Abstract
Background
Children with autism spectrum disorders often present with comorbid anxiety disorders that cause significant functional impairment. This study tested a modular cognitive behavioral therapy (CBT) program for children with this profile. A standard CBT program was augmented with multiple treatment components designed to accommodate or remediate the social and adaptive skill deficits of children with ASD that could pose barriers to anxiety reduction.
Method
Forty children (7–11 years old) were randomly assigned to 16 sessions of CBT or a 3-month waitlist (36 completed treatment or waitlist). Therapists worked with individual families. The CBT model emphasized behavioral experimentation, parent-training, and school consultation. Independent evaluators blind to treatment condition conducted structured diagnostic interviews and parents and children completed anxiety symptom checklists at baseline and posttreatment/postwaitlist.
Results
In intent-to-treat analyses, 78.5% of the CBT group met Clinical Global Impressions-Improvement scale criteria for positive treatment response at posttreatment, as compared to only 8.7% of the waitlist group. CBT also out-performed the waitlist on diagnostic outcomes and parent reports of child anxiety, but not children's self-reports. Treatment gains were maintained at 3-month follow-up.
Conclusions
The CBT manual employed in this study is one of the first adaptations of an evidence-based treatment for children with autism spectrum disorders. Remission of anxiety disorders appears to be an achievable goal among high-functioning children with autism.
Keywords: Cognitive behavioral therapy, autism spectrum disorders, anxiety disorders, parent-training
Anxiety disorders are common among children with autism spectrum disorders (ASD) and are associated with heightened impairment in social functioning (Bellini, 2004; de Bruin, Ferdinand, Meester, de Nijs, & Verheij, 2007), leading investigators to call for treatments that address anxiety-related symptoms in ASD (e.g., Sofronoff, Attwood, & Hinton, 2005; Volkmar & Klin, 2000). Although probably efficacious intervention programs have been developed for typically developing youth with anxiety disorders (e.g., Barrett, Dadds, & Rapee, 1996), the linguistic, cognitive, and social characteristics of ASD (e.g., Baker, Koegel, & Koegel, 1998) may render standard treatment approaches less effective for children with ASD. This study is a randomized, controlled trial testing a modified cognitive behavior therapy (CBT) protocol for children with ASD and comorbid anxiety disorders.
Autism, Asperger syndrome, and pervasive developmental disorder not otherwise specified (PDD-NOS) affect as many as 1 out of 150 children (Centers for Disease Control, 2007), and many higher-functioning children with ASD are not diagnosed until elementary school or later (Fombonne, 2003). These disorders are typified by severe deficits in social communication and marked idiosyncratic behavior. Significant impairment in social and school/occupational functioning is common. Even when compared to other types of childhood psychopathology, ASD is particularly severe and longstanding (Howlin, Goode, Hutton, & Rutter, 2004).
Comorbid psychological disorders are common in the ASD population, with anxiety disorders affecting 30–80% of the sampled children in multiple studies (de Bruin et al., 2007; Klin, Pauls, Schultz, & Volkmar, 2005; Muris, Steerneman, Merckelbach, Holdrinet, & Meesters, 1998). The relative frequency of anxiety disorders among children with ASD indicates that anxiety could be an important treatment focus for many children on the autism spectrum (Volkmar & Klin, 2000). A recent survey conducted by the National Autistic Society found that anxiety was the second most highly cited problem reported by parents (Mills & Wing, 2005). Often, additional comorbid disorders coincide with anxiety disorders in the ASD population (e.g., ADHD, ODD, depression), resulting in complex and severe clinical presentations (de Bruin et al., 2007; Klin et al., 2005; Muris et al., 1998).
Diagnosing anxiety disorders among children with ASD may be complicated by children's communication impairments and emotion recognition deficits (Leyfer et al., 2006). Furthermore, certain symptoms of anxiety disorders may appear similar to symptoms of ASD (e.g., compulsions vs. repetitive behaviors) (Muris et al., 1998). Researchers have suggested that proper diagnosis of anxiety in ASD should involve evidence of behaviors not belonging to the core domains of ASD that are consistent with the physiological, behavioral, or affective features of anxiety disorders (e.g., sympathetic nervous system arousal, fears), and should distinguish impairment in functioning due to symptoms of anxiety from that due to symptoms of ASD (e.g., a lack of participation in class due to shyness rather than to due to communication deficits or engagement in stereotypies) (Leyfer et al., 2006; Matson & Nebel-Schwalm, 2007; Reaven & Hepburn, 2003).
Several case studies and exploratory clinical trials have suggested that CBT may help lessen anxiety symptoms in children with ASD (e.g., Chalfant, Rapee, & Carroll, 2006; Reaven & Hepburn, 2003; Sofronoff et al., 2005; Sze & Wood, 2007). Sofronoff and colleagues evaluated two variants of a 6-week CBT program in group-therapy format that focused on emotion recognition and cognitive restructuring for children with Asperger syndrome. Participating children were not diagnosed with anxiety disorders at pretreatment per se. However, parent-report measures showed declines in child anxiety symptoms in the CBT groups compared to a waitlist group. A 16-week group-therapy CBT intervention tested by Chalfant and colleagues included children with ASD and concurrent anxiety disorders and found that anxiety outcomes were superior for the immediate treatment group when compared to the waitlist group. Limitations in this study were that the study therapists, rather than independent evaluators blind to treatment assignment, administered the posttreatment diagnostic interviews, and that treatment fidelity was not assessed. Thus, while CBT may be a promising intervention modality for the ASD population, methodological characteristics of the extant studies preclude conclusions about efficacy (see APA Division 12 Task Force recommendations, e.g., Chambless & Hollon, 1998). Furthermore, the structured, linear format of group therapy limits matching intervention techniques to patient characteristics. Given the heterogeneity of presenting phenotypes in high-functioning ASD and, presumably, corresponding variations in underlying pathology, individual interventions that can be tailored to a patient's specific characteristics and strengths are likely to be particularly powerful (Mundy, Henderson, Inge, & Coman, 2007). A fully modular (cf. Chorpita, Taylor, Francis, Moffitt, & Austin, 2004), individually-focused CBT intervention was developed for this study to promote optimal treatment outcomes. To our knowledge, this is the first of its kind to be empirically evaluated in the ASD population.
