Abstract
Background
Over the past two decades, drug injection-related risk behaviors have been the major drivers of the HIV epidemic in Iran. This study assesses the access of people who injected drugs (PWID) to harm reduction services (needle-exchange programs [NEP] and methadone maintenance treatment [MMT]) in Tehran, Iran in 2007, almost five years after the large-scale implementation of these programs.
Methods
572 consenting PWID (>18 years old, ever injected in the past month, lived in Tehran or its suburbs) were recruited (24 seeds) into a sero-behavioral survey using respondent-driven sampling method. Participants completed a face-to-face interview about HIV-related risk behaviors and access to harm reduction services. We calculated adjusted population estimates using RDSAT.
Results
Overall, 99.2% of the participants were male, 41.6% aged between 30–39 years old, 55.4% lived alone in the past year, 83.2% were ever incarcerated, and 88.8% lived in the southern areas of Tehran. In terms of “awareness” and “use” of services among PWID, 62.8% and 54.8% reported for NEP (respectively) and 19.7% and 9.1% for drug treatment services (respectively). PWID who lived in Northwest and South-central Tehran were more likely to be aware (85.0 and 82.8%, respectively) of one or more services than PWID who lived elsewhere. Similarly, PWID who lived with friends were more likely to be aware of (88.6%) and use (85.9%) services (vs. other living partners). Overall, 11% of the participants were aware of but had not used any harm reduction services.
Conclusions
Despite a relatively high level of access to NEP among PWID in Tehran, a sizable fraction of the population remains without access to other services five years after their implementation. The use of harm reduction may be affected by certain PWID characteristics (e.g., living partners and geographical location). Ongoing surveillance activities are necessary to track change in access over time.
Keywords: Harm reduction, needle-exchange programs, methadone, injection-drug use, respondent-driven sampling, Iran, HIV
INTRODUCTION
Drug use has been one of the most serious health and social threats facing Iran in the past two decades. In 2006, a year prior to the implementation of this study, it was estimated that nearly two million of Iran’s 65 million population used opiates (Malekinejad and Vazirian 2012). The recreational use of opium smoking has been widespread for centuries in Iran and greatly influenced by Iran’s geographical proximity to Afghanistan, the world’s largest opium producer (Razzaghi, Movaghar et al. 2006). However, over the past two decades there has been a shift in the pattern of opiate use from smoking opium to injecting heroin (Malekinejad and Vazirian 2012). Varying sources place the number of people who inject drugs (PWID) in Iran between 200,000–300,000 (MAP Network 2001; Nissaramanesh, Trace et al. 2005; Razzaghi, Movaghar et al. 2006).
Injection drug use is associated with high rates of mortality, increased risk of parenterally transmitted infections (e.g., HIV, hepatitis C, hepatitis B), crime, and violence (Razzaghi, Movaghar et al. 2006; Malekinejad and Vazirian 2012). HIV prevalence has remained under 1% in the general population, but pooled HIV prevalence among PWID participating in various surveys was estimated to be 8.7% (95% Confidence Interval: 7.5–10) and 18.4% (95%CI: 16.7–20.2) for studies conducted between 1998–2005 and 2005–2007, respectively (Rahimi-Movaghar, Amin-Esmaeili et al. 2012 Jul). The higher prevalence of HIV amongst PWID is largely attributed to equipment-sharing and subsequent sexual encounters, with additional onward transmission to non-PWID partners including spouses (Razzaghi, Movaghar et al. 2006; Razani, Mohraz et al. 2007).
Iran’s policy toward substance use has been gradually changing between early 1980’s and completion of this study (2007). Until early 1990’s, Iran’s drug policy was mainly centered on supply-reduction and criminalization. A gradual shift toward inclusion of demand-reduction in the polices started by mid 1990s(Emran, Nassirimanesh et al. 5 August 2006; Razzaghi, Rahimi et al. 2000). By the end of 1990’s, combination of factors, including increasing number of HIV positive cases among PWID and prisoners, led to emergence of relatively small-scale harm reduction programs by non-governmental organizations and advent of Triangular Clinics (i.e. outpatient clinics providing services to HIV high risk populations by integrating HIV prevention strategies, treatment of sexually transmitted diseases, and treatment and care for people who live with HIV and AIDS) in 2000(WHO Regional Office for the Eastern Mediterranean 2004; Nissaramanesh, Trace et al. 2005). In 2002, Iran’s government initiated a large-scale implementation of harm-reduction programs promoting opioid substitution treatment (OST), needle exchange program (NEP), outreach, and prison-based programs. (Nissaramanesh, Trace et al. 2005; Tait 2005; Malekinejad and Vazirian 2012).
Methadone maintenance treatment (MMT) has been a major focus of OST interventions in Iran. Other advancements in Iran include the increasing presence of community-based drop-in centers (DIC). DICs serve as points of access for clean needles, drug treatment, condoms, sexually transmitted infection screening and treatment, primary healthcare, and reliable information on risky behaviors and HIV infection (Nissaramanesh, Trace et al. 2005). The provision of syringes through pharmacies has also been initiated, allowing the legal sale of clean syringes to drug users (Razzaghi, Movaghar et al. 2006). During 2006–2007, the same year that we collected data for this study, a total of 9,675 clients received outpatient drug treatment services in Tehran (nationally 169,827) through government funded clinics, of whom 6,893 (71%) were on OST services in Tehran (nationally 69,106). Further, 16 DICs distributed a total of 2,754,000 clean needles or syringes in Tehran (nationally 5,826,00), constituting an annual average of 331 per client per year (Noroozi, Shamshiri et al. 2007). By 2009, 1,600 clinics run mostly by private and non-governmental organizations (NGO) in Iran were providing MMT services to nearly 159,000 patients (Mokri and Schottenfeld 2008; Malekinejad and Vazirian 2012). A 2012 report found that 6,022,834 free needles and syringes were distributed nationally over the course of one year, ending in September 2011 (Ministry of Health and Medical Education 2012).
