Abstract
A 7-year-old dog was presented with a history of an open lesion on the right thoracic wall, discharging honey-like fluid and small stones. Ultrasonography and computed tomographic fistulography identified a cholecystocutaneous fistula; cholecystectomy was curative. Veterinarians should consider this disease in patients with long-term discharging lesions on the right thoracic or abdominal wall.
Résumé
Fistule cholécystocutanée contenant des cholélithes multiples chez un chien. Un chien âgé de 7 ans a été présenté avec une anamnèse de lésion ouverte sur la paroi thoracique droite, d’où s’écoulait un liquide ressemblant à du miel et de petits calculs. Une échographie et une fistulographie tomographique ont identifié une fistule cholécystocutanée et une cholécystectomie a guéri l’affection. Les vétérinaires devraient considérer cette maladie chez les patients ayant des lésions suppurantes de longue date sur la paroi thoracique ou abdominale droite.
(Traduit par Isabelle Vallières)
Spontaneous cholecystocutaneous fistula (CF) is defined as a rupture of the gallbladder through all layers of the abdominal wall with the formation of a fistulous tract that connects the gallbladder to the skin (1). Cholecystocutaneous fistula is rare in humans and may be secondary to abdominal trauma, previous abdominal surgery, gallbladder stones, and biliary malignancy (1). This report describes a spontaneous cholecystocutaneous fistula containing small gallstones in a dog.
Case description
A 7-year-old, 8.5 kg spayed female Cavalier King Charles spaniel was referred with a 2-month history of a chronic draining lesion on the right ventrolateral thorax. The dog had been treated with a 4-week course of amoxicillin and clavulanic acid (Synulox; Pfizer, Rome, Italy), 12.5 mg/kg body weight (BW), PO, q12h, but there was no resolution of the discharge. Physical examination of the dog revealed a subcutaneous mass (4 cm × 4 cm) along the caudal right ventrolateral thoracic wall, draining a “honey-like” fluid associated with some small stones. The rest of the physical examination was within normal limits. Cytological examination of the fluid revealed purulent exudate and the stones were sent for compositional analysis. Complete blood cell count and serum biochemistry were unremarkable. On ultrasonography, the wound contained echogenic fluid and small structures with acoustic shadowing. A fistulous tract containing mineralized foci was also visualized, which appeared to connect the subcutaneous wound to the apex of the gallbladder. The gallbladder contained apparently mineralized material.
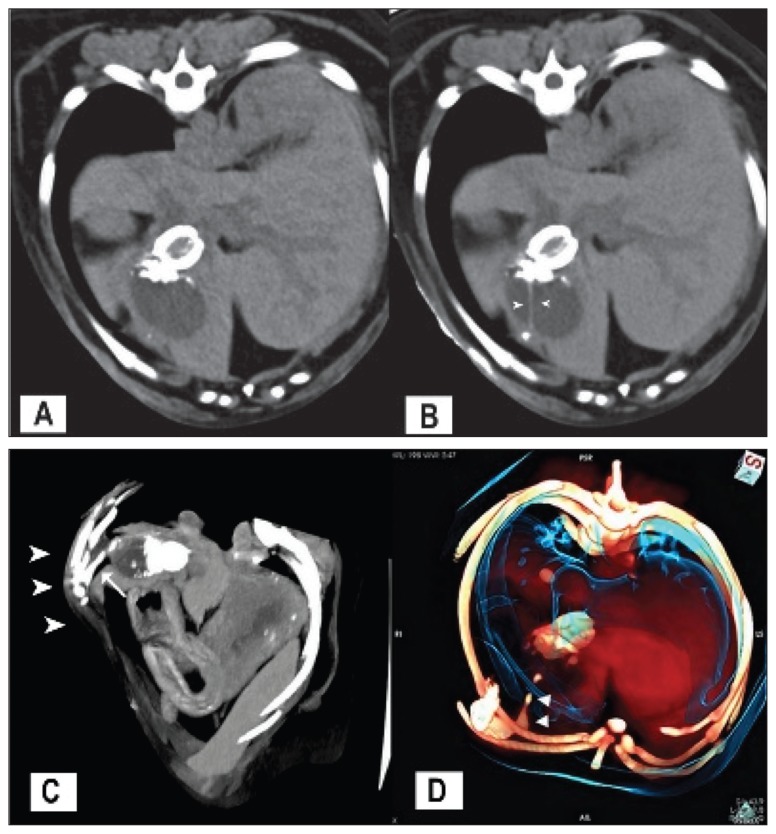
