Abstract
Adults with autism face high rates of unemployment. Supported employment enables individuals with autism to secure and maintain a paid job in a regular work environment. The objective of this study was to assess the cost-effectiveness of supported employment compared with standard care (day services) for adults with autism in the United Kingdom. Thus, a decision-analytic economic model was developed, which used outcome data from the only trial that has evaluated supported employment for adults with autism in the United Kingdom. The main analysis considered intervention costs, while cost-savings associated with changes in accommodation status and National Health Service and personal social service resource use were examined in secondary analyses. Two outcome measures were used: the number of weeks in employment and the quality-adjusted life year. Supported employment resulted in better outcomes compared with standard care, at an extra cost of £18 per additional week in employment or £5600 per quality-adjusted life year. In secondary analyses that incorporated potential cost-savings, supported employment dominated standard care (i.e. it produced better outcomes at a lower total cost). The analysis suggests that supported employment schemes for adults with autism in the United Kingdom are cost-effective compared with standard care. Further research needs to confirm these findings.
Keywords: autism, cost-effectiveness, economics, supported employment
Introduction
Autism spectrum conditions (henceforth ‘autism’) affect at least 1.1% of the adult population in England (Brugha et al., 2012). The cost of supporting people with autism is considerable. Knapp et al. (2009) estimated that the annual cost of supporting adults with autism in the United Kingdom amounted to £25 billion in 2006. A substantial part of this cost comprised staffed/supported accommodation costs, as well as productivity losses for individuals and their carers.
Adults with autism have high rates of unemployment. A survey by the National Autistic Society (NAS) in the United Kingdom reported that only 15% of adults of working age with autism are in full-time paid employment (Rosenblatt, 2008). Moreover, the majority of jobs held by adults with autism are unskilled and poorly paid (Howlin et al., 2013). Adults with autism are more likely to switch jobs frequently, have difficulty adjusting to new job settings and earn lower wages compared with typically developing peers (Howlin, 2000; Hurlbutt and Chalmers, 2004; Jennes-Coussens et al., 2006; Müller et al., 2003).
Supported employment schemes assist people with disabilities in finding and retaining jobs in order to increase their independence and improve their self-esteem. In contrast to other vocational programmes such as sheltered workshops or day services, supported employment schemes aim to involve clients in competitive rather than sheltered employment; job placements are individualised based on client preferences, strengths and work experience. Clients are supported in finding and applying for work (instead of undergoing lengthy pre-employment assessment and training, or coping with traditional interview situations); moreover, once in employment they are provided with continuing and individualised support (Bond et al., 2001).
Research on supported employment programmes for individuals with mental health problems or intellectual disabilities indicates that these schemes are superior to sheltered workshops or other day service options. Advantages include greater financial gains for the employees, wider social integration, increased worker satisfaction, higher self-esteem, more independent living, reduced family burden including a lower need for providing informal care, and service cost-savings (Beyer and Kilsby, 1996; Bond et al., 1997, 2001, 2008; Crowther et al., 2001; Graetz, 2010; Griffin et al., 1996; Heffernan and Pilkington, 2011; McCaughrin et al., 1993; Noble et al., 1991; Rhodes et al., 1987; Stevens and Martin, 1999). Specialised supported employment schemes also enable individuals with autism to secure and maintain a paid job in a regular work environment. For instance, there is evidence for significant effects of ‘Prospects’ (established by the NAS in 1994), one of the few specialised employment services for individuals with autism in the United Kingdom, on the likelihood of finding paid employment (Mawhood and Howlin, 1999). Moreover, follow-up results are suggestive of long-term beneficial effects with significant job retention 7–8 years after the initiation of the supported employment programme (Howlin et al., 2005). There is also evidence from non-UK studies on adults with autism for a positive impact of supported employment programmes on employment levels and job retention (Hillier et al., 2007; Keel et al., 1997), on autistic behaviours (Garcia-Villamisar et al., 2000), quality of life (Garcia-Villamisar et al., 2002) and executive function (Garcia-Villamisar and Hughes, 2007). The key elements associated with successful schemes include careful job placement, prior job training, advocacy, follow-up monitoring and long-term support to ensure job retention (Keel et al., 1997; Mawhood and Howlin, 1999; Trach and Rusch, 1989; Wehman and Kregel, 1985).
However, provision of supported employment schemes has considerable resource implications, especially in the current economic situation. Therefore, an economic analysis was undertaken to examine the cost-effectiveness of supported employment schemes for adults with autism in the United Kingdom from the perspective of the National Health Service (NHS) and personal social services (PSS), using decision-analytic modelling. The analysis considered two measures of outcome: the total number of weeks in employment and the quality-adjusted life year (QALY; Loomes and McKenzie, 1989). The economic model described in this article was constructed to support the development of a National Institute for Health and Care Excellence (NICE) clinical guideline on the recognition, referral, diagnosis and management of adults on the autism spectrum (National Collaborating Centre for Mental Health, 2012). The analysis presented here is an update to the guideline analysis, using most up-to-date published cost figures, and incorporating the total number of weeks in employment as an extra outcome measure.