To understand the access to harm reduction services among active PWID in Tehran and the factors influencing them nearly five years after the implementation of harm reduction programs, we measured awareness about (knowledge) and use of the services using data from a HIV bio-behavioral survey conducted in 2007.
METHODS
We conducted a cross sectional survey in 2006–2007 to estimate the prevalence of HIV and related risk behaviors in Tehran, Iran. Details of the methods, procedures, and HIV prevalence results of this study have been published elsewhere (Malekinejad 2008). In brief, adult (>18 years old) active PWID (self-reported any injection in the past 30 days) were recruited using respondent-driven sampling (RDS). The feasibility and acceptability of RDS was assessed through a comprehensive formative assessment that included 40 key informant interviews and nine focus group discussions among PWID in Tehran (Razani, Mohraz et al. 2007). In brief, we initially recruited 14 seeds and conducted interviews only at our main research site, the Iranian Research Center for HIV/AIDS (IRCHA). Due to the lack of recruitment progress, from week 15 and onward we recruited 10 more seeds from four drop-in centers (Northeast, South, South Central, Southeast of Tehran) as our satellite recruitment sites to maximize the diversity of the sample and improve physical access of potential participants to survey sites. To facilitate the recruitment process, we paid $2.14 (increased from $1.05, starting week 15) to those who agreed to participate and completed the survey (primary incentive) and an additional $1.07 (increased from $0.54 starting from week 15) for every eligible person they referred to the study. Also, we limited the number of recruitment coupons to three per person and the coupons expired after one month. Recruited participants were given the option to attend either the research site at IRCHA or one of the satellite sites during designated hours.
The study sample was recruited over the course of 44 weeks. Twenty-four total seeds initiated the chain referral, distributing a total of 1,726 referral coupons. At the site, the eligibility of the referral cases was assessed by one trained staff and repeat referrals were excluded based on physical biomarkers and date of birth. In the end, 572 (including 24 seeds) eligible volunteers participated in the study. Participants underwent HIV testing and counseling as well as an in-person interview using a structured questionnaire to collect data on demography, history of incarceration, drug use, sexual risk behaviors, and access to harm reduction programs. Participation was voluntary and PWID were enrolled in the study once they provided verbal consent.
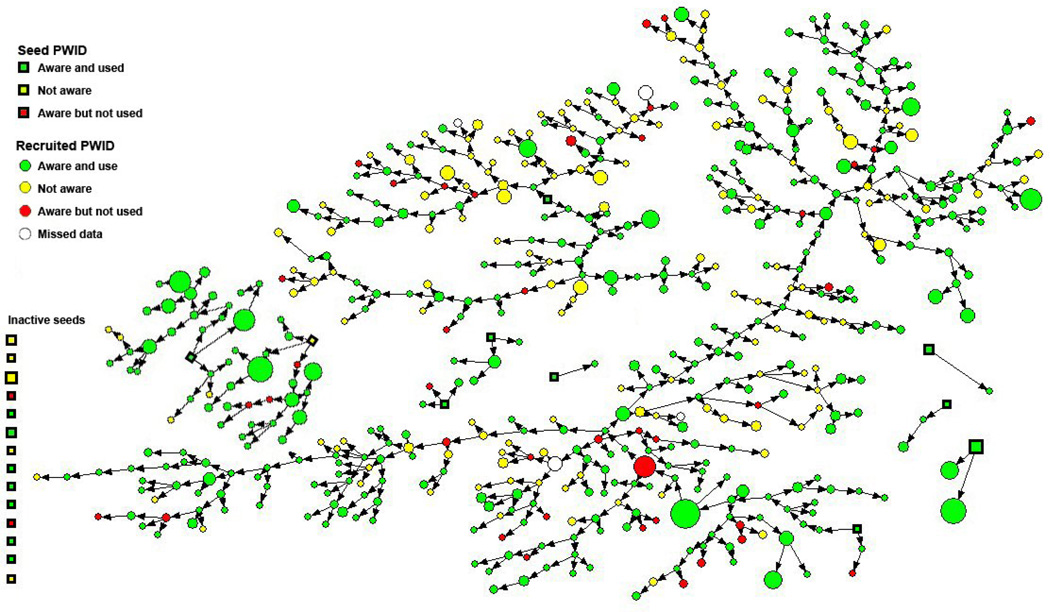
For this paper, we explored the levels of access to harm reduction services in the community (as opposed to within prison facilities that offered limited access to harm reduction) among this population. We defined access as 1) ever aware of service(s), and 2) ever used service(s). Then, we analyzed the association between individual demographic variables and access to harm reduction services through stratified analysis. Using the self-reported personal network size (i.e., “How many other drug injectors have you met in the last week whom you know by name and face?”) and the referral pattern of participants (Figure 1), we calculated adjusted population point estimates and 95% confidence intervals (CI) for demographic predictors and outcome variables using the RDS Analysis Tool version 6.0 (RDSAT). Outcome variables included access to NEP, MMT, and detoxification services as well as a composite harm reduction variable that was defined to include any of these three types of services. We further examined access to NEP by considering the proportion of participants with knowledge of specific locations to access services in Tehran. Further, we assessed and reported the gap as the percentage of all PWID reported being aware of certain services and not ever using them.
Figure 1.
Chain of recruitment in people who inject drug (PWID) and participated in our respondent-driven sampling survey in Tehran, Iran 2007 by (ever) awareness and use of any harm reduction services (n=572). Shape of nodes represents the recruitment role (square: seed, circle: recruited) of PWID. Size of shapes reflects self-reported network size. Arrow represents the recruitment pattern. Color represents level of access (see legend).
The study was reviewed and approved by the ethical committees of the University of California, Berkeley, the University of California, San Francisco, and the Iranian Ministry of Health and Medical Education.
