Abstract
Purpose
Schools are increasingly a part of vaccine provision, because of laws mandating provision of information by schools about vaccination, school entry requirements, and mass vaccination campaigns. We examined preferences for programmatic aspects of voluntary school mass vaccination programs (i.e., “vaccination days”).
Methods
We analyzed data from a national sample of United States parents of adolescent males ages 11–19 years (n = 308) and their sons (n = 216), who completed an online survey in November 2011.
Results
Sons believed that adolescents should be able to get vaccinated without parental consent at a younger age than parents did (p < .001) and were more willing to participate in vaccination days without a parent present (p = .04). Parents perceived school vaccination days to be a more convenient way to get their sons recommended vaccines if they were younger parents, had older adolescent sons, supported laws letting schools share vaccination records with health care providers, or had sons who were previously immunized at school (all p < .05). Parents of older sons were less likely to want their sons’ vaccination records sent home (odds ratio [OR] = .47; 95% confidence interval [CI], .29–.77) or to their sons’ physicians (OR = .61; 95% CI, .37–.98) compared with parents of younger sons, but more likely to prefer their sons’ records be entered in an immunization registry (OR = 1.66; 95% CI, 1.05–2.63).
Conclusions
Sons’ age had an important role in support for vaccination days and preferences for sharing vaccination information with health care professionals. Parents and sons had similar beliefs about vaccination in schools, but the sons’ responses suggested an interest in greater autonomy.
Keywords: Adolescent health, Immunizations, School health, School-located vaccination, School vaccination programs, Mass vaccination
National guidelines for the United States (US) recommend routine vaccination against meningococcus; tetanus, diphtheria, and pertussis (Tdap); and human papillomavirus (HPV) among adolescents ages 11–12 years [1–4]. Healthy People 2020 has set national health targets for immunization coverage of at least 80% among all adolescents for meningococcal and Tdap vaccines and for HPV vaccine among females [5]. Although Healthy People 2020 objectives do not yet reflect the newer national guidelines for HPV vaccination of boys [4], leading authorities in pediatric health encourage routine inoculation of adolescent boys similar to their female counterparts [6,7]. In addition, even though Tdap has reached the national coverage goal and meningococcal soon will, rates vary substantially for these two vaccines by state, ranging from as low as 28% to up to 95% [8]. In contrast, HPV vaccine coverage lags far behind; only 35% of adolescent girls and around 1% of adolescent boys had completed the series in 2011 [8].
Reasons for low vaccine uptake in the US are complex, but include adolescents having fewer preventative care visit than other age groups [9], health care providers not recommending the vaccine [8,10], and missing opportunities for concomitant vaccination [10]. Furthermore, health care use among adolescents differs by sex, with boys seeking fewer preventative care visits as they get older, compared with girls [11]. Because most adolescents attend school [12], providing immunizations in this setting has the potential to increase overall vaccine coverage [13]. Although school health centers have had an important role in providing immunization services across the country, only around 2,000 school health centers exist nationally, providing services to around 6% of all schools [14] and only a fraction of school-going adolescents [15].
As an alternative, mass vaccination programs at schools may be more viable than school health centers, and they had substantial successes in the US and other countries [16–18]. For example, the Centers for Disease Control and Prevention identifies schools as an ideal location to supply catch-up doses to adolescents for hepatitis B. Demonstration projects in California, Louisiana, and Oregon achieved 65% to 78% completion rates for hepatitis B vaccination, a three-dose series to the current dosing schedule for HPV vaccine, among adolescents whose parents gave consent [16]. In the United Kingdom and Australia, school immunization programs achieved 70% to 80% HPV vaccine initiation among adolescent girls [17,18], substantially higher than current HPV vaccine initiation rates in the US.
A growing body of research has found support for schools as a potential site to administer adolescent immunizations among health care professionals [19] and parents [19,20]. Leading professional and government organizations support providing vaccines in alternative settings [13,21], which has the potential to increase vaccination, particularly for those who are at risk of not receiving vaccines through the traditional medical home [22,23]. Most research has focused on provider preferences, barriers to program implementation, or correlates of acceptability [20]. To our knowledge, limited research has explicitly explored parents’ and their adolescent children’s preferences for implementing and conducting these vaccination days. The purposes of our study were to describe parents’ and their adolescent sons’ attitudes toward and preferences for programmatic features of school-located vaccination days and to assess differences in these perceptions between parents and their sons. We also examined parents’ perceived convenience of having their sons receive adolescent vaccines during a school vaccination day.
