Abstract
Objective:
To study the efficacy of oral carvedilol in acute treatment of atrial fibrillation (AF) with fast ventricular rate.
Materials and Methods:
In an open-label, single-arm trial, oral carvedilol was administered to 35 patients of AF in escalating doses from 3.125 mg o.d. to 12.5 mg b.i.d.
Results:
A successful result was seen in 25 patients (71.4%) with 4 converting to sinus rhythm, rate control to less than 90 bpm in 16 and a 20% rate reduction in 5 patients. Two patients developed hypotension needing withdrawal of the drug.
Conclusion:
Escalating doses of oral carvedilol can be effectively and safely used in the acute treatment of AF with fast ventricular rate.
Keywords: Acute treatment, atrial fibrillation, carvedilol, oral tablet, rate control
INTRODUCTION
Atrial fibrillation (AF) is the most common sustained arrhythmia whose prevalence and incidence have been shown to be increasing in the past two decades.[1] The global burden of AF was estimated to be about 33.5 million in 2010[1] and it has been christened as the epidemic of the new millennium.[2] Though data in India are scarce, the PANARM study suggested that AF is the most common arrhythmia (66% of all arrhythmias) seen by clinicians;[3] the average age of the Indian AF patient is a decade younger than their Western counterpart[3] and Rheumatic valvular heart disease is the most common cause here.[4]
Studies like AFFIRM and RACE, and other long-term follow-up studies too concluded that, in the treatment of AF, rate control was not inferior to a rhythm control strategy;[5,6,7,8] their patients were however elderly and non-rheumatic. The CRRAFT study, conducted in the Indian context, showed that after 1 year, those who were in sinus rhythm had lesser mortality, and, improved NYHA class and exercise tolerance.[9] Though newer drugs like dronedarone and vernakalant have provided additional opportunities for rhythm control,[10] rate reduction continues to be the major treatment modality offered to patients with AF with the use of beta blockers almost doubling from 20% to 43% in America in the past decade.[11] The aim of the present study was to assess the efficacy of escalating doses of oral carvedilol in the acute management of patients with AF with fast ventricular rate (FVR).
MATERIALS AND METHODS
This was an open-label single-arm trial (Clinical Trial Registration No. REF/2014/06/007054) of escalating doses of oral carvedilol in 35 patients of AF with FVR, admitted to the Cardiology Ward of King George Hospital, Visakhapatnam, who fulfilled the inclusion criteria and who were willing to participate in the study were included in the study. Inclusion criteria included age above 18 years and documented history of AF for at least 1 week and with a ventricular rate of 100/min or above on the ECG. Patients were excluded if they were pregnant/lactating women, or had a systolic blood pressure (SBP) less than 100 mm Hg. Those with history of bradyarrhythmia, bronchial asthma or drug allergy were excluded as were those who were in NYHA Class IV on admission. Patients on digoxin were permitted to enroll but those on other antiarrhythmics like beta blockers, calcium channel blockers and amiodarone were excluded. Consent was obtained from all patients before administering the drug.
History was obtained and clinical examination and routine investigations were done including ECG and echocardiogram. A long strip of ECG in LII and V1, for at least 12 seconds each, was taken to calculate the ventricular rate. The ventricular rate was calculated as the number of QRS complexes in a 10 second strip multiplied by 6. The rates in the two strips were averaged to obtain the ventricular rate. An ECG was repeated after 1 hour to confirm FVR.
Oral carvedilol was administered, in daily escalating doses, to patients as per the following schedule till an end point was reached - 3.125 mg once daily on Day 1, to 3.125 mg b.i.d. on Day 2 to 6.25 mg b.i.d. to 9.375 mg b.i.d. to a maximum dose of 12.5 mg b.i.d. on Day 5.
End points included conversion to sinus rhythm or a ventricular rate of 90 bpm or below at rest or a dose of 12.5 mg b.i.d. Patients were withdrawn from the study if they developed adverse effects like hypotension (SBP below 90 mm Hg) or increasing dyspnea or pulmonary crepitations or ronchi, or when the treating doctor deemed it necessary. Patients whose ventricular rate reduced by 20% of baseline rate but still above 90 bpm were permitted to continue to the next dose if the treating doctor thought further reduction in rate was necessary.
