Abstract
OBJECTIVE
Children from food-insecure families (ie, families that lack access to sufficient, safe, and nutritious food) are at risk for developmental problems. Food insecurity disproportionately occurs among low–socioeconomic status (SES) and low-income families; however, interventions that supplement families’ income or diet have not eradicated food insecurity. This may be because food insecurity is also related to nonfinancial factors such as the presence of maternal mental health problems. To clarify whether addressing mothers’ mental health problems may be a promising strategy for reducing the burden of food insecurity, we tested the hypothesis that low-SES families are especially vulnerable to food insecurity when the mother experiences depression, alcohol or drug abuse, psychosis spectrum disorder, or domestic violence.
METHODS
We used data from a nationally representative cohort of 1116 British families (the Environmental Risk Longitudinal Study). Food insecurity, family SES, maternal mental health and exposure to domestic violence, and children’s behavioral outcomes were measured by using validated methods.
RESULTS
Overall, 9.7% of study families were food-insecure. Among low-SES families, controlling for income variation, food insecurity cooccurred with maternal depression (odds ratio [OR]: 2.82 [95% confidence interval (CI): 1.62–4.93]), psychosis spectrum disorder (OR: 4.01 [95% CI: 2.03–7.94]), and domestic violence (OR: 2.36 [95% CI: 1.18– 4.73]). In addition, food insecurity predicted elevated rates of children’s behavior problems.
CONCLUSIONS
Among families with young children, food insecurity is frequent, particularly when the mother experiences mental health problems. This suggests that interventions that improve women’s mental health may also contribute to decreasing the burden of food insecurity and its impact on the next generation.
Keywords: food insecurity, mental health, socioeconomic factors, families, longitudinal study
Food insecurity, defined as lack of access to “sufficient, safe, and nutritious food that meets individuals’ dietary needs and preferences for an active and healthy life”1 affects 5% to 15% of families in the United States and Canada2–6 and is increasingly recognized as a public health concern in Europe.7,8 Children who grow up in food-insecure families are at risk for health and developmental problems,4–6,9–13 and identifying families who are at risk for food insecurity is a public health priority.
A key risk factor for food insecurity is low income.14 Thus, interventions that aim to tackle food insecurity and its consequences on families have primarily focused on supplementing poor families’ income to help them purchase nutritious foods (eg, Supplemental Nutrition Assistance Program or the Special Supplemental Nutrition Program for Women, Infants, and Children in the United States15; Healthy Start program in the United Kingdom16). Other programs have set out to provide school-based meals for children who live in poverty (eg, School Meals program in the United States17; the Free School Lunch program in the United Kingdom18). Such subsidized school meal programs can have beneficial effects on children’s nutritional and behavioral outcomes19; however, they do not always match the students’ tastes and are sometimes perceived as stigmatizing. As a result, many eligible students do not participate15; therefore, despite such programs, food insecurity remains an important public health issue across developed nations, suggesting that improving families’ financial circumstances or supplementing children’s diet does not suffice to eliminate food insecurity.
A few previous studies suggested that in addition to low income, an important risk factor for families’ inadequate food access is the mother’s experience of mental health problems.20,21 We sought to provide additional evidence for the role of mental health by testing the hypothesis that among socioeconomically deprived families, those in which the mother experiences mental health problems are most likely to be food-insecure. If this hypothesis is supported, then the finding would recommend experimental initiatives to test whether treatment of women’s mental health problems can reduce children’s food insecurity.
Specifically, using a national sample of British families with young children, we systematically tested whether among low–socioeconomic status (SES) families, maternal depression, psychotic symptoms, alcohol- or drug-related problems, or experience of domestic violence are associated with food insecurity. Moreover, because consequences of food insecurity are less well studied in Europe than in the United States, as a secondary aim we verified that, in our sample, food insecurity predicted children’s behavioral outcomes.
METHODS
Study Population
The Environmental Risk (E-Risk) study follows 1116 British families who were selected from a register of all 1994– 1995 twin births in England and Wales (see Moffitt22 for a full description of sampling methods). Families were selected to represent the distribution of maternal age at first birth in the population23 (ie, by matching maternal age to the general population, older mothers whose twins resulted from assisted reproduction were underrepresented). As previously shown, findings from the E-Risk sample can be generalized to the general population of British families with children who were born in the 1990s, because participants are comparable on maternal age at first birth, prevalence of maternal depression, maternal reading level, child IQ, and child behavioral problems.22
The sample was established in 1999–2000, when participating children were 5 years of age. Study families were assessed in home visits in 1999–2000, 2001–2002 (98% of the original sample), and 2005–2006 (96% of the original sample). All interviews were conducted by research interviewers who completed a formal 15-day training program to attain certification to a rigorous reliability standard. The E-Risk study received ethical approval from the Maudsley Hospital Ethics Committee.
