Abstract
OBJECTIVE
To examine the incidence of incisional hernias (IHs) and propose a simple modification to reduce the incidence of IHs. Robot-assisted radical prostatectomy (RARP) historically uses a vertical midline camera port incision to extract the prostate.
METHODS
Of 900 consecutive RARPs, the initial 735 had a vertical and subsequent 165 transverse incisions. Two methods were used to identify IHs: clinic visits noted in the prospective database and screening using electronic mail. We compared the baseline factors between the vertical IH and IH-free cohorts. The maximal scar width was recorded in 178 consecutive men presenting to our clinic: vertical (n = 107) and transverse (n = 71).
RESULTS
IHs occurred significantly more often after a vertical incision (5.3% vs 0.6%, P = .005). The IH rates after a vertical incision could be estimated to be as great as 16.7% (18 of 108) using the electronic mail respondents or as low as 3.3% (21 of 627) according to clinic follow-up. On univariate analysis, baseline age, International Index of Erectile Function 5-item questionnaire, prostate weight, bother score (all P ≤ .05), and body mass index (P = .058) were associated with an increased risk of an IH. After adjusting for baseline factors on multivariate logistic regression analysis, the relative odds of developing an IH with a vertical versus transverse incision was 11 (95% confidence interval 1.5–82). The average maximal scar width was reduced from 5.5 to 2.0 mm (P < .0001).
CONCLUSION
In the present sample population, the vertical IH rate was estimated to be potentially as low as 3.3% or as great as 16.7%. On multivariate analysis, a greater body mass index and larger prostate size significantly increased the risk of hernia development. Transverse incisions dramatically reduced the rate of IHs and the maximal scar width. The IH rates varied significantly by reporting method.
The incisional hernia (IH) rates after robot-assisted radical prostatectomy (RARP) have not been well characterized. In several large RARP series, the IH rate was estimated at 0.2%–3% but with very inadequate and unclear follow-up.1–4 For traditional surgery the IH rate has been 5%–19%.5–8 However, even in the Cochrane database,8 only 54% of all randomized controlled trials had follow-up of ≥1 year. Long-term follow-up for IH has shown that the rate at 1 year might not reflect the true incidence of this outcome, and in some series, 35% of all IHs occurred after 3 years.5 The incidence of IHs remains a concern because of its reoperation rate; secondary repair failures as great as 45% have been observed.8
The published surgical data suggest that the rate of IH is significantly reduced with a transverse incision versus a vertical incision. In a meta-analysis of standard surgical cases for abdominal surgery, transverse incisions were less prone to fail than were midline incisions,8 especially for incisions at or above the navel. This has also been evaluated in the published urology data, and a prospective randomized trial of open radical prostatectomy showed no significant differences in the hernia incidence between Pfannenstiel and vertical incisions. However, their findings do not apply well because the incisions were below the navel and were extraperitoneal, which has a much lower risk of hernia formation than trans-peritoneal procedures above the navel.9
In the present series, we estimated the incidence of IH in our RARP patient cohort and examined the effects of a transverse versus vertical midline incision on the cosmesis, incisional failure, and reoperation rates.
MATERIAL AND METHODS
From 2002 to 2009, 900 RARPs were performed by a single surgeon (T.A.), with all the data maintained in a prospective database. A total of 735 patients (patients 1–735) had a vertical incision and 165 (patients 736–900) had a transverse incision for the midline camera port. All closures were performed by the assisting fellow or senior resident and were documented prospectively in the electronic database. All data were collected and analyzed under an institutional review board-approved protocol.
The vertical and transverse incision and closure techniques are nearly identical, except for the orientation of the skin and fascial incision. After insufflation, a 1.5-cm transverse incision was made just above the navel, with the subcutaneous fat spread with a clamp. A standard 10–12 nonbladed single use port was placed for the camera port. Once the procedure was completed and the robot undocked, the entrapment bag strings were transitioned to this camera port site. The transverse skin incision (Figure 1) was evenly extended 2–3 mm on both sides; next, the fascial incision was similarly extended laterally and evenly for a total transverse length of 2–4 cm, depending on the prostate size. The muscle and peritoneum were bluntly stretched, usually with retractors, and the prostate was removed. The fascia was closed transversely with a running, slowly absorbing polydioxanone suture, placing the needle deep to the fascia but superficial to the rectus muscle. No attempt was made to approximate the peritoneum or midline muscle. The vertical incision and closure were exactly the same, except for the orientation of the skin and fascial incisions. The closure time was the same, except that the transverse incision was a little easier to close because the muscle was an excellent guide for needle placement. If a concurrent umbilical hernia was present, we positioned the incision in the navel fold and placed the port through the hernia, if possible. When closing the fascia, we incorporated broad bites to ensure closure of all fascial defects.
