Abstract
Purpose
Although replacement of the ureter with a bowel segment is indicated for large ureteral defects, it is still a challenging technique for urologists. We present our experience and outcome of ureteral reconstruction using bowel segments.
Materials and Methods
Ureteral reconstruction with bowel segments was performed in eight patients in our institute between 1969 and 2009. We investigated the position and length of the ureteral defect and methods of reconstruction as well as the patients' backgrounds, postoperative complications, and clinical outcomes.
Results
Five patients underwent ureteral replacement with isolated ileal segments alone. In one patient, the ureter was reconstructed by using the Yang-Monti procedure with the ileum. A colon segment was used in two patients who required bladder augmentation for tuberculous contracted bladder at the same time. Metabolic acidosis occurred in three patients having a solitary kidney and the ureter had to be replaced by a relatively long intestinal segment. Two patients who received preoperative radiation therapy were required to undergo additional operations. Long-term cancer-free survival was achieved in one patient who underwent ileal substitution for low-grade renal pelvic cancer.
Conclusions
Although ureteral replacement with a bowel segment is a challenging and useful procedure, attention must be paid to the possibility of metabolic acidosis, which is likely to occur in patients having a solitary kidney with renal insufficiency or in patients requiring a long intestinal segment for reconstruction. In addition, preoperative radiation therapy for the pelvic organs may cause postoperative complications.
Keywords: Colon, Ileum, Reconstructive surgical procedures, Ureter
INTRODUCTION
The surgical management of ureteral defects is decided on the basis of the level and length of the defect. A short defect involving the upper or mid ureter is most appropriate for ureteroureterostomy. A short defect of the lower ureter is usually managed by ureteroneocystostomy with or without a psoas hitch or Boari flap [1]. For long ureteral defects, however, a surgical option such as renal autotransplantation, transureteroureterostomy, or ureteral reconstruction using bowel segments is needed. Reconstruction of the ureter with tissue lined with urothelium is preferable because urothelium is not absorptive. In addition, the urothelium is resistant to the inflammatory and potentially carcinogenic effects of urine [2]. In a situation in which a ureteral defect cannot be bridged by tissue lined with urothelium, ureteral reconstruction using bowel segments has been demonstrated to be a satisfactory option [3].
Shoemaker [4] reported the first reconstruction of the ureter using the ileum in 1911. In an online database, Chung et al. [5], Armatys et al. [6], and Wolff et al. [7] reported large cases series. In Japan, however, there has been only one case series report, including four patients who underwent ureteral interposition in a single center [8]. Thus, opportunities for ureteral interposition are still limited in single institutes in Japan.
In this study, we present our clinical experience with eight patients who underwent ureteral reconstruction with the use of bowel segments in our institute.
MATERIALS AND METHODS
We performed ureteral reconstruction by using bowel segments for eight patients in Sapporo Medical University School of Medicine between January 1969 and December 2009. According to the descriptions in the patients' medical charts, we retrospectively examined each patient's age, gender, clinical history, location and length of the ureteral stricture or obstruction, reconstructive methods, postoperative complications, and clinical outcomes. This study protocol was reviewed and approved by the Ethical Committee in Sapporo Medical University School of Medicine (Institutional Review Board No. 262-61). Each patient provided informed consent on our website (http://web.sapmed.ac.jp/uro/).
RESULTS
Between 1969 and 2009, the ureters of eight patients consisting of two males and six females (seven unilateral, one bilateral) were replaced with bowel segments owing to tuberculous ureteral stricture in two, urogenital malignancy in two, stricture after nonurological surgery in two, stricture after radiation in one, and an intractable vesicovaginal fistula in one. The median age at surgery was 42 years (range, 36-65 years). The patients' characteristics are shown in Tables 1 and 2, and the details of the surgical procedures are shown in Figs. 1, 2, 3, 4, 5, 6, 7 and 8. The median follow-up period was 60 months (range, 7-260 months). Brief summaries of the patients' clinical courses are provided below.
TABLE 1.
Patients' characteristics
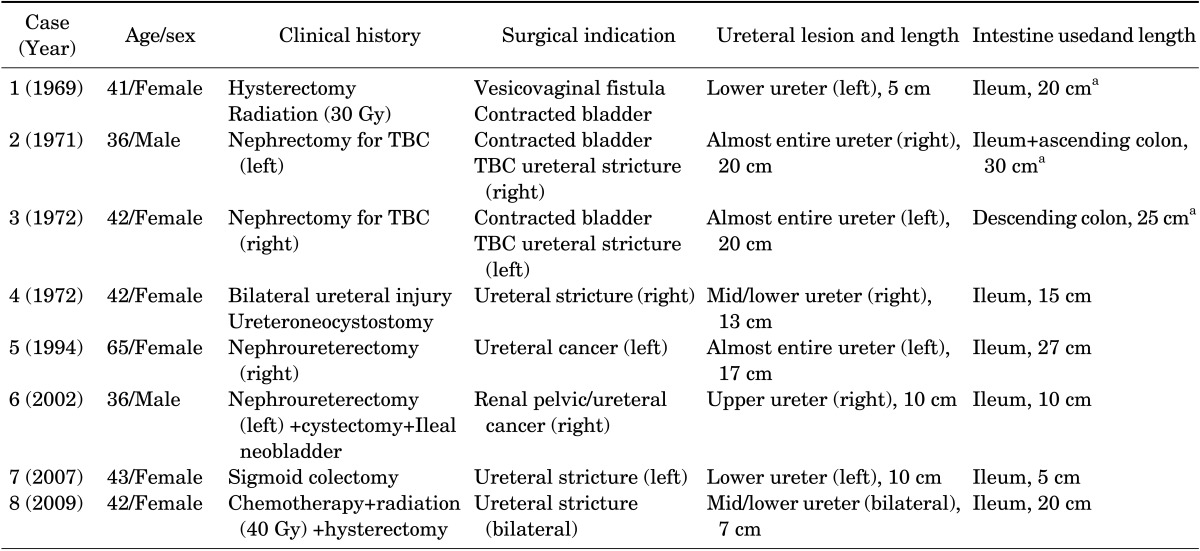
TBC, tuberculosis.
a:Including intestine for cystoplasty.
