.11, 1.41) | <.001 | ||
| Race | |||||
| Non-Hispanic White (ref.) | 1.00 | — | — | ||
| Non-Hispanic Black | 0.90 | (0.80, 1.03) | .126 | ||
| Hispanic | 1.63 | (1.38, 1.91) | <.001 | ||
| Other | 1.28 | (1.07, 1.53) | .002 | ||
| Sex | |||||
| Female | 1.00 | — | — | ||
| Male | 1.86 | (1.70, 2.03) | <.001 | ||
| Age | |||||
| 65–74 years old (ref.) | 1.00 | — | — | ||
| Less than 65 years old | 1.18 | (1.01, 1.37) | .034 | ||
| 75–84 years old | 1.19 | (1.09, 1.30) | <.001 | ||
| 85 years old or greater | 1.65 | (1.47, 1.85) | <.001 | ||
| Self-reported health status | |||||
| Good, Very Good, or Excellent (ref.) | 1.00 | — | — | ||
| Fair or Poor | 1.37 | (1.25, 1.51) | <.001 | ||
| No ADLs (ref.) | 1.00 | ||||
| IADL Only | 1.32 | (1.19, 1.48) | <.001 | ||
| 1 or 2 ADLs | 1.39 | (1.27, 1.52) | <.001 | ||
| 3 + ADL s | 1.32 | (1.13, 1.54) | <.001 | ||
| Usual Source of Care | |||||
| Doctor Office, Clinic or HMO (ref.) | 1.00 | — | — | ||
| Hospital OPD/ER | 1.07 | (0.84, 1.37) | .572 | ||
| Other | 1.35 | (1.16, 1.57) | <.001 | ||
| None | 2.20 | (1.82, 2.67) | <.001 | ||
SOURCE: Medicare Current Beneficiary Survey, Access to Care File, 2012.
Men were more likely than women to have low activation (adjusted OR=1.86, p<.001). Beneficiaries in the under 65 age group (adjusted OR=1.18, p=.034), the 75–84 age group (adjusted OR=1.19, p<.001), or the 85 and older age group (adjusted OR=1.65, p<.001) were more likely to have low activation compared to those in the 65–74 year age group.
Fair or poor health was associated with low activation (adjusted OR=1.37, p=.001), as was having an IADL (adjusted OR=1.32, p<.001), one or two ADLs (adjusted OR=1.39, p=.001), or three or more ADLs (adjusted OR=1.32, p<.001). Having no usual source of care was a strong predictor of low activation (adjusted OR=2.20, p<.001), compared to usually getting care through a doctor’s office or clinic.
Service utilization for moderate and high activation beneficiaries was compared to low activation beneficiaries among the FFS population using pairwise comparisons (Exhibit 4). Inpatient stays did not differ significantly. Moderate and high activation beneficiaries had a significantly higher mean number of office visits (4.82 and 4.96, respectively) compared to low activation beneficiaries (4.18). The opposite pattern is found in utilization of home health agencies, with average visits of 1.27 for moderate activation beneficiaries and 1.08 for high activation beneficiaries, compared to an average of 2.30 visits for low activation beneficiaries, a significant difference. Number of outpatient visits, represented by a count of outpatient bills, was not significantly associated with higher activation levels, with a mean number of 2.84 bills for low activation, 2.65 for moderate activation, and 2.76 for high activation patients.
Exhibit 4. 2012 Service Utilization Among FFS Beneficiaries, By Activation Level.
| Low | Moderate | High | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | ||||
| Inpatient Stays | 0.15 | 0.01 | 0.15 | 0.01 | 0.14 | 0.01 | |||
| Office Visits | 4.18 | 0.10 | 4.82* | 0.10 | 4.96* | 0.09 | |||
| HHA Visits | 2.30 | 0.35 | 1.27* | 0.11 | 1.08* | 0.10 | |||
| Outpatient Bills | 2.84 | 0.10 | 2.65 | 0.07 | 2.76 | 0.08 | |||
NOTES:
Pairwise comparisons (moderate and high activation versus low) with Dunnett adjustment.
