Abstract
Context:
Thoracic trauma causes significant morbidity; however, many deaths are preventable and few patients require surgery. Intercostal chest drainage (ICD) for hemo/pneumothorax is simple and effective; the main problem is residual hemothorax, which can cause lung collapse and empyema.
Aims:
Our study aimed to analyze the relationship between radiological chest tube parameters (position and intrathoracic length) and the frequency of residual hemothorax.
Settings and Design:
This prospective analytical study was conducted in a large tertiary care hospital in north India over 2 years till March 2013.
Materials and Methods:
Patients of chest trauma aged 18-60 years, with hemothorax or hemopneumothorax requiring ICD insertion were included in the study. Bedside ICD insertion was performed as per current standards. Immediate post-ICD chest radiographs were used to record lung status and ICD position (chest tube zone and intrapleural length). Residual hemothorax was defined as any collection identified on radiological investigations after 48 hours of ICD placement.
Statistical Analysis:
Univariate analysis was performed with the chi-square test or Student's t-test as appropriate, while multivariate analysis using stepwise logistic regression; a P-value < 0.05 was significant.
Results:
Out of 170 patients of chest trauma, 154 underwent ICD insertion. Most patients were young (mean age: 31.7 ± 12 years) males (M:F = 14:1). Ninety-seven patients (57.1%) had isolated chest injuries. Blunt trauma (n = 119; 77.3%) and motor vehicle accidents (n = 72; 46.7%) were the commonest causes. Mean hospital stay was 9 ± 3.94 days, and mortality 2/154 (1.1%). Residual hemothorax was seen in 48 (31%). No ICD zone or length was significantly associated with residual hemothorax on univariate or multivariate analysis.
Conclusion:
Intrapleural ICD zone or length does not affect the frequency of residual hemothorax.
Keywords: Chest trauma, intrapleural chest tube parameters, residual hemothorax
INTRODUCTION
Trauma is now a leading cause of death worldwide, especially motor vehicle crashes. More than 90% of motor vehicle crashes occur in the developing world.[1] In India, 1.2 million people die in road accidents and about five million are disabled annually. A vast majority of those killed and injured are pedestrians, motorcyclists and pillions riders, and bicyclists. Trauma is also caused by falls, firearm injuries, burns, assault, falling objects, and natural and man-made disasters.[2,3]
Thoracic trauma is a significant cause of morbidity and mortality. Conditions like rib fractures, hemopneumothorax, and lung contusion can lead to significant patient distress; however, many in-hospital deaths due to thoracic trauma are preventable. Less than 10% of blunt and only 15-30% of penetrating chest injuries require operative intervention.[4] An initial chest radiograph is useful to detect hemothorax or hemopneumothorax after trauma. Approximately 300-400 mL of blood is required for the costo-phrenic angle to be obliterated on an erect chest radiograph. The majority of hemothoraces cease spontaneously, and require only simple drainage with intercostal chest drains (ICDs).[5] Till the 1980s, it was believed that the optimum position of chest tubes was posteriorly for hemothorax and anteriorly for pneumothorax.[6,7,8] Often, two chest tubes were inserted simultaneously for these roles. Advanced Trauma Life Support (ATLS) guidelines recommend one chest tube in trauma victims, directed posteriorly and straight.[6] If the ICD retains its function, it is usually not re-positioned.[6,7,8] However, there are no guidelines regarding the direction and intrapleural length of ICD, which maximizes the drainage.
Intrapleural collections identified after an optimal period (48-72 hours) of intercostal drainage after trauma are known as residual or retained hemothorax.[9,10] The incidence of residual hemothorax has been variably reported from 5% to 30%.[9,10,11,12,13] The exact incidence has not been studied in the Indian population. Residual hemothorax is difficult to evacuate due to the onset of fibrosis. Loss of lung volume accompanied by stasis predisposes to empyema.[9,12,13] Factors predisposing to residual hemothorax are clotted hemothorax or tube-related factors viz., small caliber, incorrect placement, or a kinked tube.[14] It has been shown that chest tube diameter has little effect on the effectiveness of drainage.[15] However, the relationship between ICD parameters (position and intrathoracic length) and the frequency of residual collection has not been studied.
