Abstract
A substantial disparity exists in the prevalence and effective self-management of diabetes among African Americans in the United States. Community-level programs have the potential to affect self-efficacy and may be helpful in overcoming common barriers to self-management. The Neighborhood Health Talker Program used community members trained as cultural health brokers to engage their communities in conversations about “living diabetes well.” Program evaluators used mixed methods to analyze post-conversation surveys and Health Talker field notes. These indicated an increase in diabetes-related knowledge and increased confidence among conversation participants. Conversations included discussion of barriers and facilitators to lifestyle changes and effective self-management that are frequently overlooked in a clinical setting.
Rates of chronic diseases such as type 2 diabetes are increasing in the general U.S. population.1 The burden and prevalence of type 2 diabetes is experienced disproportionately by African Americans in the United States, resulting in more frequent extreme adverse outcomes, including amputation, blindness, and premature death.2–9 This disparity may be, in part, the result of a lack of access to adequate information about how to self-manage diabetes and a reticence among this population to ask questions of their health care providers (HCPs).10–12 Additionally, the poverty experienced disproportionately by African Americans is associated with exposure to numerous deleterious health risks, including poor access to adequate health care. When health care is available (e.g, safety net HCPs), African Americans and other marginalized populations often delay seeking treatment because of the cost, perceived discrimination, and perceived inadequacy of treatment.13,14 As a result, many chronic diseases, including type 2 diabetes, are often diagnosed at more advanced stages in African-American populations than in non-Hispanic white populations,15 and African Americans with type 2 diabetes are more likely to suffer the aforementioned complications. For this reason, diabetes prevention and self-management education efforts need to target this high-risk population.
Wide-scale adoption of healthy eating habits, sufficient physical activity, screen-time reduction, nonsmoking, stress reduction, and regular medical check-ups could prevent an enormous number of chronic disease–related deaths each year. However, individual behavior change happens within a multifaceted sociocultural context, and, thus, programs that effectively promote behavior change are those that adequately address social context and account for cultural nuances.16–19 Diabetes prevention and self-management programs that accomplish this include group visits for minority and disadvantaged patients with diabetes to improve self-management and promote greater trust in medical providers,20 home health care interventions for vulnerable populations,21 and peer coaches from similar economic circumstances.22 Similarly, programs employing community health workers, family health advocates, or cultural health brokers have improved diabetes self-management and patient-physician relationships.10,23,24
The approach presented in this article—cultural health brokering—has been documented as an effective approach to reducing disease outcome disparities in study populations.10,23,24 Cultural health brokers are individuals who are knowledgeable in a particular sociocultural context and who advocate on behalf of individuals or groups by providing health information in culturally sensitive ways and serving as a mediator between community members and the health care sector.25 Cultural health brokers need not be experts on any particular health topic; however, they must be equipped with the ability to navigate the health care system and find answers to health-related questions. They have a lived cultural context in which to translate cultural misconceptions and cultural euphemisms. They also may have the ability to tap into resources and elicit information that may otherwise be missed. Community conversations led by cultural health brokers emphasize the common community experience and provide a venue for people who share similar cultural norms to discuss their experiences and work collaboratively to troubleshoot their problems. Because minority populations are frequently disenfranchised from many institutions and services, including health care services, cultural health brokers may be an integral way to acceptably reconnect them.24
Building on successful cultural health broker models25 to address the health disparities experienced in Buffalo, N.Y., the Erie Niagara Area Health Education Center (ENAHEC) in 2009 pilot-tested the Neighborhood Health Talker Program, with evaluation assistance from the Primary Care Research Institute (PCRI) within the Department of Family Medicine at the State University of New York (SUNY) at Buffalo. The Health Talker program was an initiative in which African-American members of medically underserved communities received diabetes-specific cultural health broker training developed by the authors to work within their communities to improve access to health information and diabetes self-management skills.26 The aim of this pilot was to examine the potential of a model to improve community members’ knowledge and access to diabetes information and promote activation of diabetes self-management skills. This article presents the results of a program evaluation assessing the content and community perception of Health Talker–led community conversations centered on diabetes knowledge, prevention, and self-management.
Study Methods
Study setting
The city of Buffalo had a poverty rate in 2010 of 29.6%.27 Poverty in the city is most heavily concentrated on the east and west sides of the city, and 15 of the city’s 79 census tracts have poverty rates > 40%.25 This poverty disproportionately affects the city’s racial and ethnic minorities; 81.4% of African Americans in the city live in high-poverty neighborhoods.27 Nearly the entire downtown region of Buffalo is categorized as both a Health Professional Shortage Area and a Medically Underserved Area. This includes seven entire zip codes and portions of four additional zip codes.28 In a recent health risk appraisal study, ∼ 17% of residents in the east side of Buffalo had diabetes.29 This is the highest rate in the entire Western New York region.
ENAHEC piloted the Neighborhood Health Talker Program in Buffalo in 2009 during a 6-month period. PCRI was contracted to conduct a program evaluation of this pilot. PCRI evaluation staff received approval from the SUNY at Buffalo Social and Behavioral Sciences institutional review board for the analysis and publication of de-identified program evaluation data.
Study population
Health Talkers.
Neighborhood Health Talkers were members of the east side community to which the health information was targeted. Community members who were active in various area community organizations were recruited by ENAHEC through formal presentations at block club meetings, housing projects, and community centers and through word of mouth and then interviewed for participation in the training program. This pilot program included 12 women and 1 man ranging in age from 35 to > 65 years of age, all of whom self-identified as black/African American. The majority had at least a 4-year college degree. The methodology for recruitment and training of the cultural health brokers has been described elsewhere.26 Health Talkers were compensated for their time and signed consent forms allowing for the analysis of their de-identified written conversation summaries.