Methods
Interventions assessed
Supported employment schemes can be delivered by a range of different providers including health, social care and third-sector organisations. The economic analysis utilised resource use estimates and unit costs available for individual placement and support (IPS) for adults with mental health problems from a NHS and PSS perspective (Curtis, 2012). IPS is an effective approach in the provision of supported employment (Heffernan and Pilkington, 2011; National Collaborating Centre for Mental Health, 2012); hence, it has been recommended in relevant guidance published by the Department of Health (2006). The economic analysis drew on the findings of a small (N = 50) quasi-experimental parallel group controlled trial that compared supported employment with standard care for adults with autism in the United Kingdom (Mawhood and Howlin, 1999). The analysis also included follow-up data for the supported employment arm of that trial reported in a separate publication (Howlin et al., 2005). This trial was selected as it is one of the very few evaluative studies of the effects of supported employment for adults with autism and the only one based in the United Kingdom. Supported employment was provided by support workers who were responsible for the assessment of clients (level of functioning, past educational and job history), for job finding and work preparation, as well as for ensuring that clients could cope with all the social and occupational requirements of employment. They also spent time educating and informing potential and existing employers, and advising work colleagues and supervisors on how to deal with or avoid problems (Mawhood and Howlin, 1999). All individuals in the comparison group had access to employment advice from Disability Employment Advisors (DEAs) based in Job Centres. The role of DEAs is to help individuals with disabilities find work or gain new skills and to conduct employment assessments to identify what type of work or training suits an individual’s profile of skills and difficulties. Due to lack of resource use data in the control group, the cost of standard care in the economic model was assumed to correspond to the cost of day services, which have been reported as an alternative to supported employment in terms of relevant resource use (Curtis, 2012).
Study population
The study population in the intervention group in Mawhood and Howlin (1999) comprised individuals with a formal diagnosis of autism and an IQ ≥ 70 on either the verbal (verbal IQ (VIQ)) or the performance (performance IQ (PIQ)) scale of the Wechsler Adult Intelligence Scale (WAIS; Wechsler, 1958); all were actively seeking work and lived within the London area. The control group included individuals with autism of similar intellectual and linguistic ability who were actively seeking work and lived in metropolitan cities outside London, with none of the cities being in areas of high unemployment. None of the participants in the trial were receiving treatment for psychiatric or other problems that might have affected their ability to work. In the intervention group, the mean (standard deviation (SD)) WAIS full-scale IQ score was 98.8 (16.3), VIQ score was 104.1 (17.3) and PIQ score was 91.6 (15.7). In the control group, the respective WAIS scores were 97.7 (16.8), 101.6 (15.8) and 92.2 (17.0). Thus, the economic analysis is directly relevant to adults with autism without intellectual disability.
Economic model structure
A simple decision-tree followed by a two-state Markov model was constructed using Microsoft Excel XP in order to assess the costs and outcomes associated with provision of supported employment versus standard care in adults with autism actively seeking employment. The structure and parameters of the decision-tree were determined by data reported in Mawhood and Howlin (1999). According to the decision-tree structure, adults with autism seeking employment were offered either supported employment or standard care (day services) over 17 months on average. As a result, a number of participants in each group found paid employment. Subsequently, a Markov model was developed to estimate the number of adults being in employment every year, from endpoint of the decision-tree (i.e. from the end of provision of the intervention) and up to 8 years, using the 8-year follow-up data reported in Howlin et al. (2005). The Markov model, which was run in yearly cycles, consisted of the states of ‘employed’ and ‘unemployed’. Each year every individual moved between the ‘employed’ and ‘unemployed’ states or remained in their current state. People in the ‘unemployed’ state of the Markov model in both arms of the analysis (i.e. people who had received supported employment and those who had received standard care while in the decision-tree) received standard care (day services). People in the ‘employed’ state of the Markov model spent only a proportion of each year (and not the full year) in employment. A schematic diagram of the economic model is presented in Figure 1.
Figure 1.
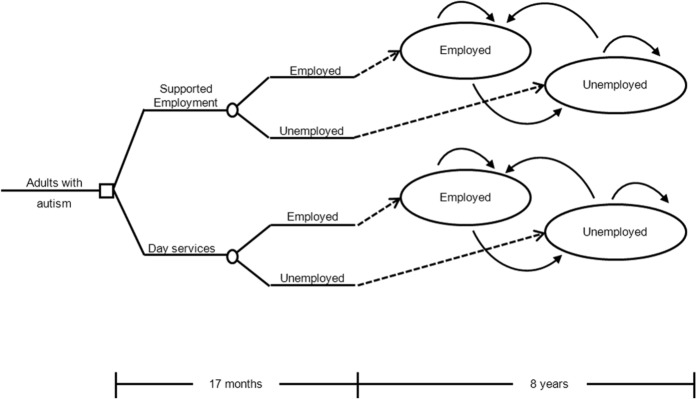
Schematic diagram of the economic model structure constructed for the assessment of the cost-effectiveness of supported employment versus standard care (day services) in adults with autism.
Clinical input parameters
Clinical input parameters for the decision-tree (i.e. the probability of employment under standard care and the relative effect of supported employment) were taken from Mawhood and Howlin (1999). Regarding the Markov component of the model, the annual transition probability from the ‘employed’ to the ‘unemployed’ health state was estimated based on 8-year follow-up data reported in Howlin et al. (2005); the annual transition probability from the ‘unemployed’ to the ‘employed’ health state was estimated using employment data for the control group in Mawhood and Howlin (1999).
It was acknowledged that people in the ‘employed’ state of the Markov model did not necessarily remain employed throughout the year. The mean proportion of actual time in employment for individuals in the ‘employed’ state was taken from Bond et al. (2008).
Utility data
A systematic search of the literature identified no studies reporting utility scores for adults with autism. In order to estimate QALYs for adults with autism being in either the ‘employed’ or the ‘unemployed’ health state, we utilised relevant data reported in Squires et al. (2012), who conducted an economic analysis to support NICE public health guidance on managing long-term sickness absence and incapacity for work (NICE, 2009). Squires et al. (2012) estimated utility scores for the health states of ‘being at work’ and ‘being on long-term sick leave’ using the findings of Peasgood et al. (2006), who transformed 36-item Short-Form Health Survey (SF-36) data derived from members of the general population participating in the British Household Panel Survey (Office for National Statistics, 2001) into Short-Form Health Survey six-dimensional health state classification (SF-6D) utility scores, using the algorithm developed by Brazier et al. (2002).