RESULTS
Five hundred forty-eight (excluding 24 seeds) active PWID were recruited in this study; 543 had sufficient data for the analysis of most variables presented here (Table 1). Virtually all (541) were male; 41.6% (95% Confidence Interval 35.5 – 46.2%) age 30–39 years; 34.9% (95% CI 30.2 – 40.2%) homeless; 55.4% (95% CI 49.9 – 61.0%) lived alone; 7.7% (95% CI 4.2 – 10.3%) lived with family; and 6.3% (95% CI 4.1 – 9.1%) lived with friends. PWID appeared relatively well-educated with 45.7% (95% CI 40.4 – 51.9%) having completed middle school and 35.3% (95% CI 28.2 – 39.4%) having completed high school or higher. However, 45.8% (95% CI 39.6 – 51.0%) were unemployed. Forty-six percent (95% CI 41.1 – 52.5%) had never been married, and 44.3% (95% CI 38.9 – 49.9%) were no longer married. The vast majority, 83.2% (95% CI 81.1 – 88.1%), had a lifetime history of incarceration at the time of the study. Overall, 71.8% (95% CI 67.4–77.6%) had never been tested for HIV; of those who had been tested, 11.9% (95% CI 8.6–15.7%) reported that the test result was negative, 4.2% (95% CI 0.9–5.5%) tested positive, and 10.5% (95% CI 7.7–13.9%) never received test results (Table 1).
Table 1.
Crude and adjusted estimates of demographic variables, incarceration history, and HIV testing among people who inject drugs (n=572), Tehran, Iran 2007.
| Variable | N* | Freq. | Crude % | Adjusted % (95% CI) |
|---|---|---|---|---|
| Age group, years | ||||
| 20–29 | 543 | 135 | 24.9 | 26 (21.6–31.6) |
| 30–39 | 225 | 41.4 | 41.6 (35.5–46.2) | |
| 40–49 | 128 | 23.6 | 23.1 (19.4–28.7) | |
| 50+ | 55 | 10.1 | 9.3 (5.6–11.8) | |
| Residential status | ||||
| City of Tehran | 543 | 512 | 94.3 | 93.2 (89.5–96.1) |
| Sub-urban area of Tehran | 31 | 5.7 | 6.8 (3.9–10.5) | |
| Tehran region of residence | ||||
| Northwest | 471 | 23 | 4.9 | 4.3 (2.0–5.1) |
| Northeast | 24 | 5.1 | 6.9 (3.5–12.6) | |
| Southwest | 160 | 34.0 | 36.6 (29–42.3) | |
| South-central | 202 | 42.9 | 40.4 (34.1–47.7) | |
| Southeast | 62 | 13.2 | 11.8 (8.5–16.6) | |
| Resided longest in the last year | ||||
| Home | 543 | 223 | 41.1 | 45.5 (39.8–50.9) |
| Motel | 13 | 2.4 | 1.8 (0.7–3.4) | |
| Homeless | 191 | 35.2 | 34.9 (30.2–40.2) | |
| Prison | 69 | 12.7 | 11.4 (7.8–14.6) | |
| Narcotics Anonymous camp | 39 | 7.2 | 5.7 (3.4–8.2) | |
| Other | 8 | 1.5 | 0.8 (0.3–1.4) | |
| Living arrangement | ||||
| Family | 543 | 35 | 6.4 | 7.7 (4.2–10.3) |
| Extended Family | 143 | 26.3 | 29.8 (24.6–35.9) | |
| Alone | 319 | 58.7 | 55.4 (49.9–61.0) | |
| Friends | 39 | 7.2 | 6.3 (4.1–9.1) | |
| Other | 7 | 1.3 | 0.8 (0.3–1.6) | |
| Education level | ||||
| Elementary | 467 | 92 | 19.7 | 19.1 (15.5–25.3) |
| Middle School | 206 | 44.1 | 45.7 (40.4–51.9) | |
| High School and more | 169 | 36.2 | 35.3 (28.2–39.4) | |
| Employment status | ||||
| Any | 543 | 270 | 49.7 | 54.2 (49–60.4) |
| None | 273 | 50.3 | 45.8 (39.6–51.0) | |
| Marital status | ||||
| Never married | 543 | 251 | 46.2 | 46.2 (41.1–52.5) |
| Currently married | 48 | 8.8 | 9.4 (6.0–11.5) | |
| No longer married | 243 | 44.8 | 44.3 (38.9–49.9) | |
| Other | 1 | 0.2 | 0.2 (0.0–0.5) | |
| Ever incarcerated | ||||
| Yes | 543 | 451 | 83.1 | 83.2 (81.1–88.1) |
| No | 92 | 16.9 | 16.8 (11.9–18.9) | |
| HIV status (self-reported) | 71.8 (67.4–77.6) | |||
| Never tested | 543 | 394 | 72.6 | 10.5 (7.7–13.9) |
| Tested but did not get results | 63 | 11.6 | 4.2 (0.9–5.5) | |
| HIV positive | 13 | 2.4 | 11.9 (8.6–15.7) | |
| HIV negative | 69 | 12.7 | 1.7 (0.0–4.2) | |
| Indeterminate | 4 | 0.7 |
Seeds and participants with missing values were excluded.
Freq: Frequency; Crude %: unadjusted recruitment proportions; Adjusted %: estimated population proportions calculated by RDSAT; CI: Confidence interval
As presented in Table 2, compared to other services, awareness about and use of NEP were reported more frequently by PWID at 62.8% (95% CI 56.3 – 68.8%) and 54.8% (95% CI 49.0 – 61.9%), respectively. These figures were next highest for detoxification services, calculated at 19.7% (95% CI 14.8 – 24.8%) and 9.1% (95% CI 5.8 – 14.1%) respectively, followed by MMT, at 18.1% (95% CI 13.6 – 23.1%) and 6.9% (95% CI 4.2 – 9.8%), respectively. Seventy percent (95% CI 63.6 – 75.4%) reported awareness of any program (i.e. either NEP, detoxification services, or MMT), and 59.5% (95% CI 53.6 – 66.2%) had ever used one or more of them.