Significance at p-value<.05.
SOURCE: Medicare Current Beneficiary Survey, Access to Care File, 2012.
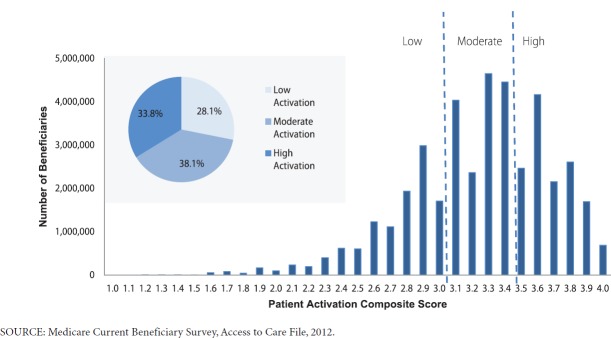
Lastly, the relationship between Medicare reimbursement costs and activation level was examined in a descriptive analysis among the FFS population (Exhibit 5). Total Part A,5 and total Part B,6 inpatient and outpatient costs do not vary significantly across activation level. High activation beneficiaries have physician costs that are higher than the average costs for low activation beneficiaries. Exhibit C1 in Appendix C contains detailed results.
Exhibit 5. Average Reimbursement by Activation Level in the FFS Population.
Discussion
In general, findings on the characteristics of low activation Medicare beneficiaries are consistent with previous research that has focused on the overall adult population (Hibbard & Cunningham, 2008). In bivariate descriptive analyses, low activation was higher in beneficiaries with fair or poor health status, low functional status, minority race, and less education. In short, Medicare beneficiaries in traditionally underserved populations are more likely to lack the knowledge, skills, and confidence necessary to manage their own medical care. A multivariate logistic regression predicting low activation supported this conclusion. Controlling for other demographic variables, the strongest predictors of low activation included low educational attainment and not having a usual source of care. When examining average utilization and costs in the FFS population, high activation patients have higher physician costs. Low activation patients appear to get more treatment in an inpatient setting while high activation patients get more treatment in the physician setting.
It should be noted that the relationship between health status and patient activation is potentially multidirectional. Sicker individuals may be physically unable to take an active role in their health care, or they may be more likely to manage their own care out of necessity due to their complex needs. They may be unwell due in part to their low activation levels and resultant poor health care, or they may have low activation levels due to their poor health and physical limitations. Exploring this relationship is beyond the scope of this study.
There are a number of key policy questions related to patient activation and the data presented in this brief: What can be done to increase activation in the least engaged groups? What is the impact of low activation patients on costs and health outcomes? In which settings or environments are better decisions made? What impact does activation by itself have on disparities in quality of care? What are Medicare programs doing to target the populations with lower activation? Future research should investigate more recent Medicare program efforts (such as Accountable Care Organizations and Medical Homes) towards increasing activation in the Medicare population and whether the outcomes of these efforts are leading to increases in quality and decreases in costs. Programs such as the Blue Button Initiative, which enables beneficiaries to download their own health records from a website, have the potential to increase patient activation through greater sharing of information.
This analysis has several limitations that are worth noting. To start, the cross-sectional nature of the analysis limits inferences regarding temporality when predicting low patient activation. We cannot deduce from this analysis, for example, whether poor health status predates low patient activation, or is an outcome from it, or if the relationship is multidirectional. This study used self-reported data, and cost data is only available for the fee-for-service population. Similarly, this study’s generalizability is limited as the survey population was restricted to the non-institutionalized Medicare population that was healthy enough to self-report. All questions in the patient activation scale are weighted equally, when in fact certain questions may be stronger predictors of activation than others. Although the patient activation scale has not been externally validated, survey questions are consistent with previous studies and a sensitivity analysis raised no concerns. Further research on MCBS patient activation questions could address some of these limitations and also demonstrate any correlation with the PAM.
This study demonstrates an underutilized portion of a major Medicare survey that could prove to be of significant value to health services researchers and policy analysts. The MCBS content and sample size are significant and, while this study provides an initial dive into the subject of patient activation, there are many areas pertaining to this topic of research that can be refined and advanced upon by future MCBS users.