Figure 1.
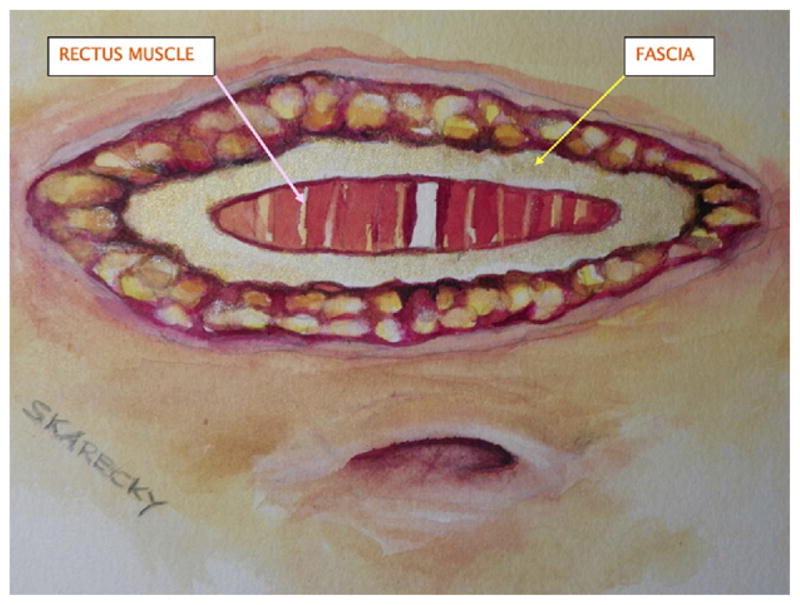
Transverse incision shown above navel, with innermost oval shown as rectus muscle bands. Fascial layer depicted immediately above muscle bands below dermal layers.
As a tertiary referral center, long-term follow-up data are obtained by clinic visits, telephone correspondences, postcards, and letters and, in the present study, an electronic mail survey. By reviewing the database for the patients seen in our clinics, we identified 22 men with IHs after a vertical incision and 1 patient with IH after a transverse incision. The average follow-up for the vertical cohort was 3.6 years and 1.5 years for the transverse cohort. To further assist in estimating the rate, we queried, using electronic mail, all known electronic mail addresses (n = 443) in our database, screening specifically for IH. Of this group, 79 (17.8%) were not deliverable. Of the delivered messages, 145 men (40%) responded; however, 5 responded but gave no IH answer, for a response rate of 39% (140 of 359). Our electronic-mail cohort identified 17 additional vertical IHs from 108 men with vertical incisions and no IHs from 32 men with transverse incisions. From the 2 methods used to identify IH (clinic visits noted in the prospective database and screening using electronic mail), 40 His were found (39 vertical and 1 transverse). We compared the baseline factors between the vertical IH and IH-free cohorts only.
To evaluate cosmesis, the maximal scar width of the camera port incision was measured by the clinic registered nurse (R.J.) in 178 consecutive men presenting to our clinic (vertical, 107 and transverse, 71). No scar size measurements were obtained from the electronic-mail group.
Univariate statistical analysis was performed using t tests and chi-square or Fisher’s exact tests (SAS, version 9.1, SAS Institute, Cary, NC). Logistic regression analysis was used to investigate the risk of IH associated with the incision type after adjusting for the baseline covariables. Independent variables significant at P < .15 were retained in the final model.
RESULTS
The baseline demographics were similar for men undergoing either a vertical or transverse camera port incision (Table 1). The IH rate was greater for the vertical incisions than for the transverse incisions (5.3% vs 0.6%, respectively, P = .005) and varied substantially by method of query (12.9% for the electronic-mail response vs 2.9% using clinic follow-up, P < .001; Tables 2 and 4). The estimated vertical IH rate could conceivably be reported as low as 3.3% (21 of 627) or as great as 16.7% (18 of 108) using electronic mail. The average follow-up for the 2 query methods was 3.6 years for the vertical group and 1.5 years for the transverse group.
Table 1.