A common finding in the ASD intervention literature is that skills and behavioral improvements acquired in therapeutic programs do not generalize to the settings where they are needed (e.g., school) (e.g., Hwang & Hughes, 2000). Therefore, additions and modifications to standard CBT protocols are necessary in order to produce generalized and durable change in children with ASD (e.g., Attwood, 2004).
The few articles published on CBT for anxiety in children with ASD have primarily focused on ways of adapting traditional CBT to help children access it, such as using visual aids and providing compensatory emotion education (e.g., Sofronoff et al., 2005). However, CBT may need to be substantially expanded to address ASD-related clinical characteristics that may cause or compound anxiety symptoms, or render them less treatable. Three such characteristics include poor social skills and perspective taking; poor adaptive skills; and circumscribed interests and stereotypies.
First, poor social skills are a key autism-related deficit that may reduce the efficacy of traditional CBT unless modifications are made. If a youth with social anxiety lacks basic social skills, these deficits must be compensated for prior to the youth facing feared social situations (e.g., joining in games with peers) (see Kasari, Chamberlain, & Bauminger, 2001). For instance, friendship skills may help youth with ASD to compensate for theory-of-mind deficits prior to initiating interactions with new peers (Frankel & Myatt, 2003; Kasari et al., 2001). Complementary peer intervention can increase peers' tolerance for differences in social communication and enhance their receptiveness to social overtures from children with ASD (Rogers, 2000). Parent and school provider involvement may also help support generalization in target settings (cf. Reaven & Hepburn, 2006).
Second, researchers have consistently found adaptive skill deficits, such as poor self-care and organizational skills, in individuals with higher-functioning ASD (e.g., Klin et al., 2007). Although anxiety disorders are typically characterized by unrealistic fears and perceptions of inefficacy, such self-care deficits may compound anxiety problems by introducing actual barriers to proficiency in feared situations. For example, some children with ASD might find typical CBT assignments such as going on play dates and sleepovers to be particularly daunting because their poor self-care skills could actually lead to humiliation (e.g., due to being unable to wipe; get shoes on and off; change into swimwear or pajamas; etc.), thus preventing success and self-efficacy. If ASD-related self-care deficits are not remediated prior to attempting these kinds of tasks during the course of CBT, children would likely experience failure rather than mastery. Integrating interventions that address self-care skill deficits may help children with ASD benefit more from traditional CBT techniques.
Third, circumscribed interests and stereotypies are core ASD symptoms that can interfere with developing social relationships and distract children from full participation in school (Attwood, 2003). Due to the ego-syntonic nature of circumscribed interests, they often can be incorporated into treatment as metaphors and incentives to increase children's motivation (Attwood, 2003; Baker et al., 1998) and foster therapeutic rapport (Sze & Wood, 2007). However, it is likely that treatment elements that can suppress the expression of such interests and the public display of repetitive mannerisms may be needed to enhance reciprocal social relationships with peers and others. Without addressing these core ASD symptoms, traditional CBT interventions such as graded exposure to social situations may be rendered less effective because peers respond less positively, preventing affected children from experiencing peer interactions as benign.
Developing efficacious interventions for children with ASD is a challenging endeavor, in part due to the severity and chronicity of ASD and the clinical complexity of the overlapping comorbid disorders with which many children present. Treatment approaches must consider and address the deficits in ASD that could undermine the efficacy of traditional CBT. Such modifications have been made to an existing family-focused CBT program for youth with anxiety disorders (Wood & McLeod, 2008). This study is the first evaluation of the modified treatment protocol. It was hypothesized that CBT would outperform a waitlist condition on a battery of child anxiety measures commonly used to test the efficacy of CBT in typically developing children.
Method
Participants
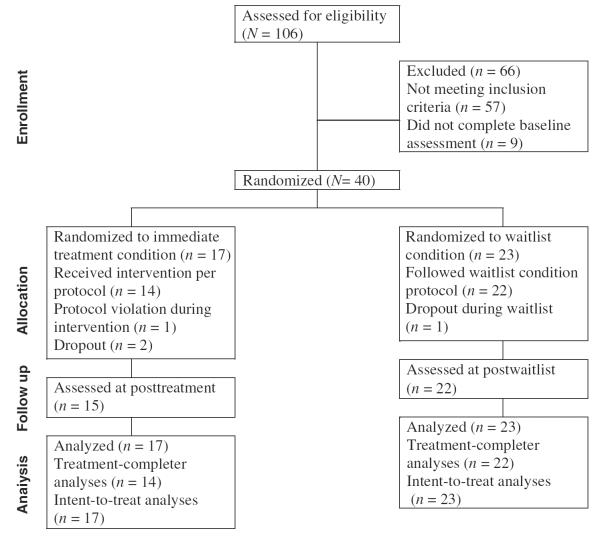
The intent-to-treat sample included 40 children with ASD and an anxiety disorder living in a major metropolitan area of the western United States, ranging in age from 7–11 years (M = 9.20, SD = 1.49), and their primary parents (defined as parents who were primarily responsible for overseeing the child's daily activities). Sample size was determined using a power analysis assuming a large ES for group differences at posttreatment/postwaitlist. This ES estimate was used in view of previous CBT trials for child anxiety disorders that have generated large effects (e.g. Barrett et al., 1996; Wood, Piacentini, Southam-Gerow, Chu, & Sigman, 2006). Children were referred by a medical center-based autism clinic, regional centers, parent support groups, and school personnel such as inclusion specialists. See Figure 1 for descriptive data on patient flow through the study.
Figure 1.
CONSORT flow diagram
Participants met the following inclusion criteria: (a) met research criteria for a diagnosis of autism, Asperger syndrome, or PDD-NOS (see below); (b) met research criteria for one of the following anxiety disorders: separation anxiety disorder (SAD), social phobia, or obsessive compulsive disorder (OCD) (see below);1 (c) were not taking any psychiatric medication at the baseline assessment, or were taking a stable dose of psychiatric medication (i.e., at least one month at the same dosage prior to the baseline assessment), and (d) if medication was being used, children maintained the same dosage throughout the study. This study was approved by a university-based IRB. Parents gave written informed consent and children gave written assent to participate in the study.