The MCBS Patient Activation Supplement was first introduced as part of the MCBS in Fall 2001 and consists of three domains identified through principal component factor analysis: (1) confidence in their ability to navigate their health care, (2) communication in health care settings, and (3) knowledge-seeking behavior about health. Analyses can be done on individual domains or on a composite measure combining the three domains. The multipurpose nature of the MCBS allows users to access data that are not available in working with other data sources, such as linked survey and administrative data in the MCBS files and longitudinal applications.
In summary, the MCBS Patient Activation Supplement is a rich resource for examining patient activation in the Medicare population and can be used for a wide range of analyses. Examples of possible analyses that can be done with the MCBS include examining demographic and health characteristics of low activation patients, exploring the association between patient activation and cost and utilization, or further validation of the patient activation scale.
Disclaimer
The authors have been requested to report any funding sources and other affiliations that may represent a conflict of interest. The authors reported that there are no conflict of interest sources. The views expressed in this article are those of the authors and do not represent official policy of the Department of Health and Human Services.
Acknowledgement
The authors would like to acknowledge Kim Lochner, Paul Guerino, and Gerry Adler for their contributions to this manuscript.
Appendices
Appendix A. Patient Engagement Questions, by Domain.
| Confidence | |||
| PAINSTRC | How confident are you that you can follow instructions to care for yourself at home? | ||
| PAMEDREC | How confident are you that you can follow this kind of instruction, to change your habits or lifestyle? | ||
| PANECESS | Please tell me how confident are you that you can identify when it is necessary for you to get medical care. | ||
| PASIDEFX | How confident are you that you can identify when you are having side effects from your medications? | ||
| Communication | |||
| PAANSWR | Do you … leave your doctor’s office feeling that all of your concerns or questions have been fully answered? | ||
| PADREXPL | My doctor explains things to me in terms that I can easily understand. | ||
| PADRLISN | My doctor listens to what I have to say about my symptoms and concerns. | ||
| PADVICE | I can call my doctor’s office to get medical advice when I need it. | ||
| Information Seeking | |||
| PADRQUEX | Do you … bring with you to your doctor visits a list of questions or concerns you want to cover? | ||
| PAHCONDS | Do you … read about health conditions in newspapers, magazines, or on the internet? | ||
| PALISTRX | Do you … take a list of all of your prescribed medicines to your doctor visits? | ||
| PAOPTION | Do you … talk with your doctor or other medical person about your options if you need tests or follow-up care? | ||
| PARXINFO | Do you … read information about a new prescription, such as side effects and precautions? | ||
| PATRSLT | Do you … make sure you understand the results of any medical test or procedure? | ||
| Other Questions | |||
| PACHGDRS | How likely are you to change doctors if you are dissatisfied with the way you and your doctor communicate? | ||
| PADISAGR | How likely are you to tell your doctor when you disagree with him or her? | ||
Appendix B. Creating Scale from the Patient Activation Questionnaire, MCBS Access to Care
The patient activation scale was developed using methods similar to Hibbard and Cunningham (2008), and is outlined below:
The scale of each questionnaire response is reversed so that a higher number is an indication of more patient engagement.
Responses with a value of “don’t know,” “refused,” “not ascertained,” or “inapplicable” are given a score of 0.
SP’s with a value of “don’t know,” “refused,” “not ascertained,” or “inapplicable,” on half or more of the variables of each scale are dropped from the analysis. This removed 30 beneficiaries.
To construct the scale, a raw score is summed from the responses in each scale, and the weighted score is obtained by dividing the sum of the scores by the number of non-missing items for each beneficiary.
Levels of engagement are determined. Weighted scores below the mean minus one-half of the standard deviation are designated low activation scores, weighted scores above the mean plus one-half of the standard deviation are designated high activation scores, and scores in the middle are designated moderate activation scores.