Cost data
The main analysis included only costs associated with provision of IPS and day services. In two secondary analyses, in addition to those costs, we considered (a) potential accommodation savings and (b) other NHS and PSS costs, including mental health-care costs, other primary and secondary care costs and local authority costs.
Intervention costs for supported employment and day services were based on Curtis (2012). Supported employment was assumed to be provided by specialists in Band 6 salary scale according to the NHS Agenda for Change (National Audit Office, 2009) with a caseload of 20 clients. The mean annual cost per person participating in a supported employment scheme under these conditions has been estimated at £3594 per client in 2012 (Curtis, 2012). Day services were conservatively assumed to be provided by unqualified staff in Band 3 salary scale, also at a caseload of 20 clients, at a rate of 34 sessions per year. The mean annual cost per person attending day services under these conditions has been estimated at £1938 in 2012 (Curtis, 2012).
The economic model utilised a 17-month cost for each of the interventions during the decision-tree period. Regarding the Markov component of the model, individuals in the ‘unemployed’ state were assumed to incur the annual cost of day services in every model cycle they remained unemployed, and this applied to both arms of the model (i.e. supported employment and day services).
Secondary analysis I – consideration of a shift in type of accommodation
Change in employment status may have important implications for the accommodation status of adults with autism. If gaining employment shifts a percentage of adults with autism living in supported accommodation and residential care to private accommodation, this may lead to substantial savings to PSS. This secondary analysis estimated the impact on the cost-effectiveness of supported employment following an increase in private accommodation by 1% and a reduction in supported accommodation and residential care by 0.5% each, in adults with autism who found paid employment. Accommodation costs were taken from Curtis (2012).
Secondary analysis II – inclusion of other NHS and PSS costs
The impact of supported employment on health and social care service usage by adults with autism is not known; nevertheless, Schneider et al. (2009) reported changes in costs to mental health, primary and secondary care, local authority and voluntary day care services incurred by people with mental health problems (mainly schizophrenia, bipolar disorder, anxiety or depression) associated with gaining employment after registration with supported employment schemes. Cost data from this study were used in this secondary analysis to assess the cost implications of supported employment to the NHS and PSS.
All costs were expressed in 2012 prices, uplifted, where necessary, using the Hospital and Community Health Services (HCHS) Pay and Prices Index (Curtis, 2012). Discounting1 of costs and outcomes was undertaken at an annual rate of 3.5%, as recommended by NICE (2012). Supplemental Material 1 provides the methodology details including all assumptions made in the economic model as well as the sources and values of all model input parameters.
Data analysis
To take into account the uncertainty characterising the model input parameters, a probabilistic analysis was undertaken, in which input parameters were assigned probabilistic distributions rather than being expressed as point estimates (Briggs et al., 2006). The types of distributions assigned to each input parameter and the methods employed to define their range are described in Supplemental Material 1. Subsequently, 1000 iterations were performed, each drawing random values out of the distributions fitted onto the model input parameters. Mean costs and QALYs for each intervention were calculated by averaging across 1000 iterations and were used to estimate an incremental cost-effectiveness ratio (ICER). This ratio, defined as the mean difference in costs divided by the mean difference in benefits between two interventions, expresses the additional cost per extra unit of benefit resulting from one intervention rather than the alternative. If one intervention is shown to be both less costly and more effective than its comparator, then this intervention is dominant and is clearly the cost-effective option; in such cases, no ICER needs to be estimated.
Results of probabilistic analysis are also presented in the form of cost-effectiveness acceptability curves (CEACs), which demonstrate the probability of supported employment being cost-effective relative to standard care at different levels of willingness to pay per extra unit of benefit, that is, at different cost-effectiveness thresholds (Fenwick et al., 2001).
One-way sensitivity analyses (run with the mean point estimates rather than the distributions of the input parameters) explored the impact of the uncertainty characterising the model input parameters on the main analysis: the intervention cost for supported employment and standard care was changed by ±40% to investigate whether the conclusions of the analysis would change. In addition, a threshold analysis explored the minimum relative effect of the supported employment that was required in order for the intervention to be cost-effective using the NICE cost-effectiveness threshold.
Results
Main analysis
The results of the main analysis are presented in Table 1. Supported employment is associated with a somewhat higher total cost but also results in higher numbers of weeks in employment and QALYs compared with standard care. The ICER of supported employment versus standard care is £18 per extra week in employment and £5600 per QALY; the latter is well below the NICE cost-effectiveness threshold of £20,000–£30,000/QALY (NICE, 2012) indicating that, using NICE criteria for decision-making, supported employment is a cost-effective option for adults with autism in the United Kingdom.
Table 1.
Results of main analysis: mean costs, number of weeks in employment and QALYs of supported employment and standard care per adult with autism seeking employment, over the time horizon of the analysis (17 months of intervention + 8 years follow-up)
| Mean total intervention cost over 17 months | Mean total day service cost over 8-year follow-up (incurred by unemployed only) | Mean total cost | Mean number of weeks in employment | Mean number of QALYs | |
|---|---|---|---|---|---|
| Supported employment | £5044 | £4193 | £9237 | 136 | 5.42 |
| Standard care (day services) | £2742 | £5893 | £8635 | 102 | 5.31 |
| Difference | £2302 | −£1700 | £602 | 34 | 0.11 |
| Cost-effectiveness | ICER of supported employment versus standard care: £18/extra week in employment; £5600/QALY | ||||
QALY: quality-adjusted life year; ICER: incremental cost-effectiveness ratio.