Families were excluded if (a) the child had a verbal IQ less than 70 (as assessed in previous testing, or, if there was any question about the child's verbal abilities noted by the independent evaluator at baseline, on the basis of the Wechsler Intelligence Scale for Children-IV administered by the independent evaluator); (b) the child was currently in psychotherapy or social skills training, or was receiving behavioral interventions such as applied behavior analysis; (c) the family was currently in family therapy or a parenting class; (d) the child began taking psychiatric medication or changed his/her dosage during the intervention; or (e) for any reason the child or parents appeared unable to participate in the intervention program.
Table 1 presents descriptive information for participating families. Thirty-seven primary parents also reported their annual family income. Nine (24.3%) reported an income below $40,000; 10 (27.1%) reported an income between $40,001 and $90,000; and 18 (48.6%) reported an income over $90,000 per year.
Table 1.
Demographics, diagnoses, and medication usage for children in the immediate treatment (IT) and waitlist (WL) conditions
| IT No. (%) n = 17 | WL No. (%) n = 23 | χ2 / t | |
|---|---|---|---|
| Child sex (male) | 12 (71%) | 15 (65%) | .13 |
| Child age | 9.18 (SD = 1.42) | 9.22 (SD = 1.57) | −.09 |
| Parent sex (female) | 14 (82%) | 18 (78%) | .10 |
| Parent graduated from college | 12 (71%) | 13 (60%) | .83 |
| Parent married/remarried | 14 (82%) | 19 (83%) | .00 |
| Child ethnic background | |||
| Caucasian | 8 (47%) | 11 (48%) | 2.50 |
| Latino/Latina | 2 (12%) | 3 (13%) | |
| Asian/Pacific Islander | 4 (23%) | 2 (9%) | |
| African American | 0 | 1 (4%) | |
| Multiracial | 3 (18%) | 6 (26%) | |
| Asian/ Caucasian | 1 | 1 | |
| Asian/Latino | 0 | 1 | |
| African American/Caucasian | 0 | 2 | |
| Latino/Caucasian | 1 | 1 | |
| Middle Eastern/Caucasian | 1 | 0 | |
| Multiracial (> 3) | 0 | 1 | |
| Autism spectrum disorders | |||
| Autistic disorder | 9 (53%) | 11 (48%) | 1.13 |
| PDD-NOS | 6 (35%) | 11 (48%) | |
| Asperger syndrome | 2 (12%) | 1 (4%) | |
| Baseline anxiety disorders | |||
| SoP | 13 (76%) | 22 (96%) | 3.29 |
| SAD | 8 (47%) | 16 (70%) | 2.06 |
| OCD | 8 (47%) | 9 (39%) | .25 |
| GAD | 11 (65%) | 8 (35%) | 3.51 |
| Other comorbid diagnoses | |||
| ADHD | 9 (53%) | 15 (65%) | .61 |
| Dysthymia/MDD | 3 (18%) | 0 | 4.39* |
| ODD/CD | 2 (12%) | 6 (26%) | 1.25 |
| PTSD | 0 | 1 (4%) | .76 |
| Psychiatric medication use | |||
| SSRI | 2 (12%) | 3 (13%) | .01 |
| Atypical antipsychotic | 3 (18%) | 3 (13%) | .16 |
| Stimulant or atomoxetine | 4 (24%) | 7 (30%) | .23 |
Note. IT = immediate treatment condition; WL = waitlist condition. SoP = social phobia; SAD = separation anxiety disorder; OCD = obsessive-compulsive disorder; GAD = generalized anxiety disorder; ADHD = attention deficit hyperactivity disorder; MDD = major depressive disorder; ODD = oppositional defiant disorder; CD = conduct disorder; PTSD = posttraumatic stress disorder.
p < .05.
Intervention program
Therapists included eleven doctoral students in clinical or educational psychology and two doctoral-level psychologists. All therapists were in (or had graduated from) an educational or clinical psychology doctoral program at a major research university, had at least one year of previous clinical experience, and had experience working with children with autism. Therapists received at least 8 hours of initial training on the intervention, read the treatment manual, listened to a set of audiotapes of a model therapist conducting the treatment, and attended weekly hour-long meetings with clinical supervisors (doctoral level psychologists who developed the protocols). Therapists worked with families for 16 weekly sessions, each lasting 90 minutes (about 30 minutes with the child and 60 minutes with the parents/family), implementing a version of the Building Confidence CBT program (Wood & McLeod, 2008) modified by the study authors for use with children with ASD. As with other CBT programs for child anxiety disorders, the manual includes coping skills training (e.g., affect recognition, cognitive restructuring, and the principle of exposure) followed by in vivo exposure (facing feared situations repeatedly while using the coping skills that have been learned, and remaining in the situations until habituation occurs). A hierarchy is created in which feared situations are ordered from least to most distressing. Children work their way up the hierarchy and are rewarded as they attempt increasingly fearful activities. The parent training components of the intervention focus on supporting in vivo exposures, using positive reinforcement, and using communication skills to encourage children's independence and autonomy in daily routines.
Enhancements to the manual were designed to address poor social skills, adaptive skills deficits, circumscribed interests and stereotypies, poor attention and motivation, common comorbidities in ASD (e.g., disruptive behavior disorders), and school-based problems. In the revised manual, four new modules for children, four new modules for parents, and a school-intervention module address social skills deficits. In these modules, children and parents are taught friendship skills (e.g., giving compliments, acting like a good sport, becoming a good playdate host, etc.) (cf. Frankel & Myatt, 2003) and children are given social coaching by the therapist, parents, and available school providers on appropriate ways to enter interactions and (later in treatment) maintain conversations with peers. Unlike traditional social skills training, social coaching is provided on-site immediately before attempting to join a social activity at school or home or in public, adapting promising priming techniques developed for children with autism (Koegel, Werner, Vismara, & Koegel, 2005). These skills are practiced at school and during play dates and are reinforced with a comprehensive reward system that relies on both daily privileges and longer-term incentives. And a set of new modules address the social isolation that many children with ASD experience at school by setting up peer `buddy' and mentoring programs (with the child serving as both mentor and mentee). These modules are also intended to enhance social acceptance and theory of mind (cf. Fulk & King, 2001; King-Sears, 2001; Maheady, Harper, & Mallette, 2001; Rogers, 2000) and remediate social avoidance (e.g., a preference for sitting alone during recess – a behavior that is often multiply determined by poor social skills, a rejecting social environment, as well as tertiary social anxiety). Two meetings are scheduled at the child's school to teach the social intervention techniques to relevant school providers (e.g., aides, teachers).