Methods
Participants
The HPV Immunization in Sons (HIS) study is a longitudinal study of attitudes and health beliefs about HPV vaccination for adolescent males. We provide further detail about the HIS study design and procedures elsewhere [24,25] and briefly here. Parents were members of an existing, online national panel constructed using list-assisted, random-digit dialing, and address-based sampling of US households [26]. In exchange for participation, parents received points from the survey company that they could later redeem for small cash payments. Households without existing Internet access received laptops with Internet service. We obtained parents’ consent for their sons to complete a survey; sons provided assent before participating. The Institutional Review Board at the University of North Carolina at Chapel Hill approved the study.
Parents and their adolescent sons completed baseline surveys online in August and September 2010. In November 2011, the survey company sent e-mails inviting parents (n = 421) who participated in the study at baseline to complete a follow-up survey. Of those, 327 parents (78%) and 228 of their sons (54%) completed follow-up surveys. Data for the present study came from the follow-up survey. We excluded participants from analysis if sons were home schooled (parents, n = 16; sons, n = 9) or parents did not indicate the type of school their sons attended (parents, n = 3; sons, n = 3), which resulted in an analytic sample of 308 parents and 216 sons. Slightly over half of parents who participated in the follow-up survey were female, were <45 years of age, and had at least some college education (Table 1). About half of the sons were ages 11–15 years. Most sons had seen a health care provider for a preventive visit in the past year. Parents who completed follow-up surveys were more likely to have at least some college education and to report a household income of at least $60,000 than were non-respondents (both p < .05) but did not differ on other assessed demographic characteristics [25]. Sons who participated at follow-up were more likely to attend public schools than were sons who did not complete the follow-up survey (p < .05), but participants and non-participants did not differ on any of the other demographic variables examined.
Table 1.
Characteristics of respondents, reported by parents (n = 308)
| n (%) | |
|---|---|
| Parent characteristics | |
| Sex | |
| Female | 159 (52) |
| Male | 149 (48) |
| Age | |
| <45 years | 192 (59) |
| ≥45 years | 135 (41) |
| Race/ethnicity | |
| Non-Hispanic white | 207 (67) |
| Non-Hispanic black | 29 (9) |
| Hispanic | 58 (19) |
| Other race/ethnicity | 14 (5) |
| Education | |
| High school degree or less | 126 (41) |
| Some college or more | 182 (59) |
| Marital status | |
| Divorced, widowed, separated, never married | 65 (21) |
| Married or living with a partner | 243 (79) |
| Son characteristics | |
| Age | |
| 11–15 years | 166 (54) |
| 16–19 years | 142 (46) |
| Saw health care provider in past year | |
| No | 64 (21) |
| Yes | 243 (79) |
| Ever received vaccines at school | |
| No | 255 (83) |
| Yes | 43 (14) |
| Do not know | 10 (3) |
| Type of school attending | |
| Public school | 276 (90) |
| Private school | 32 (10) |
| Household characteristics | |
| Annual household income | |
| <$60,000 | 141 (46) |
| ≥$60,000 | 167 (54) |
| Urbanicity | |
| Rural | 48 (16) |
| Urban | 260 (84) |
| Region of residence | |
| West | 62 (20) |
| Midwest | 77 (25) |
| Northeast | 64 (21) |
| South | 105 (34) |
Measures
The parent and son surveys (accessible at http://www.unc.edu/~ntbrewer/hpv.htm) contained items drawn from the literature and our own previous vaccine research [24,27–29]. Before questions about school-located vaccination and programmatic features of these days, the parent/son survey presented the following scenario: “Imagine that [son’s name/your] school hosts vaccination days several times a year. On these days, a health care provider gives recommended vaccines to students. For some students, the vaccines are free, while for others there may be a cost.”
The parent survey assessed how parents preferred to receive information about adolescent vaccines (e.g., Tdap, meningococcal, and HPV vaccines) and to consent for their sons to get a vaccine at school, as well as their preferences for days and times to attend a school vaccination day, and methods for having their sons’ medical records updated with vaccines given. For these questions, parents were asked to indicate all answers that applied. Additional items asked parents how much they agree with the statements: “Vaccination days at [son’s name]’s school would be a convenient way for him to get vaccines,” and “Vaccination days would help students get vaccines who may not get them otherwise.” The 5-point response scale ranged from “strongly disagree” (1) to “strongly agree” (5).