Conversation participants.
The people who participated in conversations led by Health Talkers about diabetes prevention and self-management were community members primarily from within the Health Talkers’ personal spheres. For example, Health Talkers who frequented a senior community center engaged conversation participants there, and a Health Talker who led a youth summer health education camp spoke with the youths about diabetes prevention and self-management. Other groups included workplace peers, members of area churches, and Health Talkers’ friends and family members.
Program Design
Health Talkers participated in 20 hours of formal training during 1 week that addressed skills and methods in leadership and cultural health brokering, basic diabetes knowledge, and health literacy.26 The curriculum was approved by Buffalo State College for continuing professional education credit. Instruction about diabetes knowledge was led by J.S.R., who has been trained as a master trainer in the Stanford Chronic Disease Self-Management Program and the Stanford Diabetes Self-Management Program. Additionally, two Health Talker trainees were practicing nurses (a licensed practical nurse and a registered nurse), who offered additional instructional support. Training materials were compiled from American Diabetes Association resources,30 the International Curriculum for Diabetes Health Professional Education,31 and Diabetes for Dummies.32
After training, each Health Talker led at least five community conversations between July and October 2009 about “living diabetes well.” These were held in churches, community centers, housing projects, and other places where people gather. Some Health Talkers held spontaneous conversations during their daily activities (e.g., one Health Talker led a conversation during a family gathering, and another led one with her church choir group when they were together for practice). Additionally, the Health Talkers established a resource library in their community that consisted of information about HCPs, diabetes self-management tips, recipe cards and cookbooks, and other relevant healthy-living information.26
To ensure the integrity of the training and provide additional support to the Health Talkers during this time, the Health Talkers, program leaders, and evaluators met monthly. At these meetings, the group debriefed about the conversations and discussed successes and difficulties experienced by the Health Talkers. These meetings were not recorded, nor was content systematically collected by the project team.
Health Talkers approached each conversation prepared with certain topics but allowed the group to set the pace and determine the major areas of focus. These conversations were designed to be unstructured. Health Talkers usually began conversations with questions such as, “What is diabetes?” or “What does it mean to have diabetes?” and then let the participants guide the discussion, maintaining a position as a reference or resource but allowing conversations to develop naturally. Many of the youth conversations began with a viewing of the film So Leroy Has Diabetes from the Keisha and Friends series developed by ENAHEC. This is an animated illustration of a child learning about his diagnosis and coming to terms with it with the help of his friends. The conversations lasted anywhere from 30 minutes to 2 hours and ranged in size from 3 to 15 participants. Health Talkers occasionally opted to lead conversations jointly.
Data collection
The evaluation of the pilot program used mixed methods. Qualitative data included Health Talker written summaries of conversation content. Quantitative data included community member conversation participant demographics and perceptions of the conversation’s impact on their knowledge of diabetes and self-management techniques. These two data types are described in more detail below.
Health Talker written conversation summaries.
The Health Talkers documented each community conversation with written summaries submitted to ENAHEC that included the number of participants, location, date, time, and primary discussion topics.
Anonymous survey of conversation participants.
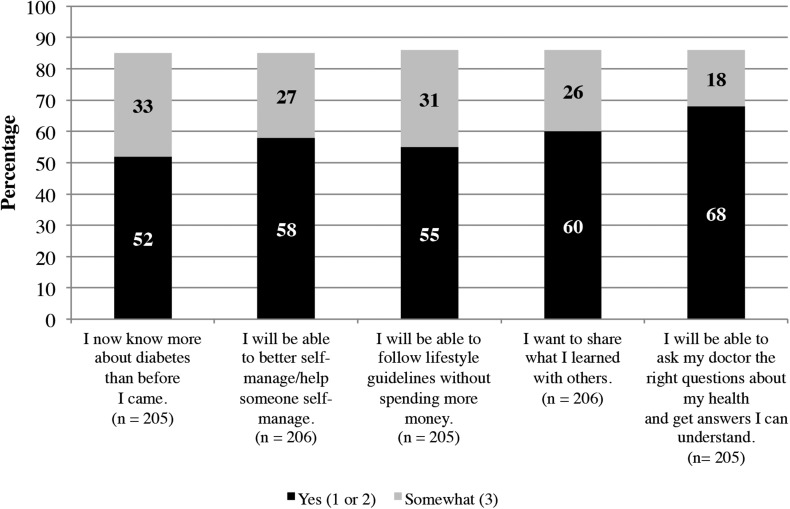
Immediately after the conversations, Health Talkers asked community members to voluntarily complete anonymous written evaluations designed to elicit their feedback on the conversation experience. Demographic information, including age, sex, formal educational level, and experience with diabetes, was also collected. These 10-item surveys included five questions using a 5-point Likert scale querying knowledge gained during the conversation, personal and family diabetes status, and demographics. The variables are shown in Table 1 and Figure 1.
Table 1.
