Abstract
Objectives
The aim of this study was to assess the effectiveness of the Smart Care service for the diabetes management.
Methods
Fifty-six patients with diabetes mellitus were recruited in Daegu, Korea. All participants completed a diabetes management education course (diet, exercise, and complications) for their self-care and received access to a care management website through a netbook and smartphone. The website accepts uploads of glucose level, body weight, HbA1c, low-density lipoprotein cholesterol level, and blood pressure. Participants communicated with the care manager through the internal management system of the website. The intervention was applied for 6 months.
Results
Participants receiving the Smart Care service had lower blood glucose and HbA1c during 6 months follow-up when 1-month values (p < 0.001) were compared. There was no significant difference in body weight and body mass index between 1 month and 6 months. The average number of remote consultation with the Smart Care service per person was 10.4 by nurses, 3.0 by nutritionists, and 1.6 by sports curers. Regression analysis indicated that the number of times counseling was offered by nurses influences body weight and that the number of minutes of telephone counseling influences both body weight and body mass index.
Conclusions
We have confirmed that the Smart Care service might be an effective system for reduction in blood glucose and HbA1c. We expect that the Smart Care service will contribute to delaying diabetes complications and improving the quality of life of patients with diabetes.
Keywords: Diabetes Mellitus, Telemedicine, Remote Consultation, Medical Informatics, Health Services
I. Introduction
In the past, one of the vital purposes of medicine was the management of acute diseases; however, the main task of medicine is the management of chronic diseases today. Longer life expectancy, population aging, and increases in chronic diseases, especially higher diabetes prevalence, have all helped direct social attention towards health management and the quality of life, thereby amplifying the demand for medical care on a daily basis [1,2]. A report on diabetic patients in Korea indicates that 10.1% of persons aged 30 years or older as well as 22.7% of those aged 65 years or older have the disease [3]. As in-hospital treatment of patients with diabetes is a great financial burden to the healthcare system, it is recommended that each patient should self-manage their condition when it is necessary to have efficient communication without time restrictions between the patient and the specialist as well as to reduce medical cost [4,5].
According to InformationWeek Healthcare, an online journal, 78% of 1,002 survey participants recently cited insufficient amount of time as a problem in the communication between patients and medical specialists [6].
The medical community has been considering a new paradigm of using the internet and mobile communications to deal with this issue [7,8]. Yu et al. [8] studied the u-Health remote health service system; the diabetic management program included consultation sessions with research nurses based on the transmitted data from the blood glucose monitoring system by using mobile phones. Cho et al. [9] instructed their patients to transfer glucose, blood pressure, and body weight data for the nurses, nutritionists, and endocrinologists to monitor. Feedback was given at the request of a patient or upon the observation of significant changes in blood glucose level. Kim [10] reported improvements in HbA1c just through providing patients with simple mobile phone texts and Web-based feedback. There are ongoing studies actively testing a variety of software and u-Health medical equipment in search of alternative methods of medical communication for the self-care of patients with chronic illness [11,12,13,14,15]. The u-Health service is expected to change the venue of medical service from conventional hospitals to personal everyday spaces, making it easier for patients to self-manage their chronic conditions [5,16,17]. With little time restriction between the patient and the medical expert, the u-Health service is also anticipated to provide patients with self-confidence in managing their illnesses, to prevent any possible complications, and to increase their compliance with medical treatments [18].
An exemplary demonstration project that combines IT and the u-Health service is the Smart Care service developed by the Ministry of Knowledge and Economy of Korea [1,2,11]. The Smart Care system, currently under development for public use, is an IT-based everyday medical service intended to reduce medical costs, especially for low-income households [11]. The outcomes of u-Health service funded publicly and/or privately for the treatment of chronic illnesses will provide basic clinical data to facilitate further u-Health service projects. These will also expedite similar projects, accelerating the commercialization of the u-Health service in the near future [5,9,11,12,13,14,15].
From among the medical institutions participating in the "2011 Smart Care demonstration scheme by the Ministry of Knowledge Economy of Korea," we chose a group of patients with diabetes from primary healthcare centers in Korea to test the effectiveness of the Smart Care service by investigating pre-post service changes in blood glucose level, body weight, body mass index, glycated hemoglobin (HbA1c) level, fasting glucose level, low-density lipoprotein cholesterol level, and systolic/diastolic blood pressure.
