Abstract
Objective
This study examined trajectories of posttraumatic stress disorder symptoms in Hurricane Katrina affected youth.
Method
A total of 426 youth (51% female; 8–16 years old; mean age=11 years; 75% minorities) completed assessments at 4 time points post-disaster. Measures included Hurricane impact variables (initial loss/disruption and perceived life threat); history of family and community violence exposure, parent and peer social support, and post-disaster posttraumatic stress symptoms.
Results
Latent class growth analysis demonstrated that there were three distinct trajectories of posttraumatic stress disorder symptoms identified for this sample of youth (resilient, recovering, and chronic, respectively). Youth trajectories were associated with Hurricane-related initial loss/disruption, community violence, and peer social support.
Conclusions
The results suggest that youth exposed to Hurricane Katrina have variable posttraumatic stress disorder symptom trajectories. Significant risk and protective factors were identified. Specifically, youth Hurricane and community violence exposure increased risk for a more problematic posttraumatic stress disorder symptom trajectory, while peer social support served as a protective factor for these youth. Identification of these factors suggests directions for future research as well as potential target areas for screening and intervention with disaster exposed youth.
Limitations
The convenience sample limits the external validity of the findings to other disaster exposed youth, and the self-report data is susceptible to response bias.
Keywords: Posttraumatic stress symptoms, Children, Disasters, Growth mixture modeling
0. Introduction
An estimated 14% of American youth experience a disaster during their childhood (Becker-Blease et al., 2010). Disaster-exposed youth are at risk for developing symptoms of posttraumatic stress disorder (PTSD), (Norris et al., 2002; Osofsky et al., 2009; Yelland et al., 2010). Research on the longitudinal course of youth PTSD following disasters indicate that the majority of symptoms remit in the months and years following the event (Kronenberg et al., 2010); however, persistence or worsening of symptoms also has been documented (e.g., Bokszczanin, 2007; Goenjian et al., 2005; John et al., 2007; Lai et al., in press).
Hurricane Katrina was one of the worst natural disasters in U.S. history in terms of death, destruction, and delayed recovery (Knabb et al., 2006). Researchers studying youth who experienced Katrina have found variability in post-trauma symptoms. For instance, Marsee (2008) found that 63% of youth reported symptoms of PTSD 15–18 months post-Katrina, while 27% reported no symptoms. In comparison, Kronenberg et al. (2010) found that 45% of youth did not meet the clinical cutoff for symptoms at either a two or three year post-Katrina assessment time point, and 27% who initially met the clinical cutoff at year two, were recovered one year later. However, there were some youth who exhibited more chronic pattern trajectories, with 23% of youth demonstrating no reductions in symptoms over time, and 4% had an increase in symptoms. These findings are commensurate with how (Bonanno and Mancini, 2008) conceptualize post-disaster adult recovery patterns, in terms of resilience (absence of elevated PTSD symptoms), recovery (initially elevated PTSD symptoms that decline to adaptive functioning levels), chronic dysfunction (elevated PTSD symptoms that do not abate with time), and delayed trauma (PTSD symptoms increase over time to elevated levels).
To date, published research examining post-disaster outcomes in youth over time has relied on analytic strategies that permit assessment of mean-level changes in PTSD symptoms. This approach does not allow characterization of differing trajectories of more chronic and less symptomatic children. Growth mixture modeling is an analytic approach that allows for explication of differing trajectories (Curran and Hussong, 2003; Muthén and Asparouhov, 2008), as well as factors associated with each trajectory. This approach has been increasingly utilized in the adult trauma and PTSD symptom literature (e.g., Dickstein et al., 2010; Elliott et al., 2005; Galatzer-Levy et al., 2011; Orcutt et al., 2004), with results indicating significant heterogeneity in trajectories of PTSD symptoms over time.
Although growth mixture modeling has not yet been applied to studying youth after natural disasters, a few emerging studies have used these techniques with youth exposed to other types of trauma (e.g., Amstadter et al., 2009; Le Brocque et al., 2010; Nugent et al., 2009). For example, Nugent and colleagues (2009) examined latent class trajectories of PTSD symptoms in youth ages 7 to 18 years who had been exposed to family violence. Results indicated a resilient trajectory group and a persistent symptom trajectory group. Similarly, Le Brocque et al., 2010 used this approach to examine the course of PTSD symptoms for youth following an accidental injury. Three trajectories emerged, including youth who were resilient following the accident, those who initially experienced high levels of stress but recovered quickly, and, lastly, those with chronic stress patterns. Collectively, these studies support the notion that youth response to trauma is not homogenous, and that the distinct PTSD trajectory paths emerge.
Patterns of post-disaster recovery in youth are impacted by multiple factors that can serve to enhance the risk of negative trajectories or promote resilience (Weems and Overstreet, 2008), and such factors can be important in distinguishing PTSD trajectories. Similar to prior research examining youth outcomes post-disaster (e.g., La Greca et al., 1998; La Greca et al., 2010; Vernberg et al., 1996; Russoniello et al., 2002; Neuner et al., 2006), emerging research evaluating Katrina-affected youth indicate differential outcomes based on individual-level and microsystem-level (i.e., family and other systems in the child’s immediate environment, Brofenbrenner, 1979) risk and protective factors. For instance, several studies have indicated that individual-level factors, such as Hurricane loss and life disruption following Katrina, are associated with youth-reported posttraumatic stress symptoms (Kelley et al., 2010; Rowe et al., 2010). Furthermore, Weems et al. (2007) found that youth pre-disaster anxiety and negative affect significantly influenced Katrina-related posttraumatic stress symptoms. In regard to microsystem-level factors, (Kronenberg et al., 2010) found that life stressors, including school and family problems, increased risk for poor long-term outcomes post-Katrina, while Kelley and colleagues (2010) found that violence exposure and parent behavior significantly impacted youth PTSD symptoms.