Measures
We examined (1) family sociodemographic characteristics as predictors assessed at baseline in 1999–2000, (2) maternal mental health and domestic violence assessed in 2001–2002, and (3) children’s behavioral outcomes assessed in 2005–2006. Food insecurity was assessed twice: in 2001–2002 and in 2005–2006.
Food Insecurity
The family’s food situation was reported by the mother to a clinical interviewer and coded by using a 7-item scale developed by the US Department of Agriculture (Table 1).24 This scale distinguishes families that are (1) food-secure (ie, there is no evidence of food insecurity; 0–1 positive responses), (2) food-insecure without hunger (ie, food insecurity is evident, but there is no reduction in the family’s food intake; 2–4 positive responses), or (3) food-insecure with hunger (ie, food intake is reduced; 5–7 positive responses). In our study, fewer than 2% of families experienced food insecurity with hunger, so we combined them with the other food-insecure families. Using both assessments available to us, we identified families who were ever food-insecure (food-insecure in 2001–2002 and/or in 2005–2006 [9.7%]) and compared them with families who were always food-secure (food-secure in 2001–2002 and in 2005–2006 [90.3%]). In addition, we compared families who were persistently food-insecure (food-insecure in 2001–2002 and in 2005–2006 [2.5%]) or transiently food-insecure (food-insecure in 2001–2002 or in 2005–2006 [7.2%]) with families who were always food-secure.
TABLE 1.
Household Food-Insecurity Scale (Prevalence of Responses in the E-Risk Study)24
| Item | Positive Response | % |
|---|---|---|
| In the past 12 months | ||
| 1. The food that we bought just didn’t last. | Sometimes or often true | 12.1 |
| 2. We couldn’t afford to eat balanced meals. | Sometimes or often true | 9.3 |
| In the past 12 months | ||
| 3. Did you ever eat less than you felt you should because there wasn’t enough money to buy food? | Yes | 6.3 |
| 4. Were you ever hungry but didn’t eat because you couldn’t afford enough food? | Yes | 3.0 |
| 5. Did you or other adults in your house ever cut the size of your meals or skip meals because there wasn’t enough money for food? | Yes | 7.1 |
| 6. Did you ever cut the size of any of your children’s meals or skip meals because there wasn’t enough money for food? | Yes | 0.4 |
| 7. If yes to any of the above, how often did this happen? | Some months but not every month or almost every month | 5.1 |
Family Sociodemographic Characteristics
Following research suggesting that food insecurity is related not only to income but also to other socioeconomic characteristics that capture individuals’ level of nonfinancial resources,14,20,25 we focused on food insecurity among low-SES families. SES was assessed by a standardized composite of 3 indicators: household income, parental education (the highest of mother’s or father’s), and parental occupational grade (the highest of mother’s or father’s). We then standardized all 3 SES indicators and summed them. Low SES was defined as the lowest tertile of the SES distribution.26
To account for the possibility that food-insecure and food-secure families may differ with regard to characteristics other than SES and maternal mental health characteristics, we systematically verified differences with regard to other family characteristics. Mother’s age at study inception, children’s ethnic background, the number of individuals living in the household, and mother’s employment status were reported by the mother. Mother’s partnership status was assessed by using a life history calendar,27 which allowed us to determine the number of months the mother lived without a partner since the children were born. Mother’s reading level was tested using the Wide Range Achievement Test 3.28 Mothers who scored below the 15th percentile of the standard distribution (a score of ≤39) were considered to have reading difficulty.29
Mother’s Mental Health, Substance Abuse, and Experience of Domestic Violence
Depression was assessed by using the Diagnostic Interview Schedule30 following Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria.31,32
Psychosis spectrum disorder was also assessed by using the Diagnostic Interview Schedule, which inquires about characteristic symptoms: hallucinations, delusions, disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms (avolition, flat affect, alogia). Our interview ruled out symptoms with plausible explanations and symptoms that occurred solely under the influence of alcohol or drugs. Following Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria for schizophrenia, women were classified as having a psychosis spectrum disorder given the presence of hallucinations plus at least 2 other symptoms, as well as evidence of social, occupational, or self-care dysfunction.33 Our goal was not to diagnose clinical schizophrenia but to identify women who endorse impairing psychosis-like experiences and beliefs, given compelling evidence that psychosis spectrum syndromes in the general population are more prevalent than registered treated cases of schizophrenia.34
Alcohol- and drug-related problems were assessed with questions from the Short Michigan Alcoholism Screening Test35 and the Drug Abuse Screening Test.36 Internal consistency reliabilities for both scales were >0.70. A symptom was considered to be present when the mother endorsed the symptom as being “very true or often true.” Following previous research, we classified mothers who reported ≥4 symptoms as having an alcohol- or drug-related problem.37,38
Mothers’ experience of domestic violence was assessed by incurring ~ 12 acts of physical violence on the basis of the Conflict Tactics Scale.39 This domestic violence scale has high internal consistency reliability (Cronbach’s α = .89)40 and high interpartner agreement reliability (latent correlation = 0.77)41 and is a strong predictor of which couples in the general population experience clinically significant violence involving injury or intervention by official agencies.42 Mothers who had experienced ≥1 incident of domestic violence were considered to be exposed.