II. Methods
1. Design
The present study examined all diabetes indicators in patients with diabetes who used the Smart Care service in order to look for any significant changes resulting from the use of the service. Previous studies on the effectiveness of the u-Health service have been mainly conducted in tertiary medical institutions [8,9,10], with few being carried out by primary healthcare institutions. The present study focused on the applicability of the u-Health care service in primary healthcare facilities; therefore, a study design was adopted in which there was a single experimental group for the comparison of data before and after the intervention.
2. Participants
The study included 56 patients with diabetes who were recruited through leaflets and posters introducing the Smart Care service. They were receiving drug treatment in primary healthcare institutions located in Daegu, Korea, between December 2011 and August 2012. Clinically experienced and licensed nurses who had received training on the Smart Care system and diabetes were charged with explaining to the interested patients the purposes and objectives of the study. Patients with serious kidney or liver complications were excluded from the study.
3. Procedure
Participating patients received six months of remote treatment that covered disease management consultations, care planning, drug administration, dietary and nutritional management, as well as an exercise regimen, while the existing hospital treatment and medications prescribed for their illness were maintained. Health specialists at the Smart Care service center included doctors who managed the overall center, full-time nurses who provided consultations and educational services, nutritionist, and sports curers. All the staff members were appropriately licensed, and they had completed separate diabetic management courses on the subjects of the Smart Care service system, namely, diet, exercise, consultations, and education.
Participants were supplied with a blood glucose monitoring system, a body composition analyzer (InBody IH-U070B; Biospace, Seoul, Korea), and a computer terminal (a PC or a smartphone) installed with the Smart Care service program. Personal training visits were given to each patient to teach them how to use all the contents. Patients using the system were to estimate their blood glucose and body composition levels at home at least once a day, or 4 times at most, and to send the data to the Smart Care service center. In addition, the primary healthcare centers transmitted the patients' laboratory data that were collected from the patient's hospital visits (five times or more) to the Smart Care central server during the study period. On the basis of the test results and the lifestyle record, a monthly health report, including a personalized exercise routine and a dietary plan, was sent to each patient. A weekly version of the report was also delivered to inform the patient of his or her health evaluation and health-related concerns.
Nurses conducted most of the consultations, with the nutritionists contacting the patients to give personal advice when necessary. Sports curers spoke to patients over the telephone when they were asked to provide guidance and instructions.
4. Ethical Concerns
The Smart Care demonstration project received authorization from the Ministry of Health and Welfare of Korea in accordance with Article 44 of the "Framework Act on Health and Medical Services" (Health and Medical Services Demonstration Projects). Those who were eligible and agreed to participate were provided explanations by research assistants about the general rationales of the study, and they were asked to complete a package of written forms, including a participation consent form.
5. Statistical Analysis
IBM SPSS ver. 20 (IBM, Armonk, NY, USA) was used for data analyses. Descriptive data on the participants and their service usage are presented in numbers, percentages, means, and standard deviations. To evaluate changes induced by the 6-month Smart Care service, repeated measure ANOVA was carried out for the glucose level, body weight, and body mass index, whereas a paired t-test was adopted for the HbA1c level, fasting glucose level, low-density lipoprotein cholesterol level, and systolic/diastolic blood pressure. Multiple regression analysis was used to determine which Smart Care service affected blood glucose level, body weight, body mass index, HbA1c, fasting glucose level, low-density lipoprotein cholesterol level, and systolic/diastolic blood pressure.
III. Results
1. Characteristics of Participants and Frequency of Blood Glucose Test
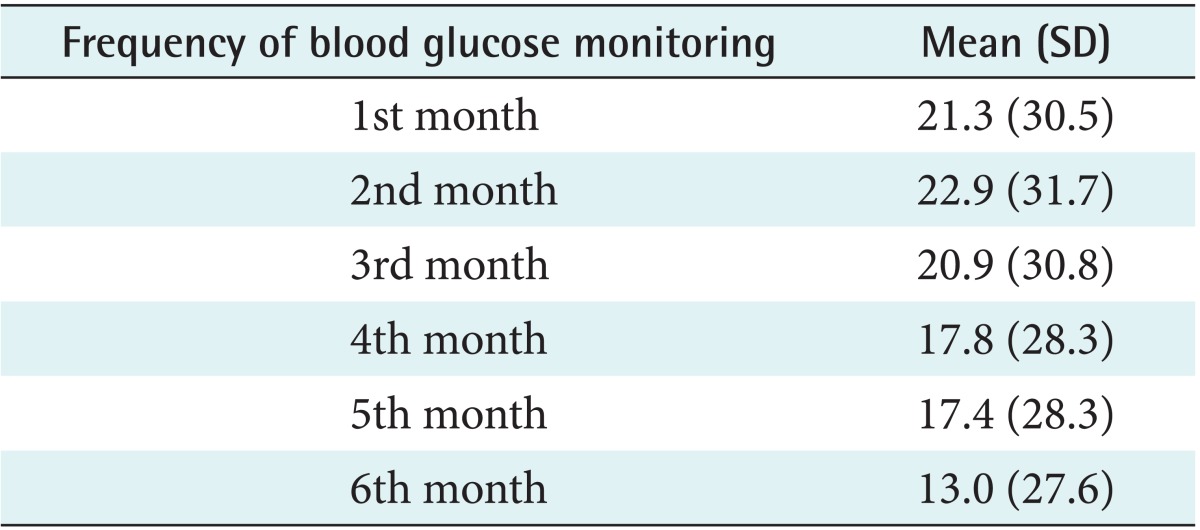
The participants included 34 men and 22 women, totaling 56 patients. The mean age of the participants was 55.2 years (Table 1). The frequency of blood glucose tests averaged 21.3 times during the first month and was reduced to 13 times in the final sixth month (Table 2).