The aim of the current study was to identify trajectories of youth’s PTSD symptoms following Hurricane Katrina, as well as risk and protective factors associated with each trajectory. In terms of risk, youth-reported disaster loss and disruption, as well as youth exposure to other traumatic events, specifically, home and community violence, were examined. Parental and peer social support, which researchers have found to be associated with positive youth post-disaster outcomes (Khoury et al., 1997; La Greca et al., 1996), were examined as potential protective factors. Latent Class Growth Analysis, a subset of growth mixture modeling, was employed to identify youth’s varying PTSD symptom trajectories. Based on prior research, we hypothesized that distinct PTSD symptom trajectories would emerge among Hurricane Katrina-exposed youth, and that youth who reported higher levels of Hurricane loss/disruption and violence exposure, as well as lower levels of social support, would be at greatest risk for a chronic and persistent PTSD symptom trajectory.
1. Method
1.1. Participants
Participants were 426 children living in New Orleans and the surrounding area when Hurricane Katrina made landfall. The majority were displaced from their home as a result of the Hurricane (75%). Children (51% female) ranged in age from 8 to 16 years old (M=11.63 years; SD=2.26) and were in grades 4–8 at Time 1. Children were primarily African American (68%), with 25% identifying as Caucasian, and 7% as other ethnicities. Median income prior to Hurricane Katrina was below $25,000; 56% of children came from single-parent households. Children in special education were excluded.
1.2. Procedures
After obtaining approval from Louisiana State University’s Institutional Review Board, principals from six schools were contacted regarding recruitment of participants for the study. Children and their parents were recruited as part of a multi-wave, longitudinal study on the psychological impact of Hurricane Katrina. Interested parent participants received a packet containing information about the study, the consent forms (for parent and child), and self-report questionnaires. Parents completed and returned consent forms and self-report questionnaires to their child’s school in a sealed envelope. Children completed questionnaires in small groups at school. Data collection was conducted by graduate students and research assistants trained in data collection procedures including explaining informed consent, assent, and the limits of confidentiality and administering questionnaires. In addition, research assistants were available to assist children with reading difficulties.
Questionnaires were administered at four time points: Time 1 was conducted at 3 months post-Katrina; Time 2 was conducted at 13 months post-Katrina; Time 3 was conducted 19 months post-Katrina; and Time 4 was conducted at 25 months post-Katrina. Subsequent to Time 1, parents were contacted regarding their continued participation and to obtain updated contact information.
Compensation was provided in several ways. At Time 1, children were provided compensation at the discretion of school personnel. This included entry into one of several $5.00 drawings or a class pizza party. During subsequent waves of the study, parents were compensated $25.00–$50.00 for participation, and children were provided with small items such as stickers or pencils.
Of the families contacted regarding their interest in the study, approximately 35% consented and completed questionnaires. At Time 1, 388 children participated in the study. An additional 38 children began participating at Time 2, but no additional participants were added during Times 3 or 4. Of the total 426 participants, (including those who first participated at Time 2) nine participants did not provide responses about their PTSD symptoms. Given that PTSD symptom severity was the primary outcome measure of this study, these nine participants were not included in the analyses. Thus, 417 participants were analyzed in this study. The number of participants who completed the UCLA PTSD Reaction Index—Revision 1 at each wave are as follows: Time 1=346 (83%); Time 2=356 (85%); Time 3=345 (83%); Time 4=331 (79%). The majority of participants completed measures at either 3 or 4 time points: 238 (57%) completed four time points; 105 (25%) completed three time points; 37 (9%) completed two time points; and 37 (9%) completed only one time point.
Demographic characteristics (gender, income, race, age) were examined to determine whether differences emerged for number of time points participants completed according to any of these variables. No significant differences were found for gender, income or race. A one-way ANOVA examining age and number of time points completed revealed a significant difference F(3, 412)=3.548, p=.02; however, post-hoc comparisons (Tukey HSD) showed only a trend such that children completing one time point were slightly older (M=12.19 years) than children who completed all four time points (M=11.51 years), p=.10.
1.3. Measures
1.3.1. Posttraumatic stress
The UCLA PTSD Reaction Index-Revision 1 (Pynoos et al., 1998) contains 18 items assessing 17 symptoms of PTSD in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition-Text Revision (DSM-IV-TR), American Psychiatric Association, 2000). Youth rated their symptoms based on their experiences related to Hurricane Katrina; symptoms were rated on a 5-point scale (0=none of the time; 4=most of the time). Two items assessed emotional numbing (items 10 and 11). The more severe score for either of these items was included when calculating total summary scores. Summary scores (possible range=0 to 68) were used to indicate PTSD symptom levels. The psychometric properties of this scale are good (see Steinberg et al., 2004), and its use in disaster-affected youth has been established (Kelley et al., 2010; Weems et al., 2010; Yelland et al.,2010). Internal consistency in the current sample was excellent across all four waves (α=.91–.93)
1.3.2. Immediate loss and disruption
The immediate loss and disruption subscale of the Hurricane-related traumatic events scale (La Greca et al., 1996; Vernberg et al.,1996) was used to assess children’s experience of loss and disruption events following Hurricane Katrina. Nine items (rated yes/no) assessed loss and disruption related to the Hurricane (e.g., having to change schools).