Appendix C. Average 2012 Service Costs Among FFS Beneficiaries, By Activation Level.
| Low | Moderate | High | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | |||||||
| Total Part A Costs | $2,293 | $138 | $2,271 | $116 | $2,539 | $147 | ||||||
| Total Part B Costs | $3,805 | $114 | $3,725 | $104 | $4,042 | $125 | ||||||
| Inpatient | $1,835 | $121 | $1,905 | $102 | $2,174 | $135 | ||||||
| Outpatient | $1,357 | $69 | $1,243 | $73 | $1,302 | $90 | ||||||
| Physician | $1,908 | $59 | $2,017 | $51 | $2,370* | $68 | ||||||
NOTES:
Pairwise comparisons (moderate and high activation versus low) with Dunnett adjustment.
Significance at p-value<.05.
SOURCE: Medicare Current Beneficiary Survey, Access to Care File, 2012.
Footnotes
While most Medicare beneficiaries receive entitlement due to age (i.e., they are aged 65+), Medicare entitlement may also be obtained due to disability or other chronic conditions (e.g., end stage renal disease). These entitlement scenarios make the Medicare population quite unique when compared to the adult population at large.
Supplements are available for the following years: 2001, 2004, 2009, 2011, 2012, 2013. The supplement excludes facility beneficiaries, proxy reporters, and new Medicare accretes for the year it is administered and so the supplement population does not mirror the Access to Care population.
The weights used in this study were developed by adjusting the standard Access to Care weights to known population counts of the ever-enrolled Medicare population using a technique referred to as ratio-raking and by applying a non-response adjustment to account for proxy non-response to the patient activation questions.
Ever-enrolled, community dwelling and able to self-report activation without proxy.
MCBS calculates Part A costs by totaling Skilled Nursing Facility (SNF), Home Health Agency (HHA), Inpatient, and Hospice reimbursements.
MCBS calculates Part B costs by totaling Outpatient and Physician reimbursements.
References
- Alexander JA, Hearld LR, Mittler JN, Harvey J. Patient-Physician Role Relationships and Patient Activation Among Individuals with Chronic Illness. Health Services Research. 2012;47(3 Pt 1):1201–1223. doi: 10.1111/j.1475-6773.2011.01354.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen KR, Hazelett SE, Radwany S, Ertle D, Fosnight SM, Moore PS. The Promoting Effective Advance Care for Elders (PEACE) Randomized Pilot Study: Theoretical Framework and Study Design. Population Health Management. 2012;15(2):71–77. doi: 10.1089/pop.2011.0004. [DOI] [PubMed] [Google Scholar]
- Berwick DM, Nolan T, Whittington J. The Triple Aim: Care, Health, and Cost. Health Affairs. 2008;27(3):759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- Butler MG, Farley J, Sleath B, Murray M, Maciejewski M. Medicare Part D Information Seeking: The Role of Recognition of Need and Patient Activation. Research in Social & Administrative Pharmacy. 2012;8(5):433–442. doi: 10.1016/j.sapharm.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, Sweeney J. Patient and Family Engagement: A Framework for Understanding the Elements and Developing Interventions and Policies. Health Affairs. 2013;32(2):223–231. doi: 10.1377/hlthaff.2012.1133. [DOI] [PubMed] [Google Scholar]
- Center for Advancing Health. Snapshot of People’s Engagement in their Health Care. 2010 Retrieved from http://www.cfah.org/file/CFAH_Snapshot_2010_Full.pdf.