Table 1.
Characteristics of participants (n = 56)
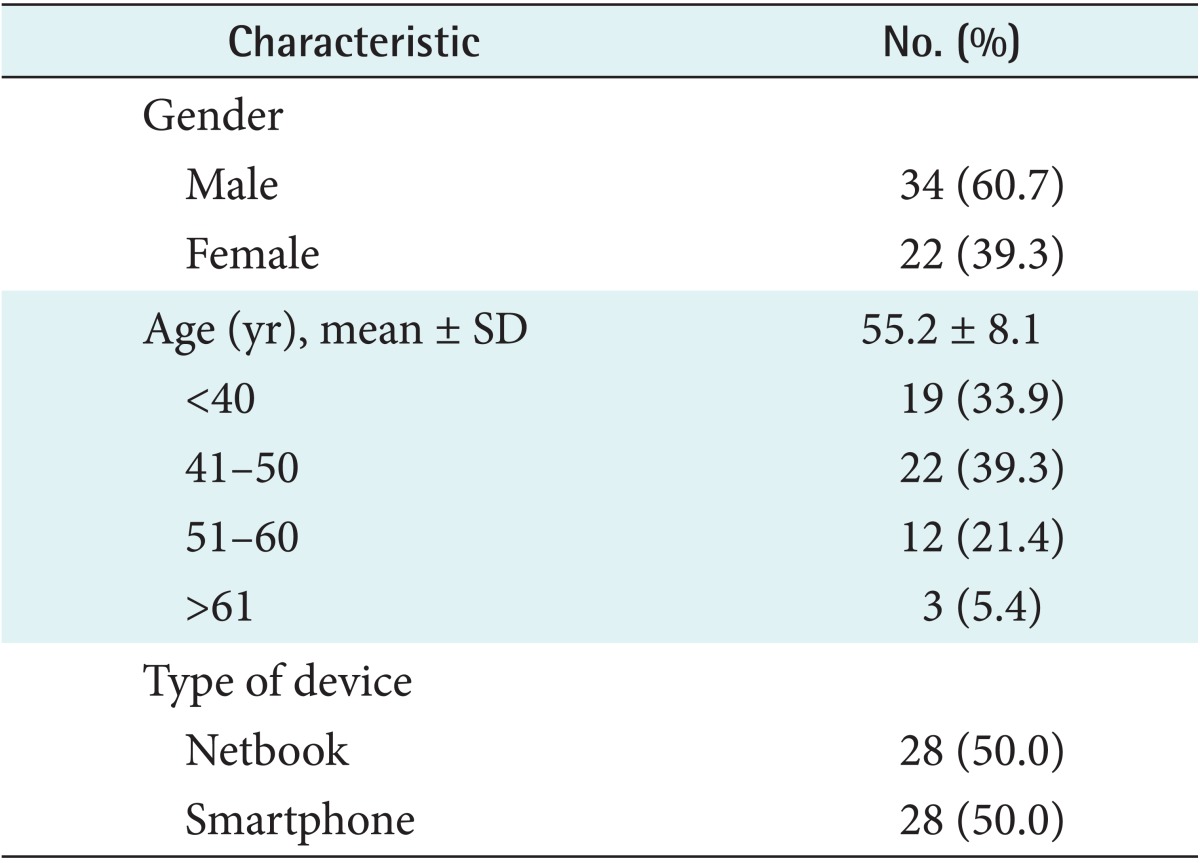
Table 2.