Note that numbers have been rounded to the nearest £ (costs), to the nearest integer (weeks in employment) and to the nearest second decimal digit (QALYs).
Figures 2 and 3 depict the cost-effectiveness plane showing the incremental costs and incremental benefits (weeks in employment and QALYs, respectively) of supported employment versus standard care resulting from 1000 iterations of the model. Figures 4 and 5 provide the CEACs showing the probability of supported employment being cost-effective compared with standard care (Y-axis) at different levels of willingness to pay per extra unit of benefit (weeks in employment and QALYs, respectively; X-axis). According to the CEACs, the probability of supported employment being cost-effective exceeds 50% when the willingness to pay for an extra week in employment equals £21, and reaches 80% at a willingness to pay equal to £110 per extra week in employment. The probability of supported employment being cost-effective using the NICE lower cost-effectiveness threshold of £20,000/QALY is 67.1%, while at the NICE upper cost-effectiveness threshold of £30,000/QALY, it is 75.2%.
Figure 2.
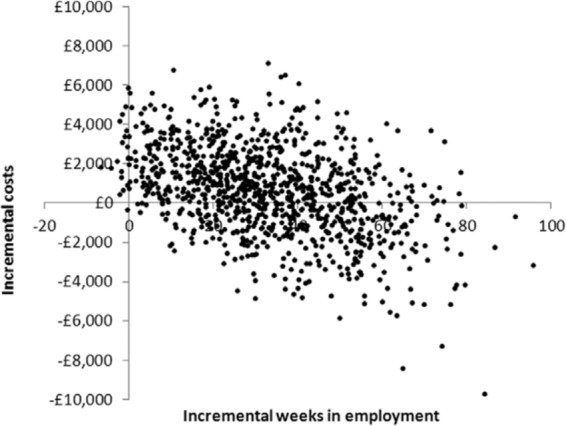
Cost-effectiveness plane showing incremental costs and weeks in employment for supported employment versus standard care per person with autism.
Results of main analysis, based on 1000 iterations.
Figure 3.
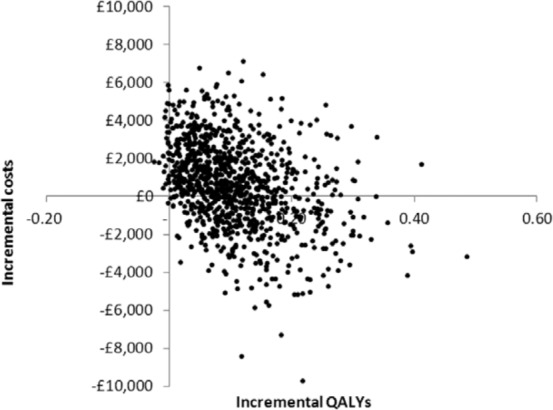
Cost-effectiveness plane showing incremental costs and QALYs of supported employment versus standard care per person with autism.
QALY: quality-adjusted life year.
Results of main analysis based on 1000 iterations.
Figure 4.
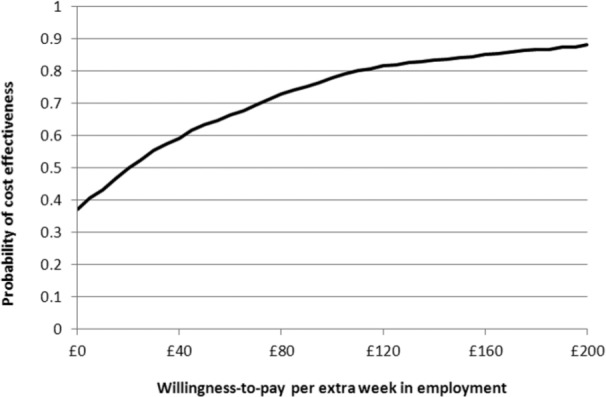
CEAC of supported employment versus standard care for different levels of willingness to pay for an extra week in employment.
CEAC: cost-effectiveness acceptability curve.
Results of main analysis.
Figure 5.
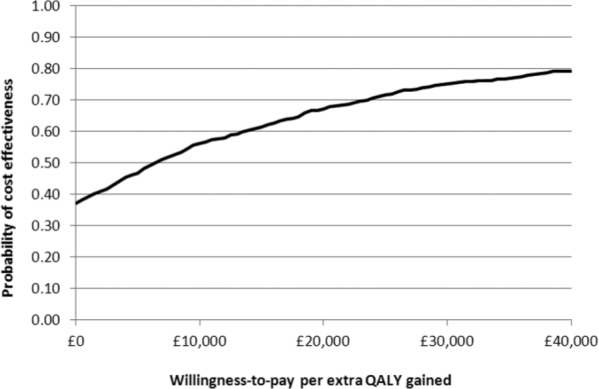
CEAC of supported employment versus standard care for different levels of willingness to pay for an extra QALY.
CEAC: cost-effectiveness acceptability curve; QALY: quality-adjusted life year.
Results of main analysis.
Secondary analyses
In both the secondary analyses, supported employment was the dominant option (more effective and overall less costly than standard care), as intervention costs were more than offset by accommodation cost-savings due to the small shift towards private accommodation (secondary analysis I), or by NHS and PSS cost-savings attributed to people finding employment (secondary analysis II). Full results of the secondary analyses are presented in Supplemental Material 2.
