Abstract
Aims:
We analyzed our series of patients with seatbelt signs (bruising) that underwent laparotomy in order to correlate injury pattern with clinical course and outcome.
Materials and Methods:
Retrospective analysis of patients with seatbelt signs presenting to the level 1 Trauma Unit between 2005 and 2010 was performed. We evaluated the nature of injuries during laparotomy associated with seatbelt signs and their treatment and complications.
Results:
There were 41 patients, 25 (61%) male, with a median age of 26 years. Median injury severity score (ISS) was 25 (range 6–66) and overall mortality was 10% (four patients). Patients were classified into three groups according to time from injury to surgery. Median time to surgery for the immediate group (n = 12) was 1.05 h, early group (n = 22) was 2.7 h, and delayed group (n = 7) was 19.5 h. Patients in the immediate group tended to have solid organ injuries; whereas, patients in the delayed group had bowel injury. Patients with solid organ injuries were found to be more seriously injured and had higher mortality (P < 0.01) and morbidity compared with patients with the “classic” bowel injury pattern associated with a typical seatbelt sign.
Conclusion:
Our data suggest that there is a cohort of patients with seatbelt injury who have solid organ injury requiring urgent intervention. Solid organ injuries associated with malpositioned seatbelts lying higher on the abdomen tend to result in hemodynamic instability necessitating immediate surgery. They have more postoperative complications and a greater mortality. Seatbelt signs should be accurately documented after any car crash.
Keywords: Bowel injury, laparotomy, seat belt, seat belt sign, solid organ injury
INTRODUCTION
Since the introduction of the three-point seatbelt in the 1970s, fatalities from road traffic crashes have fallen by up to 60%.[1,2] In road traffic injury prevention, the seatbelt and accompanying legislation is regarded as one of the most prominent successes in reducing injury rates and deaths.[3,4] Over the years, however, a well-defined injury pattern related to the use of seat belts has become the norm of presentation in patients involved in, especially, high energy impacts.[5,6]
The patterns of injury, known as seatbelt syndrome, describe injuries to underlying organs resulting from shearing forces in the lower abdomen due to restraint and rapid deceleration causing high pressure blowout intestinal perforations and mesenteric tears, or more commonly, in the chest, fractures of the sternum, ribs, and even the clavicle.[7,8] In rare cases there may be major thoracic injury with aortic transection or in the neck, injuries to major vessels.[9,10,11]
Clues to underlying injuries are bruises and abrasions on the skin following the pattern of the seatbelt, whether over the shoulder, diagonally across the chest, or a horizontal band across the lower abdomen.[12,13] When considering patients with abdominal injuries, in those who are hemodynamically unstable or obviously have peritonitis, the decision to proceed to laparotomy is straightforward; but in patients who respond well to fluid resuscitation or have equivocal findings on examination of the abdomen and are hemodynamically normal, predicting their internal injuries and clinical course tends to rely on imaging and regular evaluation of the abdomen, preferably by the same surgeon.
We report our experience in a level 1 trauma center in dealing with patients with abdominal injuries arising from seatbelt restraint in road traffic accidents, with particular attention to the subgroup of patients who underwent emergency laparotomy and had evolving clinical signs. With regard to the seatbelt-related injury pattern, we hypothesized that injuries found at laparotomy might predict outcome.
MATERIALS AND METHODS
We retrospectively reviewed the records of all patients who underwent laparotomy for abdominal injury who had a seatbelt sign after a road traffic crash at the level I Trauma Center, Hadassah University Hospital, Ein Kerem Campus, in Jerusalem, Israel, between January 2005 and October 2010. Patients with seatbelt injuries who required laparotomy were identified and data were retrieved from the Hadassah Trauma Registry and from paper and electronic medical records. Mortality was our primary outcome measure. Postoperative morbidity (surgical site infection (SSI) and pneumonia) was recorded and analyzed as a secondary outcome measure.