1.3.3. Violence exposure
The screen for adolescent violence exposure (SAVE), (Hastings and Kelley, 1997) is a 32-item, self-report questionnaire for adolescents 11–16 years old. It contains three subscales: home, school and community violence. Item frequency is rated on a on a five-point scale (0=never, 4=almost always). In this study, the home violence and community violence scales were used. Previous research has shown that the SAVE has adequate psycho-metric properties (Hastings and Kelley, 1997). Children in the 7th and 8th grades completed the SAVE. Coefficient alpha for home violence=.92 and for community violence=.96 in the current sample.
The KID-SAVE (Flowers et al., 2000) is a measure of violence exposure in younger children adapted from the SAVE. The KID-SAVE has been validated in samples with children ages 8–11 years. The KID-SAVE contains 35 items and has three scales (home, school and community violence). Home violence and community violence were used in this study. Children in the 4th through 6th grade completed the KID-SAVE. Coefficient alpha for home violence=.58 and for community violence=.92. Due to the differences in the number of items per scale, children’s scores on the home violence and community violence subscales of the SAVE and KID-SAVE were converted to z-scores.
1.3.4. Social support
The social support scale for children (SSSC), (Harter, 1985) is a widely-used, self-report measure of social support in children. It contains 24-items examining social support from four sources: parents, teachers, close friends and classmates. For each item, children selected one of two statements and then rated the statement as being either, “really true for me,” or “sort of true for me.” In an initial validation sample (Harter, 1985), three factors emerged: parent, teacher and peer social support (which combined items related to classmates and peers). In the current study, only the parent and peer social support scales were used (α=.74 for Parent support and α=.73 for peer support).
1.4. Analytic approach
Latent class growth analysis (LCGA) was conducted in Mplus (version 6.11) to identify distinct trajectories of PTSD symptoms. LCGA is a person-centered analysis and a subset of growth mixture modeling that does not allow variation to occur around mean growth curves within latent classes (Jung and Wickrama, 2008). Form for PTSD symptom curves was determined by first using conventional polynomial growth models testing linear and quadratic growth. We selected a linear form due to estimation difficulties in modeling quadratic growth, and we utilized LCGA due to estimation difficulties encountered in attempts to allow within-trajectory class variation in intercepts and slopes. Mplus employs maximum likelihood estimation for LCGA (Muthen and Muthen, 1998–2007). For a reliable model, the minimum recommended covariance coverage is .10 (Muthen and Muthen, 1998–2007). In this study, missing data coverage fell within acceptable levels, ranging from .64 to .85.
To identify the number of trajectory groups within our data, unconditional LCGA models (i.e., models that did not include risk and protective factors) for one to four trajectory group models were run. The best fitting model was chosen based upon fit indices, prior research, parsimony, and interpretability. Models were judged to have better fit and more accurate assignment of children to trajectory groups if they had a lower Akaike information criterion (AIC), lower Bayesian information criterion (BIC), lower sample size adjusted BIC, higher entropy, higher posterior probabilities, a significant Lo-Mendell-Rubin likelihood ratio test (LMR-LRT), and a significant bootstrap likelihood ratio test (BLRT) (Jung and Wickrama, 2008).
Using the model chosen from the previous step, conditional LCGA models (i.e., models containing risk and protective factors) were run, regressing trajectory group membership on risk and protective factors, chosen a priori.
2. Results
2.1. Preliminary analyses
Mean-level analysis of PTSD symptoms for all participants in this study showed a decline in severity across all time points. The average score at Time 1 (M=18.13, SD=14.57) fell within the mild range, according to published cutoff scores. Time 2 (M=14.41, SD=12.96) and Time 3 (M=12.53, SD=12.66) scores also fell within the mild range; however, by Time 4, scores had decreased to 10.57 (SD=11.18) which falls within the doubtful range. This pattern is similar to other studies showing a decline in symptom severity post-disaster (Kronenberg et al., 2010; La Greca et al., 1996).
Preliminary analysis of immediate loss/disruption due to the Hurricane showed that 86% of youth reported at least one loss/disruption event, but the average number of loss/disruption items endorsed was 3.10 (SD=2.28). These numbers compare to results found by Lai et al. (In Press) in youth affected by Hurricane Ike (1996), La Greca et al. (1996) after Hurricane Andrew. The most commonly reported events were difficulty seeing friends (60%) and having to go to a new school (52%).
With regard to violence exposure, item frequencies were compared for home and community violence on the SAVE and KID-SAVE. For youth who completed the SAVE, 66% endorsed experiencing at least one item as “sometimes” or more frequently on the home violence scale, and 85% endorsed at least one item as “sometimes” or more frequently on the community violence scale. SAVE items endorsed by at least half of participants include: “I have seen the police arrest someone in my neighborhood,” and “I have seen people scream at each other in my neighborhood.” In addition, over one-quarter of children endorsed, “I have heard of someone getting killed in my neighborhood.” On the KID-SAVE, 20% of youth endorsed at least one item as occurring, “sometimes,” or more often, on the home violence scale, and 62% endorsed at least one item on the community violence scale. KID-SAVE items reported as occurring at least “sometimes” by 50% or more of participants include: “Grown-ups scream at me at home,” “I have seen the police arrest someone,” “I have seen someone get badly hurt,” “I have seen a grown-up hit a kid,” I have seen people scream at each other,” “I have heard about someone getting killed,” “I have seen someone getting beat-up,” and “I have heard about someone getting shot.” In terms of protective factors, youth reported moderate levels of peer (M=3.08, SD=.68) and parent support (M=3.26, SD=.76), where scores ranged from one to four, a higher score indicating greater support. These results are similar to those found in other disaster studies (La Greca et al., 1996).