Our study was designed to establish the frequency of residual hemothorax in our patients, and to analyze the relationship between radiological chest tube parameters (position and intrathoracic length) and the frequency of residual hemothorax.
MATERIALS AND METHODS
This was a prospective analytical study conducted in the departments of surgery, emergency and radiodiagnosis of a teaching institute in north India from November 2011 till March 2013. Our institute is a 1500-bedded tertiary care hospital, which caters to a number of trauma patients. All patients of chest trauma between 18-60 years of age, admitted with hemothorax or hemopneumothorax requiring ICD insertion, were included in the study. Patients who died (or left hospital for any reason) before 48 hours of admission, denied consent for participation in the study, or reported after 8 hours of chest trauma were excluded.
Flow of the study
Chest trauma patients with hemothorax or hemopneumothorax underwent ICD insertion under local anesthesia at the bedside as per Advanced Trauma Life Support guidelines.[6] The ICD insertion site was marked on the fifth inter-costal space, just anterior to the mid-axillary line. After cleaning and draping the area, 2% lignocaine was infiltrated into the skin and periosteum. A transverse incision 2-3 cm in length was made, and the subcutaneous tissues were dissected bluntly. The parietal pleura was punctured with the tip of a curved artery forceps and a gloved finger inserted to safely clear adhesions and clots. The proximal end of the thoracostomy tube (28-32 Fr depending on the width of the space) was clamped with the hemostat and advanced into the pleural space to the desired length. The tube was directed posteriorly along the inside of chest wall. Intra-pleural position was confirmed by noting the fogging in the ICD with expiration or swinging of the water column after connection to an underwater seal apparatus. The tube was secured with a purse-string silk suture, and an occlusive dressing was applied.
A chest radiograph obtained immediately after ICD insertion was used to record lung expansion status and ICD position (chest tube zone and intra-pleural length; Figures 1 and 2). The output of the ICD was monitored daily. Radiological investigations viz. a repeat chest radiograph, ultrasonography or CT scan of the chest (where feasible) were performed 48 hours after ICD placement. Fully expanded lungs with no evidence of residual collection on imaging were deemed as markers of successful ICD placement. Residual hemothorax, for the purpose of our study, was defined as any collection identified on radiological investigations (chest radiograph, ultrasound chest or CT chest) after 48 hours of ICD placement.
Figure 1.
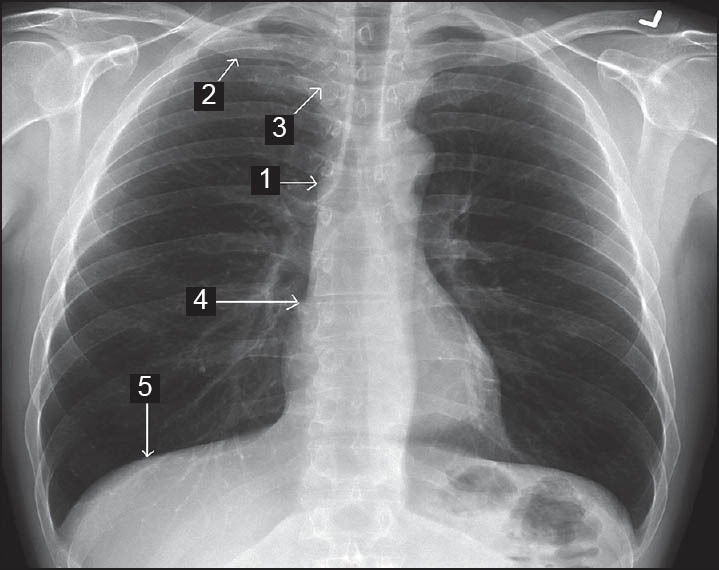
Chest tube zone classification (Zone 1: ICD lying flush with inside of rib cage; Zone 2: ICD pointing towards middle of clavicle; Zone 3: ICD pointing towards middle of mediastinum; Zone 4: ICD pointing towards middle of right/left cardiac border; and, Zone 5: ICD pointing towards the diaphragm)
Figure 2.
