Abstract
Background
The rate of teenage pregnancy in the United States is higher than in other developed nations. Teenage births result in substantial costs, including public assistance, health care costs, and income losses due to lower educational attainment and reduced earning potential.
Methods
The Contraceptive CHOICE Project was a large prospective cohort study designed to promote the use of long-acting, reversible contraceptive (LARC) methods to reduce unintended pregnancy in the St. Louis region. Participants were educated about reversible contraception, with an emphasis on the benefits of LARC methods, were provided with their choice of reversible contraception at no cost, and were followed for 2 to 3 years. We analyzed pregnancy, birth, and induced-abortion rates among teenage girls and women 15 to 19 years of age in this cohort and compared them with those observed nationally among U.S. teens in the same age group.
Results
Of the 1404 teenage girls and women enrolled in CHOICE, 72% chose an intrauterine device or implant (LARC methods); the remaining 28% chose another method. During the 2008–2013 period, the mean annual rates of pregnancy, birth, and abortion among CHOICE participants were 34.0, 19.4, and 9.7 per 1000 teens, respectively. In comparison, rates of pregnancy, birth, and abortion among sexually experienced U.S. teens in 2008 were 158.5, 94.0, and 41.5 per 1000, respectively.
Conclusions
Teenage girls and women who were provided contraception at no cost and educated about reversible contraception and the benefits of LARC methods had rates of pregnancy, birth, and abortion that were much lower than the national rates for sexually experienced teens. (Funded by the Susan Thompson Buffett Foundation and others.)
Although it has declined substantially over the past two decades, the pregnancy rate among girls and women 15 to 19 years of age remains a stubborn public health problem. Each year, more than 600,000 teens become pregnant, and 3 in 10 teens will become pregnant before they reach 20 years of age.1,2 Rates are higher among black and Hispanic teens, with 4 in 10 becoming pregnant by 20 years of age, as compared with 2 in 10 white teens.2-4 In addition to the negative health and social consequences borne by teenage mothers and their children, the national financial burden is substantial. In 2010, births involving teenage mothers cost the United States nearly $10 billion in increased public assistance and health care and in income lost as a result of lower educational attainment and reduced earnings among children born to teenage mothers.5
The President's Teen Pregnancy Prevention Initiative was launched in 2010 to address the high teenage pregnancy rate by replicating evidence-based models and innovative strategies.6 Teenage pregnancy has also been designated by the Centers for Disease Control and Prevention (CDC) as one of the six Winnable Battles because of the magnitude of the problem and the belief that it can be addressed by strategies that are known to be effective.7 The Winnable Battle target is to reduce the teenage birth rate by 20%, from 37.9 births per 1000 teens in 2009 to 30.3 per 1000 by 2015.
Long-acting, reversible contraceptive (LARC) methods, which include intrauterine devices (IUDs) and implants, have been shown to be acceptable to teens and young women, with higher continuation rates than shorter-acting methods.8,9 LARC methods reduce the likelihood of pregnancy and of repeat pregnancy among adolescents,10,11 yet less than 5% of U.S. teens report using LARC methods.12
Lack of information about effective contraception, limited access, and cost remain barriers to the use of LARC methods by teens.13-15 It is unclear whether removal of these barriers can reduce unintended pregnancy and birth rates among high-risk, sexually active teens. We assessed pregnancy, birth, and abortion rates in a cohort of teens among whom these three barriers to highly effective reversible contraception were removed, and we compared these rates with rates observed nationally among all teens in the United States.
Methods
Study Enrollment
The Contraceptive CHOICE Project was a prospective cohort study involving 9256 St. Louis area girls and women 14 to 45 years of age, in which the use of LARC methods was promoted to reduce unintended pregnancy.16 Participants were recruited through referral from medical providers, word of mouth, and study flyers. The Washington University School of Medicine in St. Louis Human Research Protection Office approved the study protocol before recruitment began, and all participants provided written informed consent. Participants 14 to 17 years of age provided written assent, and a parent or guardian provided written consent. Minors could enroll under a waiver of parental consent if they did not know the whereabouts of their parents or guardians or if they did not want their parents or guardians to know that they were seeking contraception. We enrolled four minors using the waiver.