Table 2.
Crude and adjusted estimates of ever awareness and use of harm reduction services, people who inject drugs (n=572), Tehran, Iran, 2007.
| Variable | Aware of harm reduction services | Use of harm reduction services | ||||||
|---|---|---|---|---|---|---|---|---|
| N* | Freq. | Crude % |
Adjusted % (95% CI) |
N* | Freq. | Crude % |
Adjusted % (95% CI) |
|
| Needle exchange | 543 | 379 | 69.8 | 62.8 (56.3–68.8) | 543 | 344 | 63.4 | 54.8 (49.0–61.9) |
| Drug treatment | 543 | 103 | 19.0 | 19.7 (14.8–24.8) | 543 | 43 | 7.9 | 9.1 (5.8–14.1) |
| Methadone maintenance | 543 | 120 | 22.1 | 18.1 (13.6–23.1) | 543 | 43 | 7.9 | 6.9 (4.2–9.8) |
| Any of the above** | 541 | 402 | 74.3 | 70.4 (63.6–75.4) | 541 | 363 | 67.1 | 59.5 (53.6–66.2) |
Seeds and participants with missing values were excluded.
Any harm reduction program (needle exchange, other drug treatment services or methadone maintenance therapy)
Freq: Frequency; Crude %: unadjusted recruitment proportions; Adjusted %: estimated population proportions calculated by RDSAT; CI: Confidence interval
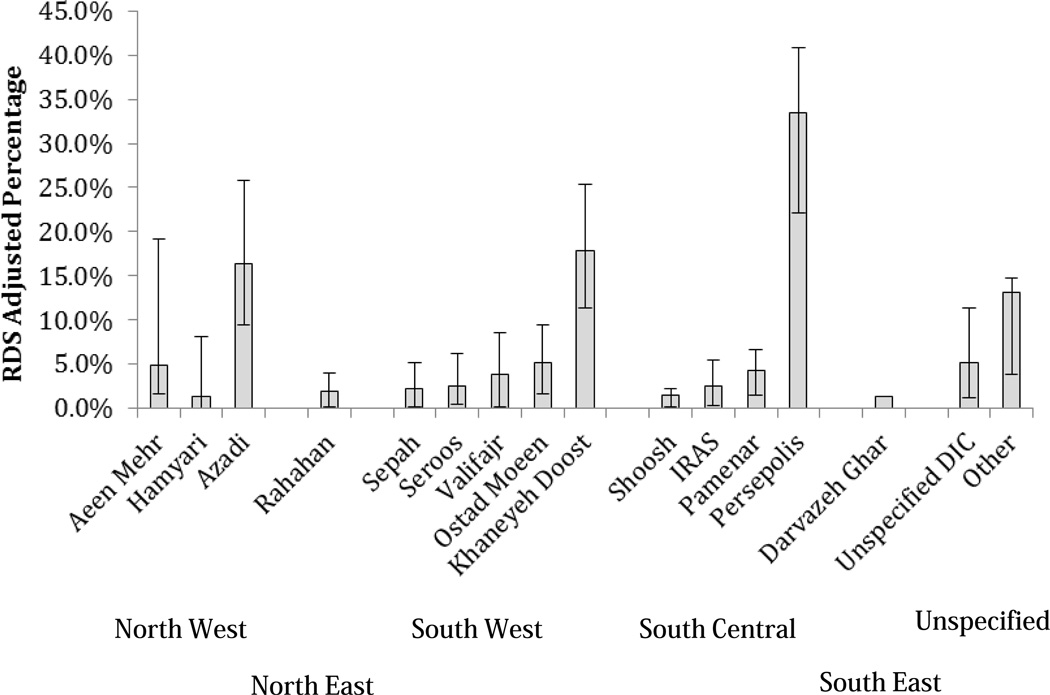
Respondents who indicated awareness of NEP were further asked to identify specific locations where the service was offered. The adjusted results are shown in Figure 2. Certain locations were clearly better known among the population of active PWID. For example, 34% (95% CI 21 – 43%) indicated Persepolis, 18% (95% CI 10–26%) indicated Khaneyeh Doost, and 17% (95% CI 9 – 29%) indicated the Azadi DIC in their responses. Many other locations were indicated by respondents but with lower frequency.
Figure 2.
Adjusted percentage (point and 95% confidence intervals) for ever awareness of specific name of centers providing needle exchange program (NEP) among people who inject drug (n=572), Tehran, Iran 2007.
Table 3 presents adjusted estimates of awareness and use of harm reduction services stratified by different PWID sub-populations. We found that respondents aged 40–49 were less likely to be aware of any of the composite harm reduction (CHR) services (52.1%, 95% CI 36.9–60.9%) or to have used CHR services (45.8%, 95% CI 34.3–57.3%) than those in other age groups. Respondents who lived in Tehran were more likely to be aware of CHR services (72.5% vs. 42.1%) and use CHR services (60.9% vs. 41.0%) than those who did not live in Tehran. Similarly, respondents who lived in Northwest Tehran were likely to be aware of CHR services (85.0%, 95% CI 58.7– 92.4%), but their use of CHR services was quite low (60.9%, 95% CI 53.3 – 88.5). Participants from Southwest Tehran reported the lowest use of CHR services (46.6%, 95% CI 36.6–57.3). Respondents who reported living with their family in the past year were less likely to be aware of CHR services (55.2%, 95% CI 30.4 – 77.0%) and use CHR services (43.9%, 95% CI 28.8 – 75.2%) than those who did not live with family. By contrast, respondents who lived with friends were more likely to be aware of CHR services (88.6%, 95% CI 75.1–95.2%) and use them (85.9%, 95% CI 71.0–93.9%).