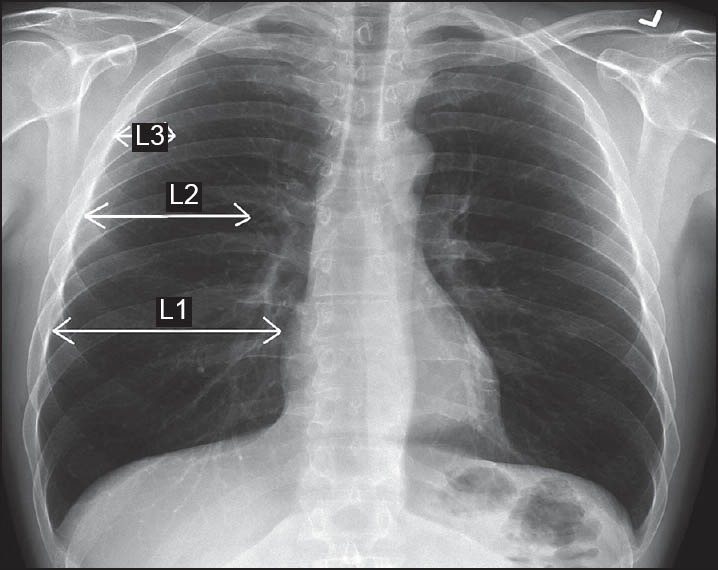
Classification of intra-pleural length of chest tube (L1: Reaching fully across the zone; L2: > 50% but not reaching fully across the zone; L3: < 50% across the zone)
ICDs were retained in patients with residual collection at 48 hours. These patients were evaluated for the presence of clotted/loculated hemothorax, lung entrapment, and lung collapse. The ICD was removed if the output was less than 100 mL/day. Patients with no residual hemothorax but significant (≥100 mL/day) ICD output or with persistent surgical emphysema had the ICDs retained. These patients were evaluated clinically and radiologically for 48 hours before considering tube removal. Patients with no residual collection were discharged and followed up after a week.
The primary outcome measures were frequency of residual hemothorax, patterns of chest tube position and intrapleural lengths, and the effect of these tube parameters on residual hemothorax.
Statistical analysis
The relationship of the different chest tube zones, different intrapleural lengths, and presence of diaphragmatic injury on one side, with the occurrence of residual hemothorax on the other, was studied using univariate analysis with the chi-square test or the Student's t-test (for qualitative and quantitative data respectively). Keeping one variable independent with others as dependant variables, multivariate analysis was performed using stepwise logistic regression. Statistical significance was considered at P-value <0.05.
RESULTS
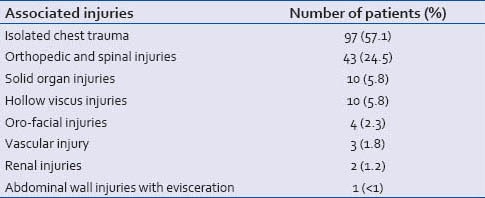
One hundred and seventy cases of chest trauma requiring inter-costal drainage were recruited for our study. After excluding 16 patients using our exclusion criteria [Table 1], 154 patients had ICD insertion on clinical or radiological grounds. The majority of patients had isolated chest injuries. Table 2 enlists the associated injuries in 154 patients.
Table 1.
Patients excluded (16/170) from the study
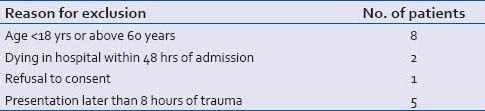
Table 2.