Another module focuses on building independence in age-appropriate self-help skills (e.g., dressing, organization) by focusing on motivating concepts for children (e.g., `becoming really grown up') and parents (e.g., focusing on the long-term sequelae of poor adaptive skills), and using a task analysis to break difficult new skills into small steps. Children's circumscribed interests and stereotypies are incorporated into the intervention in two ways. To address deficits in children's attention and motivation, therapeutic concepts (e.g., emotion recognition, cognitive restructuring) are taught using children's special interests as examples (e.g., for a child primarily interested in a particular cartoon character, the character's `feelings' and `thoughts' in anxiety-provoking or socially awkward situations could serve as the basis of discussion) and as rewards (e.g., granting access to the preferred stimulus). Later in treatment, after rapport has been established, a suppression approach is introduced, in which increasing amounts of time per day are devoted to consciously refraining from discussing or engaging in activities related to the circumscribed interest (cf. Sze & Wood, 2007) or engaging in stereotypies such as flapping. To help children understand the rationale for suppression, information about social expectations and acceptance is provided during these modules (e.g., that these behaviors are fine in private but tend to confuse peers and get in the way of friendship).
To address the most problematic aspects of comorbid disruptive behavior disorders, behavioral problems (failure to follow directions, aggression, and teasing/disrespectful language) are incorporated into the child's rewards system, using contingency management procedures. For instance, children might earn points or privileges each day for using polite language all day with one or two exceptions. As needed, school providers are recruited to send a daily school-home note to the parents to determine whether the target behaviors are met in the school setting.
The intervention program is flexible in nature and employs a modular format. Following a treatment algorithm (see Sze & Wood, 2007), therapy modules are selected on a session-by-session basis to address the child's most pressing clinical needs. Modular implementation of manualized therapies has been advocated as a means of individualizing treatments to specific children and providing more efficient clinical interventions (Chorpita et al., 2004). Despite the added flexibility of the modular format, a minimum of three sessions are spent on basic coping skills and eight are spent on in vivo exposure to ensure an adequate and comparable dose of the core elements of CBT for anxiety across cases.
Anxiety measures
Trained graduate student independent evaluators who were blind to the intervention condition of each family conducted diagnostic interviews before and immediately after intervention or waitlist. Children's Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association, 2000) disorders were assessed on the basis of separate semi-structured diagnostic interviews with the caregiver(s) and the child using the ADIS-C/P (Silverman & Albano, 1996), an instrument with favorable psychometric properties (e.g., Wood et al., 2002).
Interviewer training involved attending a presentation on the administration of the interview, observing and coding a videotaped interview, co-rating multiple live interviews conducted by a trained diagnostician, and finally, assuming satisfactory completion of the earlier steps, conducting at least one interview using the ADIS-C/P while under the supervision of a trained diagnostician.
Positive reports from either parent or child (the `or' rule) were considered sufficient for rating a criterion as present. Evaluators made ratings on the ADIS-C/P Clinical Severity Rating scale (CSR; 0 = not at all, 4 = some, 8 = very, very much) for each assigned diagnosis. Ratings of 4 or above are considered to be of a clinical level.
Fifteen percent of ADIS-C/P diagnostic assessments, including both immediate treatment and waiting list cases as well as baseline and posttreatment/postwaitlist assessments were reviewed by a diagnostic review team (also blind to participants' conditions) including trained doctoral students who routinely administered the ADIS-C/P and at least one clinical psychologist experienced in the diagnosis and treatment of childhood anxiety disorders. During these meetings, the diagnostician presented the symptoms reported by the child and his or her parents during the ADIS-C/P interview without revealing to the team the DSM-IV diagnoses that she/he had assigned. The team then came to a consensus decision about each child's diagnostic profile. Agreement between clinician and consensus severity ratings (ICCs: Social Phobia, .86; SAD, .76; and OCD, .70) and diagnoses (kappas: Social Phobia, .84; SAD, .86; and OCD, .71) was adequate.
The Clinical Global Impression (CGI) – Improvement Scale provided a global rating of improvement in anxiety symptoms ranging from 1 (completely recovered) to 5 (no change) to 8 (very much worse), and served as the primary outcome in this trial (see Wood et al., 2006). The trained graduate student independent evaluators who administered the ADIS-C/P used this scale to rate each child's improvement (or decline) at the posttreatment/postwaitlist assessment. To produce a rating, the independent evaluator conducted the follow-up interview and reviewed the baseline ADIS-C/P interviews for comparison with current signs of anxiety and related impairment. Children receiving a rating of 1, 2, or 3 (completely recovered, very much better, or much better) are considered treatment responders. Agreement between clinician and consensus-team CGI scores was perfect (kappa = 1.00).
The Multidimensional Anxiety Scale for Children (MASC; March, 1998) was administered to children and the parallel parent-report version of the MASC (cf. Wood et al., 2002) was administered to primary parents. The MASC is a 39-item, 4-point Likert-type scale with robust psychometric properties (March, Parker, Sullivan, Stallings, & Conners, 1997). Preliminary evidence suggests it may also perform well in ASD samples (Bellini, 2004). Alphas were .85 for the child MASC and .88 for the parent MASC. T-scores are not available for the parent MASC; thus, raw scores are reported for both parent and child MASC.