Children’s Behavioral Problems
Children’s psychological and behavioral problems were assessed at the age of 10 by the Achenbach family of instruments:the Child Behavior Checklist administered to mothers43 and the Teacher’s Report Form administered to teachers.44 The test manual defines children with a t score of ≥60 as having clinically significant problems.
Statistical Analysis
Food insecurity is especially likely to occur among low-SES families; therefore, we focused on this group, comparing food-insecure low-SES families with food-secure low-SES families by using multiple regression methods. For comparison, tables also present the characteristics of intermediate/ high-SES families.
RESULTS
As expected, food insecurity occurred 5.79 times (P< .0001) more frequently among low-SES families (26.0%) than among intermediate/high-SES families (4.3%). Within the low-SES group, food-insecure and food-secure families did not differ in terms of sociodemographic characteristics except for income levels, which were significantly lower among food-insecure families (Table 2); therefore, all subsequent analyses were systematically controlled for income.
TABLE 2.
Food Insecurity and Family Sociodemographic Characteristics in the E-Risk Study
| Parameter | Intermediate/High SES (N = 728) |
Low SES | OR (95% CI)a | Statistical Significance Testsb |
||
|---|---|---|---|---|---|---|
| Always Food-Secure (N= 264) |
Ever Food-Insecure (N= 96) |
T test | P | |||
| Household income, mean (SD)c | 0.45 (0.87) | −0.87 (0.46) | −1.01 (0.39) | 2.30 | .02 | |
| Mother’s age at study inception, mean (SD), yd | 35.5 (5.4) | 32.2 (5.8) | 32.0 (6.3) | −0.21 | .83 | |
| Children’s nonwhite ethnicity, % | 10.0 | 6.8 | 13.4 | 2.19 (0.96–4.97) | ||
| No. of months living without a partner, mean (SD) | 6.5 (16.3) | 22.0 (27.0) | 29.0 (30.8) | 1.52 | .12 | |
| No. of individuals in household, mean (SD) | 5.0 (1.1) | 5.2 (1.4) | 5.2 (1.7) | 0.64 | .52 | |
| Mother is employed outside the home (%) | 79.2 | 41.2 | 36.4 | 0.86 (0.52–1.41) | ||
| Mother’s reading difficulty (%) | 8.1 | 28.0 | 33.7 | 1.39 (0.82–2.36) | ||
Categorical variables were analyzed by using ORs. All analyses are adjusted for household income.
Continuous variables were analyzed by using t tests. All analyses are adjusted for household income.
Household income was measured in British pounds per year. This measure was then standardized to a mean of 0 and an SD of 1. Our findings indicate that average income levels among intermediate/high-SES families were 0.45 SD above the sample mean, whereas average income levels among low-SES families were 0.87 SD below the sample mean among those who were food-secure and 1.01 SD below the sample mean among those who were food-insecure.
The E-Risk study began in 1999 –2000, when study children were 5 years of age.
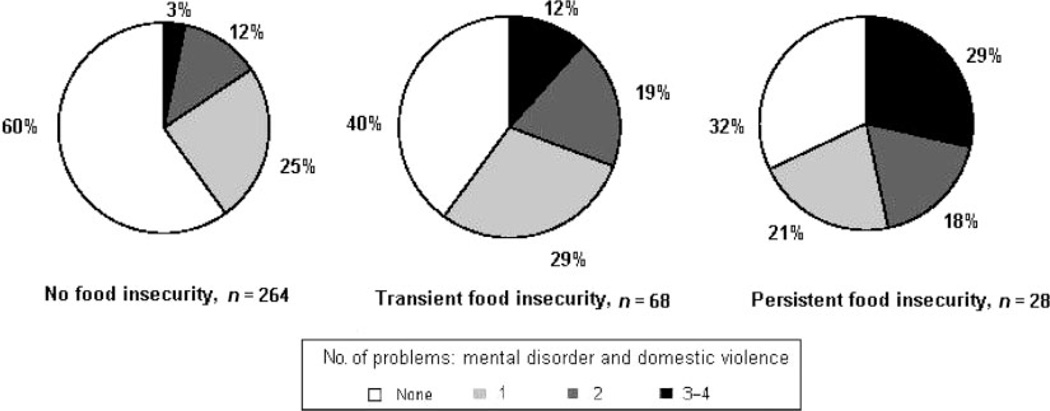
Controlling for income, we found that food-insecure low-SES families were disproportionately headed by a mother who experienced depression, a psychosis spectrum disorder, or domestic violence (Table 3). Moreover, as shown in Fig 1, food insecurity was related to the mother’s overall burden of mental health problems and domestic violence (χ2 = 57.42, P < .0001). The majority of mothers who headed food-secure families experienced no mental health problems or domestic violence; in contrast, more than two thirds of mothers from persistently food-insecure families experienced a mental health problem or domestic violence, and 29% experienced 3 or 4 such problems.