Demographics and Diabetes Status of a Sample of Community Conversation Participants (n = 208)
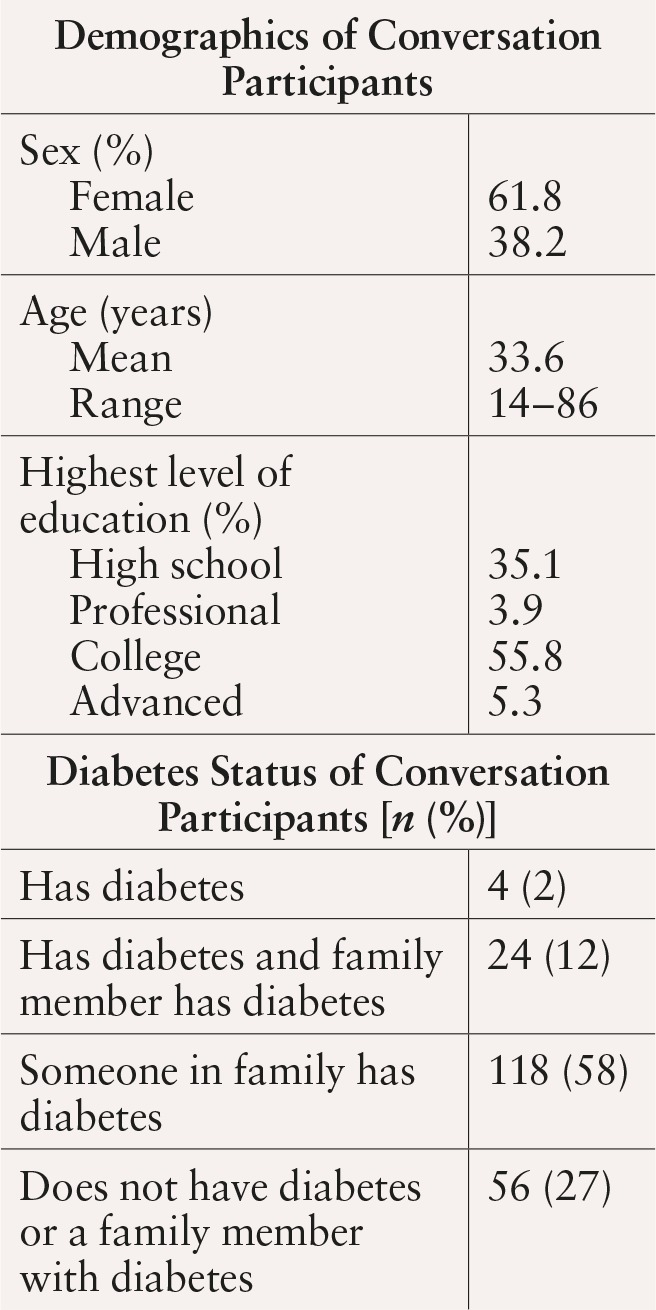
Figure 1.
Community conversation respondents’ perceptions of conversation impact on diabetes knowledge and confidence (scale of 1–5).
The survey was developed by the program leaders, who are members of the community to which the pilot program was targeted. Program evaluators were able to advocate for the inclusion of demographic information to analyze responses by population subgroups. The anonymous surveys were deemed exempt from requiring informed consent because the content was benign, and the surveys were anonymous. Evaluators accessed only de-identified program evaluation data from the program leaders.
Children as young as 14 years of age voluntarily completed the surveys. Children < 14 years of age often participated in the conversations but were not asked by the Health Talkers to complete the survey. Because this was a community program rather than a rigorous research study, survey administration was somewhat inconsistent, as indicated by the number of surveys (n = 208) compared to the estimated number of conversation participants (> 700).
Data analysis
Health Talker written conversation summaries.
The program team compiled all written conversation summaries and analyzed them for major themes using an immersion-crystallization approach. This qualitative analytic approach consists of a systematic iterative process of text interpretation and categorization to establish patterns of significance.33 To ensure rigor and quality, two anthropologists (R.B.C. and B.M.V.) reviewed the conversation summaries independently to identify the predominant topics covered within each of the Health Talker community conversations. They then developed a list of all the topics or themes along with descriptive information and categorized them by consensus. Analysts reviewed each written summary in its entirety to search for additional information, particularly Health Talker documentation of community members’ self-management strategies, misconceptions, and key concerns. Interpretive disagreements were discussed and resolved by presenting supportive evidence. Finally, the findings were shared with the program leaders from ENAHEC (M.C. and J.S.R.), who confirmed the identified themes.
Anonymous survey of conversation participants.
Evaluators entered the 208 conversation evaluation surveys completed into Microsoft Excel 2010 (Microsoft, Redmond, Wash.) and imported the data into SPSS Statistics for Windows, version 17.0. (SPSS, Inc., Chicago, Ill.) to identify frequencies of and relationships among responses (e.g., the percentage of respondents with diabetes who feel confident in their ability to self-manage their diabetes). The evaluators performed χ2 analyses to identify whether differences between subgroups were significant.