Frequency of blood glucose monitoring (n = 56)
2. Provided Smart Care Service
Table 3 gives the overall regularity of the service as requested by the patients (inbound call service) and as initiated by the service provider (outbound call service) in providing consultations and education to the patients. As for the inbound service, 56 patients used telephones, which represents 4.7 times per person on average, whereas 28 patients used video calls (2.2 times per patient), and 11 used online messaging (10.4 times per patient). The outbound service initiated by the health specialists of the center occurred through telephone calls to 56 patients (12.8 times per patient on average), video calls to 5 patients (1.2 times per patient), and online messaging to 11 patients (10.4 times per patient). Weekly and monthly health reports were delivered to 56 patients (25.3 times per patient) and 56 patients (5.2 times per patient), respectively. An average telephone consultation session lasted for 76.1 minutes per person.
Table 3.
Average number of provided service during 6 months
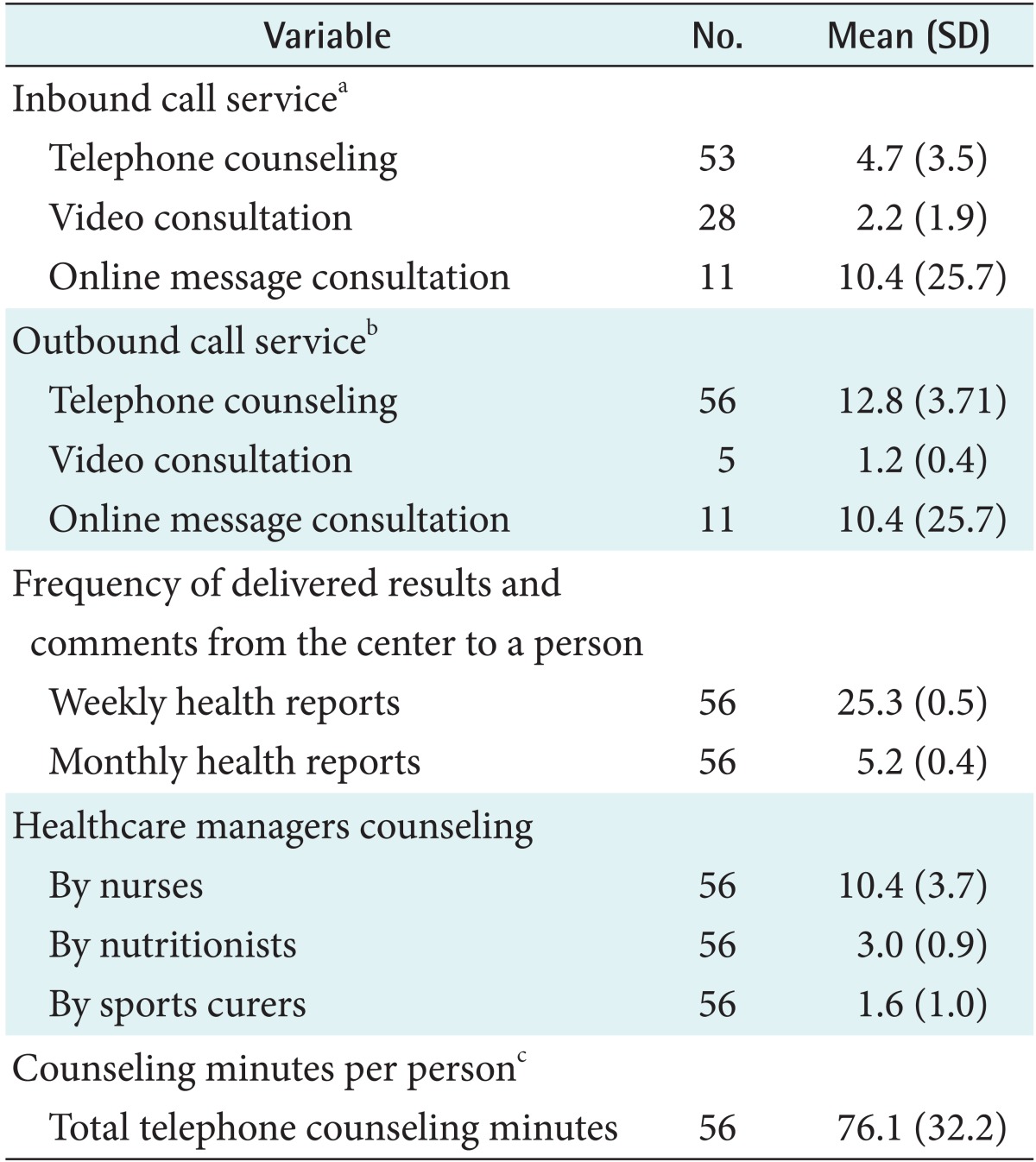
aCall from participants to the center, bcall from the center to participants, cduring 6 months.
