Introduction
The overuse of tests and procedures due to fear of malpractice litigation, known as defensive medicine,1 is estimated to cost $46 billion annually in the US,2 but these costs have been measured only indirectly. We estimated the cost of defensive medicine on three hospital medicine services in a health system by having physicians assess the defensiveness of their own orders. We hypothesized that physicians who were concerned about being targeted by litigation would practice more defensively and have higher overall costs.
Methods
We studied hospitalists at one tertiary care (Baystate Medical Center) and two community hospitals (Baystate Franklin Medical Center and Baystate Mary Lane Hospital). All hospitalists (n=42) were invited to complete a survey regarding demographic information and attitudes toward defensive medicine. We then showed physicians their orders placed the previous day and asked them to indicate the extent to which each represented defensive medicine—tests, procedures, or hospitalization performed primarily because of concern about malpractice liability—using a 5-point scale from 0 (not at all defensive) to 4 (completely defensive). Itemized order costs including daily room and board costs were obtained from the hospital's cost accounting system.
The outcomes were the percentage of orders and hospital costs due to defensive medicine. We examined the percentage of orders rated defensive (≥1) and completely defensive (4 only). The defensiveness score for each order was converted to a proportion (e.g. 1/4=0.25) and multiplied by the order's cost to estimate the cost attributable to defensive medicine. Defensive costs were summed and divided by the total cost of all rated items.
We examined the relationship between physicians’ cost due to defensive medicine and expressed attitudes about lawsuits. Using multivariable regression we examined the association between higher levels of defensiveness (> 10% of orders considered defensive) and order volume and costs.
Results
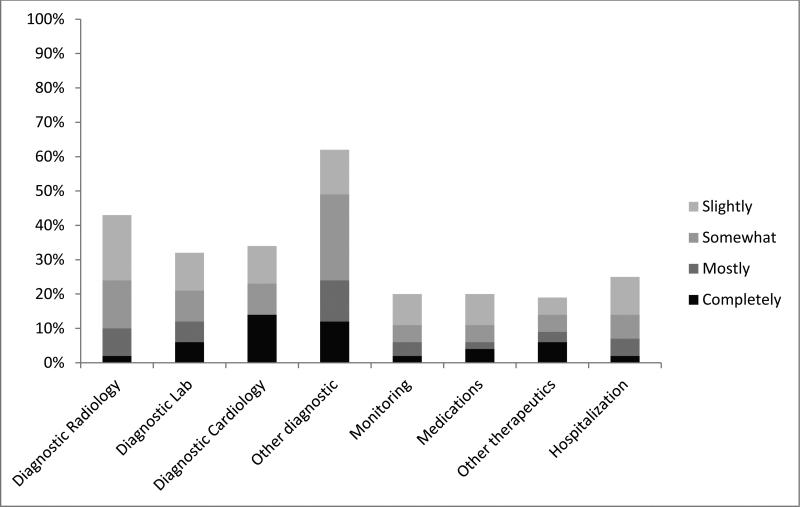
Of the 42 physicians, 39 agreed to participate; 36 (92%) completed surveys and rated 4215 orders for 769 patients. The median orders per patient was 3 (IQR 2 to 7); and per physician was 97 (IQR 61 to 141). Of the orders, 28% were defensive (Figure 1). Four physicians identified no defensive orders and 21 physicians rated at least 1 as mostly defensive (range 1% to 77%). As compared to physicians with fewer defensive orders, physicians with ≥10% defensive orders placed a similar number of orders (5.4 vs. 4.9, p=0.68) and generated similar costs per patient ($1679 vs. $1700, p=0.89).
Figure 1.
Proportion of orders deemed to be defensive by order type.
Average cost was $1695 per patient (95% CI $1566, $1824), of which $226 (13%) was defensive. Completely defensive orders represented 2.9% of costs, primarily through additional hospital days (figure 2). Physician factors—gender, training, litigation concerns—were not associated with defensive orders or costs (data not shown).
Figure 2.
Proportion of Hospital Costs Due to Defensive Medicine
Discussion
In this study of hospital medicine services at 3 institutions in a health system, 28% of orders and 13% of costs were judged to be at least partially defensive, but only 2.9% of costs were completely defensive. Most costs were due to potentially unnecessary hospitalization. Defensive medicine practices varied substantially, but physicians who wrote the most defensive orders spent less than those who wrote fewer such orders, highlighting the disconnect between physician beliefs about defensive medicine and their contribution to costs.
In 2008, Massachusetts internists reported that 27% of CT scans, 16% of laboratory tests and 14% of hospital admissions were ordered due to concerns about liability.3 We allowed our physicians to offer a graded response, which revealed that defensiveness is not absolute. Compared to the previous study, our respondents reported higher percentages of defensive medicine, but lower percentages of completely defensive medicine (2% of radiology, 6% of laboratory testing and 2% of hospital days).
Limitations of our study include its subjective nature, lack of anonymity, small sample size, and the inclusion of only hospital medicine services at three hospitals in one health system.
In conclusion, although a large portion of hospital orders had some defensive component, our study found that few orders were completely defensive, and that physicians’ attitudes about defensive medicine did not correlate with cost. Our findings suggest that only a small portion of medical costs might be reduced by tort reform.
Contributor Information
Michael B. Rothberg, Center for Value-based Care Research Medicine Institute, Cleveland Clinic, Cleveland, OH.
Joshua Class, Howard University College of Medicine Washington, DC.
Tara F. Bishop, Division of Outcomes and Effectiveness, Department of Public Health Division of General Internal Medicine, Department of Medicine Weill Cornell Medical College, New York, NY.
Jennifer Friderici, Division of Academic Affairs Baystate Medical Center, Springfield, MA.
Reva Kleppel, Department of Medicine, Baystate Medical Center, Springfield, MA.
Peter K. Lindenauer, Center for Quality of Care Research Baystate Medical Center, Springfield, MA.
References
- 1.Young PL, Olsen L. The Healthcare Imperative:Lowering Costs and Improving Outcomes: Workshop Series Summary. The National Academies Press; 2010. [PubMed] [Google Scholar]
- 2.Mello MM, Chandra A, Gawande AA, Studdert DM. National costs of the medical liability system. Health affairs. 2010 Sep;29(9):1569–1577. doi: 10.1377/hlthaff.2009.0807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Massachusetts Medical Society Investigation of Defensive Medicine in Massachusetts. 2008 [Google Scholar]