Abstract
Background:
The aim of this study is to clarify the circumstances including the locations where critical events resulting in out-of-hospital cardiopulmonary arrest (OHCPA) occur.
Materials and Methods:
Subjects of this population-based observational case series study were the clinical records of patients with nontraumatic and nonneck-hanging OHCPA.
Results:
Of all 1546 cases, 10.3% occurred in a public place (shop, restaurant, workplace, stations, public house, sports venue, and bus), 8.3% on the street, 73.4% in a private location (victim's home, the homes of the victims’ relatives or friends or cheap bedrooms, where poor homeless people live), and 4.1% in residential institutions. In OHCPA occurring in private locations, the frequency of asystole was higher and the outcome was poorer than in other locations. A total of 181 OHCPA cases (11.7%) took place in the lavatory and 166 (10.7%) in the bathroom; of these, only 7 (3.9% of OHCPA in the lavatory) and none in the bath room achieved good outcomes. The frequencies of shockable initial rhythm occurring in the lavatory and in bath room were 3.7% and 1.1% (lower than in other locations, P = 0.011 and 0.002), and cardiac etiology in OHCPA occurring in these locations were 46.7% and 78.4% (the latter higher than in other locations, P < 0.001).
Conclusions:
An unignorable population suffered from OHCPA in private locations, particularly in the lavatory and bathroom; their initial rhythm was usually asystole and their outcomes were poor, despite the high frequency of cardiac etiology in the bathroom. We should try to treat OHCPA victims and to prevent occurrence of OHCPA in these risky spaces by considering their specific conditions.
Keywords: Bathroom, lavatory, OHCPA, out-of-hospital cardiopulmonary arrest, the relation between outcome and location
INTRODUCTION
In the past decade, greater numbers of people are noticing the importance of immediate rescue for collapsed persons and are becoming interested in rescue procedures such as cardiopulmonary resuscitation (CPR).[1,2] Academic entities and associations have been changing the guidelines for CPR and the rescue of collapsed or injured persons. The numbers of citizens who are willing to perform CPR and who have actually performed CPR when they are advised to do CPR by personnel of emergency call center using telephone CPR advice are increasing.[2] Rescuers can often use publicly accessible automated external defibrillators (AEDs) during CPR, which have been increasingly placed in public locations.[3] However, it is still unclear where and how frequently the medical emergency events resulting in out-of-hospital cardiopulmonary arrest (OHCPA) occur and where we are likely to encounter victims of OHCPA. Although there are many previous reports showing risky place for OHCPA, they roughly categorized the area such as public space, private space, and so on. There is few information concerning more detailed locations or rooms in the area. This information is important for preparing students of CPR to rescue these victims of OHCPA quickly, preventing the occurrence of these critical events, and improving outcomes overall. It is far more important to prevent the occurrence of events, resulting in OHCPA than to resuscitate patients with OHCPA. The aim of this study is to clarify the circumstances including the locations where critical events resulting in OHCPA occur and to clarify the conditions that pose risks for OHCPA, particularly to clarify the risks inherent in lavatories and bath rooms in a typical Japanese urban area (in Japan, lavatories and the rooms in which baths are taken are generally separate; we use the term “bath room” to distinguish them from the American multipurpose “bathroom”).
MATERIALS AND METHODS
Study protocol and data collection
This study was a population-based observational case series study under the emergency medical service (EMS) system with quick transport by ambulance service with emergency life-saving technicians (ELSTs) in a typical urban city in Japan. The clinical records of patients with OHCPA treated in our emergency department (ED) were reviewed. Patients with nontraumatic and nonneck-hanging OHCPA treated in the study period were enrolled. Cases of OHCPA occurring after contact with EMS team at the scene were included, while OHCPA occurring in the hospitals ED were excluded. Patients in home medical care system who were planned to be transferred to the destined hospital with OHCPA due to terminal stage of malignant disease or aging were also excluded. In reviewing our records, we focused on the place where OHCPA or the lethal event inducing OHCPA occurred, and other relevant information concerning OHCPA.
Just after arrival at our ED, ELSTs filled out ED forms made in and specific for our hospital as well as action reports for prehospital EMS records made in and specific for the fire department of our city. One resident or staff of our ED interviewed bystanders and the ELST as to who found the victim and where, whether someone witnessed the collapse of the victims or not, whether the victim had preceding symptoms or not, and so on. Our interviewer devoted himself to information control and gathered information on the patient in as much detail as possible without directly treating the patient. Our clinical records were entered on the spot and checked in two subsequent conferences in our ED.[1,4] Etiology of OHCPA was defined after detailed interview, blood examinations and some perimortem imagings such as ultrasonography, computed tomography.[1]
The study period was 5 years comprising two separate periods, with the first period lasting from September 2002 to February 2005 and the second period from September 2007 to February 2010. We selected these periods because the international and national guidelines for CPR changed their recommendation for CPR at the end of 2005. During these periods, old or new guidelines and our protocol for CPR according to these guidelines were thought to be generally accepted by all dispatchers, ambulance crews, and other EMS team members including ELSTs, hospital staff, and citizens. Just before and immediately after the guidelines for CPR were officially changed, the treatment strategies of the EMS system and their protocol for OHCPA as well as in-hospital treatment strategies for OHCPA were in transition.