Associated injuries in 154 patients of chest trauma
Demographic data
The mean age of the patients was 31.7 ± 12 years. About 50% patients were less than 30 years of age. Cases of chest trauma requiring ICD insertion were predominantly males (n = 144; 93.5%); the male:female ratio was 14:1.
Mechanisms of chest trauma
Blunt trauma was the predominant mechanism of chest trauma (n = 119; 77.3%); motor vehicle accidents (n = 72; 46.7%) were the commonest cause, followed by falls (26; 17.1%), train accidents (2; 1.3%), assault (11; 7.2%), and animal injuries (7; 4.6%). Penetrating trauma affected 35 patients (22.7%); stab injury due to assault was the predominant cause (n = 33, 94.3%) while 2 patients had gunshot injuries.
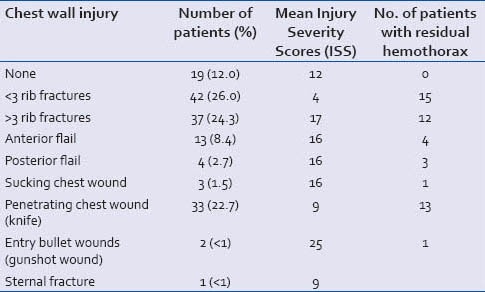
The majority of our patients (n = 107; 70%;) reached the hospital within 4 hours of trauma. The type and extent of injury to the chest wall was noted [Table 3]. Injury Severity Scores are also mentioned. The right hemithorax was affected in 81 (52.6%) cases, left in 73 (47.4%), and 24 cases (31%) were bilateral.
Table 3.
Types of chest wall injuries
Ninety patients (58.4%) had hemopneumothorax while 64 patients (41.6%) had hemothorax alone. In 2 patients, we performed exploratory thoracotomy and found cardiac tamponade in 1, and traumatic rupture of the right main-stem bronchus in the other; intraoperative pericardiocentesis and primary bronchial repair were done respectively. Post-operative recovery was uneventful. Ten patients (6.5%) had traumatic diaphragmatic injury with resultant diaphragmatic hernia. Operative intervention and primary repair was performed in all.
In 95 patients (62%), we inserted the ICD on clinical grounds, whereas in 41 patients (27.4%), it was inserted ICD on radiological grounds. Eleven patients needed combined criteria for ICD insertion. Intraoperative insertion was performed in 7 patients.
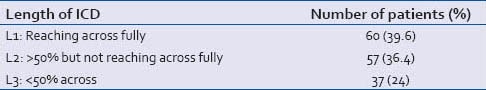
One hundred and eleven patients (72%) had complete lung expansion following ICD insertion, as evident in the immediate post-ICD chest radiographs. The mean hospital stay was 9 ± 3.94 days, and the mortality rate was 2/154 (1.1%). Tables 4 and 5 show the number of ICDs placed in the respective zones and intrapleural lengths (vide supra). The duration of drainage was less than 3 days in 54 (35%) cases; in 15 (9.8%), it exceeded 5 days.
Table 4.
Distribution of ICDs according to zones
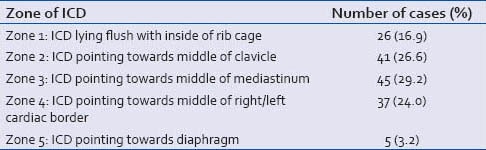
Table 5.
Distribution of ICDs at different intrapleural lengths
Residual hemothorax
Radiological investigations (chest radiograph and/or ultrasound chest and/or CECT chest, wherever feasible or indicated) were performed after 48 hours of ICD insertion to identify residual hemothorax. Chest radiographs were done in 148 (96%) patients; 47 (30.7%) were diagnosed with residual hemothorax. These were confirmed using ultrasound of the thorax in 26 patients. Ultrasound of the thorax after 48 hours was done in 57 (37%) patients; a residual collection was identified in 29 (50.8%) patients. In one case, ultrasound detected a residual collection when the chest radiograph was normal. CECT chest was done in 27 cases (17.5%); it showed residual hemothorax in 15 patients (55.6%).