Patients were classified as having a seatbelt sign if they had a bruise on the abdomen, chest, or neck corresponding to the site of the restraints. Data collected from the patients included: demographics; the exact mechanism of injury; position within the car; injury severity score (ISS); physiological status upon arrival in the Emergency Department (ED); time from crash to operative intervention; anatomical location of injuries; intraoperative findings; length of hospitalization; management and treatment during hospital course; and complications and outcome. Concomitant injuries were managed according to the specific pathology. Patients with fatal head injury or those who required immediate craniotomy were excluded. All patients described had seatbelt signs. The exact location of the seatbelt sign, however, was not recorded on most admission charts.
Indications for laparotomy included hemodynamic instability with a strong suspicion of an intra-abdominal injury, diffuse peritonitis, or radiological findings indicating bowel perforation or mesenteric tear, and clinical deterioration in patients managed expectantly. Repeat imaging was based on clinical suspicion of internal injury.
Hemodynamic instability in our study was defined as a heart rate above 100 beats per min with a systolic blood pressure of less than 90 mmHg. All patients underwent initial imaging of the abdomen with focused sonographic assessment for trauma (FAST) in the ED. Our institutional policy is to admit for observation patients with a seatbelt sign. FAST is performed at the bedside and a radiologist does this routinely in all cases of major trauma. Computed tomography (CT) scan with intravenous contrast was performed on patients who were hemodynamically normal or stable. Injury to the small bowel, large bowel, or both without solid organ injury was termed ‘isolated bowel injury’. ‘isolated solid organ injury’ was similarly defined.
Statistical analysis
Data are presented as median and interquartile range (IQR). Chi-squared test for trends and the Kruskal-Wallis test were used to compare categorical and continuous variables, respectively, between the three groups. Fisher's exact test was used to compare categorical variables as appropriate. A P-value of 0.05 or less was considered statistically significant. Statistical analysis was performed using Statistical Package for Social Sciences (SPSS) version 11.5 (SPSS, Chicago, IL).
RESULTS
Patient characteristics
Over the study period 1,071 patients were admitted after a car crash where seatbelt use was documented (three-point seatbelt only as a standard). Forty-one patients (3.8%) with documented abdominal seatbelt signs underwent exploratory laparotomy and form the study group. Backseat passengers were significantly more likely to require laparotomy compared with drivers and front seat passengers (15/190, 7.9% versus 16/602, 2.7% and 10/279, 3.6%, respectively, P = 0.005).
Patients were classified into three groups according to the timing of emergency surgical intervention: ‘Immediate’; ‘early’; and ‘delayed’. Twelve patients (29.3%) were taken to the operating room (OR) within a median of 1.05 h (range 0.5-1.6 h) and were labeled the ‘immediate’ group. Twenty-two patients (53.6%) were stable enough to undergo initial (CT) evaluation. These patients were taken to the OR within a median of 2.7 h (range 1.15-11.8 h) and were labeled the ‘early’ group. Seven patients (17.1%) were admitted and underwent initial evaluation, but their injuries were only recognized later. This group was termed the ‘delayed’ group and underwent laparotomy at a median of 19.5 h (range 12.2-51 h) after investigation and clinical review.
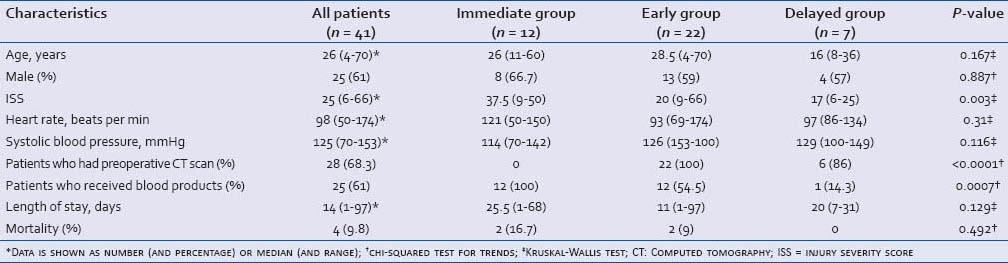
Table 1 summarizes the characteristics of all 41 patients. Patients in the delayed group tended to be younger and had significantly lower ISS compared with the immediate and early groups. Five of the seven patients (71.4%) in the delayed group were backseat passengers and none were drivers. Four of seven patients (57.1%) in the delayed group were ≤16 years old, significantly more compared with the early and immediate groups (four of 22, and one of 11, respectively, P = 0.026).