2.2. Identifying the trajectories
2.2.1. Unconditional models
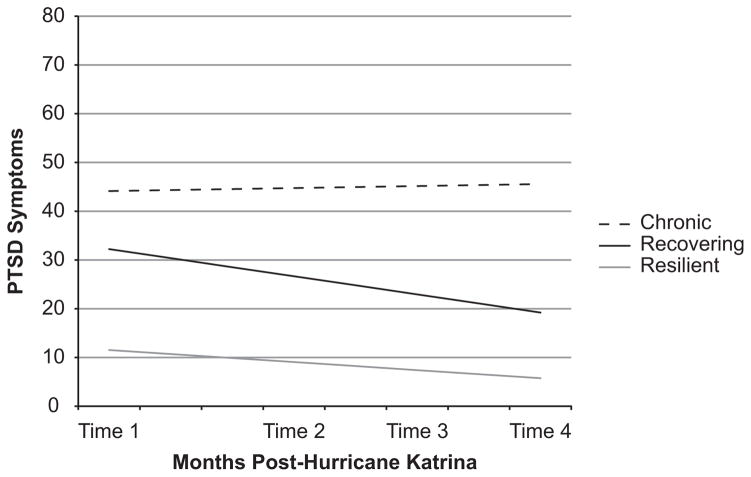
Unconditional LCGA models for one to four trajectory group solutions were run (see Table 1). The three trajectory group solution was chosen based upon fit indices, interpretability, and theory. With regard to fit, this solution had a comparatively lower AIC, BIC, and sample-size adjusted BIC values. Entropy and posterior probabilities were reasonably high for this solution. Further, this solution contained trajectories that were of substantive interest. These trajectories closely fit theoretical trajectories identified among disaster affected adults (Bonanno et al., 2010, 2006; Orcutt et al., 2004). The trajectories were named: (a) Chronic (4%), (b) Recovering (27%), and (c) Resilient (70%).
Table 1.
Fit indices and group assignment accuracy for unconditional LCGA models.
| Number of trajectory groups | AIC | BIC | Sample size adjusted BIC | Entropy | Posterior probabilities | LMR-LRT | BLRT | Smallest group n |
|---|---|---|---|---|---|---|---|---|
| 1 Group | 10946.28 | 10970.48 | 10951.44 | 1 | 1 | N/A | N/A | 417 |
| 2 Groups | 10498.98 | 10535.28 | 10506.72 | .86 | .91–.97 | <.01 | <.001 | 90 |
| 3 Groups | 10361.08 | 10409.48 | 10371.40 | .86 | .87–.97 | .21 | 1 | 15 |
| 4 Groups | 10295.24 | 10355.74 | 10308.14 | .86 | .85–.95 | .06 | 1 | 4 |
Note. AIC=Akaike Information Criterion, BIC=Bayesian Information Criterion, LMR-LRT=Lo-Mendell-Rubin Likelihood Ratio Test, and BLRT=Bootstrap Parametric Likelihood Ratio Test. Entropy, LMR-LRT, and BLRT values are not available (N/A) for single group models.
Two and four-trajectory group solutions also were considered. The two-trajectory group solution had significant LMR-LRT and BLRT values, but this solution did not contain a chronic trajectory. Chronic trajectories were of substantive interest, as identifying factors related to Chronic trajectories are necessary for informing early intervention strategies. The four-trajectory group solution had the smallest AIC, BIC, and sample-size adjusted BIC values, as well as a significant LMR-LRT. However, this solution contained a very small trajectory group, which we labeled “Chronic,” of only four children, and the trajectories identified did not closely match theory.
2.3. Predicting trajectory group membership
After selection of the unconditional three-trajectory group solution, we ran a conditional model adding risk factors (i.e., immediate loss/disruption, home violence, community violence) and protective factors (i.e., parent social support, peer social support) as predictors of trajectory group membership.
Descriptive information from this conditional model is provided in Table 2, and the trajectory groups are depicted in Fig. 1. To characterize average slopes and intercepts of these trajectories, we utilized established severity guidelines for the UCLA Reaction Index-Revised (e.g., Rodriguez et al., 2001; Steinberg et al., 2004). The chronic trajectory group (4%) reported severe levels of PTSD symptoms at three months post-disaster. These symptoms did not decline over time. The Recovering trajectory group (25%) reported moderate levels of PTS symptoms at three months post-disaster. By 24 months post-disaster, children’s PTSD symptom levels had declined to the mild range. The majority of children comprised the resilient trajectory group (71%). This group reported average PTSD symptom levels in the mild range at three months post-disaster. PTSD symptoms declined to the doubtful range by 24 months post-disaster.
Table 2.
Parameters for the three-trajectory group conditional model.
| Class | n (%) | Intercept
|
Slope
|
||
|---|---|---|---|---|---|
| Estimate | SE | Estimate | SE | ||
| Chronic | 16 (4%) | 44.13*** | 4.17 | .07 | .26 |
| Recovering | 106 (25%) | 32.24*** | 1.79 | 3.62*** | .13 |
| Resilient | 295 (71%) | 11.54*** | .79 | 3.28*** | .04 |
p<.001.
Fig. 1.
Latent trajectories for the three-trajectory group conditional model.
Next, odds ratios were examined to determine which risk and protective factors predicted the likelihood of falling into a specific trajectory. For these analyses, it was necessary to designate a reference group (see Table 3). First, we compared the recovering and chronic trajectory groups to the resilient group. For every additional loss and disruption event reported, the children were 1.33 times more likely to fall in the recovering group (CI=1.13–1.56), as compared to the resilient group. For every standard deviation that children fell above the mean on the community violence measure, children were 2.05 times more likely (CI=1.20–3.51) to fall in the recovering group, and 4.04 times more likely (CI=1.52–10.75) in the Chronic group versus the resilient group. For every additional unit of social support, children were.84 times less likely to fall in the Chronic versus the resilient group (OR=.16, CI=.04–.63). No other risk or protective factors were significantly related to probability of falling in the recovering or chronic groups, as compared to the resilient group. Thus, likelihood of falling into the recovering group was associated with greater immediate loss and disruption and greater community violence. Likelihood of falling in the chronic group was associated with greater community violence exposure. In contrast, likelihood of falling in the resilient group was associated with greater peer support.