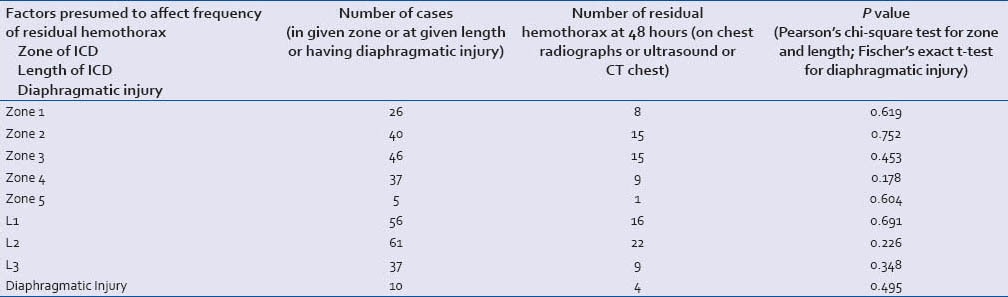
A total of 48 (31%) patients had identifiable residual hemothorax. Hence, primary ICD insertion was successful in 106 (71%) patients. Table 6 depicts the effect of the ICD parameters under study and diaphragmatic injury on residual hemothorax. No single factor was significantly associated with the presence of residual hemothorax; this was also evident on multivariate analysis.
Table 6.
Univariate analysis to study effect of a particular ICD zone or length or diaphragmatic injury on residual hemothorax
DISCUSSION
This study was designed to improve our understanding of demographics and management of thoracic trauma in our set-up. The clinical unit involved in the study has been dedicated to trauma care for many years. The growing number of automobiles with concurrent RTIs and thoracic trauma prompted us to review our practices and protocols. We felt that tube thoracostomy, despite the frequency of its usage, was not being utilized optimally in the current scenario. Thus, this procedure was the focus of our approach.
Blunt thoracic trauma is directly responsible for 20-25% of all trauma-related deaths and a major contributor in another 50%.[1] The vast majority of patients can be successfully managed with bedside thoracostomy or intensive care. The causes of preventable deaths are diaphragmatic injuries, cardiac tamponade, contained vascular injuries of the mediastinum and tracheo-bronchial injuries. These constitute less than 10% of cases and need definitive/operative intervention.[2,3,6]
Our hospital caters to a unique socio-geographical area. It is one of the three largest hospitals of the capital city region, catering to a population of more than 500,000. Being close to the highway at the periphery of the urban area, we receive a robust mix of high-velocity motor vehicle crashes, assault victims, and animal injuries. Despite the hurdles, our data shows that most patients are brought to the hospital within a few hours or the ‘golden period.’ An earlier study from our institute had noted a delay in presentation due to poor rural connectivity.[16] Other demographic variables are similar to data from similar settings.[16,17,18] The most affected people are males in the age group of 25-40 years, i.e., the most productive period. Road traffic injuries, penetrating injuries, and falls have been documented to be the leading causes of trauma in most urban-rural areas. Animal injuries encountered in our hospitals seem to be a unique phenomenon and probably reflects haphazard urbanization and the continued use of animals for transport and agriculture.[16] Chest injury patterns viz. the proportion of rib fractures and flail chest in our patients were also similar to other studies from India. All diaphragmatic rents were localized to left side, highlighting the protective role of the liver on the right.[16,19]
In our hospital, chest trauma victims are frequently received after suboptimal initial management (pre-hospital or at lower centers). We also have a high rate of residual hemothorax compared to western figures.[9,10,11,12,13] No study from India has been carried out in this regard. Poor training in thoracostomy techniques is recognized as a significant cause of procedure-related complications and residual hemothorax. Proper insertion of the ICD by trained surgical residents leads to a better outcome.[20,21] In our hospital, the initial ICD insertion is performed by a surgical resident. We felt that a detailed evaluation of our own technique of ICD insertion was essential to identify the offending causes of residual hemothorax. It was often noted that an apparently blocked or non-draining chest tube became functional after manipulation, particularly withdrawal. We thus explored a possible correlation between residual hemothorax and intrapleural chest tube parameters. Our results have not shown a significant relationship in this regard. A confounding factor like diaphragmatic injury or injury severity is known to affect the rate of residual hemothorax.[22] Most of our patients with severe injuries (10 patients) had diaphragmatic injuries. These were carefully excluded from our analysis. Severe injuries were associated more with residual hemothorax but not significantly due to lower numbers [Table 3]. The relationship between mean Injury Severity Scores and residual hemothorax was not established; the ISS is a ‘perceived-threat-to-life’ score and not a comprehensive measure of severity.[5,22] As mentioned, we felt that diaphragmatic injuries could independently cause residual hemothorax; these were analyzed statistically. The mean Injury Severity Scores and the number of residual hemothoraces with different injuries are mentioned in Table 3. Though our results do not demonstrate a relationship between radiological chest tube parameters (position and intrathoracic length) and the frequency of residual hemothorax, we hope that continued research in this area will improve the quality of our trauma care.