Sensitivity analysis
One-way sensitivity analysis demonstrated that if the intervention cost of supported employment increased by 40% or the standard care cost decreased by 40%, the ICER rose at approximately £62 per extra week in employment or £19,000/QALY, the latter being below the NICE lower cost-effectiveness threshold of £20,000/QALY. If, on the other hand, the intervention cost of supported employment fell by just 10% or the standard care cost increased by 10%, then supported employment became dominant. Threshold analysis revealed that the minimum risk ratio of supported employment versus standard care required in order for the intervention to be considered cost-effective according to NICE criteria was 1.63 (using the lower £20,000/QALY threshold), while the main analysis utilised a mean risk ratio of 2.53 (95% confidence interval (CI) = 1.13 to 5.67), as reported in Mawhood and Howlin (1999).
Discussion
The results of the economic analysis indicate that supported employment is a cost-effective intervention for adults with autism in the United Kingdom compared with standard care (day services) from an NHS and PSS perspective, as it results in better outcomes at an ICER that is below the NICE cost-effectiveness threshold. When cost-savings due to a small shift (1%) towards private accommodation or due to changes in NHS and PSS resource use associated with finding employment were considered, supported employment was the dominant option.
Clinical effectiveness data
A limitation of the economic analysis was the narrow clinical evidence base: the source trial of effectiveness data (Mawhood and Howlin, 1999) had a small sample size (N = 50); moreover, its quasi-experimental design may have introduced bias in the analysis due to confounding factors (Morgan et al., 2000). Nevertheless, the reported effect on employment of supported employment relative to standard care was strong and significant, and follow-up data indicated the longevity of the intervention effects (Howlin et al., 2005). Mawhood and Howlin (1999) reported that the intervention was also associated with higher job levels, a higher proportion of time in employment for those employed in each group and higher wages, which were not considered in the economic analysis. It has to be noted that Mawhood and Howlin (1999) assessed a supported employment scheme based in London, where employment may be easier to find; it is possible that the effectiveness of similar schemes that are operated outside large urban areas might not be as great. Nevertheless, threshold analysis revealed that supported employment would be cost-effective under NICE criteria even if the relative effect of supported employment was lower by up to approximately 30%. Moreover, although it is likely that participants in a supported employment scheme have more chances of retaining their jobs after the end of the intervention compared with those in standard care, the model conservatively assumed that the probability of retaining employment (once obtained) was the same for supported employment and standard care arms, thus potentially underestimating the clinical and cost-effectiveness of supported employment.
It should also be noted that the study by Mawhood and Howlin (1999) was conducted in the mid-1990s, and it is possible that the labour market and the circumstances of employment have changed since then. Thus, the types of jobs available and the skills required may be different, and awareness and acceptability of issues relating to autism have likely increased, so that employers may be more willing to employ people with autism. Current rates of unemployment are similar to those in the period over which the trial was conducted, approximating 8% (Office for National Statistics, 2013). Hence, the overall opportunity to obtain employment should not be very different between now and then.
Another issue for consideration is that all participants in the Mawhood and Howlin (1999) study had a verbal or performance IQ ≥ 70. Thus, our conclusions about the cost- effectiveness of supported employment are related directly to adults with autism without intellectual disability. Nevertheless, there is evidence that supported employment also has a positive effect on employment rates in adults with autism with mild or moderate intellectual disability (Schaller and Young, 2005). Therefore, we argue that the economic analysis conclusions are likely to be applicable to adults with autism across a range of intellectual abilities, and not only to those without intellectual disability.
Measures of outcome and estimation of QALYs
The analysis considered two measures of outcome. The number of weeks in employment is an outcome directly relevant to the purpose of the intervention, and probably of most interest to intervention providers as well as clients. However, reporting the analysis output as cost per extra week in employment makes it difficult to judge the cost-effectiveness of the intervention, as it is unknown how much members of society (or policy makers) value (and would be willing to pay for) an extra week in employment. For this reason, and since NICE has explicitly expressed a willingness-to-pay threshold for a QALY, outcomes were also expressed in the form of QALYs. This enables determining the cost-effectiveness of supported employment within the NICE context and in comparison with other interventions that have been evaluated within this framework.
Utility scores, which are required for the estimation of QALYs, were not available for adults with autism. Instead, we utilised utility scores obtained from the general population for the states ‘being at work’ and ‘being on sick leave’ (Squires et al., 2012). Using these data, the economic analysis is likely to have underestimated the scope for benefit of supported employment in adults with autism, as the utility of the ‘unemployed’ state is likely to be lower than the utility of ‘being on sick leave’. Moreover, it is possible that adults with autism, because they have so few other sources of social contact, may benefit relatively more from finding employment than individuals in the general population. Employment may bring to adults with autism improved self-esteem, greater access to social networks and reduced social isolation (The Sesami Research Team and Practice Partnership, 2007). It can also lead to additional improvements in quality of life and the opportunity to make use of existing skills and knowledge that otherwise would be wasted. Finally, employment of the person with autism is also likely to have a positive effect on the quality of life of their carers and the family, which was not captured in the economic analysis.
Resource use estimates and costs
Similarly to our approach in the selection of other input data, our analysis utilised conservative estimates of intervention costs that are possible to have underestimated the cost-effectiveness of supported employment. Thus, it was assumed that supported employment was provided by specialists, whereas day services were provided by unqualified staff at a minimum number of sessions per year. A conservative assumption of a small (1%) shift in accommodation following long-term employment was shown to result in overall cost-savings in a secondary analysis. If financial independence gained from finding employment leads to a more substantial shift to private accommodation, this would lead to greater savings for social services.