Patients were monitored in the ICU for their pulse, BP, lung function and ECG. ECG was obtained every half an hour for the first two patients and it was noted that the maximum effect of oral carvedilol on ventricular rate reduction was observed after about 4-6 hours. Then onwards, a long strip of ECG was recorded for patients 6 hours after each dose.
A successful result was defined as -
Conversion to sinus rhythm
Reduction in ventricular rate to 90 bpm or below
Reduction in ventricular rate of 20% or above, compared to baseline rate
The result was defined as failure if the fall in ventricular rate is less than 20% compared to the baseline rate.
Student's t-test was used to compare means and a P < 0.05 was taken as significant.
RESULTS
There were 35 patients (18 males and 17 females) in the age range of 20-86 years (median = 33 years).
Causes of AF in the group included rheumatic mitral valve disease which was the most common etiology in 22 (62.9%), hypertensive heart disease in 5 (14.3%), dilated cardiomyopathy in 3 (8.6%) and ischemic heart disease in 2 (5.7%). Three patients had lone AF.
Most of the patients (29/35 = 82.9%) were in NYHA Class II while 6 (17.1%) were in Class III. Initial ventricular rate ranged from 111 to 195 with a mean rate of 144.8 beats per minute. Eleven patients were on digoxin therapy.
At the end of the study, the outcome of the patients was as follows -
The rhythm was converted to sinus rhythm in 4 patients (11.4%). (Rhythm Control)
The rate was reduced to <90 bpm in patients (45.7%). (Rate Control)
The rate was reduced by >20% of baseline rate, though the final rate was >90 bpm in 5 patients (14.3%).(Rate Reduction)
The rate reduction was <20% in 10 patients (failure) (28.6%).(Drug Failure).
Thus, a successful result (a, b, c above) was obtained in 25/35 patients (71.4%). Of the four patients who converted to sinus rhythm, two had lone AF, one had hypertensive heart disease and one had rheumatic mitral valve disease.
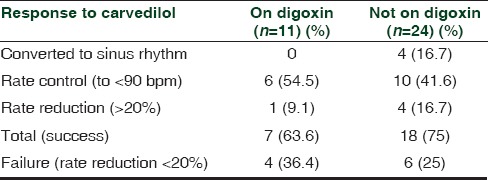
When patients on digoxin and those not on digoxin were analyzed for the effect of carvedilol, the results were not significantly different [Table 1].
Table 1.
Response of patients with atrial fibrillation to oral carvedilol among those on digoxin and those not on digoxin
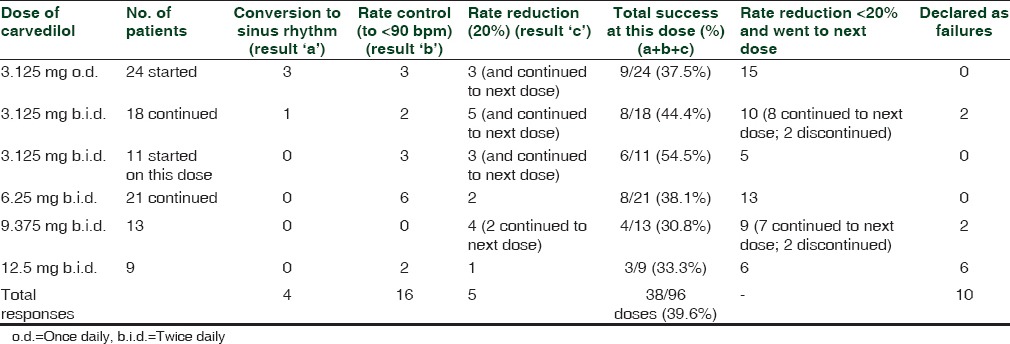
The dose of carvedilol administered ranged from 3.125 mg o.d. to 12.5 mg b.i.d. 24 patients were started on 3.125 mg o.d. and 11 on 3.125 mg b.i.d. The response depending on the dose of carvedilol was as follows [Table 2]. Thus, rate control was achieved in most number of patients (six patients) at a dose of 6.125 mg b.i.d. of carvedilol. The success rate (conversion + rate control + rate reduction) for any given dose of carvedilol ranged from 30.8% to 54.5% with a mean success rate of 39.6%.