Table 1.
Characteristics of the 41 patients with seatbelt signs
Indications for laparotomy
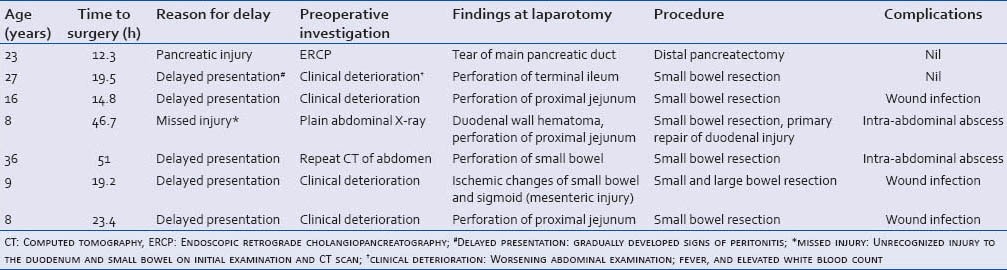
Indications for surgery in the immediate group (n = 2) were significant hemodynamic instability (n = 7) and generalized peritonitis on initial examination (n = 5). In total, preoperative CT was performed in 28 patients (68.3%). CT was performed for all patients in the early group. Indications for surgery in the early group were based on CT findings. CT scan findings included one or more of the following: Pneumoperitoneum (n = 10, 35.7%); free fluid without visible solid organ injury (n = 10, 35.7%); bowel wall thickening (n = 7, 25%); and high grade (IV-V) splenic injury with active bleeding (n = 3, 10.7%). Delayed laparotomy was performed in seven cases. Indications for surgery, reason for delay, preoperative assessment, time to surgery, and outcome in the delayed group are shown in Table 2.
Table 2.
Clinical characteristics of the delayed group
Pattern of injury
Small bowel injury (n = 24, 58%) was the most common injury found at laparotomy, followed by injury to the large bowel (n = 16, 39%) and spleen (n = 16, 39%). Gastric perforation-related to seatbelt trauma was found during laparotomy in five patients (12%). Twenty-two patients (53.6%) had isolated small bowel injury. Isolated solid organ injury was noted in 10 cases (24.4 %). Eight patients (19.6%) had combined solid organ and bowel injury. Major vascular injuries included abdominal aortic tear (n = 1), renal artery tears (n = 2), and inferior vena cava injury (n = 2). All five of these patients were taken directly to the OR due to hemodynamic instability on arrival to the ED.
The pattern of intra-abdominal injury was influenced by the time period from injury to surgery. The shorter the time period, the more common was injury to solid organs (chi-squared test for trends = 0.074). Conversely, the longer the period from injury to surgery, the more common was bowel injury (chi-squared test for trends = 0.085) [Figure 1].
Figure 1.
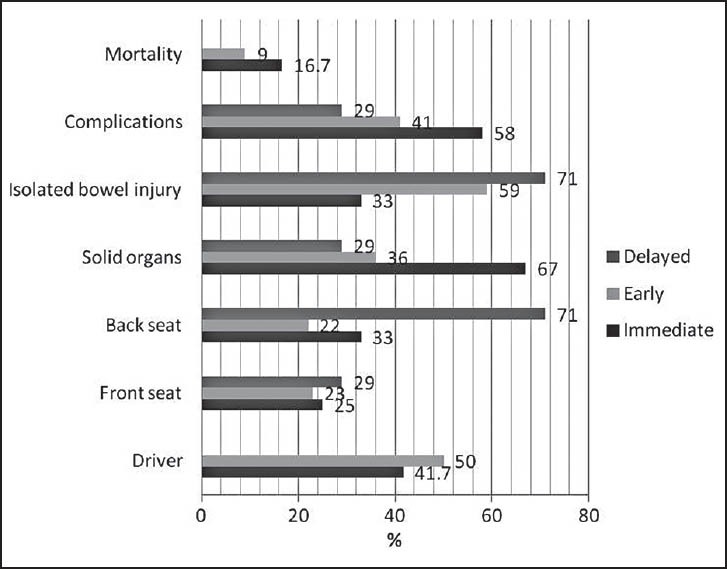
Pattern of intra-abdominal injury according to timing of laparotomy
Extra-abdominal injury
In addition to intra-abdominal injuries, other injuries included long bone fractures (n = 11, 26.8%), thoracic injuries (n = 26, 63.4%), pelvic fractures (n = 10, 24.4%), spinal injuries (n = 19, 46.3%), and brain injuries (n = 10, 24.4%). Six patients required surgery for spinal column injury and 11 patients required internal fixation of long bone fractures.