Baseline characteristics
| Baseline Characteristic | Vertical Incision (n = 1–735)
|
Transverse Incision (n = 736–900)
|
P Value* | ||
|---|---|---|---|---|---|
| Patients (n) | Mean ± SD | Patients (n) | Mean ± SD | ||
| Age (y) | 735 | 61.3 ± 7.3 | 165 | 61.3 ± 7.4 | .998 |
| PSA (ng/mL) | 735 | 6.7 ± 6.2 | 163 | 6.8 ± 5.5 | .775 |
| AUA | 734 | 8.6 ± 7.0 | 163 | 8.4 ± 6.5 | .823 |
| Bother score | 690 | 1.8 ± 1.5 | 164 | 1.7 ± 1.6 | .794 |
| IIEF-5 | 727 | 19.2 ± 7.3 | 162 | 19.6 ± 6.7 | .465 |
| BMI (kg/m2) | 735 | 26.8 ± 3.4 | 164 | 26.9 ± 3.8 | .936 |
| Prostate weight (g) | 728 | 52.2 ± 20.9 | 164 | 53.1 ± 16.7 | .599 |
| Query method (n) | .132† | ||||
| E-mail/telephone | 108 (77.1) | 32 (22.9) | |||
| Clinic | 627 (82.5) | 133 (17.5) | |||
PSA, prostate-specific antigen; AUA, American Urological Association Symptom Index; IIEF-5, International Index of Erectile Function 5-item questionnaire; BMI, body mass index; E-mail, electronic mail.
Data presented as mean ± SD or numbers, with percentages in parentheses.
t Test, unless otherwise noted.
Pearson chi-square test.
Table 2.
Baseline comparisons of those without and with incisional hernias
| Baseline Characteristic | Incisional Hernia
|
P Value* | |
|---|---|---|---|
| No | Yes | ||
| Incision | .005 | ||
| Vertical | 696 (94.7) | 39 (5.3) | |
| Transverse | 164 (99.4) | 1 (0.6) | |
| Query method | <.001 | ||
| E-mail/telephone | 122 (87.1) | 18 (12.9) | |
| Vertical | 90 (83.3) | 18 (16.7) | |
| Transverse | 32 (100.0) | 0 (0) | |
| Clinic | 738 (97.1) | 22 (2.9) | |
| Vertical | 606 (96.7) | 21 (3.3) | |
| Transverse | 132 (99.2) | 1 (0.8) | |
Data presented as number of patients, with percentages in parentheses.
Fisher’s exact test.
Table 4.
Multivariate analysis of significant predictors of incisional hernias*
| Parameter | Coefficient | P Value | Odds Ratio | 95% Confidence Interval |
|---|---|---|---|---|
| Age (continuous) | 0.050 | .077 | 1.05 | 0.99–1.11 |
| IIEF-5 (continuous) | −0.040 | .088 | 0.96 | 0.92–1.01 |
| BMI (continuous) | 0.119 | .011 | 1.13 | 1.03–1.23 |
| Prostate weight (continuous) | 0.015 | .027 | 1.01 | 1.00–1.03 |
| Query method (clinic [0] vs e-mail [1]) | 1.894 | <.001 | 6.65 | 3.26–13.57 |
| Incision (vertical [1] vs transverse [0]) | 2.396 | .020 | 10.98 | 1.47–82.26 |
Abbreviations as in Table 1.
PSA, AUA, and bother score not retained in stepwise multivariate model because of lack of significance (P > .4).
The baseline factors between the IH group and no-IH group are listed in Table 3. On univariate analyses, the baseline factors of age (P = .007), International Index of Erectile Function 5-item questionnaire (IIEF-5; P = .005), prostate weight (P = .005), bother score (P = .04), and body mass index (BMI; P = .06) were associated with an increased risk of IHs. Men with IHs had significantly larger prostates; the prostate weight is an excellent surrogate for incision size because the incision is always made “just” large enough to remove the prostate. On multivariate analysis (Table 4), we also found increasing age, prostate weight, BMI, and decreasing IIEF-5 score significantly increased the risk of IH. Additionally, men with any history of an inguinal hernia had a trend toward an increased risk of an IH.
Table 3.