TABLE 2.
Patients' characteristics
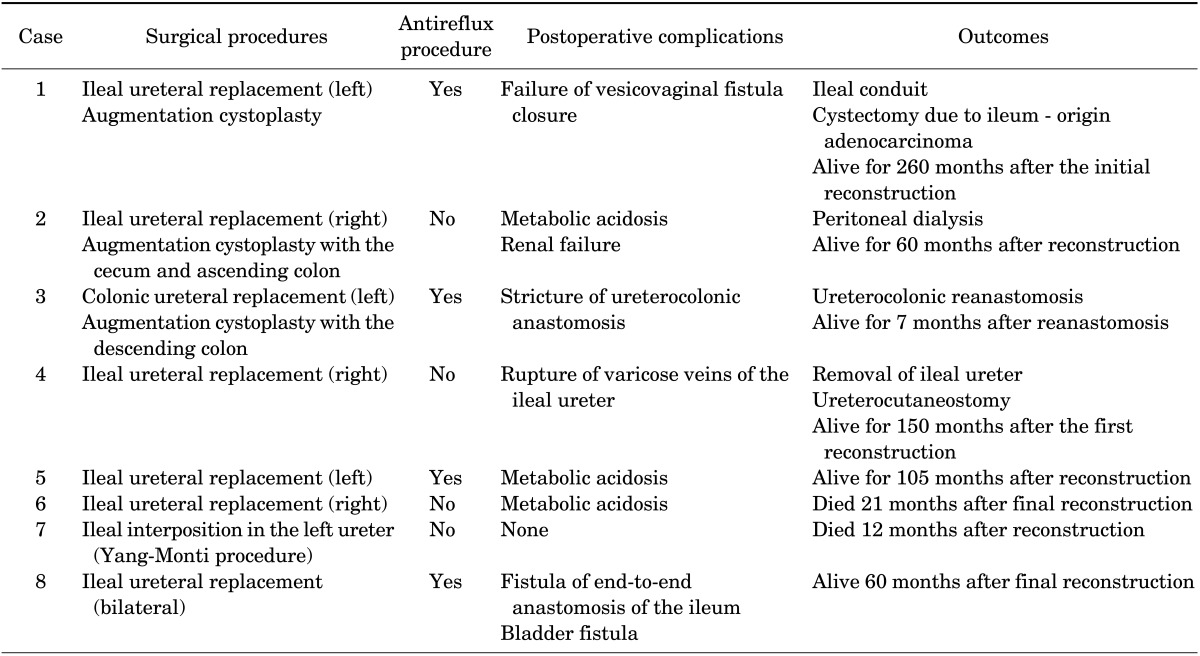
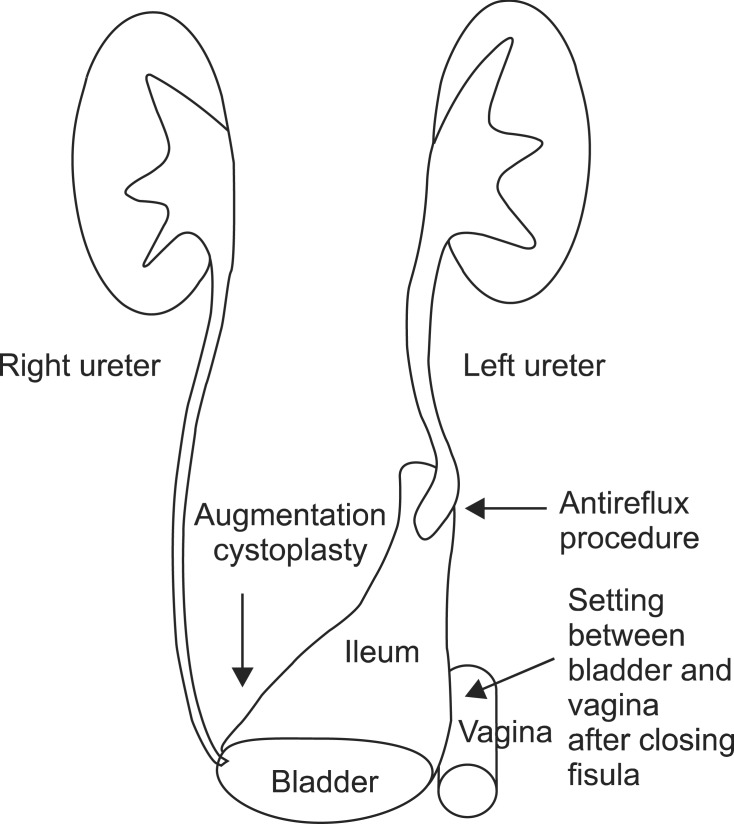
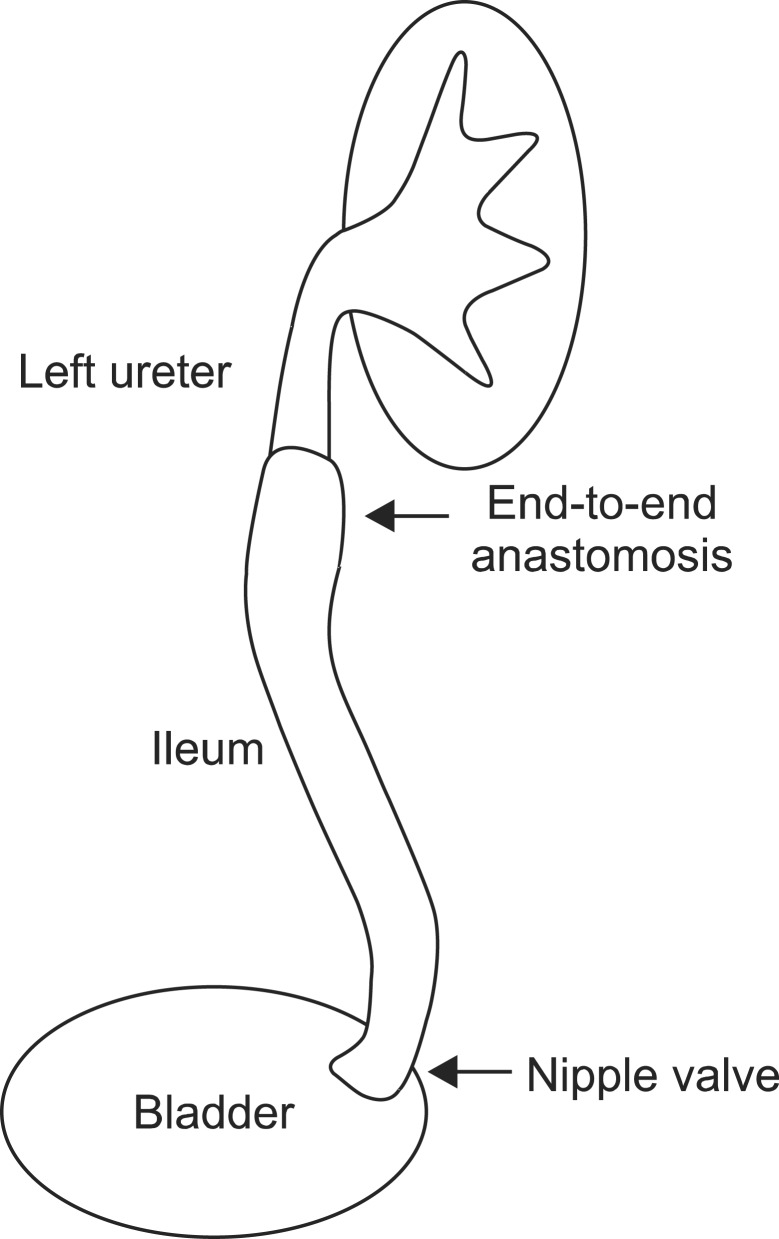
FIG. 1.