Table 3.
Odds ratios for risk and protective factors as predictors of latent trajectory class membership (three trajectory group conditional model).
| Comparison group | Resilient
|
Recovering
|
|
|---|---|---|---|
| Recovering odds ratio (95% CI) | Chronic odds ratio (95% CI) | Chronic odds ratio (95% CI) | |
| Immediate Loss/disruption | 1.33*** (1.13–1.56) | 1.20 (.72–1.99) | .90 (.52–1.54) |
| Home violence | 1.07 (.65–1.76) | .72 (.25–2.06) | .67 (.24–1.90) |
| Community violence | 2.05** (1.20–3.51) | 4.04** (1.52–10.75) | 1.98 (.78–5.00) |
| Parent social support | .91 (.48–1.72) | 1.11 (.53–2.30) | 1.23 (.61–2.44) |
| Peer social support | .70 (.36–1.36) | .16** (.04–.63) | .23* (.05–.95) |
CI=Confidence Interval.
p<.05.
p<.01.
p<.001.
Next, we compared probabilities of falling in the chronic versus the recovering group. For every additional unit of social support from peers, children were .77 times less likely to fall in the chronic versus the recovering group (CI=.05–.95). No other risk or protective factors were significantly related to the probability of falling in the chronic versus the recovering group.
3. Discussion
This study explored PTSD symptom trajectories over a two-year period for youth who were exposed to Hurricane Katrina. In contrast to other published research evaluating youth post-disaster, this study employed latent class growth analysis, a subset of growth mixture modeling techniques, which allowed for the examination of distinct PTSD symptom trajectories following a significant traumatic event, as well as risk and protective factors associated with PTSD symptom trajectories. Results indicated that youth PTSD symptom severity was best characterized by three optimum trajectories, resilient, recovering, and chronic. The majority of youth (71%) was in the resilient group and exhibited very mild symptoms in the months following Katrina, with symptoms declining over time. In comparison, approximately a quarter of the youth were classified as recovering, youth who initially reported significant PTSD symptoms (in the moderate range), but subsequently recovered. A relatively small percentage of youth (4%) displayed a chronic symptom trajectory, in which PTSD symptoms were severe immediately following Katrina, and did not remit over the 24 month period.
Historically, it has been assumed that the most common response for individuals who experience trauma is an initial but sizeable elevation in trauma symptoms followed by gradual recovery (McFarlane and Yehuda, 1996). However, emerging research examining post-disaster trajectories indicates that resilience is the most common outcome (e.g., Le Brocque et al., 2010; Nugent et al., 2009). The three trajectories found in the current study are highly commensurate with the findings of Le Broque et al. (2010), which demonstrated three similar posttraumatic stress trajectories (resilient, recovery, and chronic) in children ages 6–16 years following traumatic injury. In contrast, in the one other published study to date employing similar analytic techniques to study posttraumatic stress symptom trajectories, Nugent et al., 2009 found that youth exposed to family violence exhibited two trajectories, resilient and persistent (or chronic). Clearly, we are in the nascent stage of understanding the optimal trajectory classes for traumatized youth. At this point, there are too few studies to postulate whether different trajectories according to the type of traumatic event experienced will emerge. Nonetheless, these innovative, exploratory studies are critically important to moving the field forward, and the results, so far, have been more similar than distinct in comparison.
For this sample, Hurricane and community violence exposure emerged as important risk factors for youth trajectories post-disaster, while peer support was found to be a significant and important protective factor. Specifically, youth who reported greater loss and disruption because of Hurricane Katrina were significantly less likely to have a resilient trajectory as compared to a recovering trajectory. However, this factor was not a significant factor for distinguishing between the resilient and chronic, nor the recovering and chronic trajectories. Past studies have found Hurricane exposure to be an important associate of PTSD symptoms in post-disaster circumstances (Lai et al., In Press; Weems et al., 2010). In this study, Hurricane exposure appears to distinguish between early mild and moderate symptoms, playing less of a critical role in the development of chronic symptoms. The finding suggests that a culmination of risk factors may be necessary to produce a chronic trajectory for disaster-exposed youth.
Community violence exposure also emerged as an important risk factor that distinguished resilient youth and those who fell in recovering or chronic trajectories. The community violence measure queried both witnessing and being victimized by community violence; however it did not allow for the determination of when the community violence exposure or event occurred. Thus, it is impossible to determine whether the reported exposure occurred prior to Katrina, or whether it was a more recent experience, perhaps even directly related to the aftermath environment. Recent research suggests that children ages 2–9 years who have experienced both disaster and prior victimization are at greater risk for anxiety and depression as compared to children with no exposure or with exposure to either disaster or victimization only (Becker-Blease et al., 2010). Although this finding was not replicated for children 10 to 17 years of age, it is clearly important to continue studying the unique effects and interactions among various forms of trauma. Interestingly, home violence was not associated with any of the trajectories. Perhaps a community level risk factor is more relevant in circumstances where youth are dealing with community wide trauma, such as disaster experiences. This is the first known study to examine two types of violence exposure separately with disaster-exposed youth, and further examination of these variables is warranted.