After a statement instructing participants to suppose they had decided to get sons a vaccine at a vaccination day, two items on both the parent and the son surveys assessed willingness to do so with and without a parent present. Items had a 5-point response scale ranging from “definitely not willing” (1) to “definitely willing” (5). Items assessed parents’ and sons’ perceptions about the age at which adolescents should be able to get a vaccine without a parent’s permission. Participants selected an age, from 11 to 19 years (in yearly increments) or the response “adolescents should not be able to get vaccines without parent permission.” In addition, all participants answered an item about how acceptable it would be to hold vaccination days in public places where other students may see each other get vaccinated. The item response scale ranged from “strongly disagree” (1) to “strongly agree” (5). Finally, an item asked “if [son’s name was/you were] allowed to decide on [his/your] own, [he/I] might refuse a vaccine [I/my parents] would want [him/me] to have.” Response options ranged from “strongly disagree” (1) to “strongly agree” (5).
The survey assessed sons’ age, health care use, and previous experience with vaccination in a school setting. We categorized sons’ age as younger (ages 11–15 years) and older (ages 16–19 years). The survey company provided parents’ sociodemographic characteristics: gender, age, race/ethnicity, education level, marital status, income, urbanicity, and region of residence. We defined “urban” as living in a metropolitan statistical area and “rural” as living outside a metropolitan statistical area [30].
Data analysis
We used linear regression to identify bivariate correlates of parents’ perceived convenience of school vaccination days. A multivariate regression model included all variables associated (p < .05) in bivariate analyses. Both analyses used Huber-White standard errors for robustness to address skewing of this outcome measure [31], and reported standardized regression coefficients (betas). We used paired t-tests to assess mean differences in attitudes toward vaccination days for equivalent items on parents’ and sons’ surveys and conducted bivariate analysis on these items by sons’ age. Finally, we used logistic regression to examine the association of son’s age with parent’s preferences for how vaccination records are reported. We conducted all analyses in Stata version 12.1 (Statacorp, College Station, TX) using two-tailed tests and a critical alpha of .05.
Results
Parents preferred to learn about adolescent vaccines through school Web sites (66%) or a one-page flyer (63%) distributed by their sons’ schools. Fewer parents wanted to learn about vaccines via a 10-page informative booklet (34%) or a 1-hour presentation at school (24%). Parents preferred having vaccination days held after school (73%) instead of before (19%) or during school (32%). Parents indicated a similar preference for most days of the week (on average, 45% liked each day), although the most and least popular days were Fridays (50%) and Sundays (20%), respectively.
Consent
With respect to providing permission for their sons to get vaccinated at a school vaccination day, most parents (64%) preferred to sign a consent form that their sons would then take to school. A smaller majority of parents (55%) preferred to provide permission in person at school. Few parents preferred to offer consent via phone (22%), e-mail (26%), signed consent form mailed to school (33%), or online (36%). Overall, 85% of parents preferred to give permission to participate either through a signed consent form the son would take to school or in person at school.
Sons indicated a lower permissible age to get vaccinated without parental consent compared with parents (17 vs. 18 years; t = 6.47; p < .001) (Table 2). In addition, sons were less willing to be vaccinated in school clinics where students could see each other get the vaccine (t = 6.14; p < .001). Although sons were more willing to participate in vaccination days without their parents present, compared with their parents’ responses (t = 2.04; p = .04), sons were more willing to participate if one of their parents was present than if the parent was not present (t = 5.76; p < .001). Similarly, parents were more willing for their sons to participate if a parent was present versus not present (t = 8.67; p < .001). Compared with parents of younger adolescents, parents of older boys were more willing to let their sons participate in vaccination days in situations where students may see each other (β = .13; p = .002) or without a parent present (β = .26; p < .001). Sons showed a similar inclination; older adolescents were more willing to participate in vaccination days without a parent present than were younger boys (β = .15; p = .031).
Table 2.
Parents’ and sons’ attitudes toward vaccine consent and vaccination days
| Parents, mean (SD) | Sons, mean (SD) | p | |
|---|---|---|---|
| Vaccine consent | |||
| Age when vaccination should be permissible without parent’s permission | 18 (1.67) | 17 (2.08) | <.001 |
| Son may refuse vaccination despite parent’s desire | 3.31 (1.05) | 3.25 (1.02) | .47 |
| Willingness to vaccinate at school … | |||
| if other students may see | 3.38 (1.14) | 2.90 (1.11) | <.001 |
| without parent present | 2.74 (1.24) | 2.94 (1.21) | .04 |
| with parent present | 3.33 (1.09) | 3.31 (1.13) | .80 |
Analyses are for 216 parents and sons who both completed the survey, except for the permissible age item (n = 213). Response scale for variables other than age ranged from “strongly disagree” or “definitely not willing” (coded as 1) to “strongly agree” or “definitely willing” (coded as 5).