TABLE 3.
Food Insecurity and Maternal Experience of Mental Health Problems and Domestic Violence in the E-Risk Study
| Parameter | Intermediate/High SES, % (n) |
Low SES |
OR (95% CI)a | |
|---|---|---|---|---|
| Always Food- Secure, % (n) |
Ever Food- Insecure, % (n) |
|||
| Depression | 9.8 (71) | 14.0 (37) | 32.3 (31) | 2.82 (1.61–4.93) |
| Psychosis spectrum disorder | 2.3 (16) | 7.1 (18) | 23.7 (22) | 4.01 (2.03–7.94) |
| Alcohol- or drug-related disorder | 5.5 (40) | 9.9 (26) | 18.1 (17) | 1.76 (0.89–3.47) |
| Domestic violenceb | 13.2 (88) | 22.4 (38) | 40.8 (20) | 2.36 (1.18–4.73) |
All analyses are adjusted for household income.
Domestic violence was studied only among women who were living with a partner: n= 669 in the intermediate/high-SES group; n= 219 in the low-SES group.
FIGURE 1.
Food insecurity and maternal experience of mental health problems (depression, psychosis spectrum disorder, and alcohol- or drug-related disorder) and domestic violence among low-SES families in the E-Risk study.
At age 10, food-insecure children had higher rates of clinically significant behavioral problems (27%) as compared with food-secure children (10%; odds ratio [OR]: 2.05 [95% confidence interval (CI): 1.43–2.95]; P < .0001 adjusted for SES). This effect remained after adjustment for maternal mental health difficulties (OR: 1.64 [95% CI: 1.13–2.39]).The effect of food insecurity also applied when we examined children’s behavior problems as reported independently by mothers on the Child Behavior Checklist (β = .32, SE = .07, t = 4.43, P < .001) and by teachers on the Teacher Report Form (β = .16, SE = .07, t = 2.31, P = .02). (Significance tests involving twins were corrected for the inclusion of 2 study children in each family.45) When maternal mental health difficulties were present, 34% of children in food-insecure families had behavioral problems as compared with 18% of children in food-secure families. Similarly, when maternal mental health difficulties were absent, 18% of children in food-insecure families had behavioral problems as compared with 7% in food-secure families.
DISCUSSION
Studying a community sample of families with young children, we found that 9.7% experienced food insecurity. Low-SES families were most likely to be food-insecure, especially when they were headed by a mother who experienced depression, psychotic symptoms, or domestic violence. Additional research is now needed to test whether interventions that address women’s mental health symptoms can help to reduce the burden of food insecurity and its consequences on families.
Our study focused on food insecurity among low-SES families, guided by the observation that individuals in the low socioeconomic stratum of society are most vulnerable to food insecurity. As such, the pressing question, from a public health perspective is, “Can we identify and prevent the risk for food insecurity among families in deprived circumstances?” In many families, food insecurity occurs alongside other forms of social inequality, which must be accounted for to identify the specific role of mental health. To account for possible confounding, we examined the relationship between mental health and food insecurity among families who were matched for other forms of socioeconomic disadvantage. Within low-SES families, we further controlled for income inequalities, which allowed us to establish that the effects of mental health and domestic violence on food insecurity were independent of the effects of other forms of social and economic deprivation.
Our research has several strengths: (1) a contemporary sample representing the full range of SES in the general population of British families with children who were born in the 1990s; (2) a longitudinal design ascertaining the persistence of food insecurity during a period of 4 years; (3) validated measures of food insecurity and psychiatric disorders; and (4) statistical adjustment for income variation. We acknowledge possible limitations, however. First, all participating families had twins, which raises the question of the generalizability of our findings. Reassuringly, past research showed that families with twins are comparable to families with singletons with regard to all of the measurements used in this article: maternal mental health, family sociodemographic characteristics, and children’s behavioral problems.22,46–48 Moreover, the prevalence of food insecurity in our sample (9.7%) is consistent with reports from the United States and Canada.2–6 Second, food insecurity was reported by the mothers, raising the possibility that the assessment may have been influenced by mothers’ acute mental health symptoms49; however, in our study, mothers did not self-complete study questionnaires; they were interviewed by a highly skilled research worker with advanced training in clinical interviewing, which reduces the possibility of information bias. Moreover, mothers who took part in the study were able to schedule study visits at a time when they were well enough to complete the interview. Thus, it is unlikely that the relationship between mothers’ mental health and food insecurity in our study reflects reporting bias. Nonetheless, we cannot test this empirically, which is a limitation. In future studies, it may be relevant to obtain reports of food insecurity from several informants, including children.8 Third, although mental health problems may affect the family’s food situation, it is also possible that food insecurity is stressful and contributes to mothers’ mental health problems.6,9,14,50–52 For clarification of the direction of the association between food insecurity and women’s psychopathology, randomized trials are needed to test whether effective treatment of mothers’ mental health problems leads to improvements in the family’s food situation are needed.