Case 1: A 20-cm ileal segment was isolated for bladder augmentation and replacement of the lower part of the left ureter.
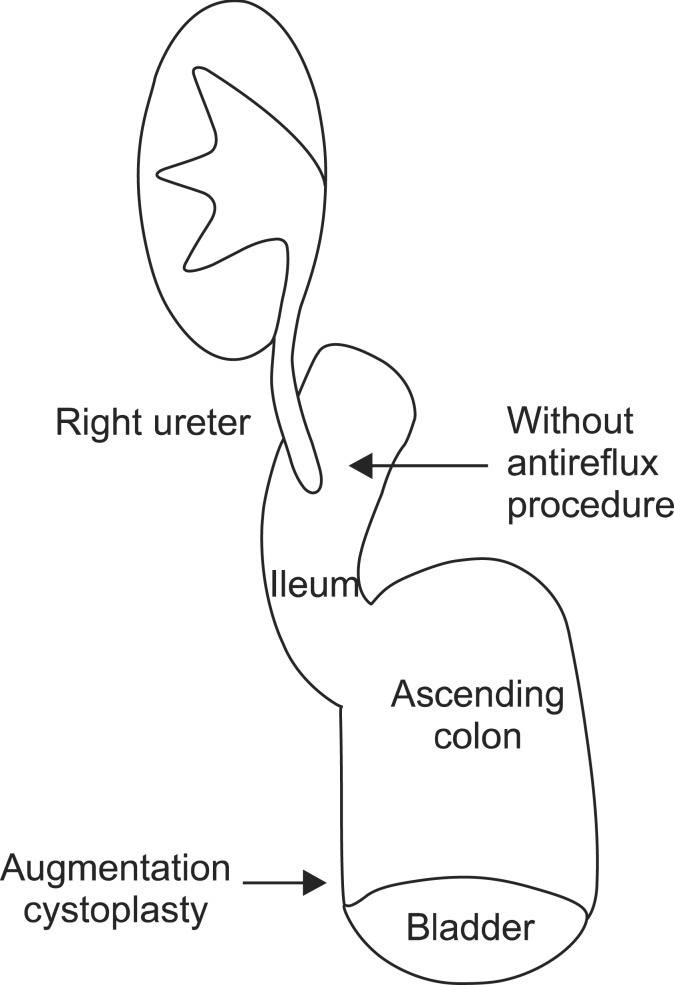
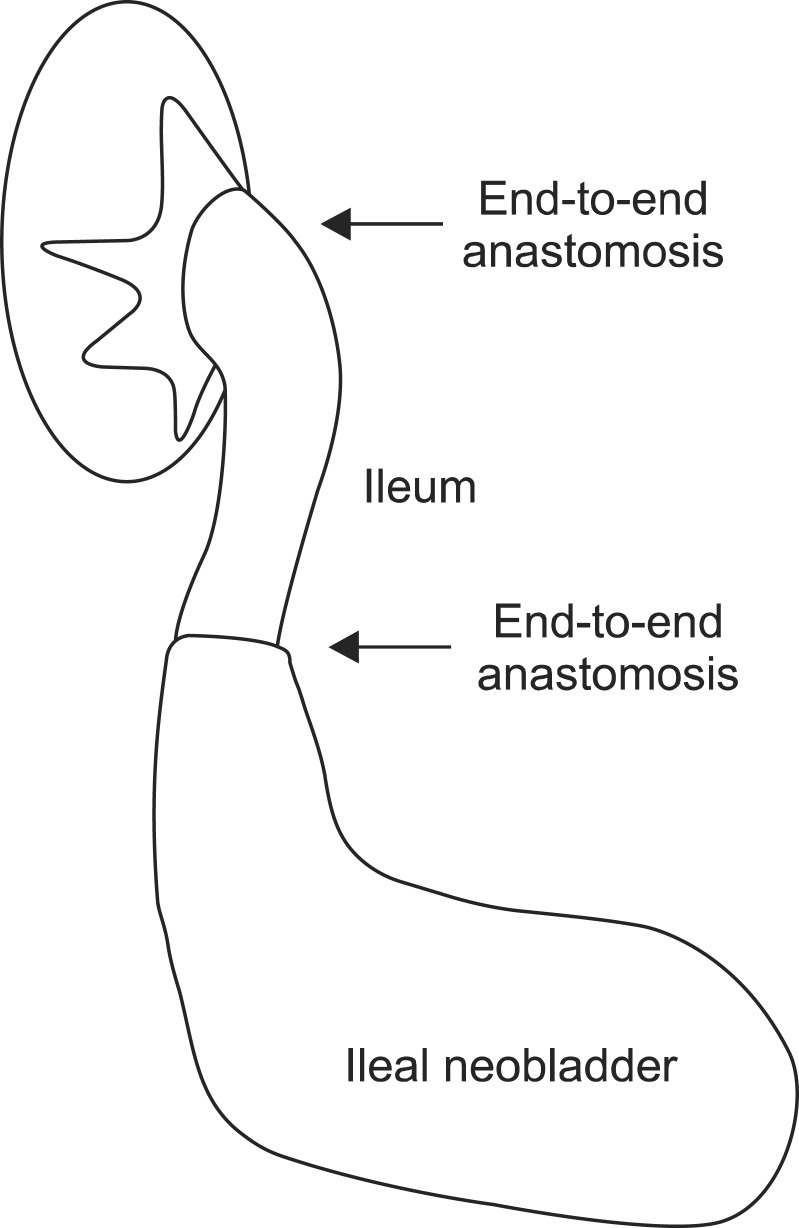
FIG. 2.