Table 2.
Response of patients with atrial fibrillation to escalating doses of oral carvedilol
Hypotension developed in two patients at a dose of 3.125 mg BID and were discontinued from the study while two patients opted out of the study at a dose of 9.375 mg bid, all four were counted as failures. Other adverse effects noted were pulmonary ronchi in one patient and pulmonary rales in another patient. One patient developed nocturnal cough. None of the patients however had symptoms of increasing heart failure requiring withdrawal of carvedilol or dose reduction.
DISCUSSION
Rate control and rhythm conversion are two options in the treatment of AF besides the more important task of stroke prevention by anticoagulation. Several studies showed that rate control is inferior to rhythm conversion.[5,6,7,8] It has been suggested that rhythm control can be the first line option in symptomatic patients without advanced structural cardiac disease or significant left atrial enlargement[12] as these render long-term maintenance of sinus rhythm more challenging. This becomes relevant in the Indian context where rheumatic valvular heart disease is the most common cause of AF.[3] The present study population was similar with 62.9% (22/35) having rheumatic mitral valve disease. The median age of the group was 33 years unlike the Western population where the average age is a decade older than their Indian counterpart.[2]
Draft guidelines issued by the NICE group recommend that rate control should be offered as the first line strategy to all people with AF; they recommend rhythm control to those patients whose AF, has a reversible cause, is of new onset AF, or is primarily responsible for heart failure in them.[13] The 2014 AHA/ACC/HRS atrial fibrillation guidelines recommend control of ventricular rate using a beta blocker or nondihyrdopyridine calcium channel antagonist for patients with paroxysmal, persistent or permanent AF.[14] Beta blockers are one of the most frequently used drugs acutely and chronically in AF and are believed to lead to improvement in symptoms and well-being[15] though a recent meta-analysis contests this by concluding that, the effect of beta blockers on outcome in systolic HF patients with AF is less than those in sinus rhythm; the analysis found no benefit in terms of reduction in mortality or hospitalization while such benefit was seen in those in sinus rhythm (OR of about 0.6).[16] Analysis of the AFFIRM study data revealed that beta blockers were more successful than calcium channel blockers in achieving rate control (70% vs 54%) either used alone or with digoxin.[17]
A strict rate control may not be necessary to aim for, among patients with AF with FVR; a lenient rate control (to <110 bpm at rest) has been shown to be as effective as strict rate control (to <80 bpm at rest) and easier to achieve, among 97% vs. 67%.[18] A rate control algorithm for patients with AF recommends a target resting heart rate to <100 bpm using beta blocker - digoxin if there is heart failure, beta blocker/verapamil/diltiazem if there is coronary artery disease, or any one or combination of these three in those without heart disease or hypertension.[19] Calcium blockers are contraindicated in most patients with significant LV systolic dysfunction[20] but can be used in those with heart failure with preserved ejection fraction.[21] Many patients of persistent AF are on digoxin therapy and amiodarone and verapamil are known to increase digoxin levels; diltiazem too has been reported to cause fatalities in patients already on digoxin.[22]
Intravenous drugs have been favored for rate control in the acute setting with conversion to oral agents for long-term maintenance, and digitalis not widely used, due to its slower onset of action compared to beta blockers and calcium antagonists.[20] On the other hand, a comment on the 2014 AF management guidelines states that “unless immediate rate control is required or an enteral route of administration is not available, oral administration is appropriate.[21]
Oral drugs such as clonidine, captopril and labetalol have been used in acute treatment protocols such as hypertensive urgencies[23,24,25] and their time to onset of action is reported as 30 to 60 minutes. Carvedilol is a newer beta blocker used as an anti-hypertensive drug and a drug for heart failure.[26] It competitively inhibits beta-1, beta-2 and alpha-1 receptors (mildly more selective for beta 1 receptors) with its antihypertensive effect starting with a single dose of 3.125 mg; the hypotensive effect begins at 30 min after oral administration; peak concentrations occur 1-2 hours after administration and elimination half-life is 2-8 hours.[27] Changes in digoxin levels are minor and there is no need for dose adjustment of digoxin. Beta blockers have a class effect on rate control in AF through their blocking action on the atrioventricular node besides also having some role in prevention, reversion to sinus rhythm and maintaining sinus rhythm after it is restored.[28] Propranolol, atenolol, metoprolol and esmolol can be given intravenously for acute rate control in AF but the IV route is not recommended in heart failure (HF) (ibid).