Complications and outcome
Eighteen patients (44%) suffered a total of 24 postoperative complications. SSI was found in 14 patients (34%), of whom seven patients (17%) developed an intra-abdominal abscess. None of the patients returned to the OR for relaparotomy because of an SSI; but two patients required percutaneous drainage, while the remaining patients were treated conservatively. Other notable complications included wound infection (n = 8, 19.5%), adult respiratory distress syndrome (ARDS; n = 4, 9.7%), pneumonia (n = 4, 9.7%), septicemia (n = 8, 19.5%), and acute renal failure (n = 4, 9.7%).
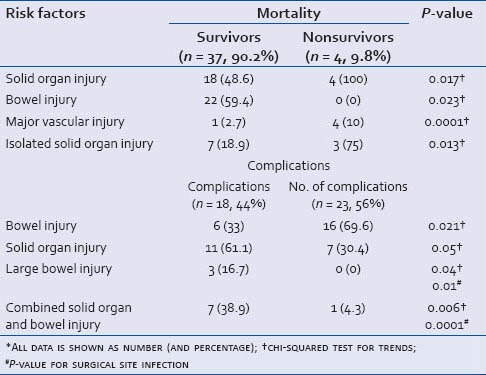
Patients with solid organ injury and patients with major vascular injury were significantly more likely to die of their wounds (four of 18 (22.2%) versus zero of 23, and four of five (80%) versus zero of 36 (0%), respectively, P = 0.017 and P < 0.0001). Injury to a solid organ and combined solid organ and bowel injuries were also associated with a higher complication rates [Table 3]. Delayed laparotomy was not associated with a higher incidence of infectious complications (two of seven (28.6%) versus 12 of 34 (35%); P = 1.0).
Table 3.
Risk factors for overall mortality and complications
Four patients died (9.7%). Two patients died within 24 h of admission from uncontrolled hemorrhagic shock: One patient, a 49-year-old backseat passenger with a suprahepatic inferior vena caval tear, cardiac tamponade, hemoperitoneum, cervical spine fracture, and head trauma; the second, a 62-year-old driver who arrived with pulseless electrical activity following crush injury to the chest and liver, and a diaphragmatic tear. Exploratory laparotomy followed by resuscitative thoracotomy and open cardiac massage were unsuccessful. Two additional patients survived initial surgery for liver, splenic, and renal injuries; but succumbed later to complications of sepsis and multiorgan failure in the intensive care unit (days 28 and 97 post injury).
DISCUSSION
Indications for laparotomy, as ever, are hemodynamic instability and peritonitis. Within the cohort of patients, albeit small, who presented with a seatbelt injury, we discuss below findings that may predict short-term outcome.
The first assertion is that the presence of a seatbelt sign should raise the suspicion of an intra-abdominal injury and that a correctly positioned seatbelt classically produces a pattern of external and internal injury, that is, sternal fracture, bowel perforation, mesenteric tear, and lumbar spinal injury. This classic injury pattern, indicating a higher incidence of abdominal injuries has been termed ‘the seatbelt syndrome’.