Case 2: Almost the entire ureter was replaced by the ileum, and the bladder was augmented with the cecum and ascending colon. The ureter was anastomosed to the ileum without an anti-reflux procedure.
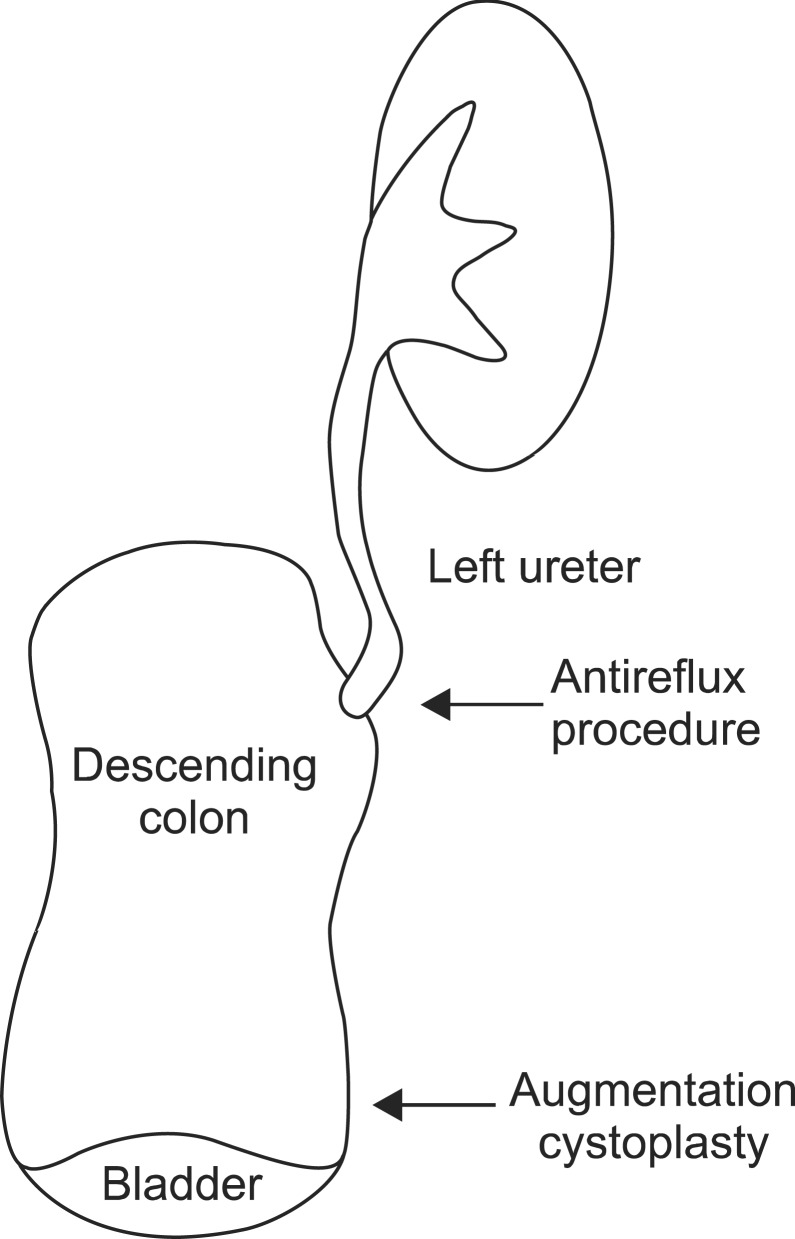
FIG. 3.
Case 3: Almost the entire ureter was replaced by the proximal segment of the descending colon and the bladder was augmented. An antireflux procedure was used in anastomosis of the ureter to the descending colon.
FIG. 4.
Case 4: The mid and lower ureter were replaced by an isolated 15-cm ileal segment that was anastomosed to the distal end of the upper ureter without an anti-reflux procedure. No antireflux procedure was used in anastomosis between the distal end of the ileum and the bladder.
FIG. 5.
Case 5: Almost the entire ureter was replaced by an isolated 27-cm ileal segment. An antireflux procedure was done for the anastomosis between the distal end of the ileum and the bladder.
FIG. 6.
Case 6: The right renal pelvis and ureter were replaced by an isolated 10-cm ileal segment. The proximal end of the ileum was anastomosed to the renal pelvis and the distal end to the proximal end of the afferent limb of the ileal neobladder.