There are few studies of carvedilol in AF and they have studied the effect of carvedilol in chronic AF for its rate reduction effect.[29] A study in 13 patients with chronic AF found that the mean ventricular rate decreased from 101.9 to 85.2 with one patient discontinuing the drug due to congestive heart failure.[29] In another study of 14 patients of dilated cardiomyopathy and AF and HF, carvedilol was shown to have improved rate control of 10-36% besides better exercise time.[30] A third study in 47 patients with persistent AF and HF (mean left ventricle ejection fraction (LVEF) of 24%) revealed that the combination of carvedilol and digoxin is superior to either drug alone in terms of rate control and LVEF.[31]
With this background, the present study was undertaken and it has shown that oral carvedilol in escalating doses can effectively reduce the ventricular rate in patients with AF with a success rate of over 70%. We have measured the success of carvedilol in terms of the proportion of patients, who had rhythm conversion or rate control or a 20% rate reduction, rather than just fall in mean ventricular rate. The former is more applicable to the real world situation where we are concerned with effects in an individual rather than overall mean fall in ventricular rate. The 71.4% success rate in the present study is similar to results of many such studies of acute rate control in AF with other drugs. In a postoperative setting including 121 patients of AF with FVR, IV diltiazem achieved stable rate control in 76% patients and IV metoprolol in 53%.[32] Though IV diltiazem and metoprolol lead to rate reduction rapidly - in 90% and 80% respectively by 20 minutes in one study[33] and IV diltiazem took a median of just 4.3 minutes in a study for rate reduction[34] - their negative inotropic effect, especially calcium channel blockers, precludes their routine use when AF is associated with significant HF or LV dysfunction. Moreover, in a recent study in 150 patients of AF with rapid ventricular rate (>120/min), the median time to achieve ventricular rate control was 3 hours with diltiazem compared to 7 hours with amiodarone and 6 hours with digoxin.[35] A tailored dosing regimen of amiodarone too took a mean of 6 hours for the rate to decrease and stabilize at 96/min.[36]
Oral drugs have been tried in very few studies for acute rate control in AF. In one study, clonidine in two doses of 75 mcg orally, 2 hours apart, in recent onset AF, led to rate reduction in eight of nine patients with six of them reverting to sinus rhythm.[37] Another comparative study in AF found that oral clonidine led to a reduction in mean heart rate by 44.4 beats per minute, compared to 52 beats with IV digoxin and 41.8 beats with IV verapamil; the authors concluded that (oral) clonidine is comparable to standard agents.[38] In another study with oral gallopamil, a calcium antagonist, there was a significant rate reduction in 10 of 20 patients, with the maximum decrease in heart rate seen 2-4 hours after administration.[39]
In the present study, leaving aside the simple rate reduction of 20%, the first dose of 3.125 mg of carvedilol produced a successful result of rhythm conversion or rate control in 17.1% (6 patients) while the second and third day doses too gave a similar successful result (17.1% each i.e. 6 patients). Thus, most of those who responded successfully to oral carvedilol did so by a dose of 6.25 mg BID (51.4%); beyond that, further successful results were not as many. Thus, oral carvedilol in escalating doses gives a satisfactory response in terms of rate control at an acceptable speed. The reason for lack of a uniform response among all patients may be genetically linked because a recent study has shown that a common beta-1 receptor polymorphism (Gly389 variant vs. Arg389 variant) predicts a more favorable rate reduction response to beta blockers in AF.[40]
Another notable finding in the present study was that only two patients (5.7%) had adverse effects (hypotension in both) necessitating cessation of drug administration and withdrawal of the patient from the study. Other side effects noted were ronchi, rales and nocturnal cough but all of these patients could tolerate and continue their carvedilol doses. None had exacerbation of heart failure necessitating drug withdrawal.