How may maternal mental health affect a family’s food situation? Symptoms of major depression include loss of interest or pleasure; decreased energy; tiredness or fatigue; and an impaired ability to think, concentrate, or make decisions.31 Research interviewers who visited E-Risk study families frequently reported that depressed mothers lacked the energy to shop for groceries or to cook family meals (eg, case 1418: “The mom felt she couldn’t find the energy to do anything. She had to make dinner for the children but found it hard to make herself do it”; case 6027: “The children say that the mom sleeps all the time, that is all she does. During our visit the children ate only junk food”). Symptoms of psychotic disorders include impaired volition, drive, and attention, and women with psychotic symptoms may have difficulty planning family meals and managing financial resources (eg, case 6340: “The mom was very vague and unclear about the children’s needs, seemed to have little interest in their activities”; case 8107: “The mother is being treated for schizophrenia and has difficulty maintaining social relationships. When her partner went to prison, she let financial matters slip and had legal problems because she did not pay tax”). Research investigating the needs of mothers with psychotic disorders has indicated that a significant proportion have unmet needs relating to benefits and food.53 Psychotic disorders can also involve paranoid delusions about food being poisoned; such delusions could lead mothers to avoid many foodstuffs and to prevent their children from eating foods that are perceived as dangerous. The frequency of this phenomenon is not known, but clinical experience suggests that it does occur in a minority of mothers with psychoses. Women who are victims of domestic violence lose the sense of control over their household and are preoccupied by intense fear. This may make them unable to attend to their children’s needs.54 Sometimes, money may be withheld by the partner so that the woman is never sure whether she will have enough to buy food for her family. In addition, domestic violence often cooccurs with mental disorders.55 There-fore, it is not surprising that, in our study, women who experienced domestic violence and mental health problems were most likely to be food-insecure. In keeping with this interpretation, although food insecurity was extremely rare in households that were not of low SES, 58% of mothers in the few intermediate/high-SES households that were food-insecure had ≥1 mental health difficulty, as compared with 29% of mothers in intermediate/ high-SES food-secure households.
As in other studies, we found elevated rates of behavioral problems among children from food-insecure families.6,11,13 Nonetheless, it is unclear whether food insecurity is a cause of child psychopathology. The cooccurrence of food insecurity with maternal mental illness raises the possibility that children from food-insecure homes carry a high familial risk for psychopathology, partly reflecting genetic transmission. If so, then the association between food insecurity and children’s behavior may not be causal. Our research design did not allow us to resolve this issue of causality; however, genetic transmission is unlikely to be the whole explanation, because, in our cohort, food insecurity significantly predicted children’s behavioral problems after controlling for mothers’ mental health and whether maternal mental illness was absent or present. Instead, it seems that maternal mental illness increased children’s risk for exposure to potentially harmful effects of food insecurity.
CONCLUSIONS
In a community sample of families, we found a 10% prevalence of food insecurity. Food insecurity most frequently occurred among families with limited socioeconomic resources, particularly those in which the mother experienced mental health problems such as depression, psychosis spectrum disorder, or domestic violence. Our finding strengthens the results of previous research, suggesting that maternal mental health problems are associated with food insecurity in multiple samples in Europe as well as in the United States.20,21 These mental health problems are frequent34,54,56,57 and disproportionately affect women in their prime childbearing and child-rearing years. By assessing the food situation of low-SES mothers who experience mental health problems or domestic violence,58 physicians may have an opportunity to identify families who are food-insecure and in which children are at risk for poor outcomes. There is now need for intervention studies to test whether improving mothers’ mental health may alleviate the impact of food insecurity on families with young children.
WHAT’S KNOWN ON THIS SUBJECT
Food insecurity, which is related to children’s behavioral and developmental problems, occurs most frequently in families with low socioeconomic position and low income; however, interventions that supplement families’ income or diet have not eradicated food insecurity.
WHAT THIS STUDY ADDS
Food insecurity seems to occur disproportionately among low-SES families in which the mother has mental health problems or experiences domestic violence. Decreasing the burden of food insecurity and its consequences on children may entail addressing mothers’ mental health needs.