Study Results
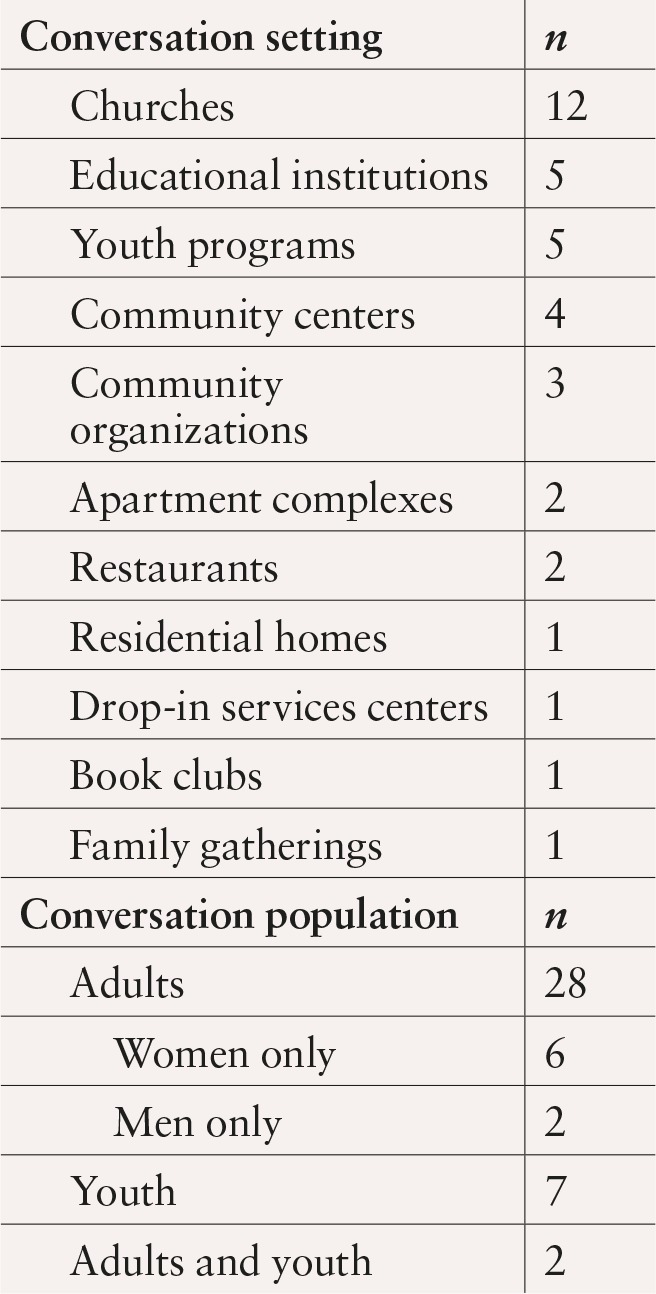
Health Talkers submitted conversation evaluations and summaries to the program leaders on a biweekly basis in person or via e-mail. Each of the Health Talkers engaged in at least five conversations, but because of joint leadership of several conversations, there were a total of 37 individual conversations. These conversations reached > 700 people in a variety of settings (Table 2). Participating community members included people of all age-groups and several races, ethnicities, and socioeconomic groups. The characteristics of the 208 participants who completed a conversation evaluation are shown in Table 1. Seventy-seven responding participants were < 20 years of age, 73 were 20–49 years of age, and 50 were > 50 years of age.
Table 2.
Health Talker Conversation Settings (n = 37)
More than 80% of respondents indicated that the community conversation had a positive effect on their knowledge and confidence about diabetes and diabetes self-management (Figure 1). Of note, 60% said they would like to share what they learned with others, and 68% answered that they “will be able to ask my doctor the right questions about my health and get answers I can understand.”
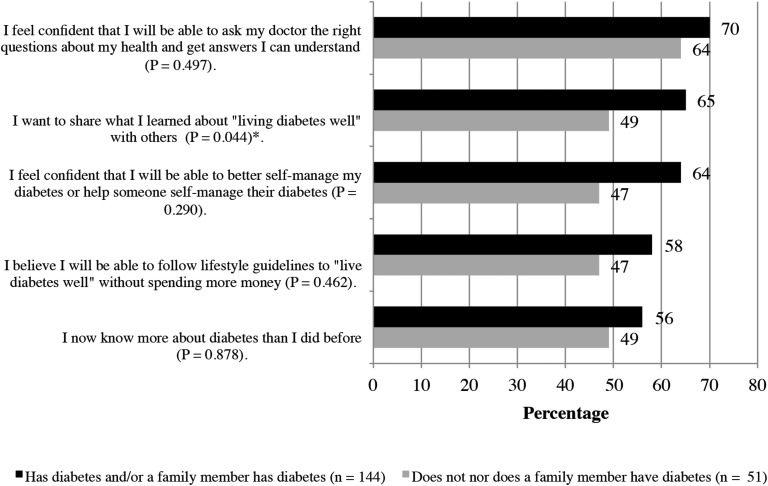
Responses to these questions varied by subgroup. For example, when compared to respondents who reported no personal experience with diabetes (themselves or family) (n = 51), a greater proportion of those with personal experience (n = 144) answered “yes” (1 or 2 on a 5-point scale) to a question asking whether they felt more confident that they will be able to better self-manage their diabetes or help someone they love to better self-manage their diabetes (P = NS). This subgroup also more frequently reported that they wanted to share what they learned about “living diabetes well” with others (P = 0.044) (Figure 2). Differences between the responses of males and females were neither substantial nor significant. Differences by age were also not substantial, with the exception of a tendency for older respondents (≥ 60 years of age) to be more likely to indicate their desire to share what they learned with others (79% answered “yes” [1 or 2] among those ≥ 60 years of age compared to 53–64% in other age-groups).
Figure 2.
Diabetes knowledge and confidence (1 or 2 on a 5-point scale) by personal experience with diabetes (n = 195).