3. Changes in Test Results after the Smart Care Service
Blood glucose showed a decreasing trend from the initial 163.8 to 149.1 mg/dL at the 4-month point, and further down to 146.4 mg/dL at the 6-month point (p < 0.001). The changes in body weight and body mass index were not significant (Table 4).
Table 4.
Change of blood glucose, body weight, and body mass index during 6 months (n = 56)
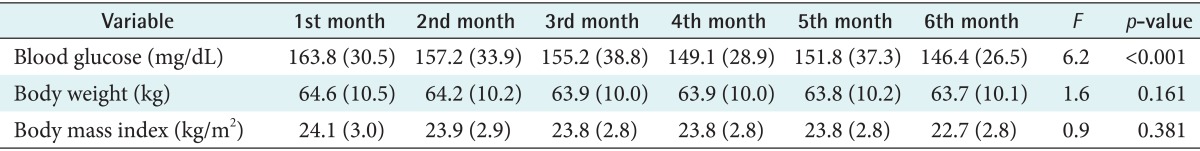
Values are presented as mean (SD).
Repeated measure ANOVA was applied.
The mean initial HbA1c was 7.5%, which decreased to 6.6% after 6 months (p < 0.001). The change in the fasting glucose level was also significant, with the initial mean estimated at 192.8 mg/dL, decreasing to 145.5 mg/dL after 6 months (p < 0.01). A similar significant tendency was found for low-density lipoprotein cholesterol (p < 0.05). Both systolic blood pressure and diastolic blood pressure dropped after the service duration, with statistical significance, from 125 to 119.6 mmHg and from 72.1 to 67.9 mmHg, respectively (p < 0.01) (Table 5).
Table 5.
Laboratory data of subjects before and after the Smart Care service
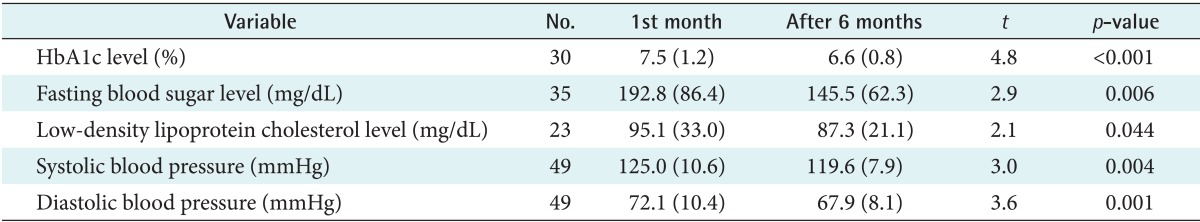
Values are presented as mean (SD).
Paired t-test was adopted.
4. Smart Care Service Influencing Laboratory Data
Multiple regression analyses were used to identify significant predictors of blood glucose level, body weight, body mass index, HbA1c, fasting glucose level, low-density lipoprotein cholesterol level, and systolic/diastolic blood pressure (Table 6). A separate multiple regression analysis was performed for each dependent variable. Each analysis included the following independent variables: number of consultations provided by nurses, number of consultations provided by nutritionists, number of consultations provided by sports curers, minutes of telephone counseling, and number of video consultations. The regression model was significant for the dependent variable of body weight (F = 6.27, p = 0.002, adjusted R2 = 0.545) and body mass index (F = 4.41, p = 0.014, adjusted R2 = 0.487). Body weight was significantly predicted by the number of consultations provided by nurses (p = 0.025) and minutes of telephone counseling (p = 0.034). Body mass index was significantly predicted by minutes of telephone counseling (p = 0.044).
Table 6.