A tentative diagnosis of cholecystocutaneous fistula with chronic cholecystitis and cholelithiasis was made and radiographic fistulography was performed. Approximately 5 mL of a non-ionic iodinated contrast medium (Iopamidol 300 mgI/mL, Iopamiro 300; Bracco, Milan, Italy) was injected into the fistula opening and radiographs of the abdomen were obtained. Mineral opacities in the gallbladder were detected but the fistulogram failed to reveal a communication between the wound and the gallbladder. The dog was anesthetised and a computed tomographic (CT) scan of the caudal thorax and cranial abdomen was performed. Subsequently, a 26 G catheter tip was inserted directly into the draining tract under ultrasound guidance, and approximately 3 mL of contrast medium (Iopamidol 300 mgI/mL, Iopamiro 300; Bracco) diluted with sterile saline to a total iodine concentration of 150 mg/mL was injected. The CT fistulography revealed a single fistulous tract extending from the 10th intercostal space, running in contact with the diaphragm and connecting to the gallbladder apex, with a length of approximately 3.3 cm (Figure 1). Many gallstones of various dimensions were seen in the gallbladder lumen and in the fistulous tract. Adhesion of the apex of the gallbladder to the diaphragm was also noted. A diagnosis of cholecystocutaneous fistula was confirmed and laparotomy was performed.
Figure 1.
A — Computed tomographic image at the level of the 7th rib without contrast medium. The dog was positioned in dorsal recumbency. Many radiopaque gallstones are present in the dependent portion of the gallbladder. B — Same computed tomographic image as in (A) with contrast medium: the fistula is filled with contrast medium and a faint hyperdense line is seen within the gallbladder, representing a jet of contrast medium in the lumen (arrowheads). C — Maximum intensity projection ventro-lateral view of the cranial abdomen (the ventral-right part of the body is on the left, the dorsal-left part of the body is on the right): the fistulous tract is filled with contrast medium (arrow) connecting the subcutaneous space (arrowheads) to the gallbladder. D — Volume rendering oblique view of the fistulous tract extending from the 10th intercostal space into the gallbladder (arrowheads). The ventral-right part of the body is on the left; the dorsal-left part of the body is on the right.
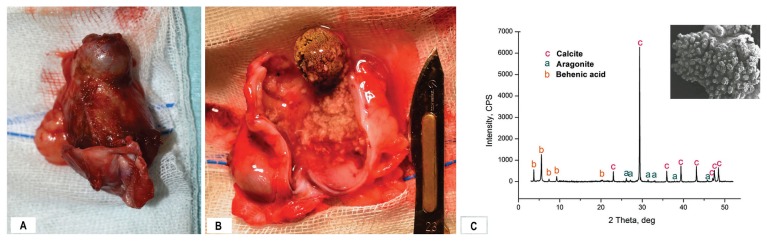
At surgery, a single fistulous tract was seen emanating from the right ventrolateral thoracic wall to above the costal margin, adherent to the diaphragm and entering into the gallbladder. The gallbladder wall appeared thickened, with adhesions to the abdominal wall, liver, omentum, and diaphragm. The largest calculus was apparently adherent to the infundibulum of the gallbladder (Figure 2). The adhesions were removed along with a portion of the diaphragm and a cholecystectomy was performed.
Figure 2.