Table 3.
Crude and adjusted estimates of ever aware and use of harm reduction services by different sub-populations of people who inject drugs (n=572), Tehran, Iran, 2007.
| Variable | Aware of harm reduction services** | Use of harm reduction services | ||||||
|---|---|---|---|---|---|---|---|---|
| N* | Freq. | Crude % | Adjusted % (95% CI) |
N* | Freq. | Crude % |
Adjusted % (95% CI) |
|
| Age group, years | ||||||||
| 20–29 | 134 | 94 | 70.1 | 73.1 (64.3–82.1) | 134 | 80 | 59.7 | 61.1 (51.9–71.8) |
| 30–39 | 225 | 175 | 77.8 | 77.0 (68.9–84.5) | 225 | 159 | 70.7 | 66.2 (57.2–74.9) |
| 40–49 | 127 | 90 | 70.9 | 52.1 (36.9–60.9) | 127 | 86 | 67.7 | 45.8 (34.3–57.3) |
| 50+ | 55 | 43 | 78.2 | 74.1 (54.5–86.5) | 55 | 38 | 69.1 | 54.3 (39.8–74.6) |
| Residential status | ||||||||
| City of Tehran | 510 | 382 | 74.9 | 72.5 (66.0–77.3) | 510 | 344 | 67.5 | 60.9 (55.0–67.7) |
| Sub-urban area of Tehran | 31 | 20 | 64.5 | 42.1 (22.3–67.7) | 31 | 19 | 61.3 | 41.0 (20.6–67.1) |
| Tehran region of residence | ||||||||
| Northwest | 23 | 17 | 73.9 | 85.0 (58.7–92.4) | 23 | 15 | 65.2 | 60.9 (53.3–88.5) |
| Northeast | 24 | 18 | 75.0 | 78.5 (56.9–95.2) | 24 | 16 | 66.7 | 74.4 (51.9–91.7) |
| Southwest | 159 | 109 | 68.6 | 61.3 (49.9–69.5) | 159 | 94 | 59.1 | 46.6 (36.6–57.3) |
| South Central | 202 | 167 | 82.7 | 82.8 (76.2–88.9) | 202 | 155 | 76.7 | 73.2 (63.0–80.6) |
| Southeast | 61 | 42 | 68.9 | 63.2 (46.7–80.7) | 61 | 40 | 65.6 | 57.1 (41.9–75.9) |
| Resided longest in last year | ||||||||
| Home | 223 | 161 | 72.2 | 70.8 (61.9–78.0) | 223 | 147 | 65.9 | 58.9 (52.8–71.3) |
| Motel | 13 | 9 | 69.2 | 55.0 (27.1–97.0) | 13 | 7 | 53.8 | 46.5 (19.1–89.3) |
| Homeless | 191 | 139 | 72.8 | 68.4 (57.8–75.5) | 191 | 130 | 68.1 | 62.3 (52.3–70.2) |
| Prison | 67 | 54 | 80.6 | 76.6 (58.4–90.4) | 67 | 44 | 65.7 | 59.2 (40.8–75.6) |
| Narcotics Anonymous camp | 39 | 32 | 82.1 | 69.3 (49.1–91.1) | 39 | 28 | 71.8 | 56.7 (36.4–80.0) |
| Other | 8 | 7 | 87.5 | 75.2 (42.1–100.0) | 8 | 7 | 87.5 | 75.3 (41.8–100.0) |
| Living arrangement | ||||||||
| Family | 35 | 22 | 62.9 | 55.2 (30.4–77.0) | 35 | 20 | 57.1 | 43.9 (28.8–75.2) |
| Extended Family | 143 | 104 | 72.7 | 72.0 (59.7–81.4) | 143 | 87 | 60.8 | 52.1 (41.6–65.5) |
| Alone | 318 | 243 | 76.4 | 69.0 (57.2–72.9) | 318 | 224 | 70.4 | 62.2 (52.9–68.2) |
| Friends | 38 | 30 | 78.9 | 88.6 (75.1–95.2) | 38 | 29 | 76.3 | 85.9 (71.0–93.9) |
| Other | 7 | 3 | 42.9 | 18.0 (2.5–58.8) | 7 | 3 | 42.9 | 18.2 (0.0–60.7) |
| Education level | ||||||||
| Elementary | 92 | 66 | 71.7 | 73.6 (61.7–85.0) | 92 | 60 | 65.2 | 61.5 (50.6–75.4) |
| Middle School | 206 | 148 | 71.8 | 66.5 (56.1–75.4) | 206 | 131 | 63.6 | 54.9 (46.8–65.9) |
| High School + | 168 | 129 | 76.8 | 73.2 (62.6–81.1) | 168 | 116 | 69.0 | 59.9 (48.8–71.1) |
| Employment status | ||||||||
| Any | 269 | 207 | 77.0 | 74.1 (65.1–81.2) | 269 | 182 | 67.7 | 61.4 (52.9–70.6) |
| None | 272 | 195 | 71.7 | 66.9 (58.7–73.6) | 272 | 181 | 66.5 | 58.0 (50.7–67.0) |
| Ever incarcerated | ||||||||
| Yes | 450 | 339 | 75.3 | 70.9 (63.7–76.5) | 450 | 306 | 68.0 | 61.1 (53.7–67.0) |
| No | 91 | 63 | 69.2 | 68.1 (51.8–77.9) | 91 | 57 | 62.6 | 52.3 (45.5–705) |
| HIV status | ||||||||
| Never tested | 393 | 273 | 69.5 | 64.1 (56.0–70.0) | 393 | 243 | 61.8 | 54.9 (47.3–61.7) |
| Tested but did not get results | 63 | 57 | 90.5 | 91.8 (84.6–97.3) | 63 | 52 | 82.5 | 83.5 (72.4–92.3) |
| HIV positive | 13 | 11 | 84.6 | 98.4 (92.7–100.0) | 13 | 10 | 76.9 | 54.5 (24.4–100.0) |
| HIV negative | 68 | 58 | 85.3 | 80.0 (67.0–93.5) | 68 | 55 | 80.9 | 76.6 (64.2–91.1) |
| Indeterminate | 4 | 3 | 75.0 | 35.4 (0.0–100.0) | 4 | 3 | 75.0 | 34.3 (0.0–100.0) |
Seeds and participants with missing values were excluded.