Smart Care service influencing laboratory data
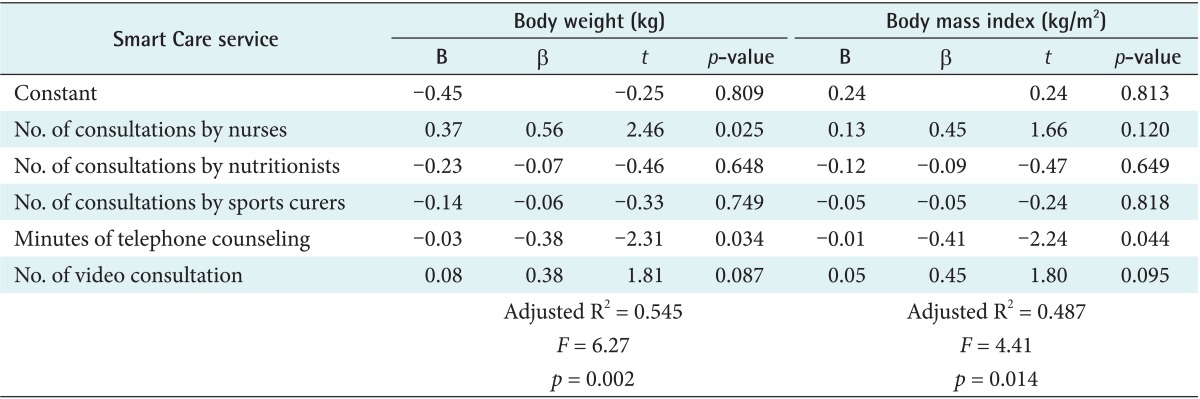
B is the unstandardized regression coefficient, β is the standardized regression coefficient.
IV. Discussion
The present study attempted to validate the effectiveness of the Smart Care service by examining changes in diabetes indicators in patients with diabetes receiving treatments from primary health institutions. The project provided patients with a specialized health management service by means of two-way communication through netbooks or smartphones. Several previous studies have dealt with patients registered in tertiary healthcare institution [8,9,10], whereas the current study focused on those registered with primary medical centers. Patients attended to by primary healthcare institutions are more likely to be in an early stage of their illness and have fewer complications, relative to their counterparts in tertiary institutions. Patients in primary care units are therefore better positioned to benefit from remote health management services and to be able to afford to continue with the program for general education and motivation. The objectives of the u-Health service for patients with diabetes are to prevent macrovascular complications-such as myocardial infarction, angina, stroke, and transient ischemic attack-and microvascular complications-such as retinopathy, kidney disease, nerve disorders, and foot ulcers-by keeping glucose level, body mass index, HbA1c level, cholesterol level, and blood pressure within the reference ranges. This could also help reduce general medical costs, as diabetes imposes a large financial burden on patients who often have to be hospitalized repeatedly due to complications [19].
We believe that we have reached a point at which society needs to agree that, to bring about meaningful changes in lifestyles and health indicators in patients with diabetes, remote IT-based health management service needs to replace the existing home monitoring systems so that patients can have access to feedback and real-time care from medical specialists [11]. As a first of its kind, the Smart Care service establishes a central service center and provides patients with specialist health consultations through telephone, video, and online messaging on a regular and on-demand basis. As a result, all diabetes indicators, including glucose level, HbA1c, fasting glucose level, low-density lipoprotein cholesterol level, and systolic/diastolic blood pressure, improved significantly, except for body mass index and body weight. After the 6-month period of Smart Care service, the mean post-meal blood glucose was within the reference range at 146.4 mg/dL (normal range 90-180 mg/dL for 2 hours after meal), whereas the fasting sugar level was beyond the reference range at 145.5 mg/dL (normal range 70-130 mg/dL). The HbA1c was 6.6%, close to the reference range (normal range for <6.5%) [20]. From previous studies [8,9,10], we noted that a short study period would make it difficult to validate the effectiveness of an experimental service. Moreover, even if a study lasted for a longer duration, the effectiveness was restricted when there were no face-to-face interactions between the patients and care providers [9,10]. The present regression analysis indicated that the number of consultations provided by nurses influences body weight, and that minutes of telephone counseling influence both body weight and body mass index. These results provide preliminary evidence that counseling has positive intervention effects on control of body weight and body mass index. As some previous studies have indicated, an IT-based u-Health service should provide emotional support and encouragement to the patient in addition to providing personal counseling for proper self-care management, rather leaving patients to depend on the technological and mechanical aspects of the service [21,22].
Our results show that the frequency of checking blood glucose was initially an average of 21.3 times, but it decreased to 13.0 times at the 6-month point. It is thought that the patients were at first eager to check their levels when the figures were unstable, but they seem to have gradually lost interest as the indicators showed more stable values with time. It is therefore necessary to give patients more encouragement and counseling so that they would continuously attend check-ups. Following the relevant guidelines based on the current glucose level and reacting to any unwanted changes can not only reduce the necessity for hospital visits but also help prevent microvascular complications [19,23]. It has been reported that stabilized fasting blood glucose levels can lead to a lower prevalence of cardiovascular complications and a lower death rate in patients with type 2 diabetes [24].