Univariate analysis of predictors of incisional hernias
| Characteristic | No IH
|
IH
|
P Value* | ||
|---|---|---|---|---|---|
| Patients (n) | Value | Patients (n) | Value | ||
| Age (y) | 860 | 61.2 ± 7.3 | 40 | 64.4 ± 6.8 | .007 |
| PSA (ng/mL) | 858 | 6.7 ± 6.0 | 40 | 7.3 ± 7.0 | .600 |
| History hernia (n) | 696 | 98 (13) | 39 | 8 (20) | .24 |
| AUA | 857 | 8.5 ± 6.9 | 40 | 10.4 ± 7.0 | .084 |
| Bother score | 817 | 1.7 ± 1.5 | 37 | 2.2 ± 1.1 | .041 |
| IIEF-5 | 850 | 19.4 ± 7.1 | 39 | 16.1 ± 8.0 | .005 |
| BMI (kg/m2) | 859 | 26.8 ± 3.4 | 40 | 27.9 ± 3.9 | .058 |
| Prostate weight (g) | 852 | 51.9 ± 19.6 | 40 | 61.1 ± 28.8 | .005 |
Abbreviations as in Table 1.
Data presented as mean ± SD or numbers of patients, with percentages in parentheses.
t Test.
Surgeon Impact
An analysis of the fellow or resident responsible for the closure showed that 68% of the closure surgeons had an IH rate of 0%–5%, 19% had an IH rate of 5%–7.5%, and 13% had an IH rate >10%. The closing surgeon was a chief resident or fellow >98% of the time. Junior level residents (years 1–3) always closed with a more senior assistant but, remarkably, had no hernias identified. Due in part to the small numbers, none of the trends was statistically significant.
Incision Orientation
The change from a vertical to transverse incision orientation has resulted in significantly fewer hernias. After adjusting for query method and baseline covariables, the relative odds for IH development was nearly 11 times greater with a vertical incision than with a transverse incision (odds ratio 10.98, 95% confidence interval 1.47–82.26; Table 4). Because of the well-known effect of tension across suture lines, we decided to measure the maximal scar width (Fig. 2) between the vertical and transverse incisions. The average maximal scar width for the vertical group was 5.5 mm versus 2.1 mm for the transverse group, nearly threefold wider (P < .0001).
Figure 2.
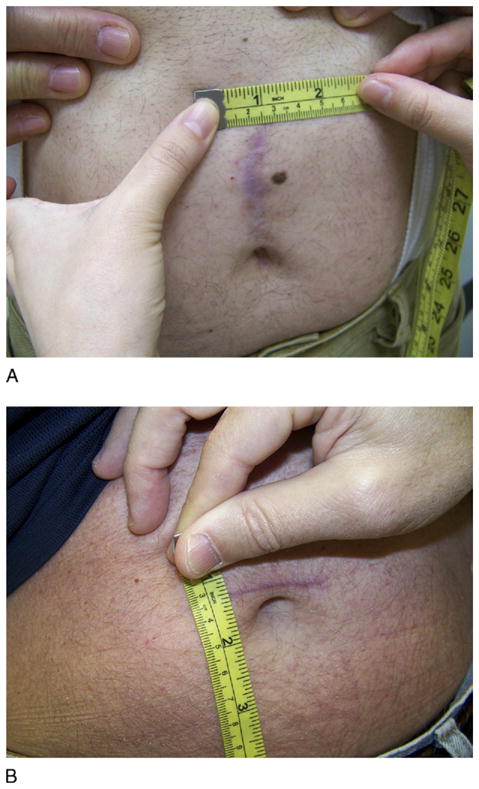
Representative (A) vertical and (B) transverse incisions and measurements.
IH Repair
At the last follow-up, of 27 men questioned specifically about IH repair, 8 (30%) confirmed it. The failure rate of the repaired IHs at the last follow-up was 37.5% (3 of 8). Also, 1 of these patients nearly died of a postoperative massive pulmonary embolism.
COMMENT
The reported cumulative incidence of IH varies from 9% to 19% in large open abdominal surgery series, and it is often an overlooked significant complication when we are counseling patients.5–8 The occurrence of IHs remains underreported, problematic to patients, and a concern because it is a complication often requiring surgical revision, with a reported failure rate of ≤45%.8 Another very concerning aspect of IHs is that their incidence increases with time and appears to be largely underreported in RARP series. This is the first study to specifically report on IHs from the midline camera port after RARP. There are likely numerous reasons for this, including, among other issues, that RARP and to some extent laparoscopic radical prostatectomy are new to urologists and that surgical margins, continence, and so forth, were and are more problematic to patients and urologists.