Any harm reduction program (needle exchange, other drug treatment services or methadone maintenance therapy);
Freq: Frequency; Crude %: unadjusted recruitment proportions; Adjusted %: estimated population proportions calculated by RDSAT; CI: Confidence interval
Regarding education level, awareness (66.5%, 95% CI 56.1 – 75.4%) and use (54.9%, 95% CI 46.8 – 65.9%) of any CHR services was lowest among respondents who had only completed middle school. Non-employed respondents were less likely to be aware of CHR (66.9% vs. 74.1%) and use CHR services (58.0% vs. 61.4%) than those with employment. Respondents with a history of incarceration were slightly more aware of CHR services (70.9% vs. 68.1%), and were more likely to have used CHR services (61.1% vs. 52.3%) than those with no such history. Respondents who had never been tested for HIV were less likely to be aware of CHR (64.1%, 95% CI 56.0–70.0%) or to have used CHR services (54.9%, 95% CI 47.3–61.7%) than those who had been tested.
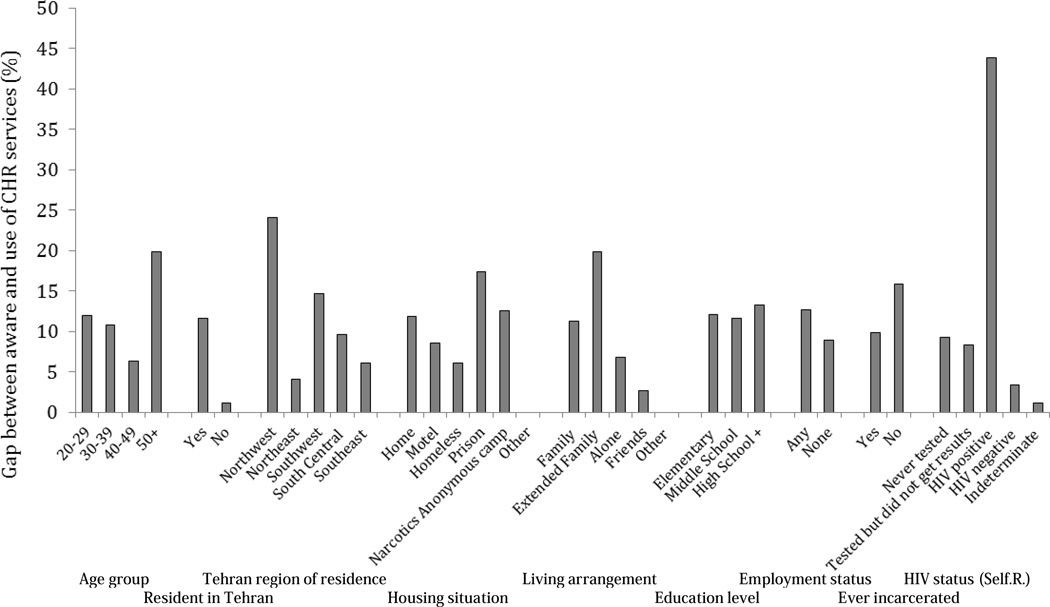
In Figure 3, we present the gap between awareness and use of CHR services. Overall, approximately 11% of PWID were aware of CHR services but never used them. This gap was higher (19.8%) among respondents who were more than 50 years of age; lived in Northwest Tehran (24.1%); reported to be in prisons for the majority of the previous year (17.4%); and self-reported being HIV positive (43.9%). The gaps for different education levels and employment were more or less similar (ranging 8.9% – 13.3%).
Figure 3.
The adjusted percentage of different sub-populations of people who inject drugs who were aware of services (any composite harm reduction - CHR - services) but did not use them (n=572), Tehran, Iran 2007.
DISCUSSION
To respond to the explosive HIV epidemic among PWID in Iran, NEP and MMT programs were implemented starting in 2002 (Nissaramanesh, Trace et al. 2005; Razzaghi, Movaghar et al. 2006). These services fall under the umbrella of the harm reduction policies that were introduced in Iran in 2002. In analyzing the effectiveness of harm reduction implementation in Iran, we found that following five years of program roll-out, awareness and use of NEP were relatively high among active PWID in Tehran but that a sizable fraction of the population was not accessing harm reduction services. Moreover, while the majority of PWID had accessed NEP, fewer than one in ten had accessed detoxification services or MMT. The lower uptake of detoxification services and MMT can be explained by several reasons, potentially including lower knowledge of their existence as compared to NEP, and the difference in motivation for detoxification and cessation of injecting via MMT than for safer injection via NEP; further explanations and ways to promote and improve access to these services in the community need to be explored. Further, our analysis of NEP by specific programs indicated that certain DIC have been recognized more than others by PWID. These specific programs may serve as models to improve uptake in other DIC and thereby increase NEP access to higher levels.