Predominant conversation themes
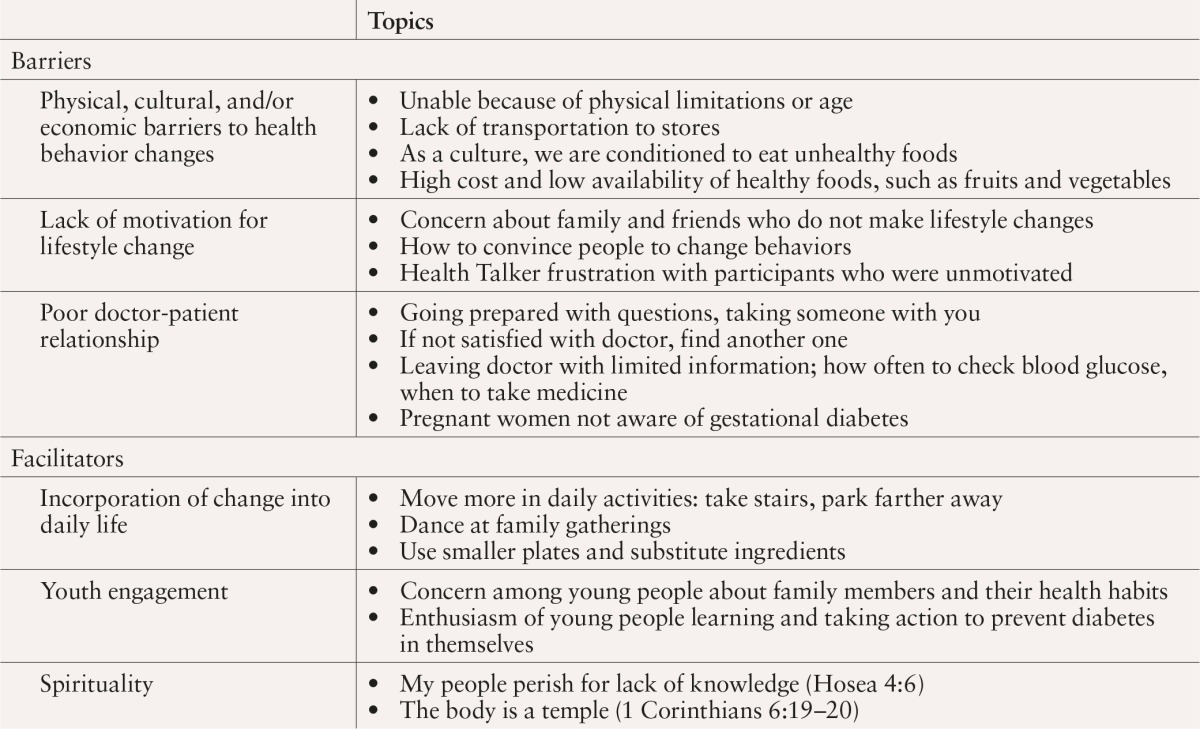
Health Talker summaries ranged in degree of detail from bulleted lists to multiple paragraphs. According to these written summaries, the conversations covered a wide range of topics related to diabetes, including disease-related knowledge and understanding, self-management, healthy lifestyles, and health care. The summaries also revealed several barriers to and facilitators of managing diabetes effectively (Table 3). Participants discussed barriers to lifestyle changes and effective self-management, including economic, cultural, and physical barriers to healthy eating and physical activity; difficulty motivating self or others to change; and poor doctor-patient communication. The facilitators of effective diabetes management discussed included making small changes in daily life, youth engagement, and spirituality.
Table 3.
Barriers to and Facilitators of Effectively Managing Diabetes (or “Living Diabetes Well”)
Barriers to effective diabetes management
Physical, economic, and cultural barriers to lifestyle change.
Although participants often said that they try to walk more, physical limitations frequently made exercising on a regular basis a difficult goal to attain. This was especially true for elderly people. As one Health Talker reported in her notes:
“One of the ladies had bad knees but walked when she could . . . . One lady used a walker to get around . . . although she could do exercise such as lifting her hands. The other two ladies also could do exercises while sitting down.”
The goal of eating healthy was also challenging for economic and cultural reasons. One participant noted, “It seems as though as a culture we are conditioned to eat unhealthy foods. At Thanksgiving, the menu is always the same: macaroni and cheese, dressing . . . .” With regard to economic barriers, one Health Talker wrote in her conversation notes:
“The participants were saying that it’s hard for them to get low-cost fruits and vegetables. We talked about trying stores such as Save-A-Lot, Aldi’s, and Price Rite, which tend to have lower-cost fruits and vegetables. They said that cost and accessibility were still problems for them and for the poor with diabetes . . . . They said that transportation to the stores is a big problem for the poor. The question was asked, ‘How do we make things more accessible for people who are diabetic, poor, with other illnesses and are motivated to eat well?’”
Health Talkers’ summaries indicate that they attempted to address some of these concerns by making suggestions for lower-cost food options, providing cooking classes or healthy low-cost food during the conversations, and stocking resource libraries with healthful cookbooks and recipe cards.
Lack of motivation to change.
Health Talkers’ summaries revealed a desire among participants to help motivate family and friends with or at risk for diabetes to make healthy lifestyle choices. Children were eager to learn what they could do to support parents with diabetes. Health Talkers reported that they frequently addressed the question of how to motivate someone who was resistant to change. One Health Talker wrote:
“They have accepted the disease for what it is, and they did not think they could change the mindset of family members or friends who have the disease. We explained some small things that could be done, for instance, dietary changes, movements around the house that constitute exercise that is not vigorous, and the biggest is change in attitude toward our health by taking charge.”
Another Health Talker similarly wrote:
“There was conversation about one of the group’s family members, who is a registered nurse who has not bought into ‘living diabetes well.’ I was able to pick up on the frustration the person was having, ‘It’s my mom, she’s a nurse, she knows what to do, but she won’t.’”
In addition, conversation notes frequently reflected frustration on the part of the Health Talkers regarding some participants’ unwillingness to make lifestyle changes that would improve their health. Concerning her own frustration with the conversation participants, another Health Talker wrote:
“One woman monitors [her husband’s] sugar, his diet, etc., but she does not have a doctor following her and does not regularly monitor her own sugar. When I questioned her as to why not, she said, ‘I know when it’s high or low and what to do,’ but she was noncompliant if any person ever were! How can you know if you don’t test yourself or even go to a doctor? I . . . urged her to take better care of herself.”
As these comments illustrate, participants and Health Talkers alike often expressed frustration with people who express no interest in losing excess weight or making lifestyle changes, and both groups found this problem difficult to solve.
Poor doctor-patient communication.