SD = standard deviation.
Correlates of parents’ perceived convenience
Most parents (81%) believed that school vaccination days would help students get vaccines who may not get them otherwise (mean, 4.0; standard deviation, .90). In addition, 63% of parents agreed or strongly agreed that school vaccination days would be a convenient way for their sons to get immunized (mean, 3.59; standard deviation, 1.12). In multivariate analyses, perceived convenience was lower among older parents (β = −.14; p = .01) (Table 3). Perceived convenience was higher among parents of older sons (β = .15; p = .006) and among those who agreed with laws letting schools share vaccination records with health care providers (β = .32; p < .001). Finally, perceived convenience was higher among parents whose sons had previously received a vaccine at school (β = .09; p < .05) compared with parents whose had sons had never received a vaccine at school.
Table 3.
Parents’ perceived convenience of their sons participating in a school vaccination day (n = 308)
| Perceived convenience, mean (standard deviation) | Bivariate β | Multivariate β | |
|---|---|---|---|
| Parent characteristics | |||
| Sex | |||
| Female | 3.58 (1.14) | Reference | |
| Male | 3.59 (1.11) | .00 | |
| Age | |||
| <45 years | 3.70 (1.04) | Reference | Reference |
| 345 years | 3.42 (1.22) | 3.12* | 3.14* |
| Race/ethnicity | |||
| Non-Hispanic white | 3.63 (1.15) | Reference | |
| Non-Hispanic black | 3.69 (.93) | .02 | |
| Hispanic | 3.45 (1.08) | 3.06 | |
| Other race/ethnicity | 3.36 (1.39) | 3.05 | |
| Education | |||
| High school degree or less | 3.65 (1.10) | Reference | |
| Some college or more | 3.54 (1.14) | 3.05 | |
| Marital status | |||
| Divorced, widowed, separated, never married | 3.65 (1.10) | Reference | |
| Married or living with partner | 3.57 (1.13) | 3.03 | |
| Supports laws that let schools share vaccination records with health care providers | |||
| Disagree or unsure | 3.05 (1.23) | Reference | Reference |
| Agree | 3.88 (.95) | .35* | .32* |
| Son characteristics | |||
| Age | |||
| 11–15 years | 3.41 (1.17) | Reference | Reference |
| 16–19 years | 3.80 (1.03) | .17* | .15* |
| Saw health care provider in past year | |||
| No | 3.62 (1.13) | .01 | |
| Yes | 3.58 (1.13) | Reference | |
| Ever received vaccines at school | |||
| No | 3.52 (1.17) | Reference | Reference |
| Yes | 3.95 (.87) | .13* | .09* |
| Do not know | 3.80 (.63) | .05 | .05 |
| Type of school attending | |||
| Public school | 3.59 (1.10) | Reference | |
| Private school | 3.56 (1.34) | 3.01 | |
| Household characteristics | |||
| Annual household income | |||
| <$60,000 | 3.65 (1.08) | Reference | |
| ≥$60,000 | 3.53 (1.17) | 3.05 | |
| Urbanicity | |||
| Rural | 3.50 (1.38) | Reference | |
| Urban | 3.60 (1.07) | .03 | |
| Region of residence | |||
| West | 3.37 (1.18) | Reference | |
| Midwest | 3.61 (1.16) | .09 | |
| Northeast | 3.54 (1.14) | .06 | |
| South | 3.72 (1.05) | .15 | |
Betas are standardized regression coefficients. Multivariate regression included variables statistically significant in bivariate analyses. Response scale for convenience ranged from “strongly disagree” (coded as 1) to “strongly agree” (coded as 5).
p < .05.
Updating vaccination records
Parents preferred to have their sons’ vaccination records mailed to their homes (69%) or directly to their sons’ physicians (67%) than to be added to an immunization registry (40%) (Figure 1), although these findings differed by age. Parents of older adolescent boys were less likely than parents of younger boys to favor having vaccination records mailed home (odds ratio [OR] = .47; 95% confidence interval [CI], .29–.77) or to their sons’ health care providers (OR = .61; 95% CI, .37–.98). In contrast, parents of older boys were more likely to favor having sons’ vaccine records be entered in an immunization registry that health care providers can access than were parents of younger sons (OR = 1.66; 95% CI, 1.05–2.63).
Figure 1.