The present study offers a few unique aspects compared with other studies on patients with diabetes. First we offered the patients weekly interactions with the medical team through telephone/video calls and online messaging, overcoming the drawback that existing u-Health services do not offer continuous contacts with medical personnel, with the patient only transmitting their test data to the central service [25]. These sessions were intended to follow the core objectives of the u-Health service, which were to save time and monetary cost that patients would incur if they visited the hospital. Second, we delivered such health-related contents as test data analysis and health information to patients once a week. The medical team would check blood glucose data transmitted by patients and send back appropriate feedback in return, as well as educational material and encouragement to patients to manage their glucose levels. This is thought to be an ideal way to maintain interest and motivate patients about diabetes management.
The present study indicates that it might be necessary to consider an IT-based remote health management system through which medical specialists can provide monitoring service and feedback to diabetes patients so that they would aim to improve their lifestyle and induce significant changes in their blood glucose levels. Although the service is dependent on IT and is remotely administered, the focus should be on the provision of active medical interventions on the part of the health specialists. It would be vital for patients to feel confident about their capability in disease management and prevention of complications. The fundamental part of diabetes management is to check blood glucose levels on a regular basis and understand each patient's personal attributes in order to find out how to keep the levels within the reference range without much variation. The ultimate aim would be to prevent complications. Health specialists are strongly advised to continue encouraging and interacting with their patients to this end.
The present study had a few limitations. First, we focused on the application of the u-Health service to patients in primary healthcare institutions where a control group was lacking in the study design. Although we succeeded in validating the potential effectiveness of the Smart Care service, we should have had a control group to make certain that the changes we observed in terms of the blood glucose level, cholesterol level, and blood pressure were indeed due to the Smart Care service. To correct this issue, we are in the process of conducting another study in a university hospital setting, consisting of an experimental group and a control group. Another issue is that there was a slight dropout rate regardless of the patient education and motivation provided by the health service team. The reasons for dropping out were manifold: lack of time, finding the tools being too difficult to use, not wanting to continue, no response, and others. Reflection on this issue and finding ways to reduce the loss of participants would be helpful for future studies. Regardless of these drawbacks, the current study was able to substantiate the effectiveness of the Smart Care service; useful data was gathered and analyzed and may be helpful in determining directions for further u-Health projects.
Acknowledgments
This study was supported by a 2010 research grant from the Ministry of Trade, Industry and Energy of Korea (No. 1003518).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Lee JY. Domestic u-Health demonstration project progress status and implications. Inf Commun Policy. 2008;20(21):25–44. [Google Scholar]
- 2.Martin S, Kelly G, Kernohan WG, McCreight B, Nugent C. Smart home technologies for health and social care support. Cochrane Database Syst Rev. 2008;(4):CD006412. doi: 10.1002/14651858.CD006412.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Korea Ministry of Health & Welfare; Korea Center for Disease Control and Prevention. Korea Health Statistics 2011 Korea National Health and Nutrition Examination Survey (KNHANES V-2) Cheongju: Korea Ministry of Health & Welfare, Korea Center for Disease Control and Prevention; 2011. [Google Scholar]
- 4.McMahon GT, Gomes HE, Hickson Hohne S, Hu TM, Levine BA, Conlin PR. Web-based care management in patients with poorly controlled diabetes. Diabetes Care. 2005;28(7):1624–1629. doi: 10.2337/diacare.28.7.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choi EH, Seo JY. u-Health for management of chronic diseases: physical activity and therapeutic exercise. J Korean Med Assoc. 2009;52(12):1154–1163. [Google Scholar]
