Abstract
The development of intramural intestinal gas may indicate a serious postoperative complication and therefore any radiological indication of such “pneumatosis intestinalis” (PI) in an unwell patient after surgery should put the clinical team on high-alert. However immediate recourse to relook laparotomy may not be always necessary and, further, in some cases may possibly accelerate the deterioration especially if it proves to be non-therapeutic. Careful and close clinical monitoring, as is described in this clinical report, may allow discriminative identification of those in whom this finding is in fact transient and therefore benign and who therefore can be successfully treated without operative re-intervention. We describe the presenting features and background scenario of PI early after laparoscopic total colectomy for medically refractory, severe ulcerative colitis and detail the critical postoperative decision pivots.
Keywords: Pneumatosis intestinalis, Laparoscopic total colectomy, Ulcerative colitis, Severe acute colitis, Portal venous gas
Core tip: The successful outcome of our patients with postoperative pneumatosis intestinalis (PI) indicates that a very individualized, nuanced management plan can allow a succesful course with conservative management. At all times it should be remembered that PI developing postoperatively is a radiographic sign rather than a specific diagnosis. It should be a factor in the decision-analysis related to clinical care and not the sole arbitrator.
INTRODUCTION
“Pneumatosis intestinalis” (PI) is the presence of extraluminal gas within the bowel wall[1]. In a symptomatic postoperative patient such a finding on plain radiology or computerized tomography (CT) is often viewed as a signal of impending or actual acute mesenteric ischaemia especially when associated with portal venous gas (PVG)[2]. Therefore many advocate immediate exploratory laparotomy due to associated high mortality rates. Here, we present two patients who developed PI (one with PVG) in association with abdominal pain and clinical signs early after laparoscopic total colectomy for acute severe ulcerative colitis but who were managed conservatively with prompt complete recovery.
CASE REPORT
Case one
A 22-year-old male known to have medically (steroid and biologic therapy) refractory ulcerative colitis (UC) was admitted with an acute exacerbation (10-15 bloody bowel movements daily for the previous 8 d). Interestingly, he had also micrognathia with several prior jaw reconstruction procedures and had both a tracheostomy and gastrostomy feeding tube. Laboratory investigations on admission showed leucocytosis [white blood cell (WBC) count = 12.29 × 10-9/L] and an elevated C-reactive protein (CRP) level of 27 mg/L and normal haemoglobin (Hb, 13.8 g/dL) and albumin (32 g/L) levels. Plain abdominal X-ray on admission showed a loss of tone and haustra of the descending and sigmoid colon (Figure 1) but no megacolon. He underwent urgent multiport laparoscopic total colectomy with end ileostomy formation without intra-operative complication within the first 48 h of admission.
Figure 1.
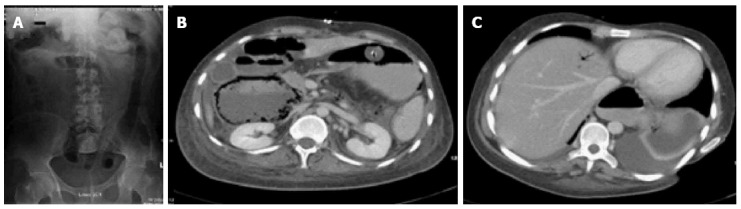
Radiology of case one. (A) Preoperative plain film of abdomen showing no pneumatosis intestinalis in comparison to (B) postoperative computerized tomogram showing extensive intramural gas and (C) portal venous gas.
While our patient was well for the first 24 h postoperatively (including stoma function), he then developed generalized abdominal pain associated with absence of stoma function, pallor, tachycardia (120 beats per minute) and hypotension (90/60 mmHg). On examination, his abdomen was soft without tenderness to palpation. An urgent CT scan of his abdomen with intravenous and oral contrast showed dilated small bowel loops with PI, associated gas within the portal venous system and a right-sided portal venous thrombus (also Figure 1). Clinical examination was unchanged after the scan and the patient symptomatically was improved. We therefore opted to closely observe and support him medically (including commencement of Total Parenteral Nutrition (TPN) and empiric antibiotic therapy to cover any possible bacterial translocation) along with therapeutic low molecular weight heparin anticoagulation. Over the next 24 h his symptoms settled fully and his ileostomy resumed functioning. He was discharged home 9 d later on oral anticoagulation. At review 3 mo post-operatively, he was well with a repeat CT abdomen showing significant interval resolution of his PI and PVG. The portal vein thrombus was still present but non- occlusive. He remains well now 18 mo after his surgery.