Peer social support emerged as a critically important protective factor for youth participants in this project. This protective factor distinguished between the resilient and chronic classes, as well as the chronic and recovering classes. Past research has found that peer social support predicts both the initial severity and course of PTSD symptoms following Hurricanes (La Greca et al., 1996; Vernberg et al., 1996). Peer social support may be particularly important during the particular developmental stages for this sample (ages 8 to 16 years), since these youth might be more reliant on peers than family to decrease isolation and assist in coping efforts following Hurricanes (Prinstein et al., 1996; Vernberg et al., 1996). Consistent with this postulation, parental support did not emerge as a protective factor. Future studies should further investigate how age, displacement, and relocation correspond with peer and parental support, and whether mediating relations emerge when examining chronic negative trajectories as outcomes.
3.1. Study strengths and limitations
This study makes a unique contribution to the literature, as it is the first known study to employ sophisticated analytic procedures to examine potential PTSD symptom trajectories in a sample of youth exposed to disaster. Additionally, this study included a measure of violence exposure, which allowed these experiences to be considered simultaneously with Hurricane exposure, decreasing the likelihood that the consequences of multiple events would be attributed to Hurricane Katrina alone.
This study also had limitations. The data are based solely on self-report measures, and, thus, are susceptible to response bias. Additionally, the convenience sample included in this study limits the external validity of the findings for other Katrina-affected youth, as well as those impacted by other disasters or traumatic events. Further, we did not model nonlinear trajectories in children’s PTSD symptom trajectories, and thus we are not able to comment upon variable rates of change in PTSD symptoms over time.
3.2. Future directions
Future research should explore additional risk and protective factors that may be important to further explicating our understanding of youth PTSD symptom trajectories, including parenting behaviors and parent mental health symptoms. Additionally, trajectories for other mental health outcomes and, more importantly, well-being in post-disaster environments should be examined. Finally, as prior research has found that new incidents of victimization are associated with increases in PTSD symptoms (Boney-McCoy and Finkelhor, 1996; Perkonigg et al., 2005), assessing timing of trauma exposure at each assessment point in post-disaster circumstances is critical.
3.3. Clinical implications
There are important clinical implications for work focusing on mental health trajectories following a vast community disaster, such as Katrina. While the majority of youth cope well psychologically or recover quickly following a significant disaster, a small, but significant group exhibit ongoing distress. Understanding what risk factors and assessment indicators can aid in early identification for those youth at greatest risk for chronic symptomatology will assist providers in best utilizing the limited resources available for intervention in post-disaster circumstances. Based on the current findings, widely disseminating screening instruments that assess youth Hurricane exposure, violence exposure, social support, and current stress symptoms in post-disaster circumstances could help in making effective triage decisions. Offering evidence-based interventions, such as trauma-focused cognitive behavioral therapy, to the youth whose profile suggest high levels of community violence exposure, low levels of peer social support, and high levels of stress symptomatology could be an effective strategy for changing the trajectories of youth at risk for chronic PTSD symptomatology.
Acknowledgments
Role of funding source
This material is based upon work supported by the US Department of Homeland Security under Award Number: 2008-ST-061-ND 0001 and a research grant from the National Institute of Mental Health (RMH-078148A).
Footnotes
Disclaimer
The views and conclusions contained in this document are those of the authors and should not be interpreted as necessarily representing the official policies, either expressed or implied, of the US Department of Homeland Security.
Conflict of interest
All other authors declare no conflicts of interest for this project.
Contributors
Author Kelley designed the overall study from which the data were collected. Author Self-Brown designed the study questions for the current study, as well as wrote the introduction and discussion. Author Lai completed the analyses and results section. Author McGill completed lit searches, contributed to the editing of the document, and completed the references. Author Thompson wrote the methods section of the paper. All authors contributed to and have approved the final manuscript.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Author; Washington D.C: 2000. Text Revision. [Google Scholar]
- Amstadter A, Resnick H, Nugent N, Acierno R, Rheingold A, Minhinnett R, Kilpatrick D. Longitudinal trajectories of cigarette smoking following rape. Journal of Traumatic Stress. 2009;22 (2):113–121. doi: 10.1002/jts.20398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker-Blease KA, Turner HA, Finkelhor D. Disasters, victimization, and children’s mental health. Child Development. 2010;81 (4):1040–1052. doi: 10.1111/j.1467-8624.2010.01453.x. [DOI] [PubMed] [Google Scholar]
- Bokszczanin A. PTSD symptoms in children and adolescents 28 months after a flood: age and gender differences. Journal of Traumatic Stress. 2007;20 (3):347–351. doi: 10.1002/jts.20220. [DOI] [PubMed] [Google Scholar]