ASD diagnostic measures
In consultation with Dr Ami Klin, a recently published diagnostic algorithm was employed to distinguish between autism, Asperger syndrome, and PDD-NOS (Klin et al., 2005). The `New System' relies on scores from the Autism Diagnosis Interview-Revised (ADI-R; Le Couteur, Lord, & Rutter, 2003), Autism Diagnostic Observation Schedule–Module 3 (ADOS; Lord, Rutter, DiLavore, & Risi, 2002), a parent-report checklist pertaining to children's circumscribed interests, and a review of all available previous assessment records. The ADI-R and ADOS were administered by doctoral students and doctoral-level psychologists who received appropriate training and certification in their administration.
Procedure
This study was conducted in compliance with a university-based IRB. Phone contact was initiated by parents referred to the study. Baseline diagnostic interviews and pencil-and-paper measures were completed over the course of two days. Children who met all inclusion/exclusion criteria were block randomized by a research assistant to either immediate treatment (IT) or waitlist (WL) using a computer randomization program (the randomization sequence was concealed from investigators until interventions were assigned). Block randomization procedures stratified children based on age and gender; hence, when a child of a particular age and gender was randomized to one of the conditions, the next child with these same characteristics was automatically assigned to the other condition. Therapists were randomly assigned to children's cases. Posttreatment assessments were completed on the final day of treatment or within a week of termination; postwaitlist assessments were conducted three months after the baseline assessment but before initiating CBT. These posttreatment and postwaitlist assessments involved readministering all of the anxiety measures. Treatment was provided in a research setting, with the exception of the two meetings held at the child's school. Families were offered $20 for participating in the two assessments.
Results
Intent-to-treat and treatment-completer sample sizes were 40 and 36, respectively (see Figure 1). Recruitment began in 9/2004 and ended in 8/2007; post-treatment assessments were completed by 12/2007.
Table 1 presents descriptive and diagnostic information for children in the two treatment conditions. Total child DSM-IV diagnoses including ASD, anxiety disorders, and additional comorbid diagnoses ranged from 2 to 6 diagnoses per child, with an average of 4.28 (SD = 1.18).
Pretreatment comparability
Pretreatment group differences were assessed with chi-square tests and t-tests. There were no statistically significant treatment group differences on the demographic and child diagnostic variables presented in Table 1, with one exception (there were 3 cases with comorbid dysthymia or major depression in IT compared to none in WL).
Intervention adherence
To evaluate therapist adherence to the intervention protocol, all therapy sessions were recorded on audiotape. Two sessions from each case were randomly selected and rated by trained undergraduate coders with substantial experience working on this trial, who checked off items listing the required topics for each module as they listened to the tapes. Sample items from the checklists are: `Built hierarchy of child's fears' (yes/no) and `established a list of highly motivating rewards' (yes/no). Results show that study therapists adhered to the required topics for each module at a rate of 94%. Two coders rated a random sample of 10% of the same tapes, and interrater reliability was excellent (for agreement on number of session goals met, ICC = .94).
Treatment outcome
Treatment completer analyses
In terms of the primary study outcome, all but one treatment completer in the IT condition (13 of 14; 92.9%) met CGI criteria for positive treatment response, compared to only 2 of 22 (9.1%) children in the WL condition (χ2 [1] = 24.70, p < .0001). Positive diagnostic status at posttreatment/postwaitlist was defined as a child meeting criteria for any of four anxiety disorder diagnoses (i.e., SAD, social phobia, OCD, or GAD) based on an ADIS-C/P CSR score ≥ 4. In the IT condition, 9 of 14 (64.3%) treatment completers did not meet criteria for any anxiety disorder diagnosis at posttreatment, whereas only 2 of 22 (9.1%) waitlist completers did not meet diagnostic criteria for any anxiety disorder at postwaitlist (χ2 [1] = 12.28, p < .0001).
ANCOVA was used to test group differences at posttreatment/postwaitlist on continuous outcome variables, with the youths' baseline anxiety scores included as a covariate. The independent evaluator's ratings on the ADIS-C/P CSR anxiety severity scale significantly differed by treatment group, F (1,33) = 54.19, p < .0001. Posttreatment/postwaitlist CSR scores were lower in the IT group than in the WL group (ES = 2.46, a large effect; Cohen, 1988) (see Table 2).
Table 2.
Anxiety scores for the immediate treatment (IT) and waitlist (WL) groups
| Baseline |
Posttreatment / Postwaitlist |
|||
|---|---|---|---|---|
| Scale | IT | WL | IT | WL |
| ADIS-CSR | ||||
| M | 5.00 | 5.14 | 2.36 | 4.77 |
| SD | .68 | .56 | 1.15 | .81 |
| Range | 4-6 | 4-6 | 1-4 | 3-6 |
| Parent MASC | ||||
| M | 71.25 | 75.38 | 58.48 | 76.57 |
| SD | 17.07 | 12.98 | 14.72 | 14.65 |
| Range | 36-98 | 56-103 | 40-98 | 56-103 |
| Child MASC | ||||
| M | 56.66 | 54.69 | 46.93 | 46.50 |
| SD | 16.84 | 16.80 | 14.76 | 15.83 |
| Range | 20-77 | 25-85 | 27-72 | 22-79 |
Note. Means are based on all available data for treatment completers; for IT n = 14; for WL n = 22. ADIS-CSR= Anxiety Disorders Interview Schedule-Clinician's Severity Rating; MASC = Multidimensional Anxiety Scale for Children. Raw scores are reported for the parent and child MASC.
For parent-report MASC scores, there was a statistically significant difference between the IT and WL groups at posttreatment/postwaitlist, F (1,32) = 19.50, p < .0001. Parent MASC scores were lower at posttreatment/postwaitlist for children in IT as compared to WL (ES = 1.23, a large effect).
There was not a significant group difference at posttreatment/postwaitlist for the child-report MASC, F (1,33) = .03, p = .87. Children in the IT and WL conditions reported a similar level of anxiety at intake and both improved by approximately the same degree at posttreatment/postwaitlist (ES = .03) (see Table 2).
Intent-to-treat analyses
Intent-to-treat (ITT) analyses were also conducted (N = 40). For the four children who dropped out, baseline scores were carried forward to posttreatment/postwaitlist. All statistically significant group differences from the treatment completer analyses remained significant in the ITT analyses. In the IT condition, 13 of 17 (76.5%) children met CGI criteria for treatment response, whereas 2 of 23 (8.7%) children in the WL condition did so. Furthermore, 9 of 17 (52.9%) IT children were diagnosis-free at posttreatment, as compared to 2 of 23 (8.7%) WL children.
