Abstract
This prospective study investigated bacterial contamination of surgical gloves during small animal surgical procedures and factors associated with glove contamination. The outer surface of surgical gloves was sampled and cultured after completion of surgical procedures. Bacterial presence and numbers were recorded. Of 78 gloves sampled from 39 surgical procedures, bacterial contamination was noted in 16/78 (21%) gloves from 12/39 (31%) procedures. There was no difference in contamination of left or right hand glove [7/39 (18%) versus 9/39 (23%)], respectively (P = 0.78). There was no impact of glove type of left hand (P = 0.41), right hand (P = 0.44) or either hand (P = 0.26) contamination, or of surgical time (P = 0.71), dominant hand (P > 0.13), surgery type (orthopedic versus soft tissue versus neurological) (P > 0.42) or surgical wound classification (P > 0.11) on the incidence of contamination.
Résumé
Contamination bactérienne des gants portés par des chirurgiens pour petits animaux dans un hôpital d’enseignement vétérinaire. Cette étude prospective a étudié la contamination bactérienne des gants chirurgicaux durant les interventions chirurgicales pour petits animaux et les facteurs associés à la contamination des gants. La surface extérieure des gants chirurgicaux a été échantillonnée et une culture a été effectuée après la réalisation des interventions chirurgicales. La présence et la numération bactériennes ont été consignées. Parmi les 78 gants provenant de 39 interventions chirurgicales, la contamination bactérienne a été signalée dans 16/78 (21 %) gants provenant de 12/39 (31 %) interventions. Il n’y avait aucune différence au niveau de la contamination du gant gauche ou droit [7/39 (18 %) contre 9/39 (23 %)], respectivement (P = 0,78). Il n’y a eu aucun impact au niveau de la contamination quant au type de gant de la main gauche (P = 0,41), de la main droite (P = 0,44) ou de l’une ou l’autre main (P = 0,26) ou à la durée de la chirurgie (P = 0,71), à la main dominante (P > 0,13), au type de chirurgie (orthopédique contre tissus mous contre neurologique) (P > 0,42) ou à la classification de la plaie chirurgicale (P > 0,11) sur l’incidence de la contamination.
(Traduit par Isabelle Vallières)
Introduction
Surgical site infections (SSIs) occur in 0.8% to 18.1% of small animal surgical procedures and result in patient morbidity/mortality, increased treatment costs, extended hospitalization, and owner/veterinarian frustration (1–4). Multidrug resistant bacteria are commonly associated with these infections, which are challenging to eliminate (5). The pathophysiology of SSIs is complex and only partially understood, but a key component is contamination of the surgical wound with a bacterial pathogen. This can occur during or after surgery, and the relative importance of these is unclear. Intra-operative wound contamination occurs most commonly from microorganisms present on the patient’s skin and airborne operating room particles and a wide range of measures are used to reduce the risk. Contamination from the surgeon’s skin microbiota is another potential source of infection, one that is addressed through pre-surgical hand asepsis and surgical gloving. However, pre-surgical hand asepsis measures do not sterilize the skin, and gloves can be an imperfect barrier, so some risk persists.
Contaminated surgical gloves could be an important source of wound contamination because of the contact of gloved hands with the surgical site. In many procedures, the surgeon’s hands are in contact with the skin of the patient, which may result in bacterial contamination of gloves that could then be transferred to the wound. Contamination can also occur through inadvertent breaches in techniques (e.g., touching a non-sterilized surface) or from glove perforations that allow the surgeon’s commensal microbiota to contaminate external surfaces of the glove. Bacterial contamination of gloves has received little attention in veterinary medicine and may be an important factor in intra-operative wound contamination. The objectives of this study were to investigate the presence of bacterial contamination of surgical gloves during small animal surgical procedures and to determine factors associated with glove contamination.
Materials and methods
Data collection
A prospective study was performed from June to August 2012 at the Ontario Veterinary College Health Sciences Centre. Consecutive small animal surgical procedures over the study period were included in the study. Ophthalmologic, interventional radiologic, and dental procedures were excluded. Gloves from faculty, house officers (residents/interns), and senior veterinary students participating in the surgical procedure were collected. The study protocol was approved by the University of Guelph Research Ethics Board.