ACKNOWLEDGMENTS
The E-Risk study is supported by the United Kingdom Medical Research Council (G9806489 and G0100527). Drs Moffitt and Caspi are Royal-Society Wolfson Research Merit Award holders.
We are grateful to the study participants and their parents. Our thanks go to Thomas Achenbach for kind permission to use the Child Behavior Checklist and to members of the E-Risk team for dedication and hard work.
ABBREVIATIONS
- SES
socioeconomic status
- E-Risk
Environmental Risk
- OR
odds ratio
- CI
confidence interval
Footnotes
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
REFERENCES
- 1.United Nations, Food and Agriculture Organization. Trade Reforms and Food Security. Rome, Italy: Food and Agriculture Organization; 2003. [Google Scholar]
- 2.Che J, Chen J. Food insecurity in Canadian households. Health Rep. 2001;12(4):11–22. [PubMed] [Google Scholar]
- 3.Evenson KR, Laraia BA, Welch VL, Perry AL. Statewide prevalences of concern about enough food, 1996–1999. Public Health Rep. 2002;117(4):358–365. doi: 10.1093/phr/117.4.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jyoti DF, Frongillo EA, Jones SJ. Food insecurity affects school children’s academic performance, weight gain, and social skills. J Nutr. 2005;135(12):2831–2839. doi: 10.1093/jn/135.12.2831. [DOI] [PubMed] [Google Scholar]
- 5.Rose D, Bodor JN. Household food insecurity and overweight status in young school children: results from the Early Childhood Longitudinal Study. Pediatrics. 2006;117(2):464–473. doi: 10.1542/peds.2005-0582. [DOI] [PubMed] [Google Scholar]
- 6.Whitaker RC, Phillips SM, Orzol SM. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006;118(3) doi: 10.1542/peds.2006-0239. Available at: www.pediatrics.org/cgi/content/full/118/3/e859. [DOI] [PubMed] [Google Scholar]
- 7.Food Standards Agency. [Accessed February 4, 2009];Review of existing UK work on food and low-income initiatives. Available at: www.food.gov.uk/multimedia/pdfs/lowincomefinalreport.pdf.
- 8.Molcho M, Gabhainn SN, Kelly C, Friel S, Kelleher C. Food poverty and health among schoolchildren in Ireland: findings from the Health Behaviour in School-aged Children (HBSC) study. Public Health Nutr. 2007;10(4):364–370. doi: 10.1017/S1368980007226072. [DOI] [PubMed] [Google Scholar]
- 9.Casey P, Goolsby S, Berkowitz C, et al. Maternal depression, changing public assistance, food security, and child health status. Pediatrics. 2004;113(2):298–304. doi: 10.1542/peds.113.2.298. [DOI] [PubMed] [Google Scholar]
- 10.Broughton MA, Janssen PS, Hertzman C, Innis SM, Frankish CJ. Predictors and outcomes of household food insecurity among inner city families with preschool children in Vancouver. Can J Public Health. 2006;97(3):214–216. doi: 10.1007/BF03405588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kleinman RE, Murphy JM, Little M, et al. Hunger in children in the United States: potential behavoral and emotional correlates. Pediatrics. 1998;101(1) doi: 10.1542/peds.101.1.e3. Available at: www.pediatrics.org/cgi/content/full/101/1/e3. [DOI] [PubMed] [Google Scholar]
- 12.Alaimo K, Olson CM, Frongillo EA. Food insufficiency and American school-aged children’s cognitive, academic, and psychosocial development [published correction appears in Pediatrics. 2001;108(3):824b. [PubMed] [Google Scholar]; Pediatrics. 2001;108(1):44–53. [PubMed] [Google Scholar]
- 13.Rose-Jacobs R, Black MM, Casey PH, et al. Household food insecurity: associations with at-risk infant and toddler development. Pediatrics. 2008;121(1):65–72. doi: 10.1542/peds.2006-3717. [DOI] [PubMed] [Google Scholar]
- 14.Ashiabi G, O’Neal K. A framework for understanding the association between food insecurity and children’s developmental outcomes. Child Dev Perspect. 2008;2:71–77. [Google Scholar]
- 15.Devaney BL, Ellwood MR, Love JM. Programs that mitigate the effects of poverty on children. Future Child. 1997;7(2):88–112. [PubMed] [Google Scholar]
- 16.UK Department of Health. [Accessed February 4, 2009];Healthy Start. Available at: www.healthystart.nhs.uk.
- 17.US Department of Agriculture, Food and Nutrition Service. [Accessed February 4, 2009];School meals. Available at: www.fns.usda.gov/cnd.
- 18.Free school lunches. [Accessed February 4, 2009]; Available at: www.directgov.uk/en/Parents/Schoolslearninganddevelopment/SchoolLife/DG_4016089/2009.