In this study, a public location was defined as a railway station, public or private office building, athletic stadium, sports venue, place of recreation, industrial place, bus or train, or other public property, excluding health care facilities (hospitals, general practitioners’ offices, or small-sized private hospitals and clinics having some beds). The street and highway, river and sea, shop or in-house work place, restaurant, and hotel were described as the “other” category and differentiated from public location. A private location was defined as a home (home of the victims and their relatives or friends), a residential institution (a nursing home, aged people residence or cheap bed rooms, where poor homeless people live). The place where OHCPA occurred was defined as the place where critical symptoms occurred, such as severe chest pain, severe headache, severe back pain, syncope, and collapse.
All procedures were conducted according to the Declaration of Helsinki and under general ethical approval using prescribed general comprehensive and inclusive consents form addressed to our hospital when patients visited our hospital at the first time concerning application of patient's data to clinical research and publishing in the form in which the source of the data cannot be detectable. Statistical differences were calculated using chi-square test.
EMS system in the study area
In Japan, an out-of-hospital EMS system has been established that involves ambulance service and ELSTs belonging to the fire department, and the in-hospital emergency department supports this system. The ELST license was established in 1991, and the activities performed by them have expanded to include defibrillation by AED, cannulation into peripheral veins and infusion of Ringer's solution, and insertion of laryngeal mask airway, esophageal gastric tube airway, and laryngeal tube. Today, some ELSTs who have received proper prearranged training are permitted to perform endotracheal intubation and can administer adrenaline under restricted conditions. Recently, television stations have broadcast information about the work of ELSTs, resulting in enlightenment of many citizens on the importance of immediate CPR and defibrillation.[1,4,5,6,7]
We are establishing a prehospital and interhospital EMS system for critical and severe patients including OHCPA in our city.[1,4,5,6,7] Yokohama is the second-largest city in Japan and our institute is located in the center of Yokohama. Yokohama has an area of 434 km2 and the population of Yokohama is 3.37 million. We selected 12 hospitals, whose EDs can receive and treat the severest patients including OHCPA patients, and which have to receive patients with OHCPA independent of their capacity. One EMS director (a medical doctor) who belongs to the 12 hospitals is stationed in the central operation center in the fire department of the city. This director advises ELSTs, orders treatment through them, and notifies the hospitals when OHCPA patients are being transferred to them. The hospital receiving CPA patients is decided upon based simply based on proximity that means our city is divided in 12 areas concerning transfer of patients with OHCPA and patients with OHCPA in each area are transfer to the destined hospital of 12 hospitals in each area, and that means the data concerning OHCPA consist of the case-series population based for each hospital, including ours [Figure 1].[1,4,5,6,7] The area is defined according to the distance and interval for transfer by ambulance considering road and highway network. That means the background population of this single center study is about 0.28 million, which figure is not accurate and unclear because population is variable every hour. In our city, most people die in hospitals, who were usually transferred to some hospitals before their death.
Figure 1.
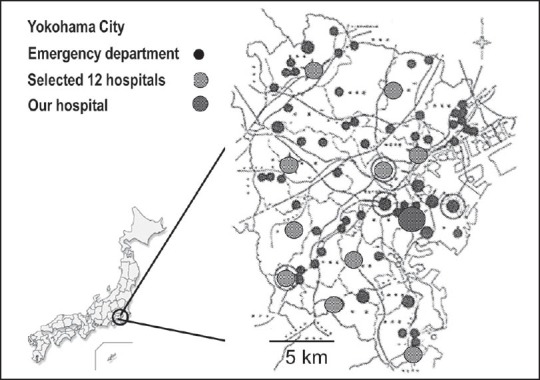
Map of Yokohama City indicating the 12 hospitals to which the emergency medical service system transfers out-ofhospital cardiopulmonary arrest (OHCPA) patients based on the nearest emergency department and which must receive OHCPA patients. For each hospital in Yokohama including our hospital, all data concerning CPA patients are population-based
RESULTS
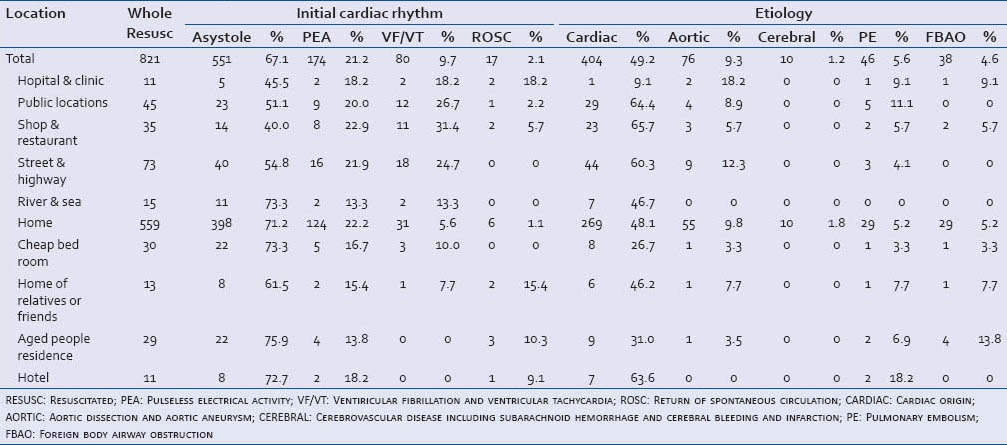
The location of the event could be identified in all 1546 patients (821 in the first period and 725 in the second period). Mean age of these patients was 70.0 years old. The prehospital mean time interval from collapse to call and interval from call to EMS arrival was 6.0 and 5.9 min. The number of available EMS units was 42 which were working in not only in our area but also in whole city. Of 1546 cases, 25 (1.6%) took place in health care facilities. A total of 159 (10.3%) occurred in a public place (shop, restaurant, and workplace, 82; railway stations, public or semipublic house, mass gathering, sports venue, coach, and bus, 77), and 127 (8.2%) occurred on the street and 19 (1.2%) in the sea or river. A total of 1134 (73.4%) took place in private locations (victims’ homes, 1050 [67.9%]; in boarding house, 69 [4.5%]; and in the homes of the victims’ relatives or friends, 15 [1.0%]). A total of 64 (4.1%) of the cardiac arrests took place in a residential institution, such as residences for the aged. Of the 1546 cases, 677 (43.8%) cases achieved return of spontaneous circulation (ROSC), 535 (34.6%) were admitted, 235 (15.2%) survived over 7 days, and 73 (4.7%) achieved Cerebral Performance Categories (CPCs) 1 and 2. The prognosis was not improved in the second period compared with the first period. The rate of 7-day survival differed among locations, from 10.2% to 39.0%, and the rate of CPC 1 and 2 differed from 1.5% to 21.1%. These rates of CPC 1 and 2 were lower than 12% in patients’ homes, cheap bed rooms, residential institutions, and hotels [Table 1]. Restricted in the second period, the frequency of asystole as the initial cardiac rhythm in OHCPA occurring in the victim's home, in the homes of the patients’ relatives or friends or the cheap bed rooms was higher than in other locations. On the contrary, the rate of cardiac etiology in OHCPA occurring in these locations and hotels was lower [Table 2].