Schneider et al. (2009) estimated the costs incurred by people with mental health problems attending employment support schemes. Participants entering work showed a substantial decrease in mental health service costs which outweighed a slight increase that was observed in non-psychiatric secondary care, leading to a statistically significant overall reduction in health and social care costs. The authors estimated that the reduction in mental health service use was a consequence of becoming employed, although the possibility that a third variable, such as cognitive impairment, might be driving both employment outcomes and service use reduction was not ruled out. The authors concluded that mental health providers may save money if service users become employed. However, the size of the study was very small (n = 32). Moreover, adults with autism may have a different pattern of health and social care service usage compared with the study population in Schneider et al. (2009), and this was the reason why the cost data reported in this study were considered only in a secondary analysis (which, nevertheless, demonstrated the dominance of supported employment when cost-savings to the NHS and PSS were considered).
Other costs such as wages earned and the tax gains to the Exchequer were not taken into account as they were beyond the perspective of the analysis. However, a simple cost exercise showed that if every additional week in employment resulting from supported employment is costed at a weekly wage of £237, estimated based on the reported mean annual salary of people who were previously supported by employment and support allowance (ESA) due to illness or disability (Adams et al., 2012), then supported employment generates an additional £7850 in productivity gains over the roughly 9.5 years of the model duration, which far outweighs the extra cost of £601 that is associated with provision of supported employment. Furthermore, evidence from the United States suggests that adults with autism who work in the community have an overall net monetary benefit at an individual level, as they generate more monetary benefits (earned wages) than monetary costs (such as taxes paid, reduction in benefits and subsidies etc.) (Cimera and Burgess, 2011).
Evidence on the cost-effectiveness of supported employment in other populations
Our findings are overall in agreement with those of other economic studies on supported employment schemes. A systematic review of studies conducted in the United States on people with various disabilities (including mental illnesses, sensory impairments, and physical or intellectual disabilities) concluded that supported employment is more cost-effective than sheltered workshops in the long term, and returns a net benefit to the taxpayers (Cimera, 2012).
In the United Kingdom, the cost-effectiveness of supported employment versus standard care (local traditional vocational services) for people with severe mental illness has been evaluated in a randomised controlled trial (RCT; Howard et al., 2010; follow-up data in Heslin et al., 2011). In this trial, supported employment in the form of IPS was provided by an external supported non-governmental employment agency. The analysis considered health and social care costs. Supported employment and standard care were found to result in similar low rates of competitive employment (13% vs 7% at 1-year follow-up, p = 0.15; 22% vs 11% at 2-year follow-up, p = 0.053) and were no different in other secondary outcomes (such as number of hours worked per week, length of job tenure, income, job satisfaction, quality of life and self-esteem). The effect of the intervention on rates of employment was significant at 2 years (p = 0.041) after controlling for all socio-demographic factors and clinical measures at baseline. No significant differences were found in overall, service or medication costs. Based on these findings, it was concluded that supported employment was likely a cost-effective option. The authors attributed the low employment rates of supported employment (which are the lowest rates reported in trials of supported employment so far) to potential difficulties in the implementation of IPS in the UK context, where it is not structurally integrated within mental health teams, as well as to economic disincentives which lead to lower levels of motivation in programme providers, clients and prospective employers. However, the study has been criticised for its bad conduct: Latimer (2010) notes that the study by Howard et al. (2010) is the first unsuccessful trial of IPS probably because vocational workers had far fewer contacts with clients and employers than normal (an observation that justifies the surprisingly low intervention cost that was reported for IPS at £296 in 2006–2007 prices), leading to a lower level of effectiveness than might have been achieved had the intensity of IPS been optimal.
The cost-effectiveness of supported employment in people with severe mental illness has also been evaluated in a multi-centre RCT conducted across 6 European cities that compared IPS with standard vocational services (Knapp et al., 2013). The economic analysis, which had a time horizon of 18 months, considered health and social care costs; the primary outcome was the percentage of individuals who worked at least 1 day. IPS was found to be more effective than standard services at an overall lower health and social care cost, and this finding was observed in disaggregated analyses for five of the six European sites, including London. Further analysis that considered productivity gains showed that IPS resulted in a net benefit of £17,000 relative to standard services. These results suggest that IPS is a cost-effective and likely cost-saving approach to enabling people with severe mental illness to get into competitive employment, representing a more efficient use of resources than standard vocational services; these conclusions are fully in line with our findings.
Conclusion
To our knowledge, this is the first study assessing the cost-effectiveness of supported employment in adults with autism. The findings of the analysis suggest that supported employment is a cost-effective intervention for adults with autism in the United Kingdom. Although the initial costs of such schemes are higher than standard care, these reduce over time, and ultimately supported employment results not only in individual gains in social integration and well-being but also in reductions of the economic burden to health and social services, the Exchequer and the wider society. This is particularly significant given the current need in the United Kingdom to reduce the substantial costs of unemployment. Further research needs to confirm these findings. Based on the clinical and economic evidence, the NICE guideline (National Collaborating Centre for Mental Health, 2012) recommends that individual supported employment programmes be considered for adults with autism of all ranges of intellectual ability, who are having difficulty in obtaining or maintaining employment. Such programmes should be individualised but include common core elements of prior and on-the-job training, advocacy, and long-term support to ensure job retention.
Acknowledgments
We thank Jasdeep Hayre for useful comments and suggestions in the development of the economic model, Naomi Glover for assistance with data extraction and methodological assessment of included trials and Sarah Stockton for creating the search strategies and conducting the database searches used for the autism in adults guideline.
Discounting refers to the process of adjusting the value of costs or benefits that occur at different time points in the future so that they may all be compared as if they had occurred at the same time. Discounting is necessary if there is a preference to defer costs until tomorrow or to enjoy benefits today (positive time preference) (Shiell et al., 2002).
Footnotes
Declaration of conflicting interests: None.