A limitation of the present study is the small size and that it was an open-label, single-arm (non-placebo controlled) study. But because the outcome was measured by an objective method of ECG, in which the heart (ventricular) rate was calculated, there was no need for blinding, nor was there scope for bias. Placebo was not used due to ethical considerations.
CONCLUSION
The overall success rate of oral carvedilol in atrial fibrillation in the present study was 71.4% including conversion to sinus rhythm and rate control/reduction with just a 5.7% incidence of adverse reactions requiring drug withdrawal. Thus, we can conclude that oral carvedilol, in escalating doses, is a reasonably safe and effective drug for the acute or semi-emergent management of patients with atrial fibrillation and fast ventricular rate and who are hemodynamically stable.
ACKNOWLEDGEMENTS
Dr. G. Sai Gopal, former Professor and Head, Department of Cardiology, Andhra Medical College, under whose guidance the study was conducted.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation: A Global Burden of Disease 2010 study. Circulation. 2014;129:837–47. doi: 10.1161/CIRCULATIONAHA.113.005119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ezekowitz MD. Atrial fibrillation: The epidemic of the new millennium. Ann Intern Med. 1999;131:537–8. doi: 10.7326/0003-4819-131-7-199910050-00011. [DOI] [PubMed] [Google Scholar]
- 3.Deore R, Vora A. Epidemiology and risk factor for atrial fibrillation in India. J Preventive Cardiol. 2014;3:505–8. [Google Scholar]
- 4.Vora A. Approach to management of atrial fibrillation in the Indian scenario. J Assoc Physicians India. 2007;(Suppl 55):30–2. [PubMed] [Google Scholar]
- 5.Wyse DG, Waldo AL, DiMarco JP, Domanski MJ, Rosenberg Y, Schron EB, et al. Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) Investigators. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347:1825–33. doi: 10.1056/NEJMoa021328. [DOI] [PubMed] [Google Scholar]
- 6.Van Gelder IC, Hagens VE, Bosker HA, Kingma JH, Kamp O, Kingma T, et al. Rate Control versus Electrical Cardioversion for Persistent Atrial Fibrillation Study Group. A comparison of rate control and rhythm control in patients with recurrent persistent atrial fibrillation. N Engl J Med. 2002;347:1834–40. doi: 10.1056/NEJMoa021375. [DOI] [PubMed] [Google Scholar]
- 7.Kosior DA, Opolski G, Torbicki A. Rhythm or rate control for persistent atrial fibrillation: Results of long term follow-up of the hot café study population. J Am Coll Cardiol. 2012;59:E617. [Google Scholar]
- 8.Ionescu-Ittu R, Abrahamowicz M, Jackevicius CA, Essebag V, Eisenberg MJ, Wynant W, et al. Comparative effectiveness of rhythm control vs. rate control drug treatment effect on mortality in patients with atrial fibrillation. Arch Intern Med. 2012;172:997–1004. doi: 10.1001/archinternmed.2012.2266. [DOI] [PubMed] [Google Scholar]
- 9.Vora A, Karnad D, Goyal V, Naik A, Gupta A, Lokhandwala Y, et al. Control of rate versus rhythm in rheumatic atrial fibrillation: A randomized study. Indian Heart J. 2004;56:110–6. [PubMed] [Google Scholar]
- 10.Lip GY, Tse HF, Lane DA. Atrial fibrillation. Lancet. 2012;379:648–61. doi: 10.1016/S0140-6736(11)61514-6. [DOI] [PubMed] [Google Scholar]
- 11.Desai AM, Cavanaugh TM, Desai VC, Heaton PC, Kelton CM. Trends in the outpatient treatment of atrial fibrillation in the USA from 2001 to 2010. Pharmacoepidemiol Drug Saf. 2014;23:539–47. doi: 10.1002/pds.3605. [DOI] [PubMed] [Google Scholar]
- 12.Amerena JV, Walters TE, Mirzaee S, Kalman JM. Update on the management of atrial fibrillation. Med J Aust. 2013;199:592–7. doi: 10.5694/mja13.10191. [DOI] [PubMed] [Google Scholar]
- 13.Atrial Fibrillation: The Management of Atrial Fibrillation. NICE Guidelines. Draft. [Last accessed on 2014 Jul 03]. Available from: http://www.nice.org.uk/nicemedia/live/13590/66265/66265.pdf .