The availability of harm reduction services in 21 high epidemic countries has been reported by Petersen et al in their current published review. Only three countries (out of 21) have reached to the internationally recommended target of 200 syringes per person per year, others far behind it. MMT coverage has been reported as less than 3% in most countries (Petersen, Myers et al. 2013 Aug). Given the heterogeneity observed and reported by Peterson et al, we looked for local evidence for the Middle East region; data on service coverage, comparable to time of this study, were mainly lacking. We noted differences between our estimates of access to harm reduction programs and those reported in other studies. For example, our study conducted in 2006–2007 found that just 6.9% of respondents had ever used MMT, while a government report on HIV/AIDS in Iran reported MMT use as high as 33% in 2006–2007 and 42.6% in 2009–2010 (Ministry of Health and Medical Education 2012). This substantial difference may reflect our study scope and sampling technique. Our study was limited to Tehran and used the RDS methodology to estimate population levels of MMT uptake while Petersen’s report summarized studies that were conducted all over Iran and did not include details on sampling methodology. Our findings on use of NEP were more consistent with existing literature. Similar to our estimate that 54.8% of PWID have used NEP, Vazirian et al. conducted a study three years prior to ours and found that 62% of male PWID in Tehran had ever received free needles/syringes (Vazirian, Nassirimanesh et al. 2005).
We showed that the composite variable of awareness and use of harm reduction services was associated with residence, living situation, and HIV status. Respondents who lived in South-central Tehran were more aware of and more likely to use services than residents of other areas. This is notable since South-central Tehran has long been recognized as a “hotspot” for drug use activities and is thought to have the highest prevalence of drug use in Tehran (Razani, Mohraz et al. 2007). It could also reflect the success of Persepolis, the pioneer harm reduction program in Tehran, and highlight an opportunity for further understanding the Persepolis model and applying it to other locations. We also found that respondents who lived with friends were more aware of and more likely to use harm reduction services than those who lived with family. This suggests that friends are possible agents of information and influence behavior related to harm reduction, and/or family may hinder access because of stricter adherence to traditional values or lack of information (Malekinejad and Vazirian 2012). Further, as we observed in Figure 1, there are several PWID who reported utilizing services (Green circles) and recruited other PWID who were not aware (Yellow circles) or had not utilized them (Red). Public health policies that recognize and harness the influence of social networks to spread awareness could improve access to harm reduction in the PWID population. Finally, with regard to HIV status, we found that respondents who were previously tested for HIV were more likely to be aware of and use other harm reduction services than those who had not been tested. However, the highest gap between awareness and utilization of harm reduction services was among the respondents who had tested HIV positive. Both of these findings suggest that policies which promote the integration of harm reduction services and HIV testing and treatment efforts may be especially beneficial to increase and facilitate access for those interested in continuing to monitor their HIV status and encourage access for those that may be more resistant.
We recognize the limitations of our study. Uncertainties and potential biases of the RDS methodology and analytic approach have been previously described (McCreesh, Frost et al. 2012; Rudolph, Fuller et al. 2013). While the long-chain peer referral method is used to penetrate further into social circles that may not be accessed by the more visible parts of the population, and the RDSAT analysis attempts to correct for the degree of connectedness to others, the assumptions underlying RDS are difficult to verify. In this case, for example, PWID more closely connected to services may be more likely to participate in our survey and this bias may not be fully corrected. Our data may therefore over-estimate the levels of use of harm reduction services. Our data were also collected several years ago. Nonetheless, 2007 represents a point in time following a five-year scale-up of services. Whether the subsequent five years have experienced further increases is not known. Further, our data relies on the self-reported use of harm reduction services, which may lead to recall bias and subjectivity of data (Richter and Johnson 2001). However, self-reported information seemed the most plausible way to gather these types of data from PWID in Tehran, and interviewers were trained on techniques to reduce potential biases associated with in-person interviews. Lastly, we note that our study found very few female PWID, a point that also underscores the limits of how representative this RDS data is of all PWID in Tehran. The low recruitment of female PWID has been particularly noted in other RDS surveys in the Middle East region (Shawky, Soliman et al. 2009; Mahfoud, Afifi et al. 2010). Why women are not injecting drugs or, if they are, why they are not participating in our and other surveys in the region is unclear. Accordingly, we are left with little information on female PWID use of harm reduction. This is especially problematic since female drug users may be more likely to suffer severe medical problems, unemployment, depression and anxiety disorders, and human rights abuses than their male counterparts (Dolan, Salimi et al. 2011). These gender-specific risk factors highlight the need for new research approaches to recruit women and assess their access to harm reduction and HIV services.
Despite these limitations, our study provides a view at a critical point in time of access to harm reduction services and to NEP specifically in Tehran. The awareness and use of harm reduction services may be affected by certain personal and family-oriented barriers (self-stigma of HIV status and living partners) and certain physical barriers (living area and physical access). Ongoing HIV surveillance activities are needed to track the trajectory in the coverage of Iran’s harm reduction efforts and their impact on the HIV epidemic. Further research can offer a more nuanced representation of access to harm reduction among PWID in Tehran by exploring motivating factors leading to access of harm reduction, satisfaction with services, and individual-level explanations for the observed gap in awareness and use of services. We suggest that future investigations examine not only the coverage but also the linkages to HIV treatment and other medical care services; the effectiveness of harm reduction programs in preventing transmission of other parenterally transmitted infections; and the social consequences of drug use.
Highlights.
Using RDS method, we examine access to harm reduction programs five years after their implementation in Tehran.
There are still certain groups of people who inject drug who are underserved for such services.
Lack of awareness, personal and family oriented as well as physical access barriers are the most important predictors for it.
Ongoing surveillance activities are necessary to track change in access over time.