Case two
A 33-year-old woman presented acutely with an acute exacerbation of her known UC despite prior steroid and infliximab therapy. Her WCC and CRP levels were elevated (12.29 × 10-9/L and 57 mg/L respectively) and she was both anaemic (10.7 g/dL) and hypoalbuminemia (27 g/L). She underwent single port laparoscopic total colectomy with end ileostomy on an urgent basis and convalesced normally for the first three postoperative days. She then developed abdominal pain and tachycardia but without abdominal tenderness. An urgent CT scan showed PI (Figure 2) but no portal venous gas. Again her symptoms and signs showed no progression and she settled with active, careful observation in addition to assiduous rehydration and empiric antibiotic therapy. Although she was discharged home on day 8 postoperatively, she was readmitted with fever and abdominal pain secondary to an intra-abdominal abscess (seen on repeat CT without any associated PI) that was drained radiologically. She made an excellent recovery thereafter and thereafter underwent laparoscopic proctectomy with ileoanal J-pouch construction twelve months after her colectomy. She is now six months post-reversal of her defunctioning loop ileostomy and her quality of life and pouch function are both excellent.
Figure 2.
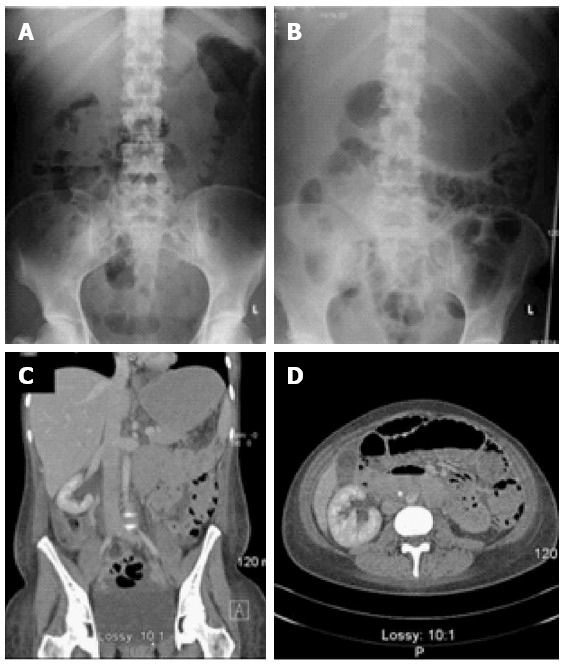
Radiology of case two. (A) and (B) comparative pre and postoperative plain radiology showing new and extensive intramural gas in the latter; C and D: Axial computerized tomograms taken on the 8th postoperative day showing marked pneumatosis intestinalis.
DISCUSSION
Much prior experience has indicated that the finding of PI (most especially in association with PVG[3]) on postoperative imaging in an unwell patient is an ominous sign that should trigger re-exploratory surgery, likely laparotomy[4,5]. However, in other settings, PI is known to have a benign course and the same appearances can be seen in association with steroid or chemotherapy usage, trauma and inflammatory conditions[6]. Furthermore, there have been reports of resolution of PI with hyperbaric oxygen therapy[7]. The clinical spectrum of PI in this way is therefore already known to range from asymptomatic to life threatening course[8]. While surgery is of course necessary in situations of bowel strangulation, frank gangrene or perforation, injudicious take-back may be non-therapeutic (the affected loop of bowel may not even be macroscopically abnormal) and in fact risk precipitating promulgation of the underlying inflammatory/thrombotic cascade mitigating towards poor outcome. While increasing use of CT imaging has led to quicker and earlier detection[9], the increasing sophistication of this modality includes greater sensitivity for non-critical findings. Management decisions should therefore be based on a combination of both radiological and laboratory findings[10] but clinical examination (repeated frequently) and judgment is paramount.
While the PI identified in both patients in this report was shown to be transient (it had resolved completely on follow-up imaging) potentially it was present prior to the operative procedure (neither had preoperative CT imaging). Certainly too the portal venous thrombosis seen in case one may have been present preoperatively as both it and PI share as risk factors many of the concomitants associated with acute colitis (namely dehydration, systemic inflammatory syndrome, immobility, steroid therapy). Colitic patients may also have an increased hereditary tendency to thrombosis[11]. Nonetheless positive intra-abdominal pressure at laparoscopy may certainly have had an additive effect and it seems more likely that the operation indeed triggered the clinical course and radiological findings.
Experiential reports on postoperative PI in symptomatic patients remain very limited. Until there is greater data on the specific incidence and an improved understanding aetiology on the conservative management of such patients, we agree that a radiological indicator of PI should put the clinical team on high-alert. However the successful outcome of our patients with a conservative course in conjunction with poor outcomes occasionally seen in those undergoing early operative intervention indicates that a very individualized, nuanced management plan is then required in order to ensure therapeutic opportunities are maximized.
COMMENTS
Case characteristics
Two unwell patients with pneumatosis intestinalis found on radiological examination early after laparoscopic total colectomy for acute severe and medically refractory colitis.