- 14.January CT, Wann LS, Alpert JS, Calkins H, Cleveland JC, Jr, Cigarroa JE, et al. 2014 AHA/ACC/HRS Guideline for the management of patients with atrial fibrillation: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014 doi: 10.1016/j.jacc.2014.03.022. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 15.Dorian P, Angaran P. ß-blockers and atrial fibrillation: Hypertension and other medical conditions influencing their use. Can J Cardiol. 2014;30(Suppl 5):S38–41. doi: 10.1016/j.cjca.2013.09.029. [DOI] [PubMed] [Google Scholar]
- 16.Rienstra M, Damman K, Mulder BA, Van Gelder IC, McMurray JJ, Van Veldhuisen DJ. Beta-blockers and outcome in heart failure and atrial fibrillation: A meta-analysis. JACC Heart Fail. 2013;1:21–8. doi: 10.1016/j.jchf.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 17.Olshansky B, Rosenfeld LE, Warner AL, Solomon AJ, O’Neill G, Sharma A, et al. AFFIRM Investigators. The Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) study: Approaches to control rate in atrial fibrillation. J Am Coll Cardiol. 2004;43:1201–8. doi: 10.1016/j.jacc.2003.11.032. [DOI] [PubMed] [Google Scholar]
- 18.Van Gelder IC, Groenveld HF, Crijns HJ, Tuininga YS, Tijssen JG, Alings AM, et al. RACE II Investigators. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362:1363–73. doi: 10.1056/NEJMoa1001337. [DOI] [PubMed] [Google Scholar]
- 19.Frankel G, Kamrul R, Kosar L, Jensen B. Rate versus rhythm control in atrial fibrillation. Can Fam Physician. 2013;59:161–8. [PMC free article] [PubMed] [Google Scholar]
- 20.Heist EK, Mansour M, Ruskin JN. Rate control in atrial fibrillation: Targets, methods, resynchronization considerations. Circulation. 2011;124:2746–55. doi: 10.1161/CIRCULATIONAHA.111.019919. [DOI] [PubMed] [Google Scholar]
- 21.Mandrola J. 2014 Atrial Fibrillation Treatment Guidelines: Ten things to like and only one to dislike. Medscape. 2014. http://www.medscape.com/viewarticle/822815#2 .
- 22.Moser LR, Panacek EA, Munger MA. Fatality due to intravenous diltiazem for acute ventricular rate control. Pharmacotherapy. 1996;16:306–10. [PubMed] [Google Scholar]
- 23.Souza LM, Riera R, Saconato H, Demathé A, Atallah AN. Oral drugs for hypertensive urgencies: Systematic review and meta-analysis. Sau Paulo Med J. 2009;127:366–72. doi: 10.1590/S1516-31802009000600009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Houston MC. Treatment of hypertensive emergencies and urgencies with oral clonidine loading and tirtration. A review. Arch Intern Med. 1986;146:586–9. [PubMed] [Google Scholar]
- 25.De A, Bala N. Drug treatment for hypertensive emergencies. Int J Res Pharm Biomed Sci. 2011;2:482–91. [Google Scholar]
- 26.Frishman WH. Carvedilol. N Engl J Med. 1998;339:1759–65. doi: 10.1056/NEJM199812103392407. [DOI] [PubMed] [Google Scholar]
- 27.Dunn CJ, Lea AP, Wagstaff AJ. Carvedilol. A reappraisal of its pharmacological properties and therapeutic use in cardiovascular disorders. Drugs. 1997;54:161–85. doi: 10.2165/00003495-199754010-00015. [DOI] [PubMed] [Google Scholar]