A — Photograph of the gallbladder, a portion of the diaphragm and the fistulous tract after cholecystectomy, showing the largest calculus stuck in the infundibulum. B — The gallbladder is cut open and the choleliths are visible along with the honey-like content. C — Electron photomicrograph of a portion of the largest cholelith (JEOL JSM-6400 SEM) and X-ray diffraction pattern of the gallstone with phase identification.
Culture swabs of the fistulous tract and gallbladder yielded Escherichia coli, susceptible to amoxicillin/clavulanic acid. The gallbladder and the fistula were sent for histopathology. The dog was discharged on amoxicillin and clavulanic acid (Synulox, Pfizer), 12.5 mg/kg BW, PO, q12h for 4 wk.
Histopathology revealed neutrophilic and lymphoplasmacytic cholecystitis. The submucosa and the muscularis layers contained hemorrhagic areas. Small basophilic aggregations (presumed to be bile) were also seen in the mucosa. The fistulous tract was lined with fragments of hyperplastic epithelium resembling that of the bile duct. The biliary calculi were similar to the small stones exuding from the draining tract, showing an admixture of calcium carbonate, behenic acid, and cholesterol.
Physical examination, CBC and serum biochemistry after 1 wk, 2, 4, and 6 months were normal with no evidence of recurrence of the fistula.
Discussion
To our knowledge, this is the first report of cholecystocutaneous fistula containing gallstones in dogs. Only 1 case of spontaneous biliary tract cutaneous fistula and 1 case of cholecystocutaneous fistula have been reported in the veterinary literature (2,3).
In humans, CF is an uncommon complication of cholelithiasis, cholecystitis, gallbladder neoplasia, abdominal trauma or previous abdominal surgery (4–6). Women over the age of 60 are most commonly affected (5,7). External biliary fistulae can also occur as a result of intrahepatic abscesses or other inflammatory processes of the biliary tree (6). The presentation of CF typically involves a painless draining sinus tract in the right upper anterior side of the abdomen (8), as in the dog of this report. Other sites involved are left hypocondrium (the upper lateral abdominal region, overlying the costal cartilages), umbilicus, right lumbar region, left-side costal margin, gluteal region, right iliac fossa, right groin, or back (6,7,9). A CF may also form internally and involve viscera, without external communication (10). This condition in humans has been associated with increased pressure in the gallbladder secondary to cystic duct obstruction, caused by calculus or neoplasia. The increase in intraluminal pressure leads to impairment of the blood flow to the gallbladder, thus causing mural necrosis and perforation (11). The external opening of the fistula can be confused with a pyogenic granuloma, infected epidermal inclusion cyst, or metastatic carcinoma (7). Discharge from the fistula may be pus, bile, or mucus. Rarely gallstones may be present (12). In our case, the honey-like discharge was associated with the presence of stones. In humans this finding, if present, is highly suggestive for cholecystocutaneous fistula (3).
The dog herein had asymptomatic chronic cholecystitis with gallstones, which could have had a role in fistula formation. In fact, the largest calculus was found impacted in the infundibulum of the gallbladder, preventing the bile from flowing normally through the cystic duct. In humans, chronic inflammation of the gallbladder can cause the fundus to adhere to the abdominal wall, triggering the formation of a fistulous tract (13).
In humans, management of an external biliary fistula depends on the underlying etiology. The acute phase requires treatment with antibiotics, analgesia, and incisional drainage of the sinus abscess. In a proportion of patients the fistula will heal spontaneously; therefore, surgery may be avoided. Surgical options include cholecystostomy with removal of the gallstones or cholecystectomy (9). There are only 2 other cases described in the veterinary literature and therefore it is not possible to recommend an elective therapy. However, cholecystectomy and removal of the fistulous tract, associated with medical therapy, were successful and resulted in complete resolution of the disease in both of the reported cases.
Diagnosis of cholecystocutaneous fistula prior to surgery or histopathology might be difficult in dogs (2,3). Unlike the 2 previous reports, diagnostic imaging played an important role in the diagnosis in this case. Ultrasound was helpful in identifying the fistulous tract and CT fistulography confirmed a communicating tract between the external sinus and the gallbladder. It was important to inject the contrast medium directly in the fistulous tract in order to visualize its path. In fact, when the contrast medium was injected into the opening of the lesion for the radiographic study, it did not enter the fistulous tract, probably because of the inability to diffuse in the narrow lumen.