Funding: The economic analysis presented in this article was based on previous work undertaken to inform a clinical practice guideline on the recognition, referral, diagnosis and management of adults on the autism spectrum developed by the National Collaborating Centre for Mental Health (NCCMH), commissioned and funded by the National Institute for Health and Care Excellence (NICE) in the United Kingdom. S.P. receives funding from NICE for the production of clinical guidelines. I.M., O.M.-V., N.C. and S.P. were paid by the NCCMH to undertake the development of autism in adults guideline. S.B.-C. received an honorarium as Chair of the Guideline Development Group (GDG). P.H. was a GDG member.
References
- Adams L, Oldfield K, Riley K, et al. (2012) Destinations of Jobseeker’s Allowance, Income Support and Employment and Support Allowance Leavers 2011. Sheffield: Department of Work and Pensions. [Google Scholar]
- Beyer S, Kilsby M. (1996) The future of employment for people with learning disabilities: a keynote review. British Journal of Learning Disabilities 24: 134–137. [Google Scholar]
- Bond GR, Becker DR, Drake RE, et al. (2001) Implementing supported employment as an evidence-based practice. Psychiatric Services 52: 313–322. [DOI] [PubMed] [Google Scholar]
- Bond GR, Drake RE, Becker DR. (2008) An update on randomized controlled trials of evidence-based supported employment. Psychiatric Rehabilitation Journal 31: 280–290. [DOI] [PubMed] [Google Scholar]
- Bond GR, Drake RE, Mueser KT, et al. (1997) An update on supported employment for people with severe mental illness. Psychiatric Services 48: 335–346. [DOI] [PubMed] [Google Scholar]
- Brazier J, Roberts J, Deverill M. (2002) The estimation of a preference-based measure of health from the SF-36. Journal of Health Economics 21: 271–292. [DOI] [PubMed] [Google Scholar]
- Briggs A, Sculpher M, Claxton K. (2006) Decision Modelling for Health Economic Evaluation. New York: Oxford University Press. [Google Scholar]
- Brugha T, Cooper SA, McManus S, et al. (2012) Estimating the Prevalence of Autism Spectrum Conditions in Adults: Extending the 2007 Adult Psychiatric Morbidity Survey. London: NHS, The Health and Social Care Information Centre. [Google Scholar]
- Cimera RE. (2012) The economics of supported employment: what new data tell us. Journal of Vocational Rehabilitation 37: 109–117. [Google Scholar]
- Cimera RE, Burgess S. (2011) Do adults with autism benefit monetarily from working in their communities? Journal of Vocational Rehabilitation 34: 173–180. [Google Scholar]
- Crowther R, Marshall M, Bond G, et al. (2001) Vocational rehabilitation for people with severe mental illness. The Cochrane Database of Systematic Reviews 2: CD003080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis L. (2012) Unit Costs of Health & Social Care 2012. Canterbury: Personal Social Services Research Unit, University of Kent. [Google Scholar]
- Department of Health (2006) Vocational Services for People with Severe Mental Health Problems: Commissioning Guidance. London: CSIP for Department of Work and Pensions and Department of Health. [Google Scholar]
- Fenwick E, Claxton K, Sculpher M. (2001) Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Economics 10: 779–787. [DOI] [PubMed] [Google Scholar]
- Garcia-Villamisar D, Hughes C. (2007) Supported employment improves cognitive performance in adults with Autism. Journal of Intellectual Disability Research 51: 142–150. [DOI] [PubMed] [Google Scholar]
- Garcia-Villamisar D, Ross D, Wehman P. (2000) Clinical differential analysis of persons with autism in a work setting: a follow-up study. Journal of Vocational Rehabilitation 14: 183–185. [Google Scholar]
- Garcia-Villamisar D, Wehman P, Navarro MD. (2002) Changes in the quality of autistic people’s life that work in supported and sheltered employment. A 5-year follow-up study. Journal of Vocational Rehabilitation 17: 309–312. [Google Scholar]
- Graetz JE. (2010) Autism grows up: opportunities for adults with autism. Disability and Society 25: 33–47. [Google Scholar]
- Griffin DK, Rosenberg H, Cheyney W. (1996) A comparison of self-esteem and job satisfaction of adults with mild mental retardation in sheltered workshops and supported employment. Education and Training in Mental Retardation and Developmental Disabilities 31: 142–150. [Google Scholar]
- Heffernan J, Pilkington P. (2011) Supported employment for persons with mental illness: systematic review of the effectiveness of individual placement and support in the UK. Journal of Mental Health 20: 368–380. [DOI] [PubMed] [Google Scholar]
- Heslin M, Howard L, Leese M, et al. (2011) Randomized controlled trial of supported employment in England: 2 year follow-up of the Supported Work and Needs (SWAN) study. World Psychiatry 10: 132–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillier A, Campbell H, Mastriani K, et al. (2007) Two-year evaluation of a vocational support program for adults on the autism spectrum. Career Development for Exceptional Individuals 30: 35–47. [Google Scholar]
- Howard LM, Heslin M, Leese M, et al. (2010) Supported employment: randomised controlled trial. British Journal of Psychiatry 196: 404–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlin P. (2000) Outcome in adult life for more able individuals with autism or Asperger syndrome. Autism 4: 63–83. [Google Scholar]
- Howlin P, Alcock J, Burkin C. (2005) An 8 year follow-up of a specialist supported employment service for high-ability adults with autism or Asperger syndrome. Autism 9: 533–549. [DOI] [PubMed] [Google Scholar]
- Howlin P, Moss P, Savage S, et al. (2013) Social outcomes in mid- to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. Journal of the American Academy of Child & Adolescent Psychiatry 52: 572–581. [DOI] [PubMed] [Google Scholar]