Chandler et al., (1997)[12] in a consecutive series of 117 patients injured in motor vehicle crashes found that of their 11.9% patients with a seat belt sign, all had underlying bowel injuries and possibly other visceral abdominal injuries. These patients were more likely to undergo laparotomy than patients without a seatbelt sign. Velmahos et al., in 1999,[13] studied 410 patients wearing seatbelts who were injured in road traffic crashes. Seventy-seven (12%) had a seatbelt sign. Of these 77 patients, 9% suffered bruising of the neck, 32% bruising on the chest, 40% bruising on the abdomen, and 19% bruising across multiple areas on the body. Three patients had myocardial contusion and 10 patients had intra-abdominal injuries (predominantly bowel and mesenteric lacerations) requiring laparotomy. They found a nearly four-fold increase in chest trauma (22.5 versus 6%; P = 0.01) and a nearly eight-fold increase in intra-abdominal injury (23 versus 3%; P < 0.0001) in the cohort restrained with seat belts as opposed to those without.
It is, therefore, common practice to suspect chest or abdominal injury in the presence of a seatbelt sign, even though not all cases will warrant surgical intervention. Where there is a high index of suspicion, but no obvious indication for immediate laparotomy, patients are observed expectantly for subtle signs of peritonitis or bleeding. Repeated clinical and radiological assessment (usually CT) is helpful in stable patients. Our experience has been to use intravenous contrast on initial CT and then repeat CT with both oral and intravenous contrast where initially stable patients have deteriorated.
Our data on patients with seatbelt signs suggest that bowel injury is more common in patients with delayed clinical signs; whereas, solid organ injury is more common in patients presenting from the outset with hemodynamic instability. Patients who suffered solid organ injury were more likely to develop postoperative complications. Additionally, solid organ injury with major vascular injury resulted in greater mortality. These solid organ injuries do not fall within the classical description of abdominal injuries associated with seatbelt syndrome, leading us to postulate that solid organ injury in restrained patients may require a higher energy of impact or may involve rotational, torsional or intrusive forces unrelated to the seatbelt, or indeed, that the seat belt was malpositioned.[14,15,16]
An ideally positioned seatbelt distributes energy across the lower abdomen and bony pelvis during impact. Incorrect seatbelt positioning, arising from poor belt quality, and poor adjustment in relation to the passenger's size, may cause serious, “nonclassical” intra-abdominal injuries. Fatal splenic injuries and fractures of the lumbar vertebra have been reported as a complication of incorrect application of the lap seatbelt strap across the abdomen.[16]
A further finding from our data was that in patients with a seatbelt sign, the risk of intra-abdominal injury is significantly higher for backseat passengers (P = 0.005) even though, as expected, ISS was significantly higher for front seat passengers and drivers. We surmised that seatbelts worn by passengers in the back seats of cars do tend to be malpositioned more commonly than in the front seats (especially as children usually sit in the back seat). Possible mechanisms of injury may be ‘jack-knifing’ forwards over a seatbelt or ‘submarining’ effects resulting in abdominal injuries as the maladjusted lap belt rides up over the iliac spines and injures solid organs and major vessels directly.[17,18] Lap belt injuries are associated with pediatric spinal cord injury in improperly restrained children. Several specific characteristics make children especially vulnerable: They have a higher center of gravity than adults, generating greater distraction forces and lap belts tend to lie over the abdomen instead of the pelvis because the iliac crests are not yet fully developed.[19] These factors may result in abdominal and spinal injuries during rapid deceleration.[20,21,22,23,24,25] In this series of 41 patients there were seven children (under 16 years of age). Delayed laparotomy was performed in four.
With these patterns in mind we suggest the following considerations when assessing patients with seat belt signs:
The presence of a seat belt sign is not on its own an indication for laparotomy,[8,11,13] but should raise clinical suspicion of significant internal injury;
The exact position of the seat belt sign may be important in terms of the underlying injury;
A seatbelt sign located over the center of the abdomen, the umbilical area or higher should alert us to the possibility of a solid organ injury in addition to the classic bowel injury expected in patients wearing appropriately-positioned seat belts that result in typical suprapubic bruises;[11,26]
Passengers in the back seat may be wearing malpositioned seatbelts and may present with nonclassical seatbelt injuries;
Documenting exactly where seatbelt bruises are on patients could be of value in determining causality between seatbelt position and organ injury. This was inadequately recorded in our institution, and we would like to stress the importance of this documentation in the future, especially as patients are usually unable to provide details about seatbelt quality or positioning.