Maintenance of treatment gains at 3-month follow-up
In the IT condition, 10 children returned for a 3-month follow-up assessment. Eight of the 10 (80%) children were diagnosis-free at follow-up. During the follow-up period, 1 treatment responder (10%) relapsed and met criteria for an anxiety disorder; 1 child (10%) who met criteria at posttreatment no longer met diagnostic criteria; and 1 child (10%) maintained a clinically significant anxiety disorder from the posttreatment assessment. For the CGI-I, 9 of the 10 children (90%) maintained their positive response to treatment with a rating of 1, 2, or 3; 1 child (10%) switched from positive response at posttreatment to a rating of 4 (slightly better).
Results from within-subject t-tests, comparing parent-reported MASC scores at posttreatment (M = 54.20, SD = 10.50) and follow-up (M = 53.36, SD = 10.82) indicate that the treatment effect was maintained through the follow-up period, t(9) = .37, p = .72). Additionally, there was no significant difference between posttreatment (M = 45.20, SD = 15.49) and follow-up (M = 48.60, SD = 12.94) child-reported MASC scores, t(9) = −.72, p = .49.
Discussion
These results offer initial support for the efficacy of an enhanced CBT program for children with ASD and comorbid anxiety disorders. Despite the high levels of comorbidity encountered in this sample, children randomized to CBT had primary outcomes comparable to those of typically developing children (without ASD) receiving CBT for anxiety disorders, with large effect sizes for most outcome measures (cf. Barrett et al., 1996; Wood et al., 2006), remission of all anxiety disorders for over half the children in immediate treatment at posttreatment and follow-up, and a high rate of positive treatment response on the CGI (78.5% from intent-to-treat analyses). An exception to this pattern of findings was child-reported anxiety, which did not yield a significant treatment effect. Overall, these results suggest that with appropriate enhancements, CBT may be potent in the treatment of anxiety disorders among children with ASD.
It is notable that CBT yielded substantial anxiety reduction given the numerous potential barriers to success related to ASD such as poor social skills, poor adaptive skills, substantial comorbidity, and circumscribed interests and stereotypies. Participating children had an average of 4.18 psychiatric disorders (including ASD). In comparison, typically developing children with anxiety disorders in a recent clinical trial of CBT had an average of 1.88 total diagnoses (Wood et al., 2006). The extent of psychopathology represented by this level of comorbidity can be daunting. The CBT protocol enhancements and modification appeared helpful in overcoming these challenges. For example, with appropriate training, parents and teachers were able to implement behavior management strategies to address disruptive and repetitive behaviors and provide cues for the use of social and adaptive skills in daily situations during the skill acquisition phase of treatment, which may have helped with anxiety reduction and skill generalization (e.g., Reaven & Hepburn, 2006). The important role played by parents and teachers suggests that moving beyond a traditional definition of the client as just the child and the treatment setting as just the outpatient therapy office is helpful for interventions in ASD. The positive results that were attained in spite of children's complex clinical presentations also likely reflect the value of maintaining focused goals – in this case, reducing anxiety and accommodating a handful of ASD-related barriers such as poor social skills – and not attempting to resolve all problems simultaneously.
Several limitations bear mentioning. Child-report MASC scores did not yield a significant effect for treatment group, in large part because there was a decrease in MASC scores from pre to post for children in both groups. It is possible that children with ASD use self-report anxiety measures in a unique way. The MASC has not been studied extensively in this population and children's MASC scores at baseline were relatively low on average, certainly lower than expected given the multiple anxiety disorders they met criteria for. Given the cognitive differences associated with ASD (e.g., poor emotion understanding, concreteness of thought), it is possible that traditional anxiety self-report measures like the MASC do not function well with this population, particularly as a measure of change. As a point of comparison, parent-report MASC scores barely declined from pre to post for the WL group. There was also substantial heterogeneity in anxiety problems in the sample, ranging from separation anxiety to social anxiety to OCD to GAD, to a mixture of some of each. The MASC does not measure OCD and GAD symptoms, and hence cannot assess the type of changes some of the children may have experienced. Alternative measurement approaches in the future might involve more comprehensive self-report measures better suited to this heterogeneity or a more flexible assessment approach that can help children express what they mean, such as the Child Anxiety Rating Scale or Berkeley Puppet Interview. However, there is also the possibility that the MASC did provide a good measure of children's perceptions of their symptoms and that these perceptions are simply discrepant from parental perceptions. A second limitation of the study is the relatively low sample size, precluding tests of moderation. Third, this study was conducted by the developers of the intervention and independent replications will be an important future step in the validation of the manual. Also, we did not collect measures of children's and family's adherence to the intervention, precluding definitive conclusions about the processes through which the treatment exerted its effects.
This is one of the first ASD-oriented adaptations of an evidence-based treatment previously used with typically developing youth to be tested in a randomized, controlled trial incorporating the methodological elements suggested by recent task forces promoting high-quality clinical trials, such as the use of independent evaluators and tests of treatment fidelity (e.g., Chambless & Hollon, 1998). Remission of anxiety disorders appears to be an achievable goal among high-functioning children with ASD if a thoughtful approach is taken.
Acknowledgements
This study was supported by grants awarded to Jeffrey J. Wood from the Cure Autism Now Foundation and the National Institute of Mental Health (MH075806). We are very grateful to the participating families.
Trial Registry Information: Clinicaltrials.gov database reference number: NCT00280670. Internet link: http://clinicaltrials.gov/ct2/show/NCT00280670.