Women and adolescent girls were eligible to participate in CHOICE if they were English-speaking or Spanish-speaking, resided in the St. Louis region or sought contraceptive services in selected community clinics, had no desire for pregnancy for at least 12 months, were sexually active or planning to be sexually active with a male partner during the next 6 months, and were not using a contraceptive method or were willing to switch to a new, reversible contraceptive method. Women and adolescent girls were ineligible if they had undergone a hysterectomy or sterilization procedure.
Study Design
CHOICE provided standardized contraceptive counseling to study participants regarding commonly used reversible contraceptive methods.17 Methods were presented in order from most to least effective, and the potential side effects, risks, and benefits of each method were reviewed. Participants were provided with their chosen method at their enrollment session in accordance with evidence-based clinical guidelines.18,19 If medical contraindications did not allow for same-day insertion of a LARC device (e.g., if pregnancy could not be ruled out definitively or if the participant had active cervicitis), participants received a shorter-acting method, such as oral contraceptive pills or depot medroxyprogesterone acetate (DMPA) injection, until their chosen method could be initiated. During the enrollment session, study staff performed a baseline interview, and participants were screened for sexually transmitted infections.
Participants were followed for 2 to 3 years, depending on their enrollment date. Telephone interviews were administered by study staff at 3 and 6 months and every 6 months thereafter. Participants received a $10 gift card after every completed follow-up survey. During the baseline and follow-up surveys, we collected detailed information regarding demographic characteristics and reproductive history, including contraceptive method use and satisfaction, sexual behavior, and pregnancy.
This analysis involves the 1404 adolescents who enrolled in CHOICE between 14 and 19 years of age, from 2007 through 2011; 716 teens were followed for 3 years, and 688 teens were followed for 2 years. At each follow-up survey, we asked participants if they had had a pregnancy. Participants who contacted study staff outside a scheduled survey or came to the clinic with concerns about possible pregnancy completed a urine pregnancy test. We recorded all pregnancies in a pregnancy log and documented the contraceptive method used at the time of conception. If the outcome of the pregnancy was known at the time of the survey (e.g., birth, miscarriage, or abortion), it was documented in the pregnancy log. If a participant was currently pregnant, we subsequently contacted her to record the pregnancy outcome.
Study Outcomes
The primary outcomes of the study were the rates of pregnancy, live birth, and induced abortion observed among participants who were 15 to 19 years of age at any time during study participation. We compared the rates in the CHOICE cohort with the most recent available rates among all U.S. teens 15 to 19 years of age, from 2010,1 and hypothesized that the rates in CHOICE would be lower than the national rates. Because the U.S. rates represent all teenage girls and women 15 to 19 years of age, including those who are and those who are not sexually experienced, we also compared the CHOICE rates with the national rates reported among sexually experienced teenage girls and women in 2008 (the most recent available data).20 In addition, we examined rates according to age and race as secondary outcomes. All analyses of rates of pregnancy, live birth, and induced abortion; teen-years of use of contraceptive methods; and failure rates of contraceptive methods included data collected when members of the cohort were 15 to 19 years of age.
Statistical Analysis
We used frequencies, percentages, medians, and ranges to describe the demographic and reproductive characteristics of the participants at the time of study enrollment. A chi-square test was performed for categorical data, and a Wilcoxon two-sample test was performed for continuous data that was not normally distributed.