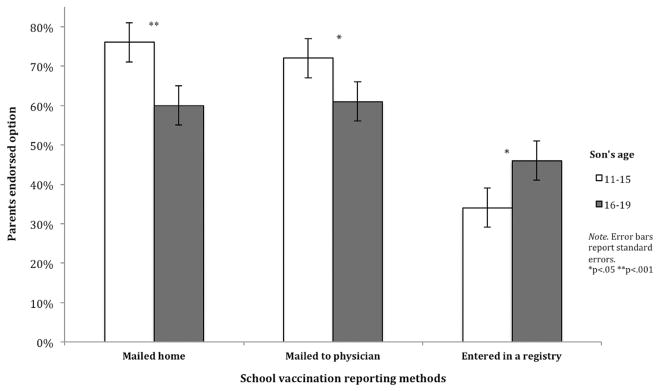
Parents’ preference for adding school vaccine information to medical records.
Discussion
Little research has addressed parents’ preferences regarding specific programmatic features of mass school vaccination, such as how parents would want to receive information about vaccines, how they would want to provide consent, and when vaccination should be offered. These features have direct implications for school vaccination programs and policies, and they provide practical information to help agencies design effective vaccination days. For example, parents generally preferred to receive vaccine information online or through a one-page flyer rather than though an information booklet or a presentation at school, which suggests that communication about vaccines should be targeted, brief, and easy to access. In addition, although parents did not express a strong preference for the day of the week on which to hold a vaccination day, many parents preferred programs to be held after school, perhaps because it would better fit parents’ work schedules. Parents were not asked about their preferences for when vaccination days should be held if they were not present. Consistent with other research examining attitudes and preferences toward school vaccination [27,32], we found that parents and sons preferred a parent to be present during vaccination, which may account, at least in part, for preferences for the time of day. Vaccination days that provide parents with appropriate vaccine information and are sensitive to parents’ schedules may garner broader support and increase overall participation.
Surprisingly, parents also had a strong inclination to consent for their sons to participate through either a signed form their sons would take to school or one that the parents would provide in person. Our data do not offer insight as to why parents did not prefer other methods potentially more convenient for them and cost-effective for schools, but it could be because of parents’ lack of familiarity with other modes of consent. Consent forms may be lost or never returned back to school [33], or parents may not have time to provide consent in person, which creates inefficiency for programs attempting to identify and provide care for adolescents most in need. Electronic methods of consent provide a direct link from parents to providers and are secure, ensuring better communication of willingness to participate in school-located health programs. School vaccination days may benefit by educating parents on the benefits of electronic methods of providing consent, potentially increasing participation.
Another important finding suggests that adolescents’ age is important for parents’ and adolescents’ willingness to participate in school vaccination days, and programmatic preferences for them. Parents of older boys were more willing to have their sons vaccinated at a school vaccination day without a parent present, and they also believed that vaccination days were more convenient than did parents of younger adolescents. We also found that older sons were more willing than younger sons to get vaccinated without a parent present. Taken together with societal and developmental norms of increasing independence as adolescents age [34], these findings suggest that parents and adolescents are more comfortable with adolescents taking increasing responsibility for their own health care as they age. Indeed, previous research with parents of adolescent girls shows that older adolescents girls are more involved in making vaccination decisions, and more likely to be the primary decision maker, than are younger girls [35]. These findings are also aligned with guidelines from major medical organizations that recommend health care services be developmentally appropriate to adolescents’ growing autonomy [36].
Interestingly, sons believed that adolescents should be able to get vaccinated without parental consent at a younger age than parents did. Minor consent laws vary by state but encompass two main areas: the legal status of minors, and the services minors intend to seek [37]. Although adolescents may seek health services such as family planning and sexually transmitted infection prevention without parental consent in most states, seeking vaccination services without parental consent would depend on the state laws and vaccine [37]. For instance, if a doctor views HPV vaccine as a method to prevent a sexually transmitted infection, the vaccine might be provided to the adolescent without parental consent [38]. In addition, adolescents’ views on vaccination may contrast with their parents’ views, which may lead some to seek vaccination without parental consent [38]. Although the legal implications of vaccination would be left to the jurisdiction of the state in which an adolescent resides, the difference in opinions involving age of consent between sons and their parents in this study again supports the need for developmentally appropriate health care for adolescents, inside and outside the medical home. Hence, vaccination days should be designed to reassure parents’ participation and adolescents’ desire to be a part of the decision-making process.