Table 1.
Outcome of out-of-hospital cardiopulmonary arrest in each location
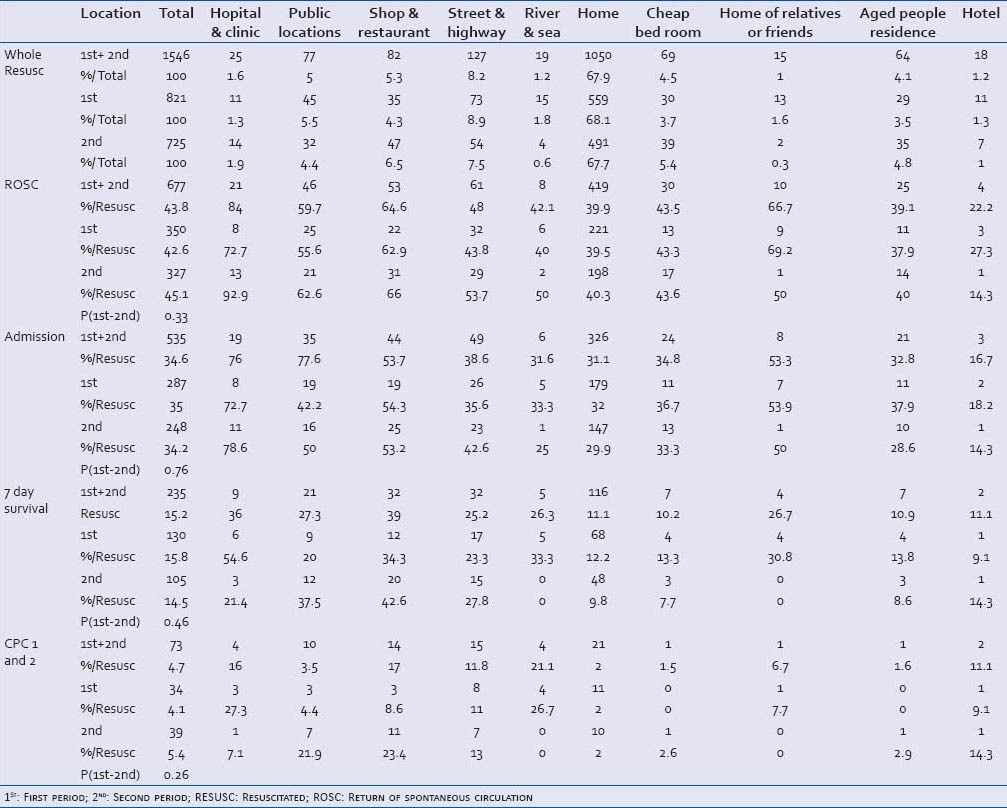
Table 2.
Initial cardiac rhythm and etiology of out-of-hospital cardiopulmonary arrest occurring in each location restricted in the second period
Of all 1546 cases, 181 cases (11.7%) took place in the lavatory and 165 (10.7%) in the bath room, particularly 143 (9.3%) in the bathtub; the rates were the same in the first and second period [Table 3]. Although 52.5% of OHCPAs in the lavatory were witnessed, only 13.3% in the bath room were witnessed. A large number of OHCPAs occurring in a lavatory, along the street or highway, in a public location, cheap bed rooms and patients’ private home were not witnessed. Of OHCPAs occurring in a bath room in the patients’ home, only 9% were witnessed [Table 4]. Although 181 OHCPA occurred in a lavatory, 82 (45.3%) achieved ROSC, 57 (31.5%) were admitted, 22 (12.2%) survived over 7 days, and 7 (3.9%) achieved CPC 1 and 2; meanwhile, only 40 (24.2%) of 165 OHCPA occurring in a bath room achieved ROSC, 30 (18.2%) were admitted, 3 (1.8%) survived over 7 days, and none achieved CPC 1 and 2 [Tables 5 and 6].
Table 3.