For this analysis, we calculated annual means and 95% confidence intervals for rates of pregnancy, live birth, and induced abortion from 2008 through 2013, because the number of pregnancies and pregnancy outcomes that occurred among teenage CHOICE participants each year was small. Each rate represents the total number of events (i.e., pregnancy, birth, or abortion) that occurred among the participants divided by the total amount of time contributed from 2008 through 2013. For a pregnancy to be considered in the analysis, the outcome of the pregnancy (i.e., birth or abortion, for the purposes of this study) had to occur before 20 years of age. This is the same approach used by the National Center for Health Statistics in calculating U.S. rates.1 We calculated the time contributed by each participant during which she was not pregnant. If at the last survey the participant reported she had not been pregnant since the previous contact, we subtracted 6 weeks of contributed time to account for the possibility of an early-stage and unknown pregnancy. For a participant who had a pregnancy, we subtracted the total time she was pregnant plus 1 month if she delivered, to account for post-partum infecundity. For participants who were lost to follow-up, the last date of contact was the cutoff point for outcomes and contributed time. All analyses were performed with the use of Stata software, version 11 (StataCorp).
Results
Characteristics of the Participants
Table 1 gives the baseline demographic and reproductive characteristics of the 1404 teenage participants, stratified by age group at enrollment (14 to 17 years vs. 18 to 19 years). Nearly 500 minors 14 to 17 years of age were enrolled in the study. Nearly half the participants reported a previous unintended pregnancy, and 18% had a history of abortion. As compared with younger teens, those who were 18 to 19 years of age reported more lifetime male sex partners and greater parity and had a higher frequency of previous sexually transmitted infections. The majority of teens in both age groups chose LARC methods, but teens 14 to 17 years of age were more likely than older teens to do so (77.5% vs. 68.4%, P<0.001). The implant was the most common contraceptive choice for participants 14 to 17 years of age, whereas an IUD was most commonly chosen by older teens (Table 1).
Table 1. Baseline Characteristics of Study Participants Overall and According to Age Group.
| Characteristic | Total Cohort (N = 1404) | 14–17 Years of Age (N = 484) | 18–19 Years of Age (N = 920) | P Value* |
|---|---|---|---|---|
| Race — no. (%)† | <0.01 | |||
| Black | 877 (62.5) | 328 (67.8) | 549 (59.7) | |
| White | 416 (29.6) | 119 (24.6) | 297 (32.3) | |
| Other | 111 (7.9) | 37 (7.6) | 74 (8.0) | |
| Low socioeconomic status — no. (%)‡ | 623 (44.4) | 163 (33.7) | 460 (50.0) | <0.01 |
| Health insurance — no./total no. (%) | <0.01 | |||
| None | 392/1361 (28.8) | 78/453 (17.2) | 314/908 (34.6) | |
| Private | 583/1361 (42.8) | 218/453 (48.1) | 365/908 (40.2) | |
| Public | 386/1361 (28.4) | 157/453 (34.7) | 229/908 (59.3) | |
| Lifetime male sex partners — median no. (range) | 3.0 (0–175) | 2.0 (0–30) | 3.0 (0–175) | <0.01 |
| Parity — no. (%) | <0.01 | |||
| 0 | 1059 (75.4) | 397 (82.0) | 662 (72.0) | |
| 1 | 289 (20.6) | 79 (16.3) | 210 (22.8) | |
| ≥2 | 56 (4.0) | 8 (1.7) | 48 (5.2) | |
| Previous unintended pregnancy — no./total no. (%) | 671/1403 (47.8) | 219/484 (45.2) | 452/919 (49.2) | 0.16 |
| History of abortion — no. (%) | 259 (18.4) | 70 (14.5) | 189 (20.5) | <0.01 |
| History of sexually transmitted infection — no. (%)§ | 331 (23.6) | 88 (18.2) | 243 (26.4) | <0.01 |
| Baseline chosen contraceptive method — no. (%)¶ | <0.01 | |||
| Hormonal IUD | 445 (31.7) | 119 (24.6) | 326 (35.4) | |
| Nonhormonal IUD | 75 (5.3) | 14 (2.9) | 61 (6.6) | |
| Etonogestrel implant | 485 (34.5) | 242 (50.0) | 243 (26.4) | |
| DMPA injection | 127 (9.0) | 51 (10.5) | 76 (8.3) | |
| Oral contraceptive pill | 175 (12.5) | 39 (8.1) | 136 (14.8) | |
| Ring | 69 (4.9) | 11 (2.3) | 58 (6.3) | |
| Patch | 28 (2.0) | 8 (1.7) | 20 (2.2) |
P values are for the comparison between the age groups (14 to 17 vs. 18 to 19 years of age).