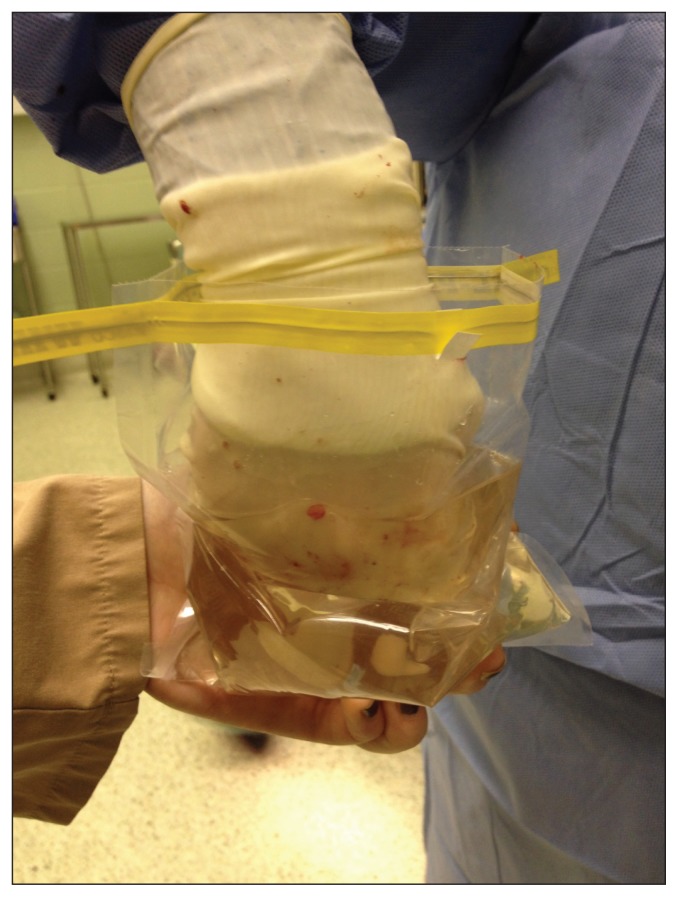
Standard protocols for presurgical hand asepsis involved a 5-minute surgical scrub with 4% chlorhexidine gluconate (BD E-Z Scrub; Becton, Dickinson and Co., Franklin Lakes, New Jersey, USA) or application of an alcohol-based hand rub (Avagard; chlorhexidine gluconate 1% solution and ethyl alcohol 61% w/w, 3M, St. Paul, Minnesota, USA) followed by open gloving in the operating room. Both gloves from each participant were sampled immediately following the completion of surgery. Surgeons placed each of their gloved hands into separate bags containing 100 mL of sterile phosphate-buffered saline (pH 7.2) which was thoroughly massaged through the outside of the bag (Figure 1). Gloves were then removed and filled with water to assess for perforation (6). Additional information collected included glove manufacturer and type, members of the surgical team (faculty/house officer/student), type of surgical procedure (soft tissue, neurologic, or orthopedic), dominant hand (left/right), surgical time (minutes), surgical wound classification (clean/clean-contaminated/contaminated/dirty), and intra-operative asepsis breaches (yes/no). Medical records of all cases were reviewed to determine if SSI occurred based on standard definitions as set forth by the US Centers for Disease Control and Prevention’s Hospital Infection Control Practices Advisory Committee (7).
Figure 1.
Image of glove sampling technique.
Bacterial enumeration
Immediately following sampling, 1 mL of the sample was inoculated onto Columbia sheep blood agar plates and incubated aerobically at 37°C for 24 h. Following incubation, visible colonies were counted and recorded.
Statistical analysis
Categorical data were evaluated by Fisher’s exact or chi-squared test. Logistic regression was used to assess the impact of surgical time on the incidence of contamination. Statistical analysis was performed on commercially available software (JMP statistical discovery; Cary, North Carolina, USA). A P-value of < 0.05 was considered significant.
Results
Gloves (n = 78) from 20 individuals in 39 surgical single procedures on dogs were sampled. These were categorized as 20 (51%) orthopedic, 18 (46%) soft tissue, and 1 (3%) neurological procedures. Twenty-four (62%) were classified as clean, 8 (21%) as clean-contaminated, 4 (10%) as contaminated, and 3 (7.7%) as dirty. No breaks in surgical asepsis were reported.