Finally, our suppositions about mechanism of injury are compounded by the experimental studies that indicate that abdominal injuries to the driver produced by the impact of the lower rim of the steering wheel may be similar to the type of injury sometimes attributed to a lap belt.[27]
In summary, current practice is that the presence of an abdominal seatbelt sign requires the treating physician to maintain a high level of suspicion for internal injuries and to perform serial clinical examination and appropriate diagnostic tests in patients not proceeding immediately to laparotomy. Based on this small series, it is our opinion that malpositioned seat belts cause a different pattern of injury. Seat belts positioned low in the abdomen, that is, in the suprapubic region, cause pressure effects on the bowel which result in bowel perforation with clinical signs that develop more gradually and result in delayed surgery, but with low mortality. Whereas, malpositioned seatbelts, lying higher on the abdomen, are associated with a greater incidence of solid organ injury. Patients with solid organ injury tend to present with hemodynamic instability warranting immediate surgery and have a higher mortality.
ACKNOWLEDGEMENTS
The authors wish to thank Irina Gertsenstein for her invaluable assistance with Trauma Registry data collection.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Abbas AK, Hefny AF, Abu-Zidan FM. Seatbelts and road traffic collision injuries. World J Emerg Surg. 2011;6:18. doi: 10.1186/1749-7922-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peden M, Scurfield R, Sleet D, Mohan A, et al., editors. Geneva: World Health Organization; 2004. World report on road traffic injury prevention. [Google Scholar]
- 3.Budd JS. The effect of seat belt legislation on the incidence of sternal fractures seen in the accident department. Br Med J (Clin Res Ed) 1985;291:785. doi: 10.1136/bmj.291.6498.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCarthy M. The benefit of seat belt legislation in the United Kingdom. J Epidemiol Community Health. 1989;43:218–22. doi: 10.1136/jech.43.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arajarvi E, Santavirta S, Tolonen J. Abdominal injuries sustained in severe traffic accidents by seatbelt wearers. J Trauma. 1987;27:393–7. doi: 10.1097/00005373-198704000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Carter PR, Maker VK. Changing paradigms of seat belt and air bag injuries: What we have learned in the past 3 decades. J Am Coll Surg. 2010:240–52. doi: 10.1016/j.jamcollsurg.2009.08.022. [DOI] [PubMed] [Google Scholar]
- 7.Abu-Zidan FM, Abbas AK, Hefny AF, Eid HO, Grivna M. Effects of seat belt usage on injury pattern and outcome of vehicle occupants after road traffic collisions: Prospective study. World J Surg. 2012;36:255–9. doi: 10.1007/s00268-011-1386-y. [DOI] [PubMed] [Google Scholar]
- 8.Slavin RE, Borzotta AP. The seromuscular tear and other intestinal lesions in the seatbelt syndrome: A clinical and pathologic study of 29 cases. Am J Forensic Med Pathol. 2002;23:214–22. doi: 10.1097/00000433-200209000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Siegel JH, Belwadi A, Smith JA, Shah C, Yang K. Analysis of the mechanism of lateral impact aortic isthmus disruption in real-life motor vehicle crashes using a computer-based finite element numeric model: With simulation of prevention strategies. J Trauma. 2010;68:1375–95. doi: 10.1097/TA.0b013e3181dcd42d. [DOI] [PubMed] [Google Scholar]
- 10.Greingor JL, Lazarus S. Chest and abdominal injuries caused by seat belt wearing. South Med J. 2006;99:534–5. doi: 10.1097/01.smj.0000216295.85100.ff. [DOI] [PubMed] [Google Scholar]
- 11.DiPerna CA, Rowe VL, Terramani TT, Salim A, Hood DB, Velmahos GC, et al. Clinical importance of the “seat belt sign” in blunt trauma to the neck. Am Surg. 2002;68:441–5. [PubMed] [Google Scholar]