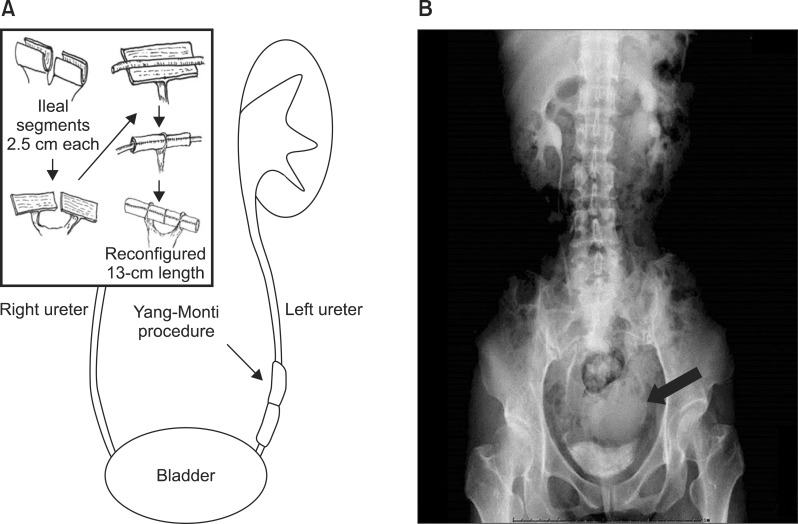
FIG. 7.
Case 7: (A) Two 2.5-cm ileal segments were isolated and their antimesenteric borders were opened and reconfigured as a tube around a 14-Fr Nélaton catheter. This provided ileal segments with a total length of 13 cm, which were interposed in the lower left ureter. (B) The interposed ileum is shown in excretory urography (arrow).
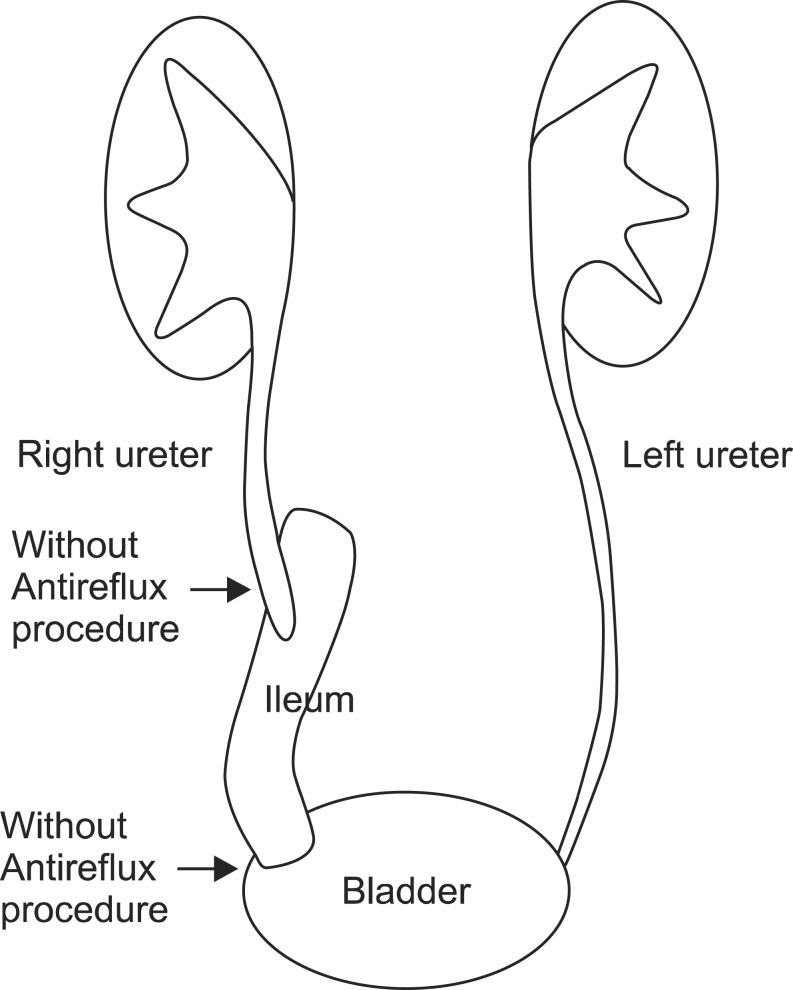
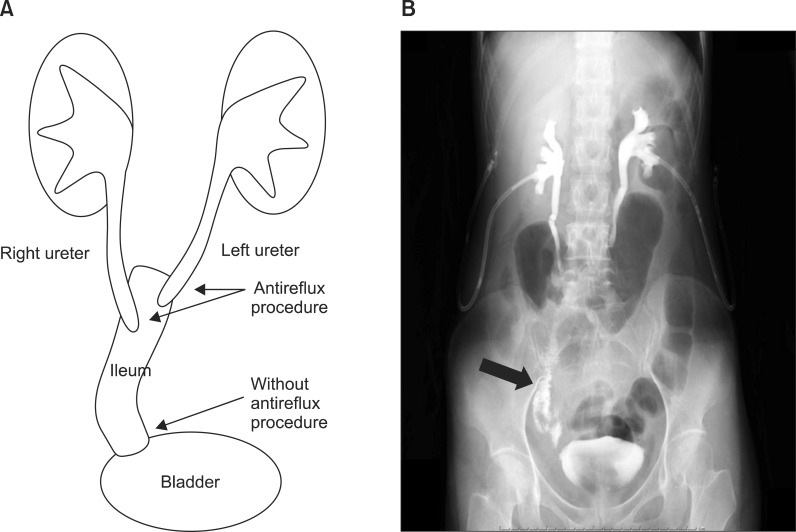
FIG. 8.
Case 8: (A) The bilateral mid and lower ureters were replaced with an isolated 20-cm ileal segment. The distal ends of both ureters and the proximal end of the ileum were anastomosed with Le Duc's antireflux method. No antireflux procedure was done for the anastomosis between the distal end of the ileum and the bladder. (B) The interposed ileum is shown in excretory urography under clamping of bilateral percutaneous nephrostomy tubes (arrow).