Number and frequency of out-of-hospital cardiopulmonary arrest occurring in the lavatory and bath room
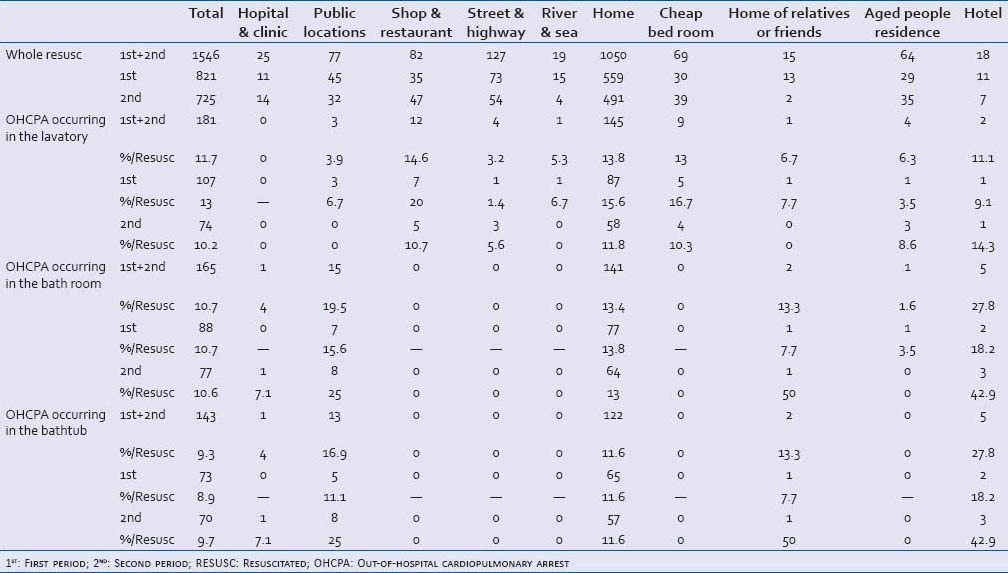
Table 4.
Witnessed out-of-hospital cardiopulmonary arrest in the lavatory and bath room
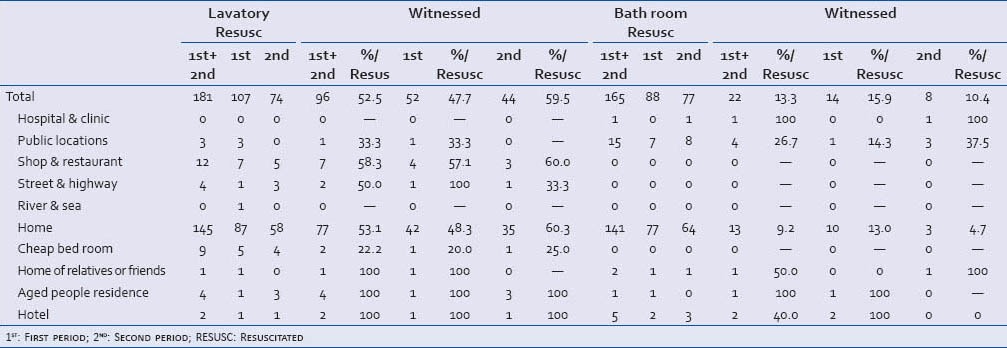
Table 5.
Outcome of out-of-hospital cardiopulmonary arrest occurring in the lavatory
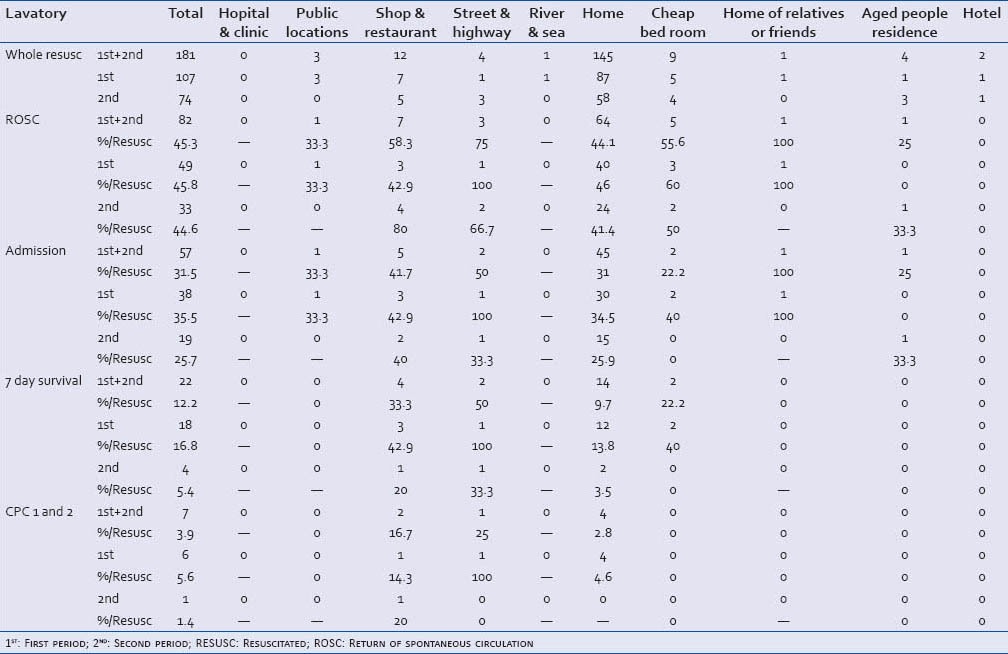
Table 6.