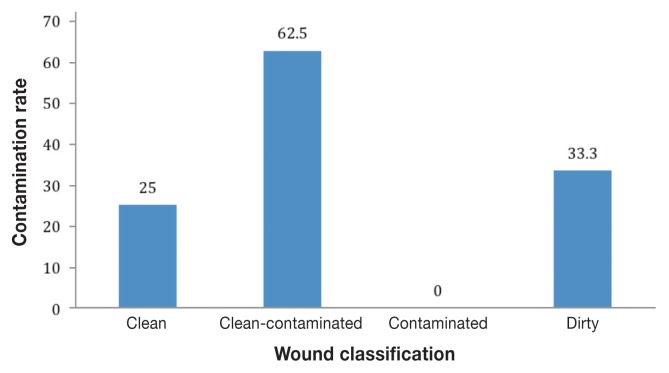
Bacterial contamination was noted on 16 (21%) gloves from 13 (33%) procedures. Contamination rates among the various classifications of surgical wounds are presented in Figure 2. Both gloves were contaminated for 3 (7.7%) procedures while single glove contamination was noted for 10 (26%) procedures. There was no difference in contamination of the left or right hand [7/39 (18%) versus 9/39 (23%), respectively (P = 0.78)].
Figure 2.
Glove contamination rates (percentages) among the various surgical wound classifications (P > 0.11).
Among contaminated gloves, contamination levels ranged from 20–930 colony forming units (CFUs) per 1 mL sample, which corresponds to 2000 to 93 000 CFUs/portion of glove surface sampled. Only 1 glove perforation was identified, the left glove from a dirty orthopedic procedure. No bacterial contamination was identified on that glove or the contralateral glove.
There was no impact of glove type on left hand (P = 0.41), right hand (P = 0.44) or either hand (P = 0.26) contamination. There was also no impact of surgical time (P = 0.71), dominant hand (P > 0.13), surgery type (orthopedic versus soft tissue versus neurological, P > 0.42) or surgical wound classification (P > 0.11) on the incidence of contamination. Surgical site infection was noted in 2/39 (5.1%) cases. Both were from clean orthopedic procedures [tibial plateau leveling osteotomy (TPLO)]. Glove contamination was present in 1 of these cases and glove perforation was not present in either case. There was no association between glove contamination and SSI, with SSI occurring in 1/12 cases (8%) where 1 or more individuals had contaminated gloves compared to 1/27 cases (4%) with non-contaminated gloves (P = 0.53).
Discussion
Sources of bacterial contamination of surgical wounds remain unclear. Despite routine protocols such as pre-surgical hand asepsis, surgical site preparation, and strict aseptic technique, 21% of surgical gloves in this study were contaminated with bacteria. This is a relatively high contamination rate of gloves worn by small animal surgeons, indicating that contamination of surgical wounds is likely a common occurrence with gloves being one source. Only 2 dogs developed SSI, both clean orthopedic procedures (TPLO), with 1 case noted to have glove contamination. Tibial plateau leveling osteotomy is a surgical procedure associated with a high SSI rate and reasons for this association are unknown. There was no statistical association between glove contamination and SSI; however, a study with a larger sample size is required to further evaluate this association.
Surgical time was not associated with bacterial contamination of gloves although it is expected that increased handling of the patients’ skin and exposure to the operating room air occur with longer surgical procedures. Surgical (and anesthesia) time has been previously associated with SSI in veterinary surgery (3) and additional study into this association is required.
Many human surgeons performing total joint replacement recommend double gloving followed by systematic outer glove renewals to limit intra-operative contamination of the surgical site and reduce the risk of exposure of the surgeon to blood borne pathogens (8–10). In 1 study, this practice rendered glove samples from subsequent stages during surgery negative for bacteria in 80% of cases (8). Additionally, a study by Ward et al (11) evaluating the effect of double gloving on subsequent contamination found that outer glove exchange 1 hour into a clean orthopedic procedure reduced the contamination rate from 23% to 10% (11). Based on the relatively high rate of glove contamination found in this study, similar recommendations should be considered in veterinary surgery for patients at high risk for SSI, particularly procedures in which an implant is placed.