- Bonanno G, Brewin C, Kaniasty K, La Greca AM. Weighing the costs of disaster: consequences, risks, and resilience in individuals, families, and communities. Psychological Science in the Public Interest. 2010;11 (1):1–49. doi: 10.1177/1529100610387086. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Galea S, Bucciarelli A, Vlahov D. Psychological resilience after disaster. Psychological Science. 2006;17 (3):181–186. doi: 10.1111/j.1467-9280.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Mancini AD. The human capacity to thrive in the face of potential trauma. Pediatrics. 2008;121:369–375. doi: 10.1542/peds.2007-1648. [DOI] [PubMed] [Google Scholar]
- Boney-McCoy S, Finkelhor D. Is youth victimization related to trauma symptoms and depression after controlling for prior symptoms and family relationships? A longitudinal, prospective study. Journal of Consulting and Clinical Psychology. 1996;64:1406–1416. doi: 10.1037//0022-006x.64.6.1406. [DOI] [PubMed] [Google Scholar]
- Brofenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Harvard University Press; Cambridge, MA: 1979. [Google Scholar]
- Curran PJ, Hussong AM. The use of latent trajectory models in psycho-pathology research. Journal of Abnormal Psychology. 2003;112 (4):526–544. doi: 10.1037/0021-843X.112.4.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickstein BD, Suvak M, Litz BT, Adler AB. Heterogeneity in the course of posttraumatic stress disorder: trajectories of symptomatology. Journal of Traumatic Stress. 2010;23 (3):331–339. doi: 10.1002/jts.20523. [DOI] [PubMed] [Google Scholar]
- Elliott P, Biddle D, Hawthorne G, Forbes D, Creamer M. Patterns of treatment response in chronic posttraumatic stress disorder: an application of latent growth mixture modeling. Journal of Traumatic Stress. 2005;18 (4):303–311. doi: 10.1002/jts.20041. [DOI] [PubMed] [Google Scholar]
- Flowers AL, Hastings TL, Kelley ML. Development of a screening instrument for exposure to violence in children: the KID-SAVE. Journal of Psychopathology and Behavioral Assessment. 2000;22:91–104. [Google Scholar]
- Galatzer-Levy IR, Madan A, Neylan TC, Henn-Haase C, Marmar CR. Peritraumatic and trait dissociation differentiate police officers with resilient versus symptomatic trajectories of posttraumatic stress symptoms. Journal of Traumatic Stress. 2011;24 (5):557–565. doi: 10.1002/jts.20684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goenjian AK, Walling D, Steinberg AM, Karavan I, Najarian LM, Pynoos R. A prospective study of posttraumatic stress and depressive reactions among treated and untreated adolescents 5 years after a catastrophic disaster. American Journal of Psychiatry. 2005;162:2302–2308. doi: 10.1176/appi.ajp.162.12.2302. [DOI] [PubMed] [Google Scholar]
- Harter S. Manual for the Social Support Scale for Children. Author; Denver, CO: 1985. [Google Scholar]
- Hastings TL, Kelley ML. Development and validation of the screen for adolescent violence exposure (SAVE) Journal of Abnormal Child Psychology. 1997;25:511–520. doi: 10.1023/a:1022641916705. [DOI] [PubMed] [Google Scholar]
- John B, Russell S, Russell PS. The prevalence of posttraumatic stress disorder among children and adolescents affected by tsunami disaster in Tamil Nadu. Disaster Management and Response. 2007;5:3–7. doi: 10.1016/j.dmr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2:302–317. [Google Scholar]
- Kelley ML, Self-Brown S, Le B, Bosson JV, Hernandez BC, Gordon AT. Predicting posttraumatic stress symptoms in children following Hurricane Katrina: a prospective analysis of the effect of parental distress and parenting practices. Journal of Traumatic Stress. 2010;23 (5):582–590. doi: 10.1002/jts.20573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury EL, Warheit GJ, Hargrove MC, Zimmerman RS, Vega WA, Gil AG. The impact of Hurricane Andrew on deviant behavior among a multi-racial/ethnic sample of adolescents in Dade County, Florida: a longitudinal analysis. Journal of Traumatic Stress. 1997;10(1):20. doi: 10.1023/a:1024808413887. [DOI] [PubMed] [Google Scholar]
- Knabb RD, Rhome JR, Brown DP. Tropical Cyclone Report Hurricane Katrina. 2006 < http://www.nhc.noaa.gov/pdf/TCRAL122005_Katrina.pdf>.
- Kronenberg ME, Hansel TC, Brennan AM, Osofsky HJ, Osofsky JD, Lawrason B. Children of Katrina: lessons learned about postdisaster symptoms and recovery patterns. Child Development. 2010;81 (4):1241–1259. doi: 10.1111/j.1467-8624.2010.01465.x. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Lai BS, Jaccard J. Hurricane-related exposure experiences and stressors, other life events, and social support: concurrent and prospective impact on children’s persistent posttraumatic stress symptoms. Journal of Consulting and Clinical Psychology. 2010;78 (6):794–805. doi: 10.1037/a0020775. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Vernberg EM, Prinstein MJ. Symptoms of posttraumatic stress in children after Hurricane Andrew: a prospective study. Journal of Consulting and Clinical Psychology. 1996;64 (4):712–723. doi: 10.1037//0022-006x.64.4.712. [DOI] [PubMed] [Google Scholar]
- Lai BS, La Greca AM, Auslander BA, Short MB. Children’s symptoms of posttraumatic stress and depression after a natural disaster: comorbidity and risk factors. Journal of Affective Disorders. doi: 10.1016/j.jad.2012.08.041. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Vernberg EM, Prinstein MJ. Symptoms of posttraumatic stress in children after Hurricane Andrew: a prospective study. Journal of Consulting and Clinical Psychology. 1996;64 (4):712–723. doi: 10.1037//0022-006x.64.4.712. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Wasserstein SB. Children’s predisaster functioning as a predictor of posttraumatic stress following Hurricane Andrew. Journal of Consulting and Clinical Psychology. 1998;66 (6):883–892. doi: 10.1037//0022-006x.66.6.883. [DOI] [PubMed] [Google Scholar]