However, many published studies are important to note. Hoer et al10 followed up 2983 patients who had undergone laparotomy during a 10-year period and calculated the incidence of an IH at almost 20%, with the presentation of 50% of the IHs >12 months postoperatively. A surgical cohort of patients was followed up prospectively for 10 years and noted that 35% of all IHs occurred after 3 years.5 The optimal method of fascial closure has also been debated in published studies. Hodgson et al,11 in a large meta-analysis of randomized controlled trials of abdominal fascial closures, comparing different suture materials and suturing techniques, showed that level 1 evidence exists for with a markedly lower rate of IH using nonabsorbable suture and a continuous suture technique. Nonabsorable suture reduced the rate by 32% and using a continuous suture technique instead of interrupted decreased the rate by 27%.11 It is also well known that IH repair is complicated by failure rates of 32%–63%.12
During the past 2–3 years, we noticed and turned our attention to IHs. The present retrospective report is our initial attempt to address this problem. A significant issue with this and all large retrospective analyses of this nature is how follow-up was accomplished. Our estimated rate of IH with vertical incisions could be as low as 3.3% or as great as 16.7%. The disparity in querying methods was most striking when using “clinic” data versus electronic mail responses (Tables 2 and 4). Men might not return to the clinic for a variety of reasons, including distance, dissatisfaction because of this complication, and other unknown reasons. Thus, we sought to increase our follow-up using electronic mail. The electronic mail query allowed men to report this complication without clinic contact. Regardless, whether the rate was 3.3% or 16.7%, it is a problem.
The IH rate after RARP has been poorly defined, with a range of 0%–3%.1–4 Patel et al1 had a rate of 0.2% (4 of 1900 cases) with average follow-up of 53 months. It is unclear, however, what the follow-up protocol consisted of to determine the true IH rate. Menon et al2 reported follow-up data for 2652 patients with a minimum follow-up of 1 year (median 36 months); however, no breakdown of the complications was provided to calculate the IH rate. In another report, Martinez-Pineiro et al3 showed the results of their initial 600 cases of laparoscopic radical prostatectomy at a large university teaching hospital. They reported an IH rate of 3%. However, the follow-up was not defined nor was notation provided of how the IH was diagnosed.3 In another series of >600 RARPs by Blatt et al,4 the incisional/inguinal hernia rate was 1.9% at 4 months of follow-up. Again, the 2 types of hernias were not stratified to help identify the true incidence of IH.
In the present study, we did not find an obvious issue with individual surgeon skill or experience. We examined the overall year of training and the experience on the service, with no significant findings. The distribution of vertical IHs was fairly even, regardless of experience. We also considered the vertical IH rate for the last 165 consecutive cases (ie, patients 571–735 with 12 IHs), which was not significantly changed at 7.3%. Consistent with no obvious finding with surgeon skill, we did find that men with vertical IHs had significantly greater prostate weight, lower IIEF-5 scores, and older age and showed a trend toward a greater BMI. These findings suggest a connection between vertical IHs and longer incisions and less vitality (low IIEF-5 scores and older age). We only performed running closures with slowly absorbing suture; hence, we cannot comment on the effectiveness of interrupted closures.
The main finding of the present study, and in previously published studies, is that a transverse incision (vs a vertical incision) can dramatically reduce the IH rate. The findings of the present study imply that vertical incisions because of their orientation have more lateral tension, tending to pull the incision apart (Figure 2) compared with transverse incisions, which would bring the fascia together. The cosmesis findings strongly support this theory. From the Cochrane review, 16 prospective randomized trials that met the criteria for evaluation with a total of 3072 patients compared midline and transverse incisions. The transverse incision was less painful, had less effect on pulmonary function, and showed a clear trend toward being less prone to rupture, dehiscence, and IH formation.8 Halm et al13 showed in a randomized controlled trial of upper abdominal cholecystectomy incisions in 150 women that a transverse versus vertical incision reduced the IH rate to 1.7% from 14.5%, respectively (P = .017). Transverse incisions were also significantly thinner (3.3 vs 8.3 mm; P < .00001). Subjective scoring by surgeon and patient found the transverse incision to be more appealing (P = .03).13 Seiler et al,14 in a randomized, double-blind equivalence trial, showed the IH rate was reduced from 16% to 12% using a transverse rather than a midline incision during major abdominal laparotomy.