The concept of optimal ICD caliber, long thought to be relevant in functioning of the tube, has recently been challenged. Inaba et al. compared small bore chest tubes (28-32 Fr) with large bore tubes (36-40 Fr) in traumatic hemothoraces in terms of volume of blood drained initially, total duration of tube placement, tube-related complications, and need for tube reinsertion. They found that the chest tube size did not impact any of the outcomes. Further, tube size did not affect the pain felt by the patients.[15]
Hence, it appears that as long as trained personnel insert intercostals drains using the existing guidelines,[6,7,8] the incidence of RH is not increased.[20,21] A few limitations are notable in our study. The availability of ultrasound and CT scan was not uniform for all our patients; this could impact the detection of RH. Another inconsistency was the variable time of ICD removal; most tubes were removed later than advocated in our protocol. Thus, more data and a stricter adherence to protocol are necessary.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gururaj G. Road traffic deaths, injuries and disabilities in India: Current scenario. Natl Med J India. 2008;21:14–20. [PubMed] [Google Scholar]
- 3.Gupta A, Gupta E. Challenges in organizing trauma care systems in India. Indian J Community Med. 2009;34:75–6. doi: 10.4103/0970-0218.45383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simon B, Ebert J, Bokhari F, Capella J, Emhoff T, Hayward T, 3rd, et al. Eastern Association for the Surgery of Trauma. Management of pulmonary contusion and flail chest: An Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73:S351–61. doi: 10.1097/TA.0b013e31827019fd. [DOI] [PubMed] [Google Scholar]
- 5.London: Trauma.org; 2004. [Last cited on 2013 Jul 30]. Chest trauma: Hemothorax [Internet] p. 2. Available from: http://www.trauma.org/archive/thoracic/CHESThaemo.html . [Google Scholar]
- 6.American College of Surgeons, Committee on Trauma. American College of Surgeons, Committee on Trauma, editors. Advanced Trauma Life Support for Doctors: ATLS Student Course Manual. 8th ed. Chicago: American College of Surgeons; 2009. Thoracic Trauma; pp. 85–109. [Google Scholar]
- 7.Toronto: Professional Practice Advisor; 2009. [Last cited on 2013 Jul 30]. College of Respiratory Therapists of Ontario. Chest needle and chest tube insertion: Clinical best practice guideline [Internet] p. 44. Available from: http://www.crto.on.ca/pdf/ppg/chest_tube_cbpg.pdf . [Google Scholar]
- 8.Hendra TJ. STHFT protocol for chest drain insertion in adults [Internet] Sheffield: Sheffield Teaching Hospitals, NHS Foundation Trust. 2005. [Last cited on 2013 Jul 30]. p. 12. Available from: http://thoracic.group.shef.ac.uk/information/files/sthft-chest-drain.pdf .