- 19.Murphy JM, Pagano ME, Nachmani J, Sperling P, Kane S, Kleinman RE. The relationship of school breakfast to psychosocial and academic functioning: cross-sectional and longitudinal observations in an inner-city school sample. Arch Pediatr Adolesc Med. 1998;152(9):899–907. doi: 10.1001/archpedi.152.9.899. [DOI] [PubMed] [Google Scholar]
- 20.Corcoran ME, Heflin CM, Siefert K. Food insufficiency and material hardship in post-TANF welfare families. Ohio State Law J. 1999;60:1395–1422. [Google Scholar]
- 21.Wehler C, Weinreb LF, Huntington N, et al. Risk and protective factors for adult and child hunger among low-income housed and homeless female-headed families. Am J Public Health. 2004;94(1):109–115. doi: 10.2105/ajph.94.1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moffitt TE E-Risk Study Team. Teen-aged mothers in contemporary Britain. J Child Psychol Psychiatry. 2002;43(6):727–742. doi: 10.1111/1469-7610.00082. [DOI] [PubMed] [Google Scholar]
- 23.Bennett N, Jarvis L, Rowlands O, Singleton N, Haselden L. Living in Britain: Results From the 1994 General Household Survey. London, United Kingdom: Her Majesty’s Stationary Office; 1996. [Google Scholar]
- 24.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Insecurity. Alexandria, VA: Office of Analysis, Nutrition, and Evaluation, Food and Nutrition Service, US Department of Agriculture; 2000. [Google Scholar]
- 25.Norris J, Scott R, Speiglman R, Green R. Homelessness, hunger and material hardship among those who lost SSI. Contemp Drug Probl. 2003;30:241–237. [Google Scholar]
- 26.Trzesniewski KH, Moffitt TE, Caspi A, Taylor A, Maughan B. Revisiting the association between reading achievement and antisocial behavior: new evidence of an environmental explanation from a twin study. Child Dev. 2006;77(1):72–88. doi: 10.1111/j.1467-8624.2006.00857.x. [DOI] [PubMed] [Google Scholar]
- 27.Caspi A, Moffitt TE, Thornton A, et al. The life history calendar: a research and clinical assessment method for collecting retrospective event-history data. Int J Methods Psychiatr Res. 1996;6:101–114. [Google Scholar]
- 28.Wilkinson GS. The Wide Range Achievement Test. 3rd ed. Wilmington, DE: Wide Range, Inc; 1993. [Google Scholar]
- 29.Rutter M, Caspi A, Fergusson D, et al. Sex differences in developmental reading disability: new findings from 4 epidemiological studies. JAMA. 2004;291(16):2007–2012. doi: 10.1001/jama.291.16.2007. [DOI] [PubMed] [Google Scholar]
- 30.Robins L, Cottler L, Bucholz K, Compton W. Diagnostic Interview Schedule for DSM-IV. St Louis, MO: Washington University School of Medicine; 1995. [Google Scholar]
- 31.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychological Association; 1994. [Google Scholar]
- 32.Kim-Cohen J, Moffitt TE, Taylor A, Pawlby SJ, Caspi A. Maternal depression and children’s antisocial behavior: nature and nurture effects. Arch Gen Psychiatry. 2005;62(2):173–181. doi: 10.1001/archpsyc.62.2.173. [DOI] [PubMed] [Google Scholar]
- 33.Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch Gen Psychiatry. 2000;57(11):1053–1058. doi: 10.1001/archpsyc.57.11.1053. [DOI] [PubMed] [Google Scholar]
- 34.Myin-Germeys IK, Krabbendam L, van Os J. Continuity of psychotic symptoms in the community. Curr Opin Psychiatry. 2003;16:443–449. [Google Scholar]
- 35.Selzer ML, Vinokur A, van Rooijen L. A self-administered Short Michigan Alcoholism Screening Test (SMAST) J Stud Alcohol. 1975;36(1):117–126. doi: 10.15288/jsa.1975.36.117. [DOI] [PubMed] [Google Scholar]
- 36.Skinner HA. The drug abuse screening test. Addict Behav. 1982;7(4):363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- 37.Crews TM, Sher KJ. Using adapted short MASTs for assessing parental alcoholism: reliability and validity. Alcohol Clin Exp Res. 1992;16(3):576–584. doi: 10.1111/j.1530-0277.1992.tb01420.x. [DOI] [PubMed] [Google Scholar]
- 38.Jaffee SR, Caspi A, Moffitt TE, Polo-Tomas M, Taylor A. Individual, family, and neighborhood factors distinguish resilient from non-resilient maltreated children: a cumulative stressors model. Child Abuse Negl. 2007;31(3):231–253. doi: 10.1016/j.chiabu.2006.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Straus MA. Measuring intrafamily conflict and violence: the Conflict Tactics (CT) scales. J Marriage Fam. 1979;41:75–88. [Google Scholar]