A weakness of the present study was the retrospective nature, especially with identifying IHs and the shorter follow-up for the transverse group. Hence, we attempted to present the data at the extremes. Another weakness was the inability to definitely differentiate between an umbilical hernia and a postoperative IH. In the clinic vertical incision group, we were able to confirm the type of hernia by physical examination for all 18 of the 39 IHs.
CONCLUSIONS
As is strongly supported by the existing data, our findings indicate that the camera port site incisions should be transverse. The incidence of IHs is probably underreported and underemphasized. In the present sample population, we estimated the vertical IH rate to be potentially as low as 3.3% or as great as 16.7%. On multivariate analysis, a greater BMI and larger prostate size significantly increased the risk of hernia. Transverse incisions dramatically reduced the IH rate and the maximal scar width after adjusting for baseline covariables. Also, the IH rate varied significantly by reporting method.
References
- 1.Patel VR, Palmer KJ, Coughlin G, Samavedi S. Robot-assisted laparoscopic radical prostatectomy: perioperative outcomes of 1500 cases. J Endourol. 2008;22:2299–2305. doi: 10.1089/end.2008.9711. [DOI] [PubMed] [Google Scholar]
- 2.Menon M, Shrivastava A, Kaul S, et al. Vattikuti Institute prostatectomy: contemporary technique and analysis of results. Eur Urol. 2007;51:648–657. doi: 10.1016/j.eururo.2006.10.055. [DOI] [PubMed] [Google Scholar]
- 3.Martinez-Pineiro L, Caceres F, Sanchez C, et al. Learning curve of laparoscopic radical prostatectomy in a university teaching hospital; experience after the first 600 cases. Eur Urol Suppl. 2006;5:914–924. [Google Scholar]
- 4.Blatt AM, Fadahunsi A, Ahn C, et al. Surgical complications related to robotic prostatectomy; prospective analysis (analysis) J Urol. 2009;181:353. [Google Scholar]
- 5.Mudge M, Hughes LE. Incisional hernia; a 10 year prospective study of incidence and attitudes. Br J Surg. 1985;72:70–71. doi: 10.1002/bjs.1800720127. [DOI] [PubMed] [Google Scholar]
- 6.Israleson LA, Jonsson T. Incisional hernia after midline laparotomy: a prospective study. Eur J Surg. 1996;162:125–129. [PubMed] [Google Scholar]
- 7.Osther PJ, Gjode P, Mortensen BB, et al. Randomized comparison of polyglycolic acid and polyglyconate sutures for abdominal fascial closure after laparotomy in patients with suspected impaired wound healing. Br J Surg. 1995;82:1080–1082. doi: 10.1002/bjs.1800820824. [DOI] [PubMed] [Google Scholar]
- 8.Brown SR, Goodfellow PB. Transverse versus midline incision for abdominal surgery. Cochrane Database Syst Rev. 2005:CD005199. doi: 10.1002/14651858.CD005199.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salonia A, Suardi N, Crescenti A, et al. Pfannenstiel versus vertical laparotomy in patients undergoing radical prostatectomy with spinal anesthesia: results of a prospective, randomized trial. Eur Urol. 2005;47:202–208. doi: 10.1016/j.eururo.2004.07.025. [DOI] [PubMed] [Google Scholar]
- 10.Hoer J, Stumpf M, Rosch R, et al. Prevention of incisional Hernia. Chirurg. 2002;73:474–480. doi: 10.1007/s00104-002-0539-9. [DOI] [PubMed] [Google Scholar]
- 11.Hodgson NC, Malthaner RA, Ostbye T. The search for an ideal method of abdominal fascial closure: a meta-analysis. Ann Surg. 2000;231:436–442. doi: 10.1097/00000658-200003000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burger JW, Luijendijk RW, Hop WC, et al. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernias. Ann Surg. 2004;240:578–585. doi: 10.1097/01.sla.0000141193.08524.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Halm JA, Lip H, Schmitz PI, Jeekel J. Incisional hernia after upper abdominal surgery: a randomised controlled trial of midline versus transverse incision. Hernia. 2009;13:275–280. doi: 10.1007/s10029-008-0469-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seiler CM, Deckert A, Diener MK, et al. Midline versus transverse incision in major abdominal surgery a randomized, double-blind equivalence trial. Ann Surg. 2009;249:913–920. doi: 10.1097/SLA.0b013e3181a77c92. [DOI] [PubMed] [Google Scholar]