Conversations frequently included comments showing that the quality of communication between medical providers and patients during office visits was a major concern. One of the community members described her frustration about her most recent doctor’s appointment. She detailed the last office visit, where she had learned of her diagnosis. Because the visit was drawing to a close with no discussion about her previous test results, she asked the doctor about them. He walked out to check the results. Shortly thereafter, a woman walked back in, handed her three prescriptions, and provided no explanation. She had to seek out the information, which she found to be difficult to access. She realized that she needed to change doctors and described that process as difficult as well. “Finding a doctor is like a new marriage,” she said. “You have to get used to a new man.”
Health Talkers’ summaries indicated that they emphasized the need for patients to develop a proactive stance toward their own care, actively seeking doctors with whom they could form good relationships and approaching medical visits prepared with lists of questions. Health Talkers reported that they or other participants suggested bringing family or friends to appointments to assist in remembering the information. The importance of doctor-patient communication was common in Health Talker notes, with phrases such as, “Open up, talk to them, don’t be intimidated. The doctor is responsible for answering your questions” appearing frequently.
Facilitators of effective diabetes management
Incorporation of change into daily life.
Several Health Talkers noted that, when it came to talking about diet and exercise, participants were able to identify ways in which they could make small changes that would help incorporate healthy eating and activity into their daily lives. For example, participants discussed doing more movement around the house for exercise, using smaller amounts of oil in recipes, using smaller plates, using turkey sausage as an alternative to traditional sausage, parking farther away from their destination, having walking meetings, dancing at family gatherings, and using stairs. One Health Talker noted:
“We discussed ways to include being active and making healthy food choices in their everyday lives. The group was able to provide examples of what they are able to do to be more active: walking, using the stairs, and I encouraged the group to just move more, dance a little, and have fun.”
Youth engagement.
Nine community conversations included youths, ranging in age from 5 to 17 years. Health Talkers who worked with these youths reported an unexpected enthusiasm and a high level of preexisting knowledge about the topics of diabetes and healthy living. Summaries indicated that some youths expressed anxiety about getting diabetes because their family members had it. Many youths had relatives with diabetes and expressed great concern for their health, as well as a strong desire to help family members manage their condition. One Health Talker documented this by writing:
“The kids were impressive. Some of them talked about helping grandma or mom test their blood or reminding them to test their blood. They talked about eating healthy foods and exercising . . . . They were helpful in teaching each other, and it was encouraging to know they had such a broad knowledge base.”
Another Health Talker reported that one young girl demonstrated her understanding of healthy living by saying, “All you have to do is eat right and exercise, and you will be OK. That goes for everybody.” The Health Talkers’ summaries of youth conversations reflect their perceptions of an encouraging level of motivation among youths to help their families and to make healthy life choices to prevent diabetes.
Spirituality.
Some Health Talkers conducted conversations in church settings. Using spiritual contexts became a powerful way in which these Health Talkers could establish a point of reference. Health Talkers and participants referenced biblical scripture to support the adoption of healthy living habits and self-management of diabetes. The most commonly cited Bible passages for supporting healthy lifestyles and self-care were, “My people perish for lack of knowledge” (Hosea 4:6; full text reads “My people are destroyed [perish] from lack of knowledge. Because you have rejected knowledge, I reject you from being a priest to me.”34) and “The body is a temple” (1 Corinthians 6:19–20; full text reads “Do you not know that your body is a temple of the Holy Spirit, within you, which you have from God? You are not your own; you were bought at a price. So glorify God with your body.”34) Health Talkers reported that these passages were useful in reminding participants and their loved ones of a person’s responsibility to take care of their God-given bodies. Health Talkers also reported using prayer at the beginning and end of conversations to help situate the conversation within a spiritual space.
Discussion
The Health Talkers’ community conversations reached > 700 people of all ages at the community level. These conversations brought the issue of “living diabetes well” into the broader community context, rather than focusing on the specific circumstances surrounding individual patients. They addressed health at the level of the whole community, regardless of whether members had personal experience with or knowledge of diabetes.
The conversations were a source of both expected and unexpected knowledge. The Health Talker model functioned well within this community, as shown by the large numbers of conversation participants and naturally occurring, unscheduled conversations with family members and friends. The Health Talkers trained in this project seemed to benefit from the trust people had in them, resulting from existing relationships and associations.
The model, which relied on word-of-mouth health information being shared by people who understand the audience because they are a part of the audience, was effective at improving health knowledge among underserved populations. Initial evaluations reflected a perceived increase in knowledge, confidence, and self-efficacy and a desire to share the information learned with others. Health Talkers shared many anecdotes about successes as a result of the conversations. In the future, the program leaders and Health Talkers may consider following up with conversation participants to find out whether they did share the information with others.
The community conversations also provided insights into health knowledge, health communication, and community-level barriers to and facilitators of living healthy lifestyles in underserved communities. Community members, and particularly young people, came to the table with more knowledge than expected, but also with concerns that centered on the system, delivery of care, and resource allocation. Of notable concern was the frustration regarding how to motivate themselves and others to live healthy lives when knowledge was not enough.
Knowledge of diabetes and healthy life choices was provided and emphasized through the community conversations, and the community members were eager to discuss these matters and learn new information. However, the conversations also illuminated participants’ concerns regarding how to implement their knowledge of healthy lifestyle choices and diabetes self-management practices. This element was not always effectively addressed through the conversations, as reflected in the reported frustration of the Health Talkers.
Significantly, the finding that participants who had firsthand experience with diabetes learned more and felt more confident with the material after the community conversation indicates an increased level of engagement that arises from receiving personal, relatable information that can be directly applied to their lived experience. This suggests that education at the community and individual level needs to be relevant and personal to maximize participants’ motivation to integrate it into their lives.