- Chubak J, Anderson ML, Saunders KW, Hubbard RA, Tuzzio L, Liss DT, Reid RJ. Predictors of 1-Year Change in Patient Activation in Older Adults with Diabetes Mellitus and Heart Disease. Journal of the American Geriatrics Society. 2012;60(7):1316–1321. doi: 10.1111/j.1532-5415.2012.04008.x. [DOI] [PubMed] [Google Scholar]
- Coulter A. Engaging Patients in Healthcare. New York (NY): McGraw-Hill Education; 2011. p. 10. [Google Scholar]
- Cunningham PJ, Hibbard J, Gibbons C. Raising Low ‘Patient Activation’ Rates Among Hispanic Immigrants May Equal Expanded Coverage in Reducing Access Disparities. Health Affairs. 2011;30(10):1888–1894. doi: 10.1377/hlthaff.2009.0805. [DOI] [PubMed] [Google Scholar]
- Greene J, Hibbard J. Why does Patient Activation Matter? An Examination of the Relationship Between Patient Activation and Health Related Outcomes. Journal of General Internal Medicine. 2012;27(5):520–526. doi: 10.1007/s11606-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure. Health Services Research. 2004;39(4 Pt 1):1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard JH, Mahoney E, Stock R, Tusler M. Do Increases in Patient Activation Result in Improved Self-management Behaviors? Health Services Research. 2007;42(4):1443–1463. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard J, Cunningham P. How Engaged Are Consumers in Their Health and Health Care, and Why Does It Matter? Center for Studying Health System Change. 2008;(8) Retrieved from http://hschange.org/CONTENT/1019/1019.pdf. [PubMed] [Google Scholar]
- Hibbard JH, Greene J, Becker ER, Roblin D, Painter MW, Perez DJ, Tusler M. Racial/Ethnic Disparities and Consumer Activation in Health. Health Affairs. 2008;27(5):1442–1453. doi: 10.1377/hlthaff.27.5.1442. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Mahoney E. Toward a Theory of Patient and Consumer Activation. Patient Education and Counseling. 2010;78(3):377–381. doi: 10.1016/j.pec.2009.12.015. [PubMed] [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Greene J, Overton V. Patients with Lower Activation Associated with Higher Costs: Delivery Systems Should Know Their Patients’ ‘Scores’. Health Affairs. 2013;32(2):216–222. doi: 10.1377/hlthaff.2012.1064. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Greene J. What the Evidence Shows about Patient Activation: Better Health Outcomes and Care Experiences; Fewer Data on Costs. Health Affairs. 2013;32(2):207–214. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- Maeng DD, Martsolf G, Scanlon D, Christianson J. Care Coordination for the Chronically Ill: Understanding the Patient’s Perspective. Health Services Research. 2012;47(5):1960–1979. doi: 10.1111/j.1475-6773.2012.01405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millenson M, Macri J. Will the Affordable Care Act Move Patient-Centeredness to Center Stage? Urban Institute, Timely Analysis of Immediate Health Policy Issues. 2012 Mar; Retrieved from http://www.rwjf.org/en/research-publications/find-rwjf-research/2012/03/will-the-affordable-care-act-move-patient-centeredness-to-center.html.
- Nease RF, Frazee SG, Zarin L, Miller SB. Choice Architecture is a Better Strategy than Engaging Patients to Spur Behavior Change. Health Affairs. 2013;32(2):242–249. doi: 10.1377/hlthaff.2012.1075. [DOI] [PubMed] [Google Scholar]
- Ryvicker M, Peng TR, Feldman PH. Patient Activation and Disparate Health Care Outcomes in a Racially Diverse Sample of Chronically Ill Older Adults. Journal of Health Care for the Poor and Underserved. 2012;23(4):1577–1589. doi: 10.1353/hpu.2012.0157. [DOI] [PubMed] [Google Scholar]
- Skolasky RL, Green AF, Scharfstein D, Boult C, Reider L, Wegener ST. Psychometric Properties of the Patient Activation Measure Among Multimorbid Older Adults. Health Services Research. 2011;46(2):457–478. doi: 10.1111/j.1475-6773.2010.01210.x. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarn DM, Young HN, Craig BM. Development of the Patient Approach and Views Toward Healthcare Communication (PAV-COM) Measure Among Older Adults. BMC Health Services Research. 2012;12(289) doi: 10.1186/1472-6963-12-289. http://www.ncbi.nlm.nih.gov/pubmed/22931537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner EH, Austin B, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving Chronic Illness Care: Translating Evidence into Action. Health Affairs. 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- Wong ST, Peterson S, Black C. Patient Activation in Primary Healthcare: A Comparison Between Healthier Individuals and Those With a Chronic Illness. Medical Care. 2011;49(5):469–479. doi: 10.1097/MLR.0b013e31820bf970. [DOI] [PubMed] [Google Scholar]