ACKNOWLEDGMENTS
We would like to thank to the directors of the drop-in centers Aeen Mehr I, Aeen-Mehr II, Azadi, and the Boo-Ali Triangular Center and the Persepolis Institute for their collaboration, and the staff of the IRCHA who provided logistical support throughout the study. We also would like to express our gratitude to Dr. Mohsen Vazirian at the Iranian National Center for Addiction Studies at TUMS who provided his expertise, Dr. Nooshin Razani at the Oakland Children’s Hospital in the United States for her contribution in study design, and Dr. Parastoo Khairandish at The Shiraz University of Medical Sciences for her contribution in data collection. Support: The original study was supported by a grant from the World Health Organization-Eastern Mediterranean Regional Office/Tropical Disease Research Programme small grant (Small Grants AMS Code 1: 43119022 and AMS Code 2: 43119040), Tehran University of Medical Sciences’ Office of the Deputy of Research (Grant No. 3895-55-02-85); and the John P. Dowdle Endowment and the Russell M. Grossman Medical Research Fund of the School of Public Health, University of California, Berkeley. Secondary data analysis for this paper was supported by a grant from US National Institute for Drug Abuse (NIDA) (Grant No. 1R21DA029473-01).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors maybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: None
References
- Dolan K, Salimi S, et al. Characteristics of Iranian women seeking drug treatment. J Womens Health (Larchmt) 2011;20(11):1687–1691. doi: 10.1089/jwh.2010.2694. [DOI] [PubMed] [Google Scholar]
- Emran R, Nassirimanesh B, et al. HIV/AIDS harm reduction in Iran. The Lancet. 2006 Aug 5;368(9534):434–435. doi: 10.1016/S0140-6736(06)69132-0. [DOI] [PubMed] [Google Scholar]
- Mahfoud Z, Afifi R, et al. HIV/AIDS among female sex workers, injecting drug users and men who have sex with men in Lebanon: results of the first biobehavioral surveys. AIDS. 2010;24(Suppl 2):S45–S54. doi: 10.1097/01.aids.0000386733.02425.98. [DOI] [PubMed] [Google Scholar]
- Malekinejad M. Assessment of the use of respondent-driven sampling for studying populations most at risk of HIV infection. Doctoral Dissertation. Dr.P.H, University of California; 2008. [Google Scholar]
- Malekinejad M, Vazirian M. Transition to injection amongst opioid users in Iran: implications for harm reduction. Int J Drug Policy. 2012;23(4):333–337. doi: 10.1016/j.drugpo.2011.09.001. [DOI] [PubMed] [Google Scholar]
- MAP Network. The Status and Trends of HIV/AIDS/STI Epidemics in Asia and the Pacific. Monitoring the AIDS Pandemic (MAP) Provisional Report. 2001 [Google Scholar]
- McCreesh N, Frost SD, et al. Evaluation of respondent-driven sampling. Epidemiology. 2012;23(1):138–147. doi: 10.1097/EDE.0b013e31823ac17c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health and Medical Education. Islamic Republic of Iran Progress Report: On Monitoring of the United Nations Special Session on HIV and AIDS. National AIDS Committee Secretariat. 2012 [Google Scholar]
- Mokri A, Schottenfeld R. "Drug Abuse and HIV Transmission in Iran - Responding to Public Health Challenges." Public Health Aspects of HIV/AIDS in Low and Middle Income Countries: Epidemiology, Prevention and Care. Ed. David Celentano and Chris Beyrer. Springer. 2008:583–599. [Google Scholar]
- Nissaramanesh B, Trace M, et al. The risk of harm reduction in the Islamic Republic of Iran. Briefing Paper 8: The Beckley Foundation Drug Policy Programme. 2005 [Google Scholar]
- Noroozi A, Shamshiri A, et al. Geographical distribution of mental, social, and addiction in 2007: substance use version. Tehran, Iranian Ministry of Health and Medical Education, Office of Mental and Social Health and Addiction. 2007 [Google Scholar]
- Petersen Z, Myers B, et al. Availability of HIV prevention and treatment services for people who inject drugs: findings from 21 countries. Harm Reduct J. 19;10:13. 2013 Aug;19(10) doi: 10.1186/1477-7517-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahimi-Movaghar A, Amin-Esmaeili M, et al. HIV prevalence amongst injecting drug users in Iran: a systematic review of studies conducted during the decade 1998–2007. Int J Drug Policy. 2012 Jul;23(4):271–278. doi: 10.1016/j.drugpo.2011.09.002. [DOI] [PubMed] [Google Scholar]
- Razani N, Mohraz M, et al. HIV risk behavior among injection drug users in Tehran, Iran. Addiction. 2007;102(9):1472–1482. doi: 10.1111/j.1360-0443.2007.01914.x. [DOI] [PubMed] [Google Scholar]
- Razzaghi E, Rahimi A, et al. Rapid assessment of drug misuse in Iran, Tehran 1998–1999. Tehran: Iranian Welfare Organization Press; 2000. [Google Scholar]
- Razzaghi EM, Movaghar AR, et al. Profiles of risk: a qualitative study of injecting drug users in Tehran, Iran. Harm Reduct J. 2006;3:12. doi: 10.1186/1477-7517-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter L, Johnson PB. Current Methods of Assessing Substance Use: A Review of Strengths, Problems, and Developments. Journal of Drug Issues. 2001;31(4):809–832. [Google Scholar]
- Rudolph AE, Fuller CM, et al. The importance of measuring and accounting for potential biases in respondent-driven samples. AIDS Behav. 2013;17(6):2244–2252. doi: 10.1007/s10461-013-0451-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shawky S, Soliman C, et al. HIV surveillance and epidemic profile in the Middle East and North Africa. J Acquir Immune Defic Syndr. 2009;51(Suppl 3):S83–S95. doi: 10.1097/QAI.0b013e3181aafd3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tait R. Iran faces up to its most lethal threat-drugs. The Guardian. 2005 [ http://www.mapinc.org/media/175]. [Google Scholar]
- Vazirian M, Nassirimanesh B, et al. Needle and syringe sharing practices of injecting drug users participating in an outreach HIV prevention program in Tehran, Iran: a cross-sectional study. Harm Reduct J. 2005;2:19. doi: 10.1186/1477-7517-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Regional Office for the Eastern Mediterranean. Best practice in HIV/AIDS prevention and care for injecting drug abusers: the triangular clinic in Kermanshah, Islamic Republic of Iran. 2004