Future research should seek to determine whether participating community members engaged in healthy behaviors at an increased and sustained rate after their participation in these community conversations. Similar studies of community health worker–implemented interventions have scheduled 3-, 6-, and/or 12-month follow-up surveys to determine whether changed knowledge and behaviors are sustained.35–37
In addition, contained within the conversation themes are possible areas that may merit further exploration when planning future clinical and educational interventions. First is the role of youths, and second is spirituality. The prevalence of these two themes within the conversation notes indicates that cultural health brokers who are members of the target community may be uniquely suited to tap into these areas as important aspects of daily life that are often overlooked in traditional health interventions. Exploring both of these areas could offer fertile ground for acknowledging the fuller social/cultural context in which people prioritize decisions about their health.
As noted, the community youths who participated in these conversations were knowledgeable and enthusiastic. Their role as forces for change within families is a potentially untapped asset that should be explored further. The presence of children in the household as a motivator for lifestyle changes has been explored in other health-related areas, such as smoking cessation,38–40 and preliminary results suggest that setting an example for children and protecting children’s health can be powerful motivators for parents to make healthy lifestyle changes.40 Burke et al.16 reported that women sometimes showed greater self-efficacy in health behaviors when acting on behalf of their children than for themselves, indicating further that family relationships may serve as a catalyst for the promotion of positive health behaviors.
The role of spirituality as a motivator for change and self-care in this community cannot be overlooked. Studies of spirituality as it relates to health care among similar populations have demonstrated that spirituality has the potential to have strong mediating effects on individuals’ self-management of chronic conditions,41–44 including diabetes. Specifically, spirituality has been noted as an important element of consideration when working with African-American populations,41,45 such as the one in this study. A belief that God gives individuals the strength needed to manage their diabetes may increase efficacy in and motivation for effective self-management and the adoption of healthy lifestyles. The role of community workers, churches, and other programs in promoting spirituality as part of overall health and as a catalyst for healthy living and effective self-management of chronic diseases such as diabetes is frequently neglected in a clinical setting. This should be explored further and incorporated, as appropriate, into community-based interventions in a more systematic and thoughtful way.
Study limitations
Because this was a small pilot of a community-based program, there were a number of limitations, which are described below.
Sample limitations.
The small sample size of Health Talker trainees is a limitation of this study. Also, the small response to the optional anonymous survey by conversation participants (208 of > 700) limits the conclusions that can be drawn from this analysis. Similarly, the program was confined geographically to one region. Therefore, the results may not be generalizable to similar populations in other parts of the country, where community, spirituality, and family dynamics may play different roles in health and self-management.
The willingness of community members to participate in conversations implies an interest in the topic and thus may mean the sample was slightly biased. This was partially mediated by the fact that some conversations took place in preexisting groups of people who were present for other reasons (e.g., choir, summer camp, or a family gathering).
Limitations to conversation summaries.
The community conversations were not audio-recorded given that many African-American communities distrust the research and health care sectors and may not speak candidly when being audio-recorded. This means that summaries were based on Health Talker recall of the conversations, which varied in detail, accuracy, and length for a variety of reasons, including the length of the time lapse between holding a conversation and summarizing it. To partially address this, the program leaders encouraged Health Talkers to write their summaries immediately after each conversation, although this did not occur in all cases.
Limitations to the survey.
The anonymous survey was designed by the program staff and did not incorporate a validated instrument (e.g., querying diabetes attitudes, diabetes-related distress, physical and psychological functioning, and diabetes self-care behaviors). This approach could have made the evaluation more comparable to other studies and should be considered in future implementations of this program.
Finally, in completing the post-conversation survey, respondents may have been inclined to provide what they perceived as the desired response (e.g. “Yes” to “I now know more about diabetes than before I came”). The program leaders and evaluators hoped to reduce this risk of social desirability by using anonymous surveys.
Limitations to identified themes.
It is important to note that the conversations in which spirituality was a prevalent theme were conducted in churches with congregation members, who would presumably have a more vested interest in spirituality as it relates to their health care. Caution must be taken when exploring the role of spirituality, which is highly individualized. This speaks to a need for personalized education that is sensitive to the social context in which it is presented and to individual preferences.
Given these limitations, the results point to considerations that should be explored as potential factors in other populations. Addressing these limitations primarily through future improvements in outreach and data collection procedures may result in more reliable results and meaningful conclusions. For example, while maintaining the community-based, sometimes impromptu nature of the conversations, Health Talkers may still be able to implement brief pre- and post-conversation surveys based on validated instruments (e.g., the Summary of Diabetes Self-Care Activities scale).35,46 Future surveys may also include questions about food and physical activity behaviors, as well as self-reported height and weight (to calculate BMI).35–37 To understand the population’s experience with diabetes more fully, Health Talkers could ask how many years have passed since participants or their family members with diabetes were diagnosed and also ask about their medication regimen.35 In the absence of access to medical records, Health Talkers may be able to ask participants who report having diabetes to share their latest A1C values during the conversation and ask again at follow-up. Although all of these approaches still rely on self-report rather than medical records or onsite measurement, they would elicit more information that would also be comparable to other similar community-based programs.
Study implications
Low-cost initiatives such as the Health Talkers program could be reproduced easily in other communities and have the potential to tap into areas such as youth engagement and spirituality that are traditionally missing from clinical encounters. Diabetes education, to be truly effective, should address the social, spiritual, and economic circumstances of people with diabetes in a holistic and encompassing way to enhance perceived self-efficacy and motivation to manage diabetes well.
Cultural health brokering models such as the one presented here may offer an effective and cost-efficient model for addressing some of these factors in ways that are relevant, impactful, and culturally appropriate for the target community. Trained neighborhood Health Talkers could be situated to address not only disease prevention and self-management, but also motivational techniques, whole-family engagement, spiritual support, and other mechanisms that may increase patients’ self-efficacy in the successful application of self-management techniques in their daily lives. This may ultimately promote more effective collaborative approaches to health behavior change and a reduction in the rates and burdens of chronic diseases such as diabetes.