Race was self-reported.
Participants were classified as having low socioeconomic status if they reported current receipt of food stamps; vouchers from the Special Supplemental Nutrition Program for Women, Infants, and Children; other welfare benefits; unemployment benefits; or difficulty in paying for transportation, housing, health or medical care, or food.
Data are based on a self-reported history of chlamydia infection, gonorrhea, or trichomoniasis.
DMPA denotes depot medroxyprogesterone acetate, and IUD intrauterine device.
Pregnancy, Birth, and Abortion Rates
The 12-month, 24-month, and 36-month follow-up rates among CHOICE participants were 92%, 82%, and 75%, respectively. During 1738 teen-years of follow-up between 2008 and 2013, teens in the CHOICE cohort reported 56 pregnancies, 32 births, 16 induced abortions, 7 miscarriages, and 1 stillbirth. Reported methods used at the time of conception included the levonorgestrel IUD (2 participants), DMPA injection (1), oral contraceptive pills (13), the ring (4), the patch (2), condoms (9), and no method (25). The teen-years of use and failure rates of contraceptive methods among the participants using these methods were as follows: 394.2 teen-years and 5.1 failures per 1000 teen-years for the levonorgestrel IUD, 193.8 teen-years and 5.2 failures per 1000 teen-years for DMPA injection, 229.0 teen-years and 56.8 failures per 1000 teen-years for oral contraceptive pills, 77.2 teen-years and 51.8 failures per 1000 teen-years for the contraceptive ring, and 32.9 teen-years and 60.8 failures per 1000 teen-years for the contraceptive patch. No pregnancies occurred with the copper IUD (57.3 teen-years) or the etonogestrel subdermal implant (633.3 teen-years).
Table 2 gives the overall rates of pregnancy, live birth, and induced abortion in the CHOICE teenage cohort; respective rates for teens in the United States in 2010 are provided for comparison. The mean annual rates were 34.0 per 1000 teens (95% confidence interval [CI], 25.7 to 44.1), 19.4 per 1000 (95% CI, 13.3 to 27.4), and 9.7 per 1000 (95% CI, 5.6 to 15.8), respectively. The corresponding 2010 rates among U.S. teens nationally were 57.4, 34.4, and 14.7 per 1000.
Table 2.
Pregnancy, Birth, and Abortion Rates among Girls and Women 15 to 19 Years of Age in the CHOICE Cohort as Compared with Those in the U.S. Population.*
Among teenage girls and women enrolled in CHOICE, 97% were sexually experienced at baseline, and 99% were sexually experienced by 12 months of follow-up. Thus, Table 2 also presents a comparison of the mean annual rates in CHOICE as compared with 2008 U.S. rates representing only sexually experienced teens. The pregnancy, birth, and abortion rates per 1000 sexually experienced U.S. teens in 2008 were 158.5, 94.0, and 41.5, respectively.