1. Case 1: 41-year-old female
Hysterectomy was performed for cervical cancer in this patient following radiation therapy (30 Gy, whole pelvis) in 1967. A vesicovaginal fistula developed near the left ureteral orifice 5 days after surgery. Two attempts at surgical repair with transvaginal and transperitoneal approaches failed. In 1969, the patient underwent a third operation consisting of a left ileal ureteral replacement and augmentation cystoplasty (Fig. 1). At that time, the left ureter was anastomosed with an antireflux procedure (submucosal tunnel method). The ileum was positioned between the bladder wall and the closed vaginal wall to prevent the recurrence of fistula formation because an omental flap was not available owing to the failure of a previous operation. However, the vesicovaginal fistula was not closed. In addition, purulent peritonitis developed postoperatively. Three months after the improvement of inflammation, she received an ileal conduit because of persistent urinary leakage from the vagina, and the reconstructed ileal segment, excluding the portion of the bladder wall, was removed. Finally, she underwent cystectomy due to adenocarcinoma originating from the ileal mucosa remaining in the bladder wall 260 months after the third operation, as we previously reported [9].
2. Case 2: 36-year-old male
The patient underwent left nephrectomy for renal tuberculosis in 1964. Because a right ureteral stricture and contracted bladder due to urinary tuberculosis developed, we performed a right ileal ureteral replacement with augmentation cystoplasty using the cecum and ascending colon in 1971 (Fig. 2). The preoperative serum creatinine level was 1.8 mg/dL. A 15-cm section of the ileum and a continuous 15-cm segment of the ascending colon were isolated. The right ureter was anastomosed to the ileum with Nesbit's method [10], and bladder augmentation was performed by using the nondetubularized ascending colon segment. Although there was no episode of pyelonephritis, metabolic acidosis occurred 6 months postoperatively. The serum creatinine level gradually increased to 8.1 mg/dL at 60 months after surgery, and the patient eventually received peritoneal dialysis.
3. Case 3: 42-year-old female
This patient underwent a right nephrectomy for renal tuberculosis in 1948. Cystostomy was done because of lower urinary tract obstruction by a tuberculous urethral stricture in 1965. Because left hydronephrosis had developed because of the stricture, which had a length of 20 cm, left colonic ureteral replacement and augmentation cystoplasty using the descending colon were performed in 1972. A 25-cm segment of the descending colon was isolated, the left ureteral stricture was removed, and the end of the ureter was anastomosed to the proximal side of the isolated colon with an antireflux procedure (submucosal tunnel method) (Fig. 3). In addition, the bladder was augmented by using the distal end of the isolated non-detubularized descending colon. After the left splint catheter was removed, hydronephrosis and an increase in the serum creatinine level gradually occurred as a result of the anastomotic stricture. After constructing the left percutaneous nephrostomy tube (PNS), reanastomosis of the ureter to the descending colon with the antireflux procedure (submucosal tunnel method) was done 3 months after control of the infection.
4. Case 4: 42-year-old female
In 1959, this patient's bilateral ureters were injured during a cesarian section and the gynecological doctors performed ureteroneocystostomy. In 1972, a right ureteral stricture with a length of 13 cm was found. The serum creatinine concentration was normal at 0.7 mg/dL. The patient underwent ureteral reconstruction with an isolated 15-cm ileal segment (Fig. 4). The right ureter was anastomosed to the proximal end of the ileum by using Nesbit's method, and the distal end was directly anastomosed to the bladder. There was no episode of pyelonephritis during the follow-up. Because of bleeding from varicose veins of the isolated ileum as a result of liver cirrhosis, the reconstructed ileal segment was removed and rediversion with right ureterocutaneostomy was performed in 1983.
5. Case 5: 65-year-old female
In 1988, this patient underwent right radical nephroureterectomy for renal pelvic cancer with pathological findings of urothelial carcinoma (UC: G2, pT1b, pN0). A single papillary tumor (UC: G2, pT1) 13 mm in diameter recurred in the left renal pelvis in 1990. Based on the patient's strong desire, partial resection of the left pelvis was done. In 1994, owing to recurrence of the tumor in the left middle ureter, 17 cm of the left ureter including the tumor (UC: G1, pTa) was excised and the defect was reconstructed by using a 27-cm ileal segment. The preoperative creatinine level was 1.1 mg/dL. The left ureter was anastomosed to the proximal side of the ileum in an end-to-end fashion and the distal side of the ileum was anastomosed to the bladder with a nipple valve [11] (Fig. 5). Two months after the final operation, the patient developed metabolic acidosis and received medical treatment. Although the serum creatinine concentration was slightly increased to 1.4 mg/dL during 105 months of follow-up, no cancer recurrence or episodes of pyelonephritis were observed.
6. Case 6: 36-year-old male
In 1975, at the age of 11 years, this patient was diagnosed as having bladder cancer, and over the next 25 years (until 2000) he underwent transurethral resection 19 times for recurrence of the cancer. In 2000, he underwent left radical nephroureterectomy for renal pelvic cancer (UC: G2, pT3, pN0). At the same time, radical cystectomy with an ileal neobladder was performed to prevent further progression of the bladder cancer. In 2001, recurrence was observed on the right ureteral end. The right ureteroileal anastomosis site was excised (UC: G1, pTa) and the right ureter was reanastomosed to the neobladder with Nesbit's method. In 2002, owing to tumor recurrence in the right renal pelvis and ureter, right pyeloureterectomy was performed and the upper urinary tract was reconstructed by using a 10-cm segment of the ileum (Fig. 6). The proximal end and distal end of the ileum were directly anastomosed to the renal pelvis and the afferent limb of the ileal neobladder, respectively, without any anti-reflux procedures. At that time, serum creatinine was 1.6 mg/dL. Three months later, treatment for metabolic acidosis was necessary. Eventually, the patient died of cancer 21 months after nephroureterectomy.
7. Case 7: 43-year-old female
After sigmoid colectomy for cancer in June 2006, a left ureteral stricture was detected in this patient in March 2007 and a ureteral stent was indwelled. Left ureteral reconstruction was done with an ileal segment by using the Yang-Monti procedure [11] in May 2007 (Fig. 7A). Left upper urinary tract dilation was not found in the excretory urography postoperatively (Fig. 7B). The patient died of recurrence of sigmoid colon cancer at 12 months postoperatively.