Acknowledgments
This project was made possible by funding from a legacy grant from Bronx Health REACH/New York Center of Excellence to Eliminate Disparity. The authors are grateful for the participation of the Health Talkers in collecting data and sharing their personal experiences. Additionally, community members who participated in conversations with Health Talkers have offered a wealth of insight that can inform chronic disease self-management interventions.
References
- Centers for Disease Control and Prevention: Percentage of civilian, noninstitutionalized population with diagnosed diabetes, by age, United States, 1980–2010. Available from http://www.cdc.gov/diabetes/statistics/prev/national/figbyage.htm. Accessed 5 March 2013
- Biello KB, Rawlings J, Carroll-Scott A, Browne R, Ickovics JR: Racial disparities in age at preventable hospitalization among U.S. adults. Am J Prev Med 38:54–60, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonsalves WC, Gessey ME, Mainous AG, 3rd, Tilley BC: A study of lower extremity amputation rates in older diabetic South Carolinians. J S C Med Assoc 103:4–7, 2007 [PubMed] [Google Scholar]
- Holman KH, Henke PK, Dimick JB, Birkmeyer JD: Racial disparities in the use of revascularization before leg amputation in Medicare patients. J Vasc Surg 54:420–426, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamps JL, Hempe JM, Chalew SA: Racial disparity in A1C independent of mean blood glucose in children with type 1 diabetes. Diabetes Care 33:1025–1027, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk JK, D’Agostino RB, Bell RA, Passmore LV, Bonds DE, Karter AJ, Narayan KMV: Disparities in HbA(1c) levels between African-American and non-Hispanic white adults with diabetes: a meta-analysis. Diabetes Care 29:2130–2136, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine DA, Allison JJ, Cherrington A, Richman J, Scarinci IC, Houston TK: Disparities in self-monitoring of blood glucose among low-income ethnic minority populations with diabetes, United States. Ethn Dis 19:97–103, 2009 [PubMed] [Google Scholar]
- Peek ME, Cargill A, Huang ES: Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev 64 (5 Suppl.):101S–156S, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitson HE, Hastings SN, Landerman LR, Fillenbaum GG, Cohen HJ, Johnson KS: Black-white disparity in disability: the role of medical conditions. J Am Geriatr Soc 59:844–850, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heisler M, Spencer M, Forman J, Robinson C, Shultz C, Palmisano G, Graddy-Dansby G, Kieffer E: Participants’ assessments of the effects of a community health worker intervention on their diabetes self-management and interactions with healthcare providers. Am J Prev Med 37 (Suppl. 1):S270–S279, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shavers VL, Lynch CF, Burmeister LF: Racial differences in factors that influence the willingness to participate in medical research studies. Ann Epidemiol 12:248–256, 2002 [DOI] [PubMed] [Google Scholar]
- Young M, Klingle RS: Silent partners in medical care: a cross-cultural study of patient participation. Health Comm 8:29–53, 1996 [DOI] [PubMed] [Google Scholar]
- Becker G: Deadly inequality in the health care “safety net”: uninsured ethnic minorities’ struggle to live with life-threatening illnesses. Med Anthropol Quart 18:258–275, 2004 [DOI] [PubMed] [Google Scholar]
- Becker G, Newsom E: Socioeconomic status and dissatisfaction with health care aomong chronically ill African Americans. Am J Public Health 93:742–748, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckles GL, Zhu J, Moonesinghe R: Diabetes—United States, 2004 and 2008. In Centers for Disease Control and Prevention: CDC Health Disparities and Inequalities Report: United States 2011. MMWR 60 (Suppl.):90–93, 2011 [PubMed] [Google Scholar]
- Burke NJ, Bird JA, Clark MA, Rakowski W, Guerra C, Barker JC, Pasick RJ: Social and cultural meanings of self-efficacy. Health Educ Behav 36 (5 Suppl.):111S–128S, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke NJ, Joseph G, Pasick RJ, Barker JC: Theorizing social context: tethinking behavioral theory. Health Educ Behav 36 (5 Suppl.):55S–70S, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frohlich KL, Corin E, Potvin L: A theoretical proposal for the relationship between context and disease. Sociol Health Ill 23:776–797, 2001 [Google Scholar]
- Krumeich A, Weijts W, Reddy P, Meijer-Weitz A: The benefits of anthropological approaches for health promotion research and practice. Health Educ Res 16:121–130, 2001 [DOI] [PubMed] [Google Scholar]
- Clancy DE, Brown S, Magruder KM, Huang P: Group visits in medically and economically disadvantaged patients with type 2 diabetes and their relationships to clinical outcomes. Top Health Inf Manage 24:8–14, 2003 [PubMed] [Google Scholar]
- Nguyen DL, DeJesus RS: Home health care may improve diabetic outcomes among non-English speaking patients in primary care practice: a pilot study. J Immigr Minor Health 13:967–969, 2011 [DOI] [PubMed] [Google Scholar]
- Ghorob A, Vivas MM, De Vore D, Ngo V, Bodenheimer T, Chen E, Thom DH: The effectiveness of peer health coaching in improving glycemic control among low-income patients with diabetes: protocol for a randomized controlled trial. BMC Public Health 11:208, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt CW, Grant JS, Appel SJ: An integrative review of community health advisors in type 2 diabetes. J Comm Health 36:883–893, 2011 [DOI] [PubMed] [Google Scholar]
- Otero-Sabogal R, Arretz D, Siebold S, Hallen E, Lee R, Ketchel A, Li J, Newman J: Physician-community health worker partnering to support diabetes self-management in primary care. Qual Prim Care 18:363–372