A standardized technique for sampling surgical gloves does not exist; however, we may have underestimated the level of bacterial glove contamination. Other studies have used enrichment media to lower the threshold for bacterial detection. We did not use enrichment for bacterial growth, which allowed for enumeration but may have underestimated the incidence of bacterial contamination. There may have also been some residual action of chlorhexidine on hands or surgical gloves that had been in contact with the patient’s skin following presurgical asepsis, although the dilution that occurred during sampling likely negates any realistic impact. Future study of glove contamination should consider a combination of direct and enrichment methods, along with identification of recovered bacteria.
We found a relatively high level of bacterial contamination on surgeons’ gloves following a variety of small animal surgical procedures. Although SSIs in veterinary medicine likely have a multifactorial etiology, reducing intra-operative contamination of surgical wound is an important measure towards SSI prevention. The role of glove contamination and development of SSI is not fully established. Regardless, in patients at high risk of SSI or in surgical procedures where SSI would have devastating consequences (e.g., total joint arthroplasty), double gloving with periodic glove changes or removal of the outer glove prior to key points in the surgical procedure (e.g., handling of implant) should be considered to reduce intra-operative contamination of the surgical wound (11). CVJ
Footnotes
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Vasseur PB, Levy J, Dowd E, Eliot J. Surgical wound infection rates in dogs and cats data from a teaching hospital. Vet Surg. 1988;17:60–64. doi: 10.1111/j.1532-950x.1988.tb00278.x. [DOI] [PubMed] [Google Scholar]
- 2.Brown DC, Conzemius MG, Shofer F, Swann H. Epidemiologic evaluation of postoperative wound infections in dogs and cats. J Am Vet Med Assoc. 1997;210:1302–1306. [PubMed] [Google Scholar]
- 3.Nicholson M, Beal M, Shofer F, Brown DC. Epidemiologic evaluation of postoperative wound infection in clean-contaminated wounds: A retrospective study of 239 dogs and cats. Vet Surg. 2002;31:577–581. doi: 10.1053/jvet.2002.34661. [DOI] [PubMed] [Google Scholar]
- 4.Weese JS. A review of post-operative infections in veterinary orthopedic surgery. Vet Comp Orthop Traumatol. 2008;21:99–105. doi: 10.3415/vcot-07-11-0105. [DOI] [PubMed] [Google Scholar]
- 5.Weese JS. A review of multidrug resistant surgical site infections. Vet Comp Orthop Traumatol. 2008;21:1–7. doi: 10.3415/VCOT-07-11-0106. [DOI] [PubMed] [Google Scholar]
- 6.ASTM D5151 06 Standard Test Method for Detection of Holes in Medical Gloves. American Society of Testing and Materials; West Conshohocken, Pennsylvania, USA: [Google Scholar]
- 7.Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guidelines for prevention of surgical site infection. Infect Control Hosp Epidemiol. 1999;20:250–278. doi: 10.1086/501620. [DOI] [PubMed] [Google Scholar]
- 8.Beldame J, Lagrave B, Lievain L, Lefebvre B, Frebourg N, Dujardin F. Surgical glove bacterial contamination and perforation during total hip arthoplasty implantation: When gloves should be changed. Orthop Traumatol Surg Res. 2012;98:432–440. doi: 10.1016/j.otsr.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 9.McCue SF, Berg EW, Saunders EA. Efficacy of double-gloving as a barrier to microbial contamination during total joint arthroplasty. J Bone Joint Surg Am. 1981;63:811–813. [PubMed] [Google Scholar]
- 10.Tanner J, Parkinson J. Double gloving to reduce surgical cross-infection. Cochrane Database Syst Rev. 2002:CD003087. doi: 10.1002/14651858.CD003087. [DOI] [PubMed] [Google Scholar]
- 11.Ward WG, Cooper JM, Lippert D, Kablawi RO, Neiberg RH, Sherertz RJ. Glove and gown effects on intraoperative bacterial contamination. Ann Surg. 2014;259:591–597. doi: 10.1097/SLA.0b013e3182a6f2d9. [DOI] [PubMed] [Google Scholar]