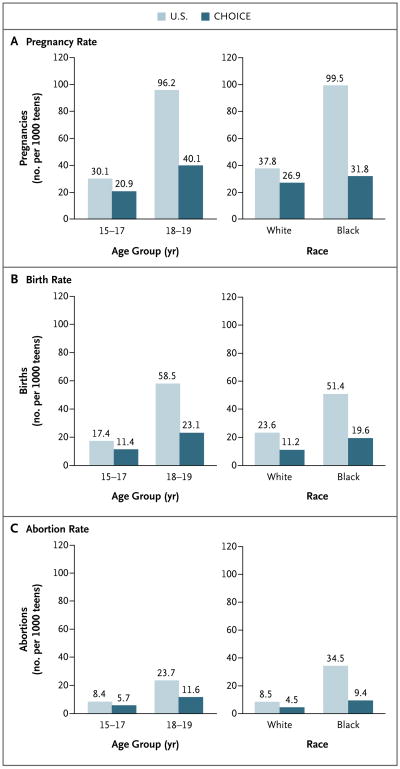
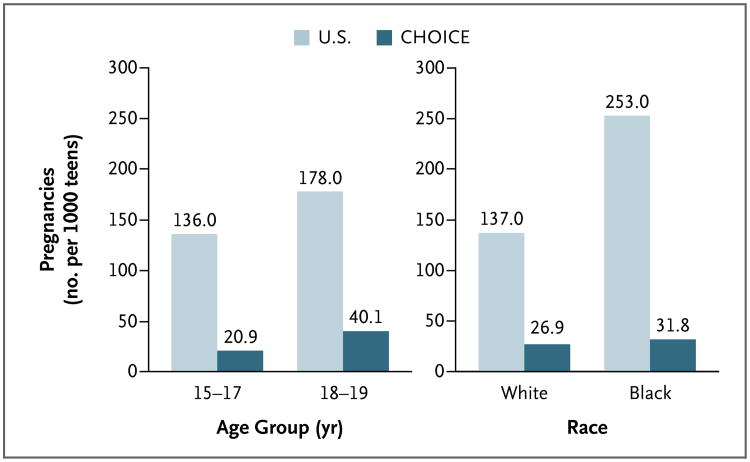
Figure 1 shows the pregnancy, birth, and abortion rates among CHOICE participants, as compared with the 2010 rates among all U.S. teens. The rates were stratified according to age group and race. For all three outcomes within each stratum, the rates among CHOICE participants were lower than the U.S. rates. The difference between rates in CHOICE and national rates was greater for those 18 to 19 years of age and among black teens. Figure 2 shows the pregnancy rates among CHOICE teens, as compared with sexually experienced U.S. teens, according to age group and race. For both age groups and both races, the CHOICE rates were substantially lower than the national rates.
Figure 1. Pregnancy, Birth, and Abortion Rates among U.S. Teenage Girls and Women, as Compared with CHOICE Participants, Stratified According to Age and Race.
Figure 2. Pregnancy Rates among Sexually Experienced U.S. Teenage Girls and Women, as Compared with CHOICE Participants, Stratified According to Age and Race.
Data for the 2008 U.S. rates stratified according to age and race are from K. Kost, Guttmacher Institute (personal communication).
Discussion
We found that pregnancy, birth, and abortion rates were low among teenage girls and women enrolled in a project that removed financial and access barriers to contraception and informed them about the particular efficacy of LARC methods. The observed rates of pregnancy, birth, and abortion were substantially lower than national rates among all U.S. teens, particularly when compared with sexually experienced U.S. teens. Stratification according to factors known to be associated with sexual behavior and pregnancy risk (age and race)21 showed that this was true among both older teens (18 to 19 years of age) and younger teens, as well as among both white and black teens.
The CDC Winnable Battle 2015 goal for teenage births is 30.3 per 1000 teens. The mean annual teenage birth rate in our cohort was 19.4 per 1000 teens, 36% lower than the 2015 goal. Our teenage pregnancy and birth rates reflect teens using highly effective contraception, with a high rate of LARC use in this cohort (i.e., 72% overall among teens). Although the rate of LARC use among teens 15 to 19 years of age in the United States has increased from less than 1% in 2002 to almost 5% in 2009, our study suggests that it is possible to achieve a much greater rate of use.12 Furthermore, teens in our cohort continued to use LARC methods longer than shorter-acting methods such as the oral contraceptive pill and DMPA injection; two thirds of teens in CHOICE were still using their LARC method at 24 months of follow-up, as compared with only one third of teens using a non-LARC method.8
The limitations of our study must be considered. First, information about pregnancy was self-reported by participants, and thus it is possible that the number of teenage pregnancies was underestimated in the CHOICE cohort. The U.S. pregnancy statistics rely on a composite of birth data, the abortion surveillance system, and self-reporting to estimate pregnancy rates. Second, teens were surveyed on a regular basis regarding their contraceptive method use, which may have influenced adherence to their contraceptive method. Third, the generalizability of our results is uncertain. Teens in CHOICE received standardized contraceptive counseling during which methods were presented in order from most to least effective. This counseling approach may differ from the usual counseling that teens receive in the United States but could certainly be applied in routine practice. Fourth, the enrollment of minors in CHOICE required parental consent. Most teens can access confidential contraceptive services without parental notification or consent, regardless of age. Minors who enrolled in CHOICE with the consent of their parent or guardian may represent a group of teens at lower risk for contraceptive nonuse and pregnancy.22 However, as compared with teens nationally, the teens enrolled in CHOICE are at greater risk for unintended pregnancy; 60% of the participants are black (vs. 16% of female teens 15 to 19 years of age in the United States),23 and almost all had had sexual intercourse at the time of enrollment, with nearly three quarters reporting sexual intercourse in the previous 30 days (vs. national frequencies of 43% and one quarter, respectively).21