Appendix
CONSORT Statement 2001 – Checklist
|
PAPER SECTION and topic |
Item | Descriptor | Reported on Page # |
|---|---|---|---|
| TITLE & ABSTRACT | 1 | How participants were allocated to interventions (e.g., `random allocation', `randomized', or `randomly assigned'). |
1, 2 |
|
INTRODUCTION Background |
2 | Scientific background and explanation of rationale. |
3–8 |
|
METHODS Participants |
3 | Eligibility criteria for participants and the settings and locations where the data were collected. |
8–9 |
| Interventions | 4 | Precise details of the interventions intended for each group and how and when they were actually administered. |
9–12 |
| Objectives | 5 | Specific objectives and hypotheses. | 8 |
| Outcomes | 6 | Clearly defined primary and secondary outcome measures and, when applicable, any methods used to enhance the quality of measurements (e.g., multiple observations, training of assessors). |
12–14 |
| Sample size | 7 | How sample size was determined and, when applicable, explanation of any interim analyses and stopping rules. |
8 |
| Randomization – Sequence generation |
8 | Method used to generate the random allocation sequence, including details of any restrictions (e.g., blocking, stratification) |
15 |
| Randomization – Allocation concealment |
9 | Method used to implement the random allocation sequence (e.g., numbered containers or central telephone), clarifying whether the sequence was concealed until interventions were assigned. |
15 |
| Randomization – Implementation |
10 | Who generated the allocation sequence, who enrolled participants, and who assigned participants to their groups. |
15 |
| Blinding (masking) | 11 | Whether or not participants, those administering the interventions, and those assessing the outcomes were blinded to group assignment. If done, how the success of blinding was evaluated. |
12–15 |
| Statistical methods | 12 | Statistical methods used to compare groups for primary outcome (s); Methods for additional analyses, such as subgroup analyses and adjusted analyses. |
16–18 |
| RESULTS Participant flow |
13 | Flow of participants through each stage (a diagram is strongly recommended). Specifically, for each group report the numbers of participants randomly assigned, receiving intended treatment, completing the study protocol, and analyzed for the primary outcome. Describe protocol deviations from study as planned, together with reasons. |
8, 15, Figure 1 |
| Recruitment | 14 | Dates defining the periods of recruitment and follow-up. |
15 |
| Baseline data | 15 | Baseline demographic and clinical characteristics of each group. |
9, 16, Table 1 |
| Numbers analyzed | 16 | Number of participants (denominator) in each group included in each analysis and whether the analysis was by `intention-to-treat'. State the results in absolute numbers when feasible (e.g., 10/20, not 50%). |
8, 15, Figure 1 |
| Outcomes and estimation |
17 | For each primary and secondary outcome, a summary of results for each group, and the estimated effect size and its precision (e.g., 95% confidence interval). |
16–18, Table 1, Table 2 |
| Ancillary analyses | 18 | Address multiplicity by reporting any other analyses performed, including subgroup analyses and adjusted analyses, indicating those pre-specified and those exploratory. |
N/A |
| Adverse events | 19 | All important adverse events or side effects in each intervention group. |
N/A |
|
DISCUSSION Interpretation |
20 | Interpretation of the results, taking into account study hypotheses, sources of potential bias or imprecision and the dangers associated with multiplicity of analyses and outcomes. |
18–21 |
| Generalizability | 21 | Generalizability (external validity) of the trial findings. |
19–20 |
| Overall evidence | 22 | General interpretation of the results in the context of current evidence. |
19, 21 |
Footnotes
Conflict of interest statement: No conflicts declared.
Copyright of Journal of Child Psychology & Psychiatry is the property of Blackwcll Publishing Limited and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
Children with primary OCD have sometimes been excluded from clinical trials of CBT for children with anxiety disorders, whereas children with primary GAD have been included (e.g. Barrett et al., 1996). However, during the pilot testing of this intervention, we found that (1) OCD was common and (2) children with OCD responded well to the treatment. However, we also noted that children with a sole diagnosis of GAD (and no other anxiety disorder) did not fare as well as expected and seemed to differ in treatment motivation and application of the coping skills. Therefore, we included children with OCD and excluded children with only a diagnosis of GAD.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th edn. American Psychiatric Association; Washington, DC: 2000. Text Revision (DSM-IV-TR) [Google Scholar]
- Attwood T. Understanding and managing circumscribed interests. In: Prior M, editor. Learning and behavior problems in Asperger syndrome. Guilford Press; New York: 2003. pp. 126–147. [Google Scholar]
- Attwood T. Cognitive behaviour therapy for children and adults with Asperger's syndrome. Behaviour Change. 2004;21:147–161. [Google Scholar]
- Baker MJ, Koegel RL, Koegel LK. Increasing the social behavior of young children with autism using their obsessive behaviors. Journal of the Association for Persons with Severe Handicaps. 1998;23:300–308. [Google Scholar]
- Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology. 1996;64:333–342. doi: 10.1037//0022-006x.64.2.333. [DOI] [PubMed] [Google Scholar]
- Bellini S. Social skill deficits and anxiety in high-functioning adolescents with autism spectrum disorder. Focus on Autism and Other Developmental Disabilities. 2004;19:78–86. [Google Scholar]
- Centers for Disease Control and Prevention Prevalence of autism spectrum disorders – autism and developmental disabilities monitoring network, 14 sites, United States, 2002. Report prepared by the US government, ID: 56(SS01) 2007:12–28. [PubMed]
- Chalfant A, Rapee R, Carroll L. Treating anxiety disorders in children with high-functioning autism spectrum disorders: A controlled trial. Journal of Autism and Developmental Disorders. 2006;33:283–298. doi: 10.1007/s10803-006-0318-4. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Hollon SD. Defining empirically supported therapies. Journal of Consulting and Clinical Psychology. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Taylor AA, Francis SE, Moffitt C, Austin AA. Efficacy of modular cognitive behavior therapy for childhood anxiety disorders. Behavior Therapy. 2004;35:263–287. [Google Scholar]