Age also had a role in how parents would want their sons’ medical records updated. Parents of older adolescents were less likely than parents of younger ones to endorse having their son’s immunization records sent to their home or to their son’s health care provider, but more likely to endorse having vaccine information entered into a registry. Although the reason for this pattern of findings is not clear from our data, it may be another indicator of parents’ increasing willingness to relinquish control over their child’s health care as their children age, or to their looking toward a time when they will not have control over their children’s medical records.
Parental concerns about updating medical records and coordinating care with their child’s medical home are a barrier to providing vaccines in alternative settings such as schools [13]. Findings from the present study provide information that school vaccination programs can use to address these concerns, and provide better coordination of care with the medical home. Although vaccine registries hold great promise for improving timely vaccine delivery [39], we found that parents’ most preferred methods for having their sons’ medical records updated were for vaccination records to be sent either to their home or directly to their son’s health care provider. Not all states have well-developed immunization information systems, and many do not yet include adolescent vaccines [40]; consistent with previous research [39], parents may not be familiar with these methods and are more accustomed to having vaccines recorded on immunization cards and kept in personal records. As a result, school vaccination programs should include education about immunization registries to inform parents and adolescents about their apparent benefits and reliability, to garner more trust with vaccination efforts outside the medical home. In addition, vaccination days should provide multiple means of vaccine reporting to accommodate parental preferences.
This study had notable strengths, including a national, population-based sample and novel items examining programmatic features of school vaccination days not previously examined. The inclusion of adolescents’ perspectives in addition to those of their parents helps to ensure relevance of findings for schools and community partners interested in developing immunization programs. Study limitations were that the cross-sectional design did not allow causal inference about willingness to participate in and perceived convenience of school vaccination days. The lower response rate among sons may have limited our ability to generalize to other male adolescents in the US. In addition, because most parents reported that their sons attended public schools, our findings may be most relevant to understanding vaccination in public school settings. Although regression analyses used robust standard errors to account for skewness, this method does not correct for potential biases in the regression coefficients. The study provides a preliminary glimpse into the practical features of implementing a school vaccination day, but further inquiry is needed to confirm attitudes regarding consent and reporting doses administered at school. In addition, survey questions addressed recommended adolescent vaccines in general, rather than identifying specific vaccines. Previous research suggests that willingness could vary for different vaccines [23]. Finally, because the study focused on adolescent boys, the generalizability of findings to adolescent girls and their parents will need to be established. Analysis from this study supports similar conclusions reached in research that focused on adolescent girls and their parents [27], and could justify further studies that include both female and male adolescents and their parents to help delineate whether preferences vary by sex.
Taken together with other research conducted on parents’ acceptability for school vaccinations [23,27,32], our study provides further support for pursuing vaccination days as a means to increase adolescent immunization coverage. More important, however, this study highlights the importance of understanding parent and adolescent preferences for specific details for conducting vaccination days to make programs practical to a targeted population. Findings also suggest creating programs that allow adolescents a measure of autonomy to be vaccinated and under what circumstances, underscoring the importance of collaborative decision making in adolescent health care. Program implementation that is sensitive to these issues may help mass vaccination programs become more acceptable among parents and their children, and increase overall vaccine coverage.
IMPLICATIONS AND CONTRIBUTION.
This study provides evidence supporting implementing mass vaccination programs at schools. Programs should adopt flexible approaches to address the desires of parents and the changing needs of adolescents as they mature.
Acknowledgments
Funding Sources
This study was supported in part by a research grant from the Investigator-Initiated Studies Program of Merck Sharp and Dohme Corp. Additional support was provided by the National Institutes of Health (Grant P30CA016058), and an NRSA in Primary Medical Care at the University of Minnesota (Grant T32HP22239). N.T.B. has also received grants and/or honoraria from Merck Sharp and Dohme and from GlaxoSmithKline.
Footnotes
Disclaimer: The opinions expressed in this paper are those of the authors and do not necessarily represent those of Merck Sharp and Dohme Corp. Merck Sharp and Dohme Corp. played no role in the study design, planning, implementation, analysis, or reporting of the findings.