Cholecystocutaneous fistula should be suspected in dogs with a discharging wound on the right thoracic or abdominal wall if ultrasonographic examination reveals mineral content in the sinus and in the gallbladder. Computed tomographic fistulography with the contrast medium injected directly into the fistulous tract may be advisable and may help in surgical planning, resulting in a less invasive surgical approach. Evaluation of the composition of calculi draining from the wound can also provide valuable information on the diagnosis and the etiopathogenesis of cholelithiasis. CVJ
Footnotes
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Ioanndis O, Paraskevas G, Kotronis A, et al. Spontaneous cholecystocutaneous fistula draining from an abdominal scar from previous surgical drainage. Ann Ital Chir. 2012;83:67–69. [PubMed] [Google Scholar]
- 2.Kligman KC, Jehn CT, Davis KM, Taylor DP, Conway JA. Spontaneous external biliary fistula in a dog. J Am Vet Med Assoc. 2007;231:919–923. doi: 10.2460/javma.231.6.919. [DOI] [PubMed] [Google Scholar]
- 3.Marquardt SA, Rochat MC, Johnson-Neitman JL. Spontaneous cholecystocutaneous fistula in a dog. J Am Anim Hosp Assoc. 2012;48:43–49. doi: 10.5326/JAAHA-MS-715. [DOI] [PubMed] [Google Scholar]
- 4.Andley M, Biswas RS, Ashok S, Somshekar G, Gulati SM. Spontaneous cholecystocutaneous fistula secondary to calculous cholecystitis. Am J Gastroenterol. 1996;91:1656–1657. [PubMed] [Google Scholar]
- 5.Birch BRP, Cox SJ. Spontaneous external biliary fistula uncomplicated by gallstones. J Postgrad Med. 1991;67:391–392. doi: 10.1136/pgmj.67.786.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nicholson T, Born MW, Garber E. Spontaneous cholecystocutaneous fistula presenting in the gluteal region. J Clin Gastroenterol. 1999;28:276–277. doi: 10.1097/00004836-199904000-00024. [DOI] [PubMed] [Google Scholar]
- 7.Hoffman L, Beaton H, Wantz G. Spontaneous cholecystocutaneous fistula: A complication of neglected biliary tract disease. J Am Geriatr Soc. 1982;30:632–634. doi: 10.1111/j.1532-5415.1982.tb05059.x. [DOI] [PubMed] [Google Scholar]
- 8.Mimin J, Watkins R. Spontaneous cholecystocutaneous fistulae secondary to calculous cholecystitis. Br J Clin Pract. 1993;47:341–342. [PubMed] [Google Scholar]
- 9.Flora HS, Bhattacharya S. Spontaneous cholecystocutaneous fistula. HPB. 2001;3:279–280. doi: 10.1080/136518201753335584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reed MWR, Tweedie JH. Spontaneous simultaneous internal and external biliary fistulae. Br J Surg. 1985;72:538. doi: 10.1002/bjs.1800720712. [DOI] [PubMed] [Google Scholar]
- 11.Cruz RJJ, Nahas J, De Figueiredo LF. Spontaneous cholecystocutaneous fistula: A rare complication of gallbladder disease. Sao Paulo Med J. 2006;124:234–236. doi: 10.1590/S1516-31802006000400012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abril A, Ulfohn A. Spontaneous cholecystocutaneous fistula. South Med J. 1984;77:1192–1193. doi: 10.1097/00007611-198409000-00039. [DOI] [PubMed] [Google Scholar]
- 13.Vasanth A, Siddiqui A, O’Donnell K. Spontaneous cholecystocutaneous fistula. South Med J. 2004;97:183–185. doi: 10.1097/01.SMJ.0000051150.63130.E8. [DOI] [PubMed] [Google Scholar]