A final limitation is that we compared a mean annual rate for the period from 2008 through 2013 with 2010 national rates. From 2008 to 2010, the pregnancy rate declined by 15% among all teens in the United States. The most recent birth data (2012) indicate that the birth rate among teens 15 to 19 years of age dropped to 29.4 per 1000, the lowest rate ever reported for the United States.24 (Data on national pregnancy and abortion rates are not yet available beyond 2010.) Even with this continued decline, the reductions observed in CHOICE are substantial and of public health importance.
In summary, we found that in a cohort of teenage girls and women for whom barriers to contraception (lack of knowledge, limited access, and cost) are removed and the use of the most effective contraceptive methods is encouraged, a large percentage opted to use LARC methods. The rates of pregnancy, birth, and abortion in our cohort were below both the most recent corresponding national rates and the CDC Winnable Battle 2015 goal.
Acknowledgments
Supported by grants from the Susan Thompson Buffett Foundation, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K23HD070979), and the National Center for Advancing Translational Sciences, National Institutes of Health (UL1 TR000448 and TL1 TR000449, to Washington University Institute of Clinical and Translational Sciences).
Dr. Madden reports receiving fees for serving on advisory boards from Bayer. Dr. Peipert reports receiving fees for serving on advisory boards from Bayer, Teva, MicroCHIPS, and Watson/Activis and grant support from Bayer, Teva, and Merck.
We thank Dr. Kathryn Kost and the staff of the Guttmacher Institute for providing us with data from unpublished tabulations of sexually experienced U.S. teens and guidance regarding the calculation of teen pregnancy, birth, and abortion rates.
Footnotes
A Quick Take animation is available at NEJM.org
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Institutes of Health.
Presented in part at the North American Forum on Family Planning, Seattle, October 6 and 7, 2013.
No other potential conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Kost K, Henshaw SK. US teenage pregnancies, births and abortions 2010: national and state trends by age, race and ethnicity. New York: Guttmacher Institute; 2014. http://www.guttmacher.org/pubs/USTPtrends10.pdf. [Google Scholar]
- 2.The National Campaign to Prevent Teen and Unplanned Pregnancy. Fast facts: how is the 3 in 10 statistic calculated? 2011 Feb; http://grist.files.wordpress.com/2011/10/fastfacts_3in10.pdf.
- 3.The National Campaign to Prevent Teen and Unplanned Pregnancy. Fast facts: teen pregnancy and childbearing among Latina teens. 2013 Dec; https://thenationalcampaign.org/sites/default/files/resource-primary-download/fast_facts_-_teen_pregnancy_and_child-bearing_among_latino_teens_decembe.pdf.
- 4.The National Campaign to Prevent Teen and Unplanned Pregnancy. Fast facts: teen pregnancy and childbearing among non-Hispanic black teens. 2013 Dec; http://thenationalcampaign.org/sites/default/files/resource-primary-download/fast_facts_-_teen_pregnancy_and_childbearing_among_non-hispanic_black_te.pdf.
- 5.The National Campaign to Prevent Teen and Unplanned Pregnancy. Counting it up: the public costs of teen child-bearing — key data. 2013 Dec; https://thenationalcampaign.org/sites/default/files/resource-primary-download/counting-it-up-key-data-2013-update.pdf.