References
- 1.Cohn AC, MacNeil JR, Clark TA, et al. [Accessed April 8, 2013];Prevention and control of meningococcal disease: Recommendations of the Advisory Committee on Immunization Practices (ACIP) Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6202a1.htm. [PubMed]
- 2.Broder K, Cortese M, Iskander J, et al. Advisory Committee on Immunization Practices (ACIP) Preventing tetanus, diphtheria, and pertussis among adolescents: Use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccines recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2006;55:1–34. [PubMed] [Google Scholar]
- 3.Markowitz LE, Dunne E, Saraiya M, et al. Quadrivalent human papilloma-virus vaccine. MMWR Morb Mortal Wkly Rep. 2007;56:1–24. [Google Scholar]
- 4.Dunne E, Markowitz L, Chesson H, et al. Recommendations on the use of quadrivalent human papillomavirus vaccine in males—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1705–8. [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services. [Accessed on April 8, 2013];Healthy People 2020 Objectives: immunization and infectious diseases. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=23.
- 6.Committee on Infectious Diseases. HPV vaccine recommendations. Pediatrics. 2012;129:602–5. doi: 10.1542/peds.2011-3865. [DOI] [PubMed] [Google Scholar]
- 7.Schuchat A, Brady MT. [Accessed November 20, 2013];HPV vaccine can’t wait: Immunization of younger teens is critical to preventing serious cancers later in life. Available at: http://aapnews.aappublications.org/content/early/2012/08/31/aapnews.20120831-1.full.
- 8.Dorell C, Stokley S, Yankey D, et al. National and state vaccination coverage among adolescents aged 13–17 Years—United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61:671–7. [PubMed] [Google Scholar]
- 9.Nordin JD, Solberg LI, Parker ED. Adolescent primary care visit patterns. Ann Fam Med. 2010;8:511–6. doi: 10.1370/afm.1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stokley S, Cohn A, Dorell C, et al. Adolescent vaccination-coverage levels in the United States: 2006–2009. Pediatrics. 2011;128:1078–86. doi: 10.1542/peds.2011-1048. [DOI] [PubMed] [Google Scholar]
- 11.Marcell AV, Klein JD, Fischer I, et al. Male adolescent use of health care services: Where are the boys? J Adolesc Health. 2002;30:35–43. doi: 10.1016/s1054-139x(01)00319-6. [DOI] [PubMed] [Google Scholar]
- 12.US Census Bureau. [Accessed on May 13, 2013];School enrollment. Available at: http://www.census.gov/hhes/school/
- 13.Lindley MC, Boyer-Chu L, Fishbein DB, et al. The role of schools in strengthening delivery of new adolescent vaccinations. Pediatrics. 2008;121:S46–54. doi: 10.1542/peds.2007-1115F. [DOI] [PubMed] [Google Scholar]
- 14.Brener ND, Wheeler L, Wolfe LC, et al. Health services: Results from the school health policies and programs study 2006. J Sch Health. 2007;77:464–85. doi: 10.1111/j.1746-1561.2007.00230.x. [DOI] [PubMed] [Google Scholar]
- 15.Strozer J, Juszczak L, Ammerman A. School-based health centers: National census school year 2007–08. Washington, DC: National Assembly on School-Based Health Care; 2010. [Accessed April 8, 2013]. Available at: http://ww2.nasbhc.org/NASBHCCensusReport07-08.pdf. [Google Scholar]
- 16.Hollinger F. Comprehensive control (or elimination) of hepatitis B virus transmission in the United States. Gut. 1996;38:S24–30. doi: 10.1136/gut.38.suppl_2.s24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stretch R, Roberts S, McCann R, et al. Parental attitudes and information needs in an adolescent HPV vaccination programme. Br J Cancer. 2008;99:1908–11. doi: 10.1038/sj.bjc.6604766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Watson M, Shaw D, Molchanoff L, et al. Challenges, lessons learned and results following the implementation of a human papilloma virus school vaccination program in South Australia. Aust NZ J Public Health. 2009;33:365–70. doi: 10.1111/j.1753-6405.2009.00409.x. [DOI] [PubMed] [Google Scholar]
- 19.Fiala SC, Cieslak PR, DeBess EE, et al. Physician attitudes regarding school-located vaccination clinics. J Sch Health. 2013;83:299–305. doi: 10.1111/josh.12031. [DOI] [PubMed] [Google Scholar]
- 20.Cooper Robbins SC, Ward K, Skinner SR. School-based vaccination: A systematic review of process evaluations. Vaccine. 2011;29:9588–99. doi: 10.1016/j.vaccine.2011.10.033. [DOI] [PubMed] [Google Scholar]
- 21.Lawrence RS, Gootman JA, Sim LJ National Research Council, Committee on Adolescent Health Care Services and Models of Care for Treatment, Prevention, and Healthy Development, Institute of Medicine. [Accessed April 5, 2013];Adolescent health services: missing opportunities. Available at: http://www.nap.edu/catalog.php?record_id=12063.