Outcome of out-of-hospital cardiopulmonary arrest occurring in the bath room
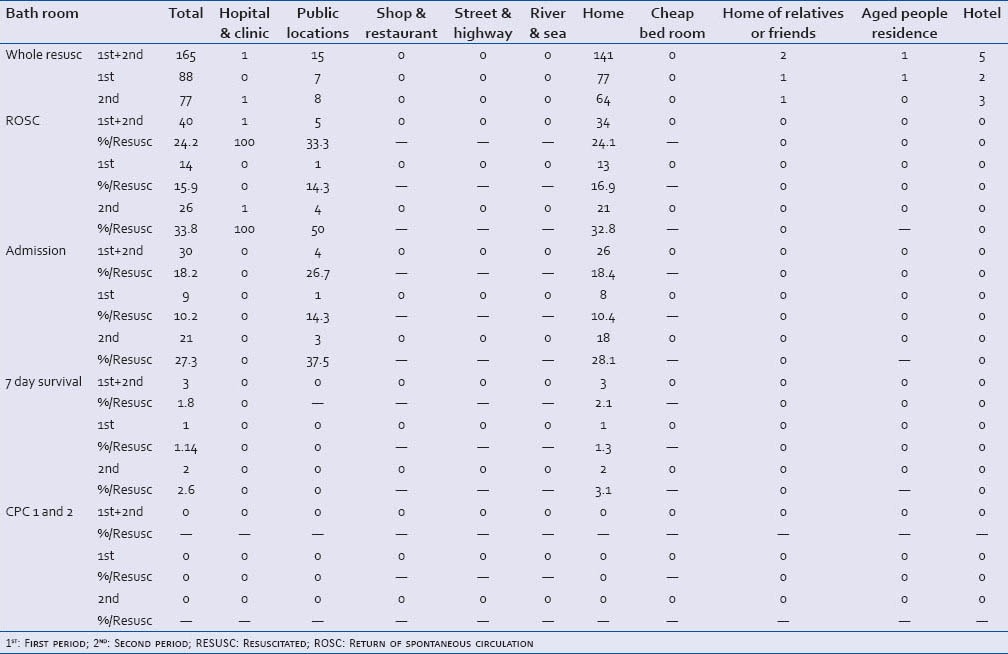
In the second period, the frequency of shockable cardiac rhythm in OHCPA occurring in the lavatory and in bath room was 3.7% and 1.1%, which was statistically lower than that of OHCPA occurring in other locations (P = 0.011, 0.002, respectively). On the contrary, the frequencies of asystole as the initial cardiac rhythm in OHCPA occurring in the lavatory and the bath room were 76.6% and 90.9%, which were statistically higher than that of OHCPA occurring in other locations (P = 0.003, <0.001, respectively). Concerning the etiology of OHCPA, the frequency of cardiac etiology was 46.7% of OHCPA occurring in the lavatory, with no statistical difference compared with that of OHCPA occurring in other locations and 78.4% of OHCPA occurring in the bath room, which was statistically higher than that of OHCPA occurring in other locations (P < 0.001) [Table 7].
Table 7.
Initial cardiac rhythm and etiology of out-of-hospital cardiopulmonary arrest (OHCPA) occurring in the lavatory and bath room compared with OHCPA occurring in other locations
DISCUSSION
Information concerning the location where critical events resulting in OHCPA occur is essential to deciding where we should place AEDs and devising ways to prevent OHCPA based on the specific conditions of each location or place, educating possible bystanders what they should do at such a location, and educating citizens what they can do at such a location. Some studies have reported that 65% of OHCPAs take place in the victims’ homes, 13% were outdoors, 3% in cars; these OHCPA cases are regarded not to be generally suitable for public access defibrillation (PAD). On the contrary, 6% of OHCPA happens in public buildings, 1% in general practitioners’ offices and 7% in care facilities, 1% at patients’ workplace, and 1% in public transport locations; these 17% of total OHCPAs are regarded as generally suitable for PAD.[8] Other authors have reported that the peak of occurrence of OHCPA is at 17:00-18:00 hours; younger patients have more cardiac arrests in the morning than in the evening, and older patients have more events in the evening than in the morning, which tendency may have been associated with bath time in the evening, a custom in the author's country.[9]
It was reported that the frequency of shockable initial cardiac rhythm was lower among patients with OHCPA witnessed in the home (35%) than among those in a public setting (60%). The authors emphasized that prompt bystander-delivered CPR should be as effective in saving lives as the widespread deployment of AEDs in homes.[10] Iwami et al.,[11] reported that although the majority of OHCPA occurred at private residences, arrests in public or in the work place had a higher chance of being found with shockable cardiac rhythm and survival than those at private residences. They concluded that a strategy considering the location of arrest is necessary to establish a system to improve the outcome of OHCPA. Eisenburger et al.,[12] reported that patients with OHCPA in a nonpublic location survived to discharge at a lower rate (31%) and had a poorer neurological outcome after 6 months (25%) than patients with OHCPA in a public location (39% and 35%). Our data also confirmed that the rate of shockable cardiac rhythm in victims of OHCPA in the home and their survival rate were lower than those in public locations.
Although these reports clarified the occurrence rate and character of OHCPAs among several locations, particularly in victim's home or public spaces, they did not consider in detail the place or room in each location, such as lavatory, bath room, or dining room. We paid attention to the detailed location such as lavatory and bath room. Victims in these places cannot be easily witnessed, and sound may be the only clue a witness has, resulting in poor outcome independent of the etiology of OHCPA. In these situations, prevention may be more necessary and effective for improvement of total death outside the hospital than rescue procedures. The dining room, bedroom, and living room are probable event locations in the home, each with a specific environment and conditions. However in Japan, the dining room is often combined with the living room and bedroom, and aged people often have meals in the bedroom or living room, not in the dining room. In this report, we did not evaluate the occurrence of OHCPA in dining room, living room, and bedroom.