- 40.Koenen KC, Moffitt TE, Caspi A, Taylor A, Purcell S. Domestic violence is associated with environmental suppression of IQ in young children. Dev Psychopathol. 2003;15(2):297–311. doi: 10.1017/s0954579403000166. [DOI] [PubMed] [Google Scholar]
- 41.Moffitt TE, Caspi A, Krueger RF, et al. Do partners agree about abuse in the relationship? A psychometric evaluation of interpartner agreement. Psychol Assess. 1997;9:47–56. [Google Scholar]
- 42.Ehrensaft MK, Moffitt TE, Caspi A. Clinically abusive relationships in an unselected birth cohort: men’s and women’s participation and developmental antecedents. J Abnorm Psychol. 2004;113(2):258–270. doi: 10.1037/0021-843X.113.2.258. [DOI] [PubMed] [Google Scholar]
- 43.Achenbach T. Manual for the Child Behavior Checklist/4–18. Burlington, VT: University of Vermont Department of Psychology; 1991. [Google Scholar]
- 44.Achenbach T. Manual for Teacher’s Report Form and 1991 Profile. Burlington, VT: University of Vermont Department of Psychology; 1991. [Google Scholar]
- 45.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 46.Gjone H, Novik TS. Parental ratings of behaviour problems: a twin and general population comparison. J Child Psychol Psychiatry. 1995;36(7):1213–1224. doi: 10.1111/j.1469-7610.1995.tb01366.x. [DOI] [PubMed] [Google Scholar]
- 47.Kendler KS, Martin NG, Heath AC, Eaves LJ. Self-report psychiatric symptoms in twins and their nontwin relatives: are twins different? Am J Med Genet. 1995;60(6):588–591. doi: 10.1002/ajmg.1320600622. [DOI] [PubMed] [Google Scholar]
- 48.Levy F, Hay D, McLaughlin M, Wood C, Waldman I. Twin sibling differences in parental reports of ADHD, speech, reading and behaviour problems. J Child Psychol Psychiatry. 1996;37(5):569–578. doi: 10.1111/j.1469-7610.1996.tb01443.x. [DOI] [PubMed] [Google Scholar]
- 49.Okai D, Owen G, McGuire H, Singh S, Churchill R, Hotopf M. Mental capacity in psychiatric patients: systematic review. Br J Psychiatry. 2007;191:291–297. doi: 10.1192/bjp.bp.106.035162. [DOI] [PubMed] [Google Scholar]
- 50.Siefert K, Heflin CM, Corcoran ME, Williams DR. Food insufficiency and physical and mental health in a longitudinal survey of welfare recipients. J Health Soc Behav. 2004;45(2):171–186. doi: 10.1177/002214650404500204. [DOI] [PubMed] [Google Scholar]
- 51.Heflin CM, Siefert K, Williams DR. Food insufficiency and women’s mental health: findings from a 3-year panel of welfare recipients. Soc Sci Med. 2005;61(9):1971–1982. doi: 10.1016/j.socscimed.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 52.Bronte-Tinkew J, Zaslow M, Capps R, Horowitz A, McNamara M. Food insecurity works through depression, parenting, and infant feeding to influence overweight and health in toddlers. J Nutr. 2007;137(9):2160–2165. doi: 10.1093/jn/137.9.2160. [DOI] [PubMed] [Google Scholar]
- 53.Howard LM, Kumar R, Thornicroft G. Psychosocial characteristics and needs of mothers with psychotic disorders. Br J Psychiatry. 2001;178:427–432. doi: 10.1192/bjp.178.5.427. [DOI] [PubMed] [Google Scholar]
- 54.Centers for Disease Control and Prevention. [Accessed February 5, 2009];Intimate partner violence: overview. Available at: www.cdc.gov/ncipc/factsheets/ipvfacts.htm.
- 55.Danielson KK, Moffitt TE, Caspi A, Silva PA. Comorbidity between abuse of an adult and DSM-III-R mental disorders: evidence from an epidemiological study. Am J Psychiatry. 1998;155(1):131–133. doi: 10.1176/ajp.155.1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Andrews G, Poulton R, Skoog I. Lifetime risk of depression: restricted to a minority or waiting for most? Br J Psychiatry. 2005;187:495–496. doi: 10.1192/bjp.187.6.495. [DOI] [PubMed] [Google Scholar]
- 57.Archer J. Sex differences in aggression between heterosexual partners: a meta-analytic review. Psychol Bull. 2000;126(5):651–680. doi: 10.1037/0033-2909.126.5.651. [DOI] [PubMed] [Google Scholar]
- 58.Ramsay J, Richardson J, Carter YH, Davidson LL, Feder G. Should health professionals screen women for domestic violence? Systematic review. BMJ. 2002;325(7359):314. doi: 10.1136/bmj.325.7359.314. [DOI] [PMC free article] [PubMed] [Google Scholar]