- Le Brocque R, Hendrikz J, Kenardy J. The course of post traumatic stress disorder: examination of recovery trajectories following traumatic injury. Journal of Pediatric Psychology. 2010;35 (6):637–645. doi: 10.1093/jpepsy/jsp050. [DOI] [PubMed] [Google Scholar]
- Marsee MA. Reactive aggression and posttraumatic stress in adolescents affected by Hurricane Katrina. Journal of Clinical Child and Adolescent Psychology 53. 2008;37 (3):519–529. doi: 10.1080/15374410802148152. [DOI] [PubMed] [Google Scholar]
- McFarlane AC, Yehuda R. Resilience, vulnerability, and the course of posttraumatic reactions. In: van der Kolk BA, McFarlane AC, Weisaeth L, editors. Traumatic Stress. Guilford; New York: 1996. pp. 155–181. [Google Scholar]
- Muthén B, Asparouhov T. Growth mixture modeling: analysis with non-Gaussian random effects. In: Fitzmaurice G, Davidian M, Verbeke G, Molenberghs G, editors. In Longitudinal Data Analysis. Chapman and Hall–CRC; Boca Raton: 2008. pp. 143–165. [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. 5. Muthen & Muthen; Los Angeles, CA: 1998–2007. [Google Scholar]
- Neuner F, Schauer E, Catani C, Ruf M, Elbert T. Post-tsunami stress: a study of posttraumatic stress disorder in children living in three severely affected regions in Sri Lanka. Journal of Traumatic Stress. 2006;19 (3):339–347. doi: 10.1002/jts.20121. [DOI] [PubMed] [Google Scholar]
- Norris FH, Friedman MJ, Watson PJ. 60,000 Disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry: Interpersonal and Biological Processes. 2002;65 (3):240–260. doi: 10.1521/psyc.65.3.240.20169. [DOI] [PubMed] [Google Scholar]
- Nugent NR, Saunders BE, Williams LM, Hanson R, Smith DW, Fitzgerald MM. Posttraumatic stress symptom trajectories in children living in families reported for family violence. Journal of Traumatic Stress. 2009;22 (5):460–466. doi: 10.1002/jts.20440. [DOI] [PubMed] [Google Scholar]
- Orcutt HK, Erickson DJ, Wolfe J. The course of PTSD symptoms among Gulf War veterans: a growth mixture modeling approach. Journal of Traumatic Stress. 2004;17 (3):195–202. doi: 10.1023/B:JOTS.0000029262.42865.c2. [DOI] [PubMed] [Google Scholar]
- Osofsky HJ, Osofsky JD, Kronenberg M, Brennan A, Hansel TC. Posttraumatic stress symptoms in children after Hurricane Katrina: predicting the need for mental health services. American Journal of Orthopsychiatry. 2009;79 (2):212–220. doi: 10.1037/a0016179. [DOI] [PubMed] [Google Scholar]
- Perkonigg A, Pfister H, Stein MB, Hofler M, Lieb R, Maercker A, Wittchen HU. Longitudinal course of posttraumatic stress disorder and posttraumatic stress disorder symptoms in a community sample of adolescents and young adults. American Journal of Psychiatry. 2005;162:1320–1327. doi: 10.1176/appi.ajp.162.7.1320. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, La Greca AM, Vernberg EM, Silverman WK. Children’s coping assistance: how parents, teachers, and friends help children cope after a natural disaster. Journal of Clinical Child Psychology. 1996;25 (4):463–475. [Google Scholar]
- Pynoos R, Rodriguez N, Steinberg A, Stuber M, Frederick C. The UCLA PTSD Reaction Index for DSM-IV (Revision 1) Los Angeles: UCLA Trauma Psychiatry Program; 1998. [Google Scholar]
- Rodriguez N, Steinberg A, Saltzman W, Pynoos R. PTSD Index: Preliminary Psychometric Analyses of Child and Parent Versions. Symposium Conducted at the 17th Annual Meeting of the International Society for Traumatic Stress Studies; New Orleans, LA. Dec, 2001. [Google Scholar]
- Rowe CL, La Greca AM, Alexandersson A. Family and individual factors associated with substance involvement and PTS symptoms among adolescents in Greater New Orleans after Hurricane Katrina. Journal of Consulting and Clinical Psychology. 2010:78. doi: 10.1037/a0020808. [DOI] [PubMed] [Google Scholar]
- Russoniello CV, Skalko TK, O’Brien K, McGhee SA, Bingham-Alexander D, Beatley J. Childhood posttraumatic stress disorder and efforts to cope after Hurricane Floyd. Behavioral Medicine. 2002;28:61–71. doi: 10.1080/08964280209596399. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer JJ, Decker KB, Pynoos RS. The University of California at Los Angeles post-traumatic stress disorder reaction index. Current Psychiatry Reports. 2004;6:96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Vernberg EM, La Greca AM, Silverman WK, Prinstein MJ. Prediction of posttraumatic stress symptoms in children after Hurricane Andrew. Journal of Abnormal Psychology. 1996;105 (2):237–248. doi: 10.1037//0021-843x.105.2.237. [DOI] [PubMed] [Google Scholar]
- Weems CF, Overstreet S. Child and adolescent mental health research in the context of Hurricane Katrina: an ecological-needs-based perspective and introduction to the special section. Journal of Clinical Child Adolescent Psychology. 2008;37:487–494. doi: 10.1080/15374410802148251. [DOI] [PubMed] [Google Scholar]
- Weems CF, Pina AA, Costa NM, Watts SE, Taylor LK, Cannon MF. Pre-disaster trait anxiety and negative affect predict posttraumatic stress in youth after Hurricane Katrina. Journal of Consulting and Clinical Psychology. 2007;75:154–159. doi: 10.1037/0022-006X.75.1.154. [DOI] [PubMed] [Google Scholar]
- Weems CF, Taylor LK, Cannon MF, Marino RC, Romano DM, Scott BG, Triplett V. Posttraumatic stress, context, and the lingering effects of the Hurricane Katrina disaster among ethnic minority youth. Journal of Abnormal Child Psychology. 2010;38 (1):49–56. doi: 10.1007/s10802-009-9352-y. [DOI] [PubMed] [Google Scholar]
- Yelland CB, Robinson P, Lock C, La Greca AM, Kokegei B, Ridgeway V, Lai B. Bushfire impact on youth. Journal of Traumatic Stress. 2010;23 (2):274–277. doi: 10.1002/jts.20521. [DOI] [PubMed] [Google Scholar]