- 22.McRee A, Reiter PL, Pepper JK, et al. Correlates of comfort with alternative settings for HPV vaccine delivery. Hum Vaccin Immunother. 2013;9:42–9. doi: 10.4161/hv.22614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kelminson K, Saville A, Seewald L, et al. Parental views of school-located delivery of adolescent vaccines. J Adolesc Health. 2012;51:190–6. doi: 10.1016/j.jadohealth.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 24.Reiter PL, McRee AL, Kadis JA, et al. HPV vaccine and adolescent males. Vaccine. 2011;29:5595–602. doi: 10.1016/j.vaccine.2011.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reiter PL, McRee A, Pepper JK, et al. Longitudinal predictors of human papillomavirus vaccination among a national sample of adolescent males. Am J Public Health. 2013;103:1419–27. doi: 10.2105/AJPH.2012.301189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dennis JM. [Accessed April 5, 2013];Description of within-panel survey sampling methodology: The Knowledge Networks approach. Available at: http://www.knowledgenetworks.com/ganp/docs/kn-within-panel-survey-sampling-methodology.pdf.
- 27.Kadis JA, McRee A, Gottlieb SL, et al. Mothers’ support for voluntary provision of HPV vaccine in schools. Vaccine. 2011;29:2542–7. doi: 10.1016/j.vaccine.2011.01.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reiter PL, Brewer NT, Gottlieb SL, et al. Parents’ health beliefs and HPV vaccination of their adolescent daughters. Soc Sci Med. 2009;69:475–80. doi: 10.1016/j.socscimed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 29.Rand CM, Humiston SG, Schaffer SJ, et al. Parent and adolescent perspectives about adolescent vaccine delivery: Practical considerations for vaccine communication. Vaccine. 2011;29:7651–8. doi: 10.1016/j.vaccine.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 30.US Census Bureau. [Accessed on May 13, 2013];Census glossery. Available at: http://factfinder.census.gov/home/en/epss/glossary_a.html.
- 31.Freedman DA. On the so-called “Huber sandwich estimator” and “robust standard errors. The American Statistician. 2006;60:299–302. [Google Scholar]
- 32.Middleman AB, Tung JS. School-located immunization programs: Do parental preferences predict behavior? Vaccine. 2011;29:3513–6. doi: 10.1016/j.vaccine.2011.02.101. [DOI] [PubMed] [Google Scholar]
- 33.Woodruff BA, Unti L, Coyle K, et al. Parents’ attitudes toward school-based hepatitis B vaccination of their children. Pediatrics. 1996;98:410–3. [PubMed] [Google Scholar]
- 34.Van Petegem S, Beyers W, Vansteenkiste M, et al. On the association between adolescent autonomy and psychosocial functioning: Examining decisional independence from a Self-Determination Theory perspective. Dev Psychol. 2012;48:76. doi: 10.1037/a0025307. [DOI] [PubMed] [Google Scholar]
- 35.McRee AL, Reiter PL, Brewer NT. Vaccinating adolescent girls against human papillomavirus—Who decides? Prev Med. 2010;50:213–4. doi: 10.1016/j.ypmed.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosen DS, Blum RW, Britto M, et al. Transition to adult health care for adolescents and young adults with chronic conditions: Position paper of the Society for Adolescent Medicine. J Adolesc Health. 2003;33:309–11. doi: 10.1016/s1054-139x(03)00208-8. [DOI] [PubMed] [Google Scholar]
- 37.English A, Shaw FE, McCauley MM, et al. Legal basis of consent for health care and vaccination for adolescents. Pediatrics. 2008;121:S85–7. doi: 10.1542/peds.2007-1115J. [DOI] [PubMed] [Google Scholar]
- 38.Farrell RM, Rome ES. Adolescents’ access and consent to the human papillomavirus vaccine: A critical aspect for immunization success. Pediatrics. 2007;120:434–7. doi: 10.1542/peds.2006-1692. [DOI] [PubMed] [Google Scholar]
- 39.Linkins RW, Salmon DA, Omer SB, et al. Support for immunization registries among parents of vaccinated and unvaccinated school-aged children: A case control study. BMC Public Health. 2006;6:236. doi: 10.1186/1471-2458-6-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ford CA, English A, Davenport AF, et al. Increasing adolescent vaccination: Barriers and strategies in the context of policy, legal, and financial issues. J Adolesc Health. 2009;44:568–74. doi: 10.1016/j.jadohealth.2008.11.015. [DOI] [PubMed] [Google Scholar]