8. Case 8: 42-year-old female
In February 2003, this patient underwent hysterectomy for stage Ib cervical cancer following radiotherapy (40 Gy, whole pelvis) and chemotherapy. In September 2008, left hydronephrosis due to a 7-cm stricture in the left lower ureter was detected. Because right hydronephrosis also appeared, bilateral PNS was constructed. In June 2009, 7-cm segments of the bilateral middle and lower ureters were dissected and the bilateral upper ureters were anastomosed to the proximal side of a 20-cm section of isolated ileum with an anti-reflux procedure (Le Duc's method) [12] (Fig. 8A). The distal end of the ileum was directly anastomosed to the bladder without an antireflux procedure. During the postoperative course, minor leakage from the functional end-to-end anastomosis of the ileum occurred, as well as fistula formation between the abscess and the bladder. Removal of the functional end-to-end anastomosis of the ileum, anastomosis between the ileum and the ascending colon, and closure of the fistula of the bladder were attempted 4 months after the initial reconstruction. Only mild upper urinary tract dilation was found in the excretory urography under clamping bilateral PNS (Fig. 8B), which were removed thereafter. No episodes of pyelonephritis occurred after the final operation. Serum creatinine did not change from 0.7 mg/dL during 60 months of follow-up.
DISCUSSION
The ileum and colon are used most often for urinary reconstruction. The merits of the ileal segment are its mobility, small diameter, and constant blood supply [3]. Contraindications for the ileal ureter are inflammatory bowel disease, an irradiated bowel, bladder neck obstruction, neurogenic bladder, renal insufficiency with a serum creatinine concentration of greater than 2 mg/dL, and hepatic dysfunction [5,13]. A colon segment has different merits that the ileal segment does not have [11]. However, when colon segments are used for ureteral reconstruction, we should keep in mind the possible demerits such as the formation of a bacterial nest in the upper urinary tract and the appearance of malignancy in the future [14]. In our institute, a colon segment was used in only two patients who required bladder augmentation for tuberculous contracted bladder in the early 1970s.
The factors that influence the amount of solute and the type of absorption are the part of the bowel, the surface area of the bowel, the time that the bowel surface is exposed to urine, the concentration of solutes in urine, renal function, and the pH of the fluid [3]. In our study, metabolic acidosis occurred postoperatively in three patients with a solitary kidney and renal insufficiency. In addition, in these three patients, replacement was done with relatively longer intestinal segments and they had a higher risk for metabolic acidosis than in the other cases. Indeed, two of the three had augmentation cystoplasty or ileal neobladder construction simultaneously. Thus, we should not neglect the close follow-up of metabolic changes in these patients.
Use of the Yang-Monti technique is theoretically advantageous in this regard owing to the shorter segment of the bowel needed, which may minimize solute reabsorption and metabolic abnormalities. In this method, a 2- to 3-cm section of ileum provides about 8 to 10 cm of reconfigured length [15]. Ali-el-Dein and Ghoneim [16] concluded that a short bowel segment was enough for reconstruction and metabolic consequences were eliminated. Other authors also demonstrated good outcomes of ureteral replacement by the same method using the colon [17,18,19,20]. Although our patient whose ureter was replaced by the Yang-Monti procedure by use of the ileum died from recurrence of sigmoid colon cancer, good results were obtained in the short-term follow-up period. Thus, this procedure could be quite useful if appropriate patients are selected.
If an antireflux mechanism is constructed, it is generally done for either the ureteral-intestinal [11] or intestinal-vesical [12,21] junction. Kato et al. [22] assumed that the most critical portion to prevent reflux could be the uretero-intestinal junction because a distant antireflux mechanism may increase the resistance of urine flow with subsequent dilatation of the ileal segment in long-term follow-up. However, the necessity of an antireflux procedure is still controversial. Waldner et al. [23] reported, on the basis of their experience, that such a procedure was unnecessary for adults with normal voiding function. On the other hand, Bazeed et al. [24] reported that it was necessary, especially for patients with decreased renal function. Although in half of our patients the urinary tracts were reconstructed without an antireflux procedure, renal insufficiency due to reflux was not observed. Only one patient without an antireflux procedure developed renal failure (Case 2). However, this may not have been due to reflux nephropathy because no reflux was observed throughout the follow-up period. Thus, our study may suggest that anastomosis without an antireflux procedure may be safely indicated for adult patients having normal preoperative renal and voiding functions.
Ureteral replacement using a bowel segment after radiation therapy is also controversial. It has been reported that patients with renal insufficiency and a history of irradiation for pelvic malignancy are contraindicated for ileal ureteral substitution because of the risk of fistula formation [23,25]. Those studies recommended the use of reconfigured colon segments outside of the radiation portal. Several studies have demonstrated that a prior history of abdominal or pelvic radiation should not serve as the sole determining factor for the selection of the bowel segment utilized during urinary diversion because there is evidence that, in most patients, the complication rate is low with use of the ileum [13,22]. In the present study, we reconstructed the ureter by using the ileum after radiation therapy in two of four patients who needed the additional surgical procedure. We presumed that the high reoperation rate in this study was mainly due to the preoperative radiation. End-to-end anastomosis of the ileum failed in one patient despite the normal appearance of the ileum during surgery. However, not only prudent selection of patients but also close perioperative and postoperative observation are mandatory when we plan to use the irradiated ileum for ureteral replacement.
This study had several limitations. First, it included only eight patients over a long period between 1969 and 2009. In addition, the reasons for ureteral reconstruction and the types of surgical procedures differed. Moreover, not all patients were treated by a single urologist. It is a possibility that this could have influenced the outcomes. However, it is unrealistic to expect that a single institute will have a sufficient number of patients with urinary reconstruction using a bowel segment in a short period. Although each patient in this study had different clinical courses, we were convinced that we provided them the optimal treatment at that time. In addition, in this context, we believe that this case series provides surgeons with clinically relevant information.
CONCLUSIONS
Ureteral replacement with a bowel segment is a challenging but useful procedure, even for patients with malignancy. However, unexpected complications might occur in patients who have a history of radiation therapy for pelvic organs or a solitary kidney without an adequate functional reserve. According to the patient's background, we must choose an appropriate treatment option and follow the patients up very carefully.
Footnotes
The authors have nothing to disclose.