- Hurlbutt K, Chalmers L. (2004) Employment and adults with Asperger syndrome. Focus on Autism and Other Developmental Disabilities 19: 215–222. [Google Scholar]
- Jennes-Coussens M, Magill-Evans J, Koning C. (2006) The quality of life of young men with Asperger syndrome: a brief report. Autism 10: 403–414. [DOI] [PubMed] [Google Scholar]
- Keel JH, Mesibov GB, Woods AV. (1997) TEACCH-supported employment program. Journal of Autism and Developmental Disorders 27: 3–9. [DOI] [PubMed] [Google Scholar]
- Knapp M, Patel A, Curran C, et al. (2013) Supported employment: cost-effectiveness across six European sites. World Psychiatry 12: 60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knapp M, Romeo R, Beecham J. (2009) Economic cost of autism in the UK. Autism 13: 317–336. [DOI] [PubMed] [Google Scholar]
- Latimer E. (2010) An effective intervention delivered at sub-therapeutic dose becomes an ineffective intervention. British Journal of Psychiatry 196: 341–342. [DOI] [PubMed] [Google Scholar]
- Loomes G, McKenzie L. (1989) The use of QALYs in health care decision making. Social Science & Medicine 28: 299–308. [DOI] [PubMed] [Google Scholar]
- McCaughrin WB, Ellis WK, Rusch FR, et al. (1993) Cost-effectiveness of supported employment. Mental Retardation 31: 41–48. [PubMed] [Google Scholar]
- Mawhood L, Howlin P. (1999) The outcome of a supported employment scheme for high functioning adults with autism or Asperger syndrome. Autism 3: 229–254. [Google Scholar]
- Morgan GA, Gliner JA, Harmon RJ. (2000) Quasi-experimental designs. Journal of the American Academy of Child and Adolescent Psychiatry 39: 794–796. [DOI] [PubMed] [Google Scholar]
- Müller E, Schuler A, Burton BA, et al. (2003) Meeting the vocational support needs of individuals with Asperger syndrome and other autism spectrum disabilities. Journal of Vocational Rehabilitation 18: 163–175. [Google Scholar]
- National Audit Office (2009) NHS Pay Modernisation in England: Agenda for Change. London: The Stationary Office. [Google Scholar]
- National Collaborating Centre for Mental Health (2012) Autism: Recognition, Referral, Diagnosis and Management of Adults on the Autism Spectrum. Leicester and London: The British Psychological Society and The Royal College of Psychiatrists. [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence (NICE) (2009) Managing Long-Term Sickness Absence and Incapacity for Work. London: NICE public health guidance 19; Available at: http://guidance.nice.org.uk/PH19 [Google Scholar]
- National Institute for Health and Clinical Excellence (NICE) (2012) Process and Methods Guides. The Guidelines Manual. London: NICE. [Google Scholar]
- Noble J, Conley RW, Banerjee S, et al. (1991) Supported employment in New York State: a comparison of benefits and costs. Journal of Disability Policy Studies 2: 39–73. [Google Scholar]
- Office for National Statistics (2001) General Household Survey. London: The Stationary Office. [Google Scholar]
- Office for National Statistics (2013) Labour Force Survey. Table A02: Summary of Employment, Unemployment and Economic Inactivity for People Aged from 16 to 64. London: Office for National Statistics; Available at: http://www.ons.gov.uk [Google Scholar]
- Peasgood T, Roberts J, Tsuchiya A. (2006) Incapacity Benefit: A Health or Labour Market Phenomenon? Sheffield: Department of Economics, University of Sheffield. [Google Scholar]
- Rhodes L, Ramsing K, Hill M. (1987) Economic evaluation of employment services: a review of applications. Journal of the Association for Persons with Severe Handicaps 12: 175–181. [Google Scholar]
- Rosenblatt M. (2008) I Exist: The Message from Adults with Autism in England. London: National Autistic Society. [Google Scholar]
- Schaller J, Young N. (2005) Competitive employment for people with autism: correlates of successful closures in competitive employment and supported employment. Rehabilitation Counseling Bulletin 49: 4–16. [Google Scholar]
- Schneider J, Boyce M, Johnson R, et al. (2009) Impact of supported employment on service costs and income of people. Journal of Mental Health 18: 533–542. [Google Scholar]
- Shiell A, Donaldson C, Mitton C, et al. (2002) Health economic evaluation. Journal of Epidemiology and Community Health 56: 85–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squires H, Rick J, Carroll C, et al. (2012) Cost-effectiveness of interventions to return employees to work following long-term sickness absence due to musculoskeletal disorders. Journal of Public Health (Oxford, England) 34: 115–124. [DOI] [PubMed] [Google Scholar]
- Stevens P, Martin N. (1999) Supporting individuals with intellectual disability and challenging behaviour in integrated work settings: an overview and a model for service provision. Journal of Intellectual Disability Research 43(Pt 1):19–29. [DOI] [PubMed] [Google Scholar]
- The Sesami Research Team and Practice Partnership (2007) The SESAMI evaluation of employment support in the UK: background and baseline data. Journal of Mental Health 16: 375–388. [Google Scholar]
- Trach JR, Rusch FR. (1989) Supported employment program evaluation: evaluating degree of implementation and selected outcomes. American Journal of Mental Retardation 94: 134–140. [PubMed] [Google Scholar]
- Wechsler D. (1958) The Measurement and Appraisal of Adult Intelligence. Baltimore, MD: Williams & Witkins. [Google Scholar]
- Wehman P, Kregel J. (1985) A supported work approach to competitive employment for individuals with moderate and severe handicaps. Journal of the Association for Persons with Severe Handicaps 10: 3–11. [Google Scholar]