- 12.Chandler CF, Lane JS, Waxman KS. Seatbelt sign following blunt trauma is associated with increased incidence of abdominal injury. Am Surg. 1997;63:885–8. [PubMed] [Google Scholar]
- 13.Velmahos GC, Tatevossian R, Demetriades D. The “seat belt mark” sign: A call for increased vigilance among physicians treating victims of motor vehicle accidents. Am Surg. 1999;65:181–5. [PubMed] [Google Scholar]
- 14.Weninger P, Hertz H. Factors influencing the injury pattern and injury severity after high speed motor vehicle accident — a retrospective study. Resuscitation. 2007;75:35–41. doi: 10.1016/j.resuscitation.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Eid HO, Abu-Zidan FM. Biomechanics of road traffic collision injuries: A clinician's perspective. Singapore Med J. 2007;48:693–700. [PubMed] [Google Scholar]
- 16.Dawson LK, Jenkins NH. Fatal intra-abdominal injury associated with incorrect use of a seat belt. J Accid Emerg Med. 1998;15:437–8. doi: 10.1136/emj.15.6.437-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kent R, Stacey S, Kindig M, Woods W, Evans J, Rouhana SW, et al. Biomechanical response of the pediatric abdomen, Part 2: Injuries and their correlation with engineering parameters. Stapp Car Crash J. 2008;52:135–66. doi: 10.4271/2008-22-0006. [DOI] [PubMed] [Google Scholar]
- 18.Kumaresan S, Sances A, Jr, Carlin F, Frieder R, Friedman K, Renfroe D. Biomechanics of side impact injuries: Evaluation of seat belt restraint system, occupant kinematics and injury potential. Conf Proc IEEE Eng Med Biol Soc. 2006;1:87–90. doi: 10.1109/IEMBS.2006.259384. [DOI] [PubMed] [Google Scholar]
- 19.Sokolove PE, Kuppermann H, Holmes JF. Association between the “seat belt sign” and intra-abdominal injury in children with blunt torso trauma. Acad Emerg Med. 2005;12:808–13. doi: 10.1197/j.aem.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 20.Santschi M, Echavé V, Laflamme S, McFadden N, Cyr C. Seat-belt injuries in children involved in motor vehicle crashes. Can J Surg. 2005;48:373–6. [PMC free article] [PubMed] [Google Scholar]
- 21.Achildi O, Betz RR, Grewal H. Lapbelt injuries and the seatbelt syndrome in pediatric spinal cord injury. J Spinal Cord Med. 2007;30:S21–4. doi: 10.1080/10790268.2007.11753964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown JK, Jing Y, Wang S, Ehrlich PF. Patterns of severe injury in pediatric car crash victims: Crash Injury Research Engineering Network database. J Pediatr Surg. 2006;41:362–7. doi: 10.1016/j.jpedsurg.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 23.Ehrlich PF, Brown JK, Sochor MR, Wang SC, Eichelberger ME. Factors influencing pediatric Injury Severity Score and Glasgow Coma Scale in pediatric automobile crashes: Results from the Crash Injury Research Engineering Network. J Pediatr Surg. 2006;41:1854–8. doi: 10.1016/j.jpedsurg.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 24.Keshavarz R, Patel R, Bachar R, Laddis D. Children in taxis: An opportunity for pediatricians and emergency physicians to save lives? Pediatr Emerg Care. 2006;22:704–9. doi: 10.1097/01.pec.0000238742.96606.20. [DOI] [PubMed] [Google Scholar]
- 25.Arbogast KB, Chen I, Nance ML, Durbin DR, Winston FK. Predictors of pediatric abdominal injury risk. Stapp Car Crash J. 2004;48:479–94. doi: 10.4271/2004-22-0021. [DOI] [PubMed] [Google Scholar]
- 26.Fakhry SM, Brownstein M, Watts DD, Baker CC, Oller D. Relatively short diagnostic delays (>8 hours) produce morbidity and mortality in blunt small bowel injury: An analysis of time to operative intervention in 198 patients from a multicenter experience. J Trauma. 2000;48:408–14. doi: 10.1097/00005373-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Nordhoff LS. 2nd ed. Boston, USA: Jones & Bartlett Learning; 2005. Motor Vehicle Collision Injuries: Biomechanics, Diagnosis, and Management. [Google Scholar]