- 9.Oğuzkaya F, Akçali Y, Bilgin M. Videothoracoscopy versus intrapleural streptokinase for management of post traumatic retained haemothorax: A retrospective study of 65 cases. Injury. 2005;36:526–9. doi: 10.1016/j.injury.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 10.Heniford BT, Carrillo EH, Spain DA, Sosa JL, Fulton RL, Richardson JD. The role of thoracoscopy in the management of retained thoracic collections after trauma. Ann Thorac Surg. 1997;63:940–3. doi: 10.1016/s0003-4975(97)00173-2. [DOI] [PubMed] [Google Scholar]
- 11.Agarwal R, Aggarwal AN, Gupta D. Intrapleural fibrinolysis in clotted haemothorax. Singapore Med J. 2006;47:984–6. [PubMed] [Google Scholar]
- 12.Bradley M, Okoye O, Dubose J, Inaba K, Demetriades D, Scalea T, et al. Risk factors for post-traumatic pneumonia in patients with retained haemothorax: Results of a prospective, observational AAST study. Injury. 2013;44:1159–64. doi: 10.1016/j.injury.2013.01.032. [DOI] [PubMed] [Google Scholar]
- 13.Karmy-Jones R, Holevar M, Sullivan RJ, Fleisig A, Jurkovich GJ. Residual hemothorax after chest tube placement correlates with increased risk of empyema following traumatic injury. Can Respir J. 2008;15:255–8. doi: 10.1155/2008/918951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meyer DM, Jessen ME, Wait MA, Estrera AS. Early evacuation of traumatic retained hemothoraces using thoracoscopy: A prospective, randomized trial. Ann Thorac Surg. 1997;64:1396–400. doi: 10.1016/S0003-4975(97)00899-0. [DOI] [PubMed] [Google Scholar]
- 15.Inaba K, Lustenberger T, Recinos G, Georgiou C, Velmahos GC, Brown C, et al. Does size matter? A prospective analysis of 28-32 versus 36-40 French chest tube size in trauma. J Trauma Acute Care Surg. 2012;72:422–7. doi: 10.1097/TA.0b013e3182452444. [DOI] [PubMed] [Google Scholar]
- 16.Mohta M, Kumar P, Mohta A, Bhardwaj R, Tyagi A, Sethi AK. Experiences with chest trauma: Where do we stand today. Indian J Crit Care Med. 2006;10:25–8. [Google Scholar]
- 17.Mishra B, Sinha Mishra ND, Sukhla S, Sinha A. Epidemiological study of road traffic accident cases from Western Nepal. Indian J Community Med. 2010;35:115–21. doi: 10.4103/0970-0218.62568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olawale OA, Owoaje ET. Incidence and pattern of injuries among residents of a rural area in South-Western Nigeria: A community-based study. BMC Public Health. 2007;7:246. doi: 10.1186/1471-2458-7-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dalal S, Nityasha, Vashisht MG, Dahiya RS. Prevalence of Chest Trauma at an Apex Institute of North India: A retrospective study. Internet J Surg. 2009:18. DOI: 10.5580/824. [Google Scholar]
- 20.Etoch SW, Bar-Natan MF, Miller FB, Richardson JD. Tube thoracostomy. Factors related to complications. Arch Surg. 1995;130:521–5. doi: 10.1001/archsurg.1995.01430050071012. [DOI] [PubMed] [Google Scholar]
- 21.Deneuville M. Morbidity of percutaneous tube thoracostomy in trauma patients. Eur J Cardiothorac Surg. 2002;22:673–8. doi: 10.1016/s1010-7940(02)00478-5. [DOI] [PubMed] [Google Scholar]
- 22.DuBose J, Inaba K, Demetriades D, Scalea TM, O’Connor J, Menaker J, et al. AAST Retained Hemothorax Study Group. Management of post-traumatic retained hemothorax: A prospective, observational, multicenter AAST study. J Trauma Acute Care Surg. 2012;72:11–22. doi: 10.1097/TA.0b013e318242e368. [DOI] [PubMed] [Google Scholar]