Witnessed OHCPA in the home setting included respiratory etiology due to chronic pulmonary disease and airway obstruction during mealtime, and other obvious noncardiac etiology.[13,14] OHCPA with cardiac etiology occurring in the home setting may not be witnessed, and their initial cardiac rhythm was recorded as unshockable because of the delay from the event to the initial record of electrocardiogram or the initial application of AED. Our data also showed the low frequency of witnessed or cardiac OHCPA in the home setting, particularly in the lavatory or bath room, where most events were unwitnessed and initial response tended to be delayed, which indicated the low propriety and usefulness of PAD for the home setting. And this fact is the cause of our low overall survival with good recovery or mild disorder and the proportions of patients with VF/VT as initial arrhythmia. It is thought to be important and effective for saving victims who are likely to experience OHCPA in the home to prevent OHCPA from occurring at each specific location, and to know the risky time, place and location in the home. We should encourage people not to stay in the risky locations if they were ill and not to strain themselves in the risky locations. Our data showed that the bath room is risky place for OHCPA occurring with cardiac etiology, particularly for aged people, and that the lavatory is also a risky place in Japan.
OHCPA persists as a major public health problem in Japan as elsewhere. Several studies have reported a decline in the incidence of shockable initial cardiac rhythm among patients with OHCPA and that unstructured and over-the-counter PAD programs are probably less effective than believed in the past.[15,16] Weisfeldt et al.,[10] reported that it was possible that delays in calling for EMS help were responsible for the low frequency of shockable initial rhythm among OHCPAs occurring at home. The time intervals within the standard EMS system are still too long, even in advanced countries, particularly in more remote areas. For example, in 2011 the mean time interval in Unnan City in Shimane, which is a typical rural area in Japan, was 9.6 min, the longest was 43 min, and it took more than 20 min in 11.5% of missions.[17] Moreover, some authors reported that patients with OHCPA in the home are typically older and more likely to have many chronic diseases that limit or preclude participation in activities outside the home; that means that the location of OHCPA may be a surrogate variable for underlying disease or disease severity.[10] More rapid activation and contact of EMS and further knowledge about where and how OHCPA occurs will perhaps be the main challenge in the future.
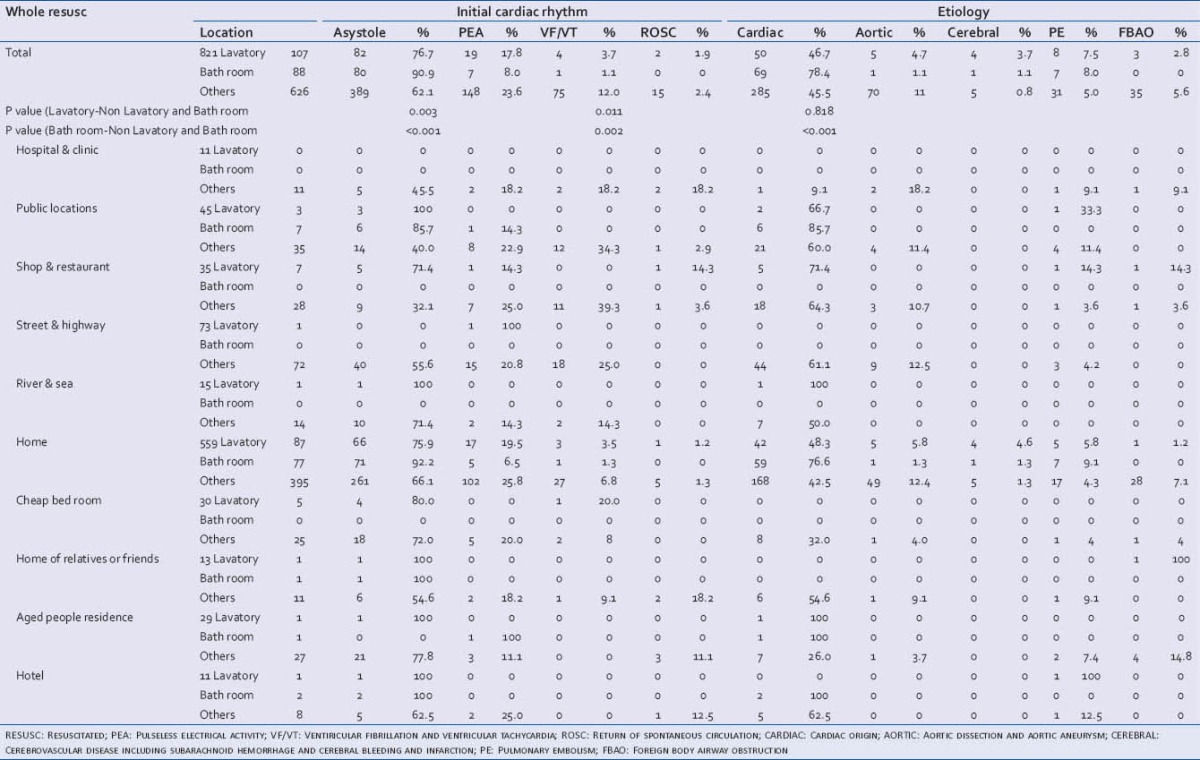
The lavatory is known as a place where blood pressure can easily increase or decrease with urination and defecation, where cardiovascular events are frequently seen and where OHCPAs frequently occur. From our results, however, more than half of the cases of OHCPA occurring in the lavatory are witnessed and can be treated quickly by lay persons and EMS, resulting in high expectancies of good outcomes. In the past or in rural areas in Japan, the lavatory was located outside of the house with a cool environment and had Japanese-style toilet equipment on which we squatted down and must keep the position [Figure 2]. Today in most lavatories in Japanese typical urban city, we sit on a toilet, as in most western countries, with a system of warming a sitting part and heating a room.