- 6.Boonstra HD. Guttmacher policy review. 1. Vol. 13. New York: Guttmacher Institute; 2010. Key questions for consideration as a new federal teen pregnancy prevention initiative is implemented. [Google Scholar]
- 7.Centers for Disease Control and Prevention. Winnable Battles fact sheet. 2012 http://www.cdc.gov/winnablebattles/pdf/wb_fact_sheet_aug2012.pdf.
- 8.O'Neil-Callahan M, Peipert JF, Zhao Q, Madden T, Secura G. Twenty-four-month continuation of reversible contraception. Obstet Gynecol. 2013;122:1083–91. doi: 10.1097/AOG.0b013e3182a91f45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenstock JR, Peipert JF, Madden T, Zhao Q, Secura GM. Continuation of reversible contraception in teenagers and young women. Obstet Gynecol. 2012;120:1298–305. doi: 10.1097/aog.0b013e31827499bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366:1998–2007. doi: 10.1056/NEJMoa1110855. [DOI] [PubMed] [Google Scholar]
- 11.Tocce KM, Sheeder JL, Teal SB. Rapid repeat pregnancy in adolescents: do immediate postpartum contraceptive implants make a difference? Am J Obstet Gynecol. 2012;206(6):481.e1–7. doi: 10.1016/j.ajog.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 12.Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007-2009. Fertil Steril. 2012;98:893–7. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kavanaugh ML, Frohwirth L, Jerman J, Popkin R, Ethier K. Long-acting reversible contraception for adolescents and young adults: patient and provider perspectives. J Pediatr Adolesc Gynecol. 2013;26:86–95. doi: 10.1016/j.jpag.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kavanaugh ML, Jerman J, Ethier K, Moskosky S. Meeting the contraceptive needs of teens and young adults: youth-friendly and long-acting reversible contraceptive services in U.S. family planning facilities. J Adolesc Health. 2013;52:284–92. doi: 10.1016/j.jadohealth.2012.10.276. [DOI] [PubMed] [Google Scholar]
- 15.Secura G, McNicholas C. Long-acting reversible contraceptive use among teens prevents unintended pregnancy: a look at the evidence. Expert Rev Obstet Gynecol. 2013;8:297–9. [Google Scholar]
- 16.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203(2):115.e1–7. doi: 10.1016/j.ajog.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madden T, Mullersman JL, Omvig KJ, Secura GM, Peipert JF. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception. 2013;88:243–9. doi: 10.1016/j.contraception.2012.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.U.S. selected practice recommendations for contraceptive use, 2013: adapted from the World Health Organization selected practice recommendations for contraceptive use, 2nd edition. MMWR Recomm Rep. 2013;62(RR-5):1–46. [PubMed] [Google Scholar]
- 19.Medical eligibility criteria for contraceptive use. 3rd. Geneva: World Health Organization; 2004. [PubMed] [Google Scholar]
- 20.Kost K, Henshaw SK. US teenage pregnancies, births and abortions, 2008: national trends by age, race and ethnicity. New York: Guttmacher Institute; Feb, 2012. [Google Scholar]
- 21.Martinez G, Copen CE, Abma JC. Teenagers in the United States: sexual activity, contraceptive use, and childbearing, 2006-2010 national survey of family growth. Vital Health Stat 23. 2011;31:1–35. [PubMed] [Google Scholar]
- 22.Harper C, Callegari L, Raine T, Blum M, Darney P. Adolescent clinic visits for contraception: support from mothers, male partners and friends. Perspect Sex Reprod Health. 2004;36:20–6. doi: 10.1363/3602004. [DOI] [PubMed] [Google Scholar]
- 23.Annual estimates of the resident population by sex, age, race, and Hispanic origin for the United States and States: April 1, 2010 to July 1, 2012. http://fact-finder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=PEP_2012_PEPASR6H&prodType=table.
- 24.Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews TJ. Births: final data for 2012. Natl Vital Stat Rep. 2013;62:1–87. [PubMed] [Google Scholar]