- 6.Lewis N. 57% of consumers use Internet for medical questions [Internet] San Francisco (CA): InformationWeek; 2012. [cited at 2014 May 23]. Available from: http://www.informationweek.com/healthcare/patient/57-of-consumers-use-internet-for-medical/240001216. [Google Scholar]
- 7.Ralston JD, Revere D, Robins LS, Goldberg HI. Patients' experience with a diabetes support programme based on an interactive electronic medical record: qualitative study. BMJ. 2004;328(7449):1159. doi: 10.1136/bmj.328.7449.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yu SH, Kim SH, Kim SY, Choi SH, Lim S, Chang YS, et al. Effects of 'ubiquitous healthcare' on the ability of self-management in elderly diabetic patients. Korean Diabetes J. 2009;33(1):58–64. [Google Scholar]
- 9.Cho JH, Chang SA, Kwon HS, Choi YH, Ko SH, Moon SD, et al. Long-term effect of the Internet-based glucose monitoring system on HbA1c reduction and glucose stability: a 30-month follow-up study for diabetes management with a ubiquitous medical care system. Diabetes Care. 2006;29(12):2625–2631. doi: 10.2337/dc05-2371. [DOI] [PubMed] [Google Scholar]
- 10.Kim SI, Kim HS. Effectiveness of mobile and internet intervention in patients with obese type 2 diabetes. Int J Med Inform. 2008;77(6):399–404. doi: 10.1016/j.ijmedinf.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 11.Chung YS, Moon MK, Lee CH. The effect of smart care ubiquitous health service on hypertension management. J Korean Acad Ind Soc. 2013;14(3):1213–1220. [Google Scholar]
- 12.Lee IK, Kim HS, Cho H. Development of an ubiquitous healthcare system based on health information exchange standards. J Korean Inst Intell Syst. 2012;22(3):273–280. [Google Scholar]
- 13.Lee SC, Chung WY. Development of mobile u-Healthcare system in WSN. J Korean Inst Commun Sci. 2012;37C(4):338–346. [Google Scholar]
- 14.Nam MH, Kim SC, Kim JS, Lee KN, Kim S, Cha JH, et al. Evaluation method of portable handheld u-Healthcare medical devices. J Inst Electron Eng Korea SC. 2012;49(2):55–62. [Google Scholar]
- 15.Yang HS, Jin JY. The u-Health care software testing method for a reliability secure. J Korean Acad Ind Soc. 2011;12(3):1427–1438. [Google Scholar]
- 16.Song TM, Lee SY, Lee KH, Jin DL, Ryu SW, Jang SH. u-Health: current status and tasks ahead. Seoul: The Korea Institute for Health and Social Affairs; 2011. [Google Scholar]
- 17.Ryu GT, Choi H. Implementation of u-Healthcare system for chronic disease management. J Inst Electron Eng Korea. 2014;51(1):233–240. [Google Scholar]
- 18.Bu D, Pan E, Walker J, Adler-Milstein J, Kendrick D, Hook JM, et al. Benefits of information technology-enabled diabetes management. Diabetes Care. 2007;30(5):1137–1142. doi: 10.2337/dc06-2101. [DOI] [PubMed] [Google Scholar]
- 19.O'Brien JA, Patrick AR, Caro JJ. Cost of managing complications resulting from type 2 diabetes mellitus in Canada. BMC Health Serv Res. 2003;3(1):7. doi: 10.1186/1472-6963-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Korea Diabetes Association. Diabetes Class [Internet] Seoul: Korea Diabetes Association; c2011. [cited at 2014 May 23]. Available from: http://www.diabetes.or.kr/general/class/medical.php?mode=view&number=322&idx=6. [Google Scholar]
- 21.Polonsky WH, Earles J, Smith S, Pease DJ, Macmillan M, Christensen R, et al. Integrating medical management with diabetes self-management training: a randomized control trial of the Diabetes Outpatient Intensive Treatment program. Diabetes Care. 2003;26(11):3048–3053. doi: 10.2337/diacare.26.11.3048. [DOI] [PubMed] [Google Scholar]
- 22.Kerr EA, Gerzoff RB, Krein SL, Selby JV, Piette JD, Curb JD, et al. Diabetes care quality in the Veterans Affairs Health Care System and commercial managed care: the TRIAD study. Ann Intern Med. 2004;141(4):272–281. doi: 10.7326/0003-4819-141-4-200408170-00007. [DOI] [PubMed] [Google Scholar]
- 23.Franciosi M, Pellegrini F, De Berardis G, Belfiglio M, Di Nardo B, Greenfield S, et al. Self-monitoring of blood glucose in non-insulin-treated diabetic patients: a longitudinal evaluation of its impact on metabolic control. Diabet Med. 2005;22(7):900–906. doi: 10.1111/j.1464-5491.2005.01546.x. [DOI] [PubMed] [Google Scholar]
- 24.Brun E, Zoppini G, Zamboni C, Bonora E, Muggeo M. Glucose instability is associated with a high level of circulating p-selectin. Diabetes Care. 2001;24(9):1685. doi: 10.2337/diacare.24.9.1685. [DOI] [PubMed] [Google Scholar]
- 25.Ramadas A, Quek KF, Chan CK, Oldenburg B. Web-based interventions for the management of type 2 diabetes mellitus: a systematic review of recent evidence. Int J Med Inform. 2011;80(6):389–405. doi: 10.1016/j.ijmedinf.2011.02.002. [DOI] [PubMed] [Google Scholar]