Figure 2.
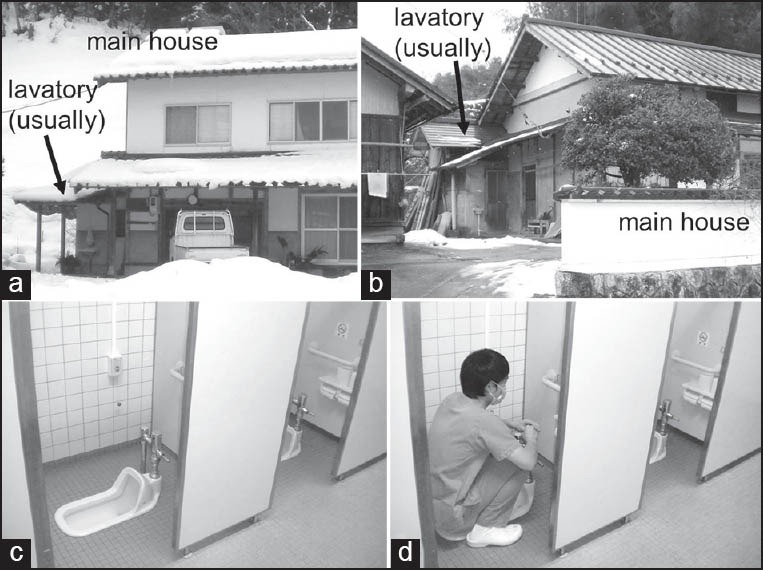
Lavatory in typical Japanese rural areas: lavatory in the separated or outside location from the main house in the typical classic Japanese house (a and b) and Japanese-style toilet equipment on which we squatted down and must keep the position (c and d)
The bath room in Japan is also known as a place where the temperature changes dynamically and where cardiovascular events are frequently seen; our data support this assumption. However, most OHCPAs in bath rooms are unwitnessed and are found a long time after the collapse, resulting in asystole. We cannot accurately evaluate the etiology of their OHCPA, cannot provide a strategy for prevention and treatment, and cannot rescue them even if they have a cardiac etiology. Prevention is thought to be more important than treatment. We have educated citizens in the large risk of critical events occurring in the bath room and several measures have been taken to cope with the situation, such as temperature control in the bath room and short bathing in the bathtub with tepid hot water. However, we have no evidence about how effective these measures are? In this study, we showed better outcomes from the view points of ROSC, admission, and short-term prognosis in the second period than in the first period, but there were no bath room-occurring OHCAP patients with good outcomes in either period. The only action we can do to improve the outcome of OHCAP in the bath room may be prevention of OHCPA.
Limitations
In this study, we defined the place where OHCPA occurred as the place where critical symptoms occurred such as severe chest pain, severe headache, severe back pain, syncope, and collapse. Most other reports have defined the place where OHCPA occurs as the place where the victims fall into OHCPA. We think that the place where the critical symptoms occur is more important for analyzing etiology, pathophysiology, preventability, and treatability of the victim than the place the victims fall into OHCPA. We frequently have seen patients who have chest pain in a restaurant and fall down on the street outside the restaurant. In some of these cases, the important place is not the street but the restaurant because we can treat their coronary disease more easily and more certainly and can provide them a chance of better outcome if we detect the event and can activate the EMS system before they suffer from OHCPA. Of course in those cases, it is easier to detect the event after the victims fall into OHCPA than before they suffer from OHCPA, so that the place where OHCPA occurs is also important. Indeed, in some of these cases the low temperature on the street may be lethal. Moreover, in cases of unwitnessed OHCPA, we cannot detect the victims suffering from critical symptoms in the place where the events occur before falling into OHCPA and we can only detect the victims in the place where they fell down.
In this study, we presented very low proportions of patients with OHCPA, with good recovery and with VF/VT in comparison to many EMS systems in Europe and North America. We enrolled all patients with OHCPA, including many unwitnessed patients who seemed to have no chance to achieve ROSC because in our city all patients with OHCPA were obligated to be transferred to the selected 12 hospital and to be attempted to resuscitate except patients displaying the full signs of death (rigor mortis, dead spot, and decapitation) and patients who underwent home medical care and were to be transferred to the destined hospital in condition of OHCPA, whose initial cardiac rhythms were usually not VF/VT. However, our home medical system is incomplete and many patients under this system were not transferred to destined hospital but to the nearest hospital of 12 hospitals and resuscitated as OHCPA patients without any advanced information. Our subjects include many these patients falling into cardiac arrest in our area who were to be transferred to the destined hospital out of our area. These conditions explain the low incidence of OHCPA, low incidence of VF/VT, and low whole survival rate with good recovery in our area. Our outcome should not be compared with those presented in other reports and should be compared within our data.