- 28.López-Sendón J, Swedberg K, McMurray J, Tamargo J, Maggioni AP, Dargie H, et al. Task ForceOn Beta-Blockers of the European Society of Cardiology. Expert consensus document on beta-adrenergic receptor blockers. Eur Heart J. 2004;25:1341–62. doi: 10.1016/j.ehj.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 29.Kodani E, Matsumoto S, Igawa O, Kusama Y, Atarashi H. Effect of carvedilol on reduction in heart rate in patients with chronic atrial fibrillation. J Clin Med Res. 2013;5:451–9. doi: 10.4021/jocmr1581w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Agarwal AK, Venugopalan P. Beneficial effect of carvedilol on heart rate response to exercise in digitalised patients with heart failure in atrial fibrillation due to idiopathic dilated cardiomyopathy. Eur J Heart Fail. 2001;3:437–40. doi: 10.1016/s1388-9842(01)00130-1. [DOI] [PubMed] [Google Scholar]
- 31.Khand AU, Rankin AC, Martin W, Taylor J, Gemmell I, Cleland JG. Carvedilol alone or in combination with digoxin for the management of atrial fibrillation in patients with heart failure? J Am Coll Cardiol. 2003;42:1944–51. doi: 10.1016/j.jacc.2003.07.020. [DOI] [PubMed] [Google Scholar]
- 32.Personett HA, Smoot DL, Stollings JL, Sawyer M, Oyen LJ. Intravenous metoprolol versus diltiazem for rate control in noncardiac, nonthoracic postoperative atrial fibrillation. Ann Pharmacother. 2014;48:314–9. doi: 10.1177/1060028013512473. [DOI] [PubMed] [Google Scholar]
- 33.Demircan C, Cikriklar HI, Engindeniz Z, Cebicci H, Atar N, Guler V, et al. Comparison of the effectiveness of intravenous diltiazem and metoprolol in the management of rapid ventricular rate in atrial fibrillation. Emerg Med J. 2005;22:411–4. doi: 10.1136/emj.2003.012047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salerno DM, Dias VC, Kleiger RE, Tschida VH, Sung RJ, Sami M, et al. Efficacy and safety of intravenous diltiazem for treatment of atrial fibrillation and atrial flutter. The Diltiazem-Atrial Fibrillation/Flutter Study Group. Am J Cardiol. 1989;63:1046–51. doi: 10.1016/0002-9149(89)90076-3. [DOI] [PubMed] [Google Scholar]
- 35.Siu CW, Lau CP, Lee WL, Lam KF, Tse HF. Intravenous diltiazem is superior to intravenous amiodarone or digoxin for achieving ventricular rate control in patients with acute uncomplicated atrial fibrillation. Crit Care Med. 2009;37:2174–80. doi: 10.1097/CCM.0b013e3181a02f56. [DOI] [PubMed] [Google Scholar]
- 36.Hou ZY, Chang MS, Chen CY, Tu MS, Lin SL, Chiang HT, et al. Acute treatment of recent-onset atrial fibrillation and flutter with a tailored dosing regimen of intravenous amiodarone. A randomized, digoxin-controlled study. Eur Heart J. 1995;16:521–8. doi: 10.1093/oxfordjournals.eurheartj.a060945. [DOI] [PubMed] [Google Scholar]
- 37.Roth A, Kaluski E, Felner S, Heller K, Laniado S. Clonidine for patients with rapid atrial fibrillation. Ann Intern Med. 1992;116:388–90. doi: 10.7326/0003-4819-116-5-388. [DOI] [PubMed] [Google Scholar]
- 38.Simpson CS, Ghali WA, Sanfilippo AJ, Moritz S, Abdollah H. Clinical assessment of clonidine in the treatment of new-onset rapid atrial fibrillation: A prospective, randomized clinical trial. Am Heart J. 2001;142:E3. doi: 10.1067/mhj.2001.116761. [DOI] [PubMed] [Google Scholar]
- 39.Neuss H, Horn HG, Mitrović V, Buss J, Schlepper M. Heart rate reduction in atrial fibrillation with a rapid ventricular response by Gallopamil, a Ca-antagonist (author's transl) Z Kardiol. 1982;71:334–9. [PubMed] [Google Scholar]
- 40.Parvez B, Chopra N, Rowan S, Vaglio JC, Muhammad R, Roden DM, et al. A common ß1-adrenergic receptor polymorphism predicts favorable response to rate-control therapy in atrial fibrillation. J Am Coll Cardiol. 2012;59:49–56. doi: 10.1016/j.jacc.2011.08.061. [DOI] [PMC free article] [PubMed] [Google Scholar]