References
- 1.Dhal DM, McDougal WS. Use of intestinal segments in urinary diversion. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 9th ed. Philadelphia: Saunders; 2007. pp. 2534–2578. [Google Scholar]
- 2.Harzmann R, Kopper B, Carl P. Cancer induction by urinary drainage or diversion through intestinal segments? Urologe A. 1986;25:198–203. [PubMed] [Google Scholar]
- 3.Hsu THS, Streem SB, Nakada SY. Management of upper urinary tract obstruction. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 9th ed. Philadelphia: Saunders; 2007. pp. 1227–1273. [Google Scholar]
- 4.Shoemaker GE. Removal of the ureter with a tuberculous kidney. Ann Surg. 1911;53:696–698. doi: 10.1097/00000658-191105000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chung BI, Hamawy KJ, Zinman LN, Libertino JA. The use of bowel for ureteral replacement for complex ureteral reconstruction: long-term results. J Urol. 2006;175:179–183. doi: 10.1016/S0022-5347(05)00061-3. [DOI] [PubMed] [Google Scholar]
- 6.Armatys SA, Mellon MJ, Beck SD, Koch MO, Foster RS, Bihrle R. Use of ileum as ureteral replacement in urological reconstruction. J Urol. 2009;181:177–181. doi: 10.1016/j.juro.2008.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wolff B, Chartier-Kastler E, Mozer P, Haertig A, Bitker MO, Roupret M. Long-term functional outcomes after ileal ureter substitution: a single-center experience. Urology. 2011;78:692–695. doi: 10.1016/j.urology.2011.04.054. [DOI] [PubMed] [Google Scholar]
- 8.Kawanishi H, Aoyama T, Sasaki M. Long-term results of ureteral replacement using ileum: report of four cases. Hinyokika Kiyo. 1999;45:431–434. [PubMed] [Google Scholar]
- 9.Takahashi A, Tsukamoto T, Kumamoto Y, Sato Y, Shibuya A, Sato M. Adenocarcinoma arising in the ileal segment of a defunctionalized ileocystoplasty. Hinyokika Kiyo. 1993;39:753–755. [PubMed] [Google Scholar]
- 10.Nesbit RM. Ureterosigmoid anastomosis by direct elliptical connection. Univ Hosp Bull. 1948;14:45. [PubMed] [Google Scholar]
- 11.Tscholl R, Tettamanti F, Zingg E. Ileal substitute of ureter with reflux-plasty by terminal intussusception of bowel: animal experiments and clinical experience. Urology. 1977;9:385–389. doi: 10.1016/0090-4295(77)90211-4. [DOI] [PubMed] [Google Scholar]
- 12.Le Duc A, Camey M, Teillac P. An original antireflux ureteroileal implantation technique: long-term followup. J Urol. 1987;137:1156–1158. doi: 10.1016/s0022-5347(17)44433-8. [DOI] [PubMed] [Google Scholar]
- 13.Mattos RM, Smith JJ., 3rd Ileal ureter. Urol Clin North Am. 1997;24:813–825. doi: 10.1016/s0094-0143(05)70422-5. [DOI] [PubMed] [Google Scholar]
- 14.Ravi R, Dewan AK, Pandey KK. Transverse colon conduit urinary diversion in patients treated with very high dose pelvic irradiation. Br J Urol. 1994;73:51–54. doi: 10.1111/j.1464-410x.1994.tb07455.x. [DOI] [PubMed] [Google Scholar]
- 15.Hinman AR, Farmer PE. The coalition for cholera prevention and control meeting. Vaccine. 2013;31:2323. doi: 10.1016/j.vaccine.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 16.Ali-el-Dein B, Ghoneim MA. Bridging long ureteral defects using the Yang-Monti principle. J Urol. 2003;169:1074–1077. doi: 10.1097/01.ju.0000050151.66653.cc. [DOI] [PubMed] [Google Scholar]
- 17.Castellan M, Gosalbez R. Ureteral replacement using the Yang-Monti principle: long-term follow-up. Urology. 2006;67:476–479. doi: 10.1016/j.urology.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 18.Pope J, Koch MO. Ureteral replacement with reconfigured colon substitute. J Urol. 1996;155:1693–1695. [PubMed] [Google Scholar]
- 19.Ubrig B, Roth S. Reconfigured colon segments as a ureteral substitute. World J Urol. 2003;21:119–122. doi: 10.1007/s00345-003-0320-9. [DOI] [PubMed] [Google Scholar]
- 20.Ubrig B, Waldner M, Roth S. Reconstruction of ureter with transverse retubularized colon segments. J Urol. 2001;166:973–976. [PubMed] [Google Scholar]
- 21.Goodwin WE, Scardino PT. Ureterosigmoidostomy. J Urol. 1977;118(1 Pt 2):169–174. doi: 10.1016/s0022-5347(17)57938-0. [DOI] [PubMed] [Google Scholar]
- 22.Kato H, Abol-Enein H, Igawa Y, Nishizawa O, Ghoneim MA. A case of ileal ureter with proximal antireflux system. Int J Urol. 1999;6:320–323. doi: 10.1046/j.1442-2042.1999.00068.x. [DOI] [PubMed] [Google Scholar]
- 23.Waldner M, Hertle L, Roth S. Ileal ureteral substitution in reconstructive urological surgery: is an antireflux procedure necessary? J Urol. 1999;162:323–326. [PubMed] [Google Scholar]
- 24.Bazeed MA, El-Rakhawy M, Ashamallah A, El-Kappany H, El-Hammady S. Ileal replacement of the bilharzial ureter: is it worthwhile? J Urol. 1983;130:245–248. doi: 10.1016/s0022-5347(17)51084-8. [DOI] [PubMed] [Google Scholar]
- 25.Boxer RJ, Fritzsche P, Skinner DG, Kaufman JJ, Belt E, Smith RB, et al. Replacement of the ureter by small intestine: clinical application and results of the ileal ureter in 89 patients. J Urol. 1979;121:728–731. doi: 10.1016/s0022-5347(17)56972-4. [DOI] [PubMed] [Google Scholar]