CONCLUSION
In a typical Japanese urban city, the proportion of patients suffering from OHCA in private locations is denoted unignorable; 73% of OHCPAs took place in private locations (victim's home, in the homes of the patients’ relatives or friends and cheap bed rooms) and 12% took place in the lavatory and 11% in the bath room. The prognosis of such events did not improve over the last decade. The frequency of VF/pulseless VT as the initial cardiac rhythm in OHCPA occurring in private locations and in hotels was lower than in other location. The frequency of shockable cardiac rhythm was lower and outcomes were much worse in OHCPA occurring in the lavatory and the bath room. We should try not only to rescue and treat OHCPA victims but also to prevent occurrence of OHCPA in these risky spaces by addressing the specific conditions responsible for the risk.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Moriwaki Y, Tahara Y, Kosuge T, Suzuki N. Etiology of out-of-hospital cardiac arrest diagnosed via detailed examinations including perimortem computed tomography. J Emerg Trauma Shock. 2013;6:87–94. doi: 10.4103/0974-2700.110752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rea TD, Eisenberg M, Culley LL, Becker L. Dispatcher-assisted cardiopulmonary resuscitation and survival in cardiac arrest. Circulation. 2001;104:2513–6. doi: 10.1161/hc4601.099468. [DOI] [PubMed] [Google Scholar]
- 3.Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, et al. Public Access Defibrillation Investigators. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–46. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 4.Moriwaki Y, Sugiyama M, Tahara Y, Iwashita M, Kosuge T, Harunari N, et al. Complications of bystander cardiopulmonary resuscitation for unconscious patients without cardiopulmonary arrest. J Emerg Trauma Shock. 2012;5:3–6. doi: 10.4103/0974-2700.93094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tahara Y, Kimura K, Kosuge M, Ebina T, Sumita S, Hibi K, et al. Comparison of nifekalant and lidocaine for the treatment of shock-refractory ventricular fibrillation. Circ J. 2006;70:442–6. doi: 10.1253/circj.70.442. [DOI] [PubMed] [Google Scholar]
- 6.Moriwaki Y, Sugiyama M, Yamamoto T, Tahara Y, Toyoda H, Kosuge T, et al. Outcomes from prehospital cardiac arrest in blunt trauma patients. World J Surg. 2011;35:34–42. doi: 10.1007/s00268-010-0798-4. [DOI] [PubMed] [Google Scholar]
- 7.Moriwaki Y, Sugiyama M, Hayashi H, Mosiello G, Cremonese F, Altomani V, et al. Emergency medical service system in Yokohama, Japan. Annali Degli Ospedali San Camillo e Forlanini (Annals of San Camillo and Forlanini Hospiptal) 2001;3:344–56. [Google Scholar]
- 8.Engdahl J, Herlitz J. Localization of out-of-hospital cardiac arrest in Goteborg 1994–2002 and implications for public access defibrillation. Resuscitation. 2005;64:171–5. doi: 10.1016/j.resuscitation.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Tsukada T, Ikeda T, Ishiguro H, Abe A, Miyakoshi M, Miwa Y, et al. Circadian variation in out-of-hospital cardiac arrests due to cardiac cause in a Japanese patient population. Circ J. 2010;74:1880–7. doi: 10.1253/circj.cj-10-0008. [DOI] [PubMed] [Google Scholar]
- 10.Weisfeldt ML, Everson-Stewart S, Sitlani C, Rea T, Aufderheide TP, Atkins DL, et al. Resuscitation Outcomes Consortium Investigators. Ventricular tachyarrhythmias after cardiac arrest in public versus at home. N Engl J Med. 2011;364:313–21. doi: 10.1056/NEJMoa1010663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iwami T, Hiraide A, Nakanishi N, Hayashi Y, Nishiuchi T, Uejima T, et al. Outcome and characteristics of out-of-hospital cardiac arrest according to location of arrest: A report from a large-scale, population-based study in Osaka, Japan. Resuscitation. 2006;69:221–8. doi: 10.1016/j.resuscitation.2005.08.018. [DOI] [PubMed] [Google Scholar]
- 12.Eisenburger P, Sterz F, Haugk M, Scheinecker W, Holzer M, Koreny M, et al. Cardiac arrest in public locations--an independent predictor for better outcome? Resuscitation. 2006;70:395–403. doi: 10.1016/j.resuscitation.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 13.Hess EP, Campbell RL, White RD. Epidemiology, trends, and outcome of out-of-hospital cardiac arrest of non-cardiac origin. Resuscitation. 2007;72:200–6. doi: 10.1016/j.resuscitation.2006.06.040. [DOI] [PubMed] [Google Scholar]
- 14.Norris RM UK Heart Attack Study Collaborative Group. Circumstances of out of hospital cardiac arrest in patients with ischaemic heart disease. Heart. 2005;91:1537–40. doi: 10.1136/hrt.2004.057018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ringh M, Herlitz J, Hollenberg J, Rosenqvist M, Svensson L. Out of hospital cardiac arrest outside home in Sweden, change in characteristics, outcome and availability for public access defibrillation. Scand J Trauma Resusc Emerg Med. 2009;17:18. doi: 10.1186/1757-7241-17-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fleischhackl R, Roessler B, Domanovits H, Singer F, Fleischhackl S, Foitik G, et al. Results from Austria's nationwide public access defibrillation (ANPAD) programme collected over 2 years. Resuscitation. 2008;77:195–200. doi: 10.1016/j.resuscitation.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 17.Moriwaki Y, Okuda J, Niwano T, Sawada Y, Ohtani J. Meaning and Issues concerning interhospital transfer using emergency medical helicopter system in rural area: Importance of the appropriate usage of medical emergency call. J Shimane Med Assoc. 2013:33. [Google Scholar]


