Sir,
Antimicrobials are one of the most common class of drugs prescribed to patients in the intensive care units (ICUs). The total antimicrobial consumption is approximately tenfold greater in ICUs than in a general hospital wards. This high density of antimicrobial use favours the development of multi-drug resistant pathogens.[1] Rice, in 2008, reported that “Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumanii, Pseudomonas aeruginosa and Enterobacter species” pathogens are responsible for causing two-thirds of hospital infections and effectively “escape” the effects of antibacterial drugs.[2] The increase in the prevalence of drug resistant pathogens is occurring at a time when the discovery of new antimicrobial agents is slowing down dramatically.[3] In order to minimize the antimicrobial resistance, it is essential that the pattern of antimicrobial utilization is known well. The aim of this study was to understand the antimicrobial utilization pattern in the ICUs of a public tertiary care hospital.
This 3-month observational study was carried out at the ICUs of a public tertiary care hospital. ICUs with 14 bed capacity handle all patients who require ICU level care. Only patients with >24 h of ICU stay and who were prescribed at least one antimicrobial were included in this study. Patient records with incomplete documentation were excluded. The age and sex of patient, disease and treatment regimen were recorded in a predesigned standardized proforma. The patients were followed for the first 7 days of ICU stay and any changes made in the treatment regimen were carefully analyzed.
Antimicrobial utilization was assessed using Rational Pharmaceutical Management plus indicators. The prescriptions were also studied for the use of similar spectrum of antimicrobials, frequent switching of antimicrobials (without considering any sensitivity report within 72 h of its administration) and antimicrobial cocktail (use of more than two broad spectrum antimicrobials, excluding metronidazole and antifungals). Results are expressed in percentages and average ± standard error of the mean, as applicable.
A total of 87 patients’ data was collected; and two patients’ were excluded. One patient had ICU stay of less than 1 day, while the other had incomplete documentation. Of these 85 patients, 48 underwent a surgery and remaining 37 patients were nonsurgical patients.
The average age of patients was found to be 39.27 ± 1.93 years. Over 75% patients were in the age group of 18-60 years. And the mortality rate was found to be 28%.
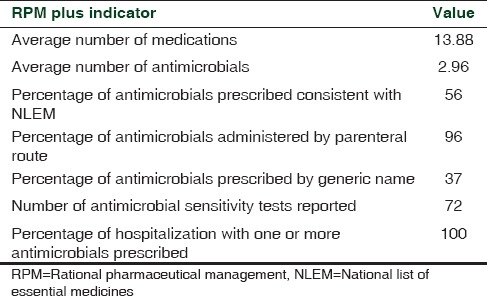
The average number of medications prescribed was found to be 13.88 ± 0.48. And, the average number of antimicrobials was found to be 2.96 ± 0.16. Adhikari et al. have shown that 45.1% of prescribed antimicrobials are consistent with National List of Essential Medicines (NLEM) 2011.[4] In this study, it was 56%, reflecting a better level of adherence to prescribing from NLEM. The common antimicrobials prescribed consistent with NLEM, were metronidazole, ceftriaxone, amikacin, amoxicillin + clavulanic acid, gentamicin and vancomycin. Approximately, 96% were administered by parenteral route. 37% of antimicrobials were prescribed by the generic name. [Table 1] These findings, however, are not in concurrence with findings from a private setting. It was shown that a total of 71.1% antimicrobial drugs were prescribed by generic name.[5] This difference is most likely due to the difference in the hospital setting (government vs private).
Table 1.
RPM plus indicators
Of 72 culture sensitivity tests performed, 43 were found to be positive. Acinetobacter sp. was the most common microorganism observed (15/43).
All the patients were prescribed at least one antimicrobial agent. 30% of the patients were prescribed three antimicrobials, 28% with 2, 14% with 1, and the remaining 28% with more than three antimicrobials.
Antimicrobial prescriptions were studied for their relative use in the ICU patients. It was found that Metronidazole was the most frequently prescribed antimicrobial (61% patients) followed by piperacillin + tazobactam (32%). Imipenem + cilastatin, cefoperazone + sulbactam and ciprofloxacin were used for 25%, 22% and 20% of patients, respectively. Metronidazole is the drug of choice for the treatment of anaerobic infections, which are usually treated empirically, without susceptibility testing.
In terms of the relative contribution to the prescribed antimicrobials, β-lactams were ranked first, contributing 41%. The second and third most commonly used antimicrobials were metronidazole and aminoglycosides in 21% and 12%, respectively. Fluoroquinolones, macrolides, oxazolidinones, antifungals and glycopeptides were used in 9%, 3%, 3%, 2%, and 1% patients, respectively.
To understand the nature of antimicrobial prescribing further, use of antimicrobials with a similar spectrum of activity, frequent switching of antimicrobials and use of antimicrobial cocktail were studied. Low values of any of these parameters indicate the careful prescribing. Use of antimicrobials with a similar spectrum of activity and frequent switching of antimicrobials was observed in only 6% of patients. Imipenem and piperacillin, amoxicillin + clavulanic acid and cefoperazone + sulbactam were the most common antimicrobial combinations with a similar spectrum prescribed. Use of more than two broad spectrum antimicrobials was seen in only 9% of patients.
Badar and Navale have reported that 77% patients were prescribed between one and three antimicrobials.[6] In this study, 72% patients were prescribed one to three antimicrobials which is similar to above mentioned study. This will have a bearing on the outcome of treatment. However, it is premature to comment on this conclusively on the basis of data on a limited number of patients.
Based on the findings of this study on 85 patients in the ICU, it appears logical that the use of antimicrobials in the ICUs should be studied over a longer period of time. The findings of prescription pattern reflect a very encouraging trend. Only 6% of patients witnessed prescription of similar spectrum antimicrobials and frequent switching. This ongoing study has provided initial evidence on antimicrobial utilization in an Indian public setting ICU.
REFERENCES
- 1.Kavar KS, Jha RK, Gaikwad NR, Jarande SS, Ranpura AM. Antibiotic use density in medicine ICU in a tertiary care rural hospital of central India. Res J Pharm Biol Chem Sci. 2012;3:133–42. [Google Scholar]
- 2.Rice LB. Federal funding for the study of antimicrobial resistance in nosocomial pathogens: No ESKAPE. J Infect Dis. 2008;197:1079–81. doi: 10.1086/533452. [DOI] [PubMed] [Google Scholar]
- 3.Mulvey MR, Simor AE. Antimicrobial resistance in hospitals: How concerned should we be? CMAJ. 2009;180:408–15. doi: 10.1503/cmaj.080239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adhikari A, Singh S, Bhowal T, Biswas S, Banerjee S, Ray M, et al. Study of prescribing pattern of antimicrobial agents in selected patients attending tertiary care hospital in India. Explor Anim Med Res. 2013;3:29–35. [Google Scholar]
- 5.Tiwari P, Singhal R, Malhotra S. Antimicrobial utilization in ICUs of a private tertiary care hospital. In: Lawrence R, Ebenezer J, Thomas G, editors. Antimicrobial Resistance: A Cause for Global Concern. New Delhi: Narosa Publishing House; 2013. [Google Scholar]
- 6.Badar VA, Navale SB. Study of prescribing pattern of antimicrobial agents in medicine intensive care unit of a teaching hospital in central India. J Assoc Physicians India. 2012;60:20–3. [PubMed] [Google Scholar]