- Cohen J. Set correlation and contingency tables. Applied Psychological Measurement. 1988;12:425–434. [Google Scholar]
- de Bruin EI, Ferdinand RF, Meesters S, de Nijs PFA, Verheij F. High rates of psychiatric co-morbidity in PDD-NOS. Journal for Autism and Developmental Disorders. 2007;37:877–886. doi: 10.1007/s10803-006-0215-x. [DOI] [PubMed] [Google Scholar]
- Fombonne E. Epidemiological surveys of autism and other pervasive developmental disorders: An update. Journal of Autism and Developmental Disorders. 2003;33:365–382. doi: 10.1023/a:1025054610557. [DOI] [PubMed] [Google Scholar]
- Frankel F, Myatt R. Children's friendship training. Brunner-Routledge; New York: 2003. [Google Scholar]
- Fulk BM, King K. Classwide peer tutoring at work. Teaching Exceptional Children. 2001;34:49–53. [Google Scholar]
- Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. Journal of Child Psychology and Psychiatry. 2004;45:212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- Hwang MB, Hughes C. The effects of social interactive training on early social communicative skills of children with autism. Journal of Autism and Developmental Disorders. 2000;30:331–343. doi: 10.1023/a:1005579317085. [DOI] [PubMed] [Google Scholar]
- Kasari C, Chamberlain B, Bauminger N. Social emotions and social relationships: Can children with autism compensate? In: Burack JA, Charman T, Yirmiya N, Zelazo PR, editors. The development of autism: Perspectives from theory to research. Erlbaum; Mahwah, NJ: 2001. pp. 309–323. [Google Scholar]
- King-Sears ME. Institutionalizing peer-mediated instruction and intervention in schools: Beyond `train and hope'. Remedial and Special Education. 2001;22:89–101. [Google Scholar]
- Klin A, Pauls R, Schultz R, Volkmar F. Three diagnostic approaches to Asperger syndrome: Implications for research. Journal of Autism and Developmental Disorders. 2005;35:221–234. doi: 10.1007/s10803-004-2001-y. [DOI] [PubMed] [Google Scholar]
- Klin A, Saulnier C, Sparrow S, Cicchetti D, Volkmar F, Lord C. Social and communication abilities and disabilities in higher functioning individuals with autism spectrum disorders: The Vineland and the ADOS. Journal of Autism and Developmental Disorders. 2007;37:748–759. doi: 10.1007/s10803-006-0229-4. [DOI] [PubMed] [Google Scholar]
- Koegel RL, Werner GA, Vismara LA, Koegel LK. The effectiveness of contextually supported play date interactions between children with autism and typically developing peers. Research and Practice for Persons with Severe Disabilities. 2005;30:93–102. [Google Scholar]
- Le Couteur A, Lord C, Rutter M. The Autism Diagnostic Interview-Revised. Western Psychological Services; Los Angeles: 2003. [Google Scholar]
- Leyfer OT, Folstein SE, Bacalman S, David NO, Dinh E, Morgan J, Tager-Flusberg H, Lainhart JE. Comorbid psychiatric disorders in children with autism: Interview development and rates of disorders. Journal of Autism and Developmental Disorders. 2006;36:849–861. doi: 10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule. Western Psychological Services; Los Angeles: 2002. [Google Scholar]
- Maheady L, Harper GF, Mallette B. Peer-mediated instruction and interventions and students with mild disabilities. Remedial and Special Education. 2001;22:4–14. [Google Scholar]
- March JS. Multidimensional anxiety scale for children. Multi-Health Systems; North Tonawanda, NY: 1998. [Google Scholar]
- March JS, Parker JDA, Sullivan K, Stallings P, Conners K. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Matson JL, Nebel-Schwalm MS. Comorbid psychopathology with autism spectrum disorder in children: An overview. Research in Developmental Disabilities. 2007;28:341–352. doi: 10.1016/j.ridd.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Mills R, Wing L. Researching interventions in ASD and priorities for research: Surveying the membership of the NAS. National Autistic Society; London: 2005. [Google Scholar]
- Mundy PC, Henderson HA, Inge AP, Coman DC. The modifier model of autism and social development in higher functioning children. Research and Practice for Persons with Severe Disabilities. 2007;32:1–16. doi: 10.2511/rpsd.32.2.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Steerneman P, Merckelbach H, Holdrinet I, Meesters C. Comorbid anxiety symptoms in children with pervasive developmental disorders. Journal of Anxiety Disorders. 1998;12:387–393. doi: 10.1016/s0887-6185(98)00022-x. [DOI] [PubMed] [Google Scholar]
- Reaven J, Hepburn S. Cognitive-behavioral treatment of obsessive-compulsive disorder in a child with Asperger syndrome. Autism. 2003;7:145–164. doi: 10.1177/1362361303007002003. [DOI] [PubMed] [Google Scholar]
- Reaven J, Hepburn S. The parent's role in the treatment of anxiety symptoms in children with high-functioning autism spectrum disorders. Mental Health Aspects of Developmental Disabilities. 2006;9:73–80. [Google Scholar]
- Rogers SJ. Interventions that facilitate socialization in children with autism. Journal of Autism and Developmental Disorders. 2000;30:399–409. doi: 10.1023/a:1005543321840. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV-Child and Parent Versions. Graywind; San Antonio, TX: 1996. [Google Scholar]
- Sofronoff K, Attwood T, Hinton S. A randomized controlled trial of a CBT intervention for anxiety in children with Asperger syndrome. Journal of Child Psychology and Psychiatry. 2005;46:1152–1160. doi: 10.1111/j.1469-7610.2005.00411.x. [DOI] [PubMed] [Google Scholar]
- Sze KM, Wood JJ. Cognitive behavioral treatment of comorbid anxiety disorders and social difficulties in children with high-functioning autism: A case report. Journal of Contemporary Psychotherapy. 2007;37:133–143. [Google Scholar]
- Volkmar FR, Klin A. Diagnostic issues in Asperger syndrome. In: Klin A, Volkmar FR, Sparrow SS, editors. Asperger syndrome. Guilford Press; New York: 2000. pp. 25–71. [Google Scholar]
- Wood JJ, McLeod B. Child anxiety disorders: A treatment manual for practitioners. Norton; New York: 2008. [Google Scholar]
- Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of Clinical Child and Adolescent Psychology. 2002;31:335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Piacentini JC, Southam-Gerow M, Chu BC, Sigman M. Family Cognitive Behavioral Therapy for child anxiety disorders. Journal of American Academy of Child and Adolescent Psychiatry. 2006;45:314–321. doi: 10.1097/01.chi.0000196425.88341.b0. [DOI] [PubMed] [Google Scholar]