Clinical diagnosis
Acute deterioration early after surgery indicating radiological investigation that showed intramural intestinal gas or “pneumatosis intestinalis” as a new finding.
Differential diagnosis
Ischaemic bowel secondary to a strangulated internal hernia, intra abdominal abscess, ileus with pneumatosis as a transient, benign co-finding.
Laboratory diagnosis
Acute inflammatory response syndrome.
Imaging diagnosis
Pneumatosis intestinalis (including one patient with portal venous gas) very concerning for grave intra-abdominal complication.
Pathological diagnosis
Benign, self-limiting complication that settled with intensive clinical observation without the need for operative re-intervention.
Treatment
Close clinical observation along with rehydration, bowel rest, analgesia and antibiotic therapy.
Related reports
Very often the concern that pneumatosis intestinalis represents ischaemic bowel means that some authors advocate immediate laparotomy even though some have then found essentially normal intraperitoneal appearances and the patients clinical deterioration continues thereafter.
Term explanation
Pneumatosis intestinalis-the presence of intramural gas within the intestine.
Experience and lessons
Careful clinical care and consideration can allow successful management without operative re-intervention of this very worrying radiological finding.
Peer review
Two interesting cases regarding symptomatic pneumatosis intestinalis post laparoscopic surgery.
Footnotes
P- Reviewer: Ahluwalia NK, El-Tawil AM, Myrelid P, Schofield JB S- Editor: Ji FF L- Editor: A E- Editor: Zhang DN
References
- 1.Azzaroli F, Turco L, Ceroni L, Galloni SS, Buonfiglioli F, Calvanese C, Mazzella G. Pneumatosis cystoides intestinalis. World J Gastroenterol. 2011;17:4932–4936. doi: 10.3748/wjg.v17.i44.4932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.See C, Elliott D. Images in clinical medicine. Pneumatosis intestinalis and portal venous gas. N Engl J Med. 2004;350:e3. doi: 10.1056/ENEJMicm020289. [DOI] [PubMed] [Google Scholar]
- 3.Ito M, Horiguchi A, Miyakawa S. Pneumatosis intestinalis and hepatic portal venous gas. J Hepatobiliary Pancreat Surg. 2008;15:334–337. doi: 10.1007/s00534-007-1246-1. [DOI] [PubMed] [Google Scholar]
- 4.Nelson AL, Millington TM, Sahani D, Chung RT, Bauer C, Hertl M, Warshaw AL, Conrad C. Hepatic portal venous gas: the ABCs of management. Arch Surg. 2009;144:575–581; discussion 581. doi: 10.1001/archsurg.2009.88. [DOI] [PubMed] [Google Scholar]
- 5.Patel NM. Hepatic Portal Venous Gas with Pneumatosis Intestinalis. Gastroenterol Res. 2009;2:51–53. doi: 10.4021/gr2009.01.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wiesner W, Mortelé KJ, Glickman JN, Ji H, Ros PR. Pneumatosis intestinalis and portomesenteric venous gas in intestinal ischemia: correlation of CT findings with severity of ischemia and clinical outcome. AJR Am J Roentgenol. 2001;177:1319–1323. doi: 10.2214/ajr.177.6.1771319. [DOI] [PubMed] [Google Scholar]
- 7.Togawa S, Yamami N, Nakayama H, Shibayama M, Mano Y. Evaluation of HBO2 therapy in pneumatosis cystoides intestinalis. Undersea Hyperb Med. 2004;31:387–393. [PubMed] [Google Scholar]
- 8.Mallappa S, Warren OJ, Kantor R, Mohsen Y, Harris S. Pneumatosis intestinalis and hepatic portal venous gas on computed tomography - a non-lethal outcome. JRSM Short Rep. 2011;2:88. doi: 10.1258/shorts.2011.011081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knechtle SJ, Davidoff AM, Rice RP. Pneumatosis intestinalis. Surgical management and clinical outcome. Ann Surg. 1990;212:160–165. doi: 10.1097/00000658-199008000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wayne E, Ough M, Wu A, Liao J, Andresen KJ, Kuehn D, Wilkinson N. Management algorithm for pneumatosis intestinalis and portal venous gas: treatment and outcome of 88 consecutive cases. J Gastrointest Surg. 2010;14:437–448. doi: 10.1007/s11605-009-1143-9. [DOI] [PubMed] [Google Scholar]
- 11.O’Connor OJ, Cahill RA, Kirwan WO, Redmond HP. The incidence of postoperative venous thrombosis among patients with ulcerative colitis. Ir J Med Sci. 2005;174:20–22. doi: 10.1007/BF03169142. [DOI] [PubMed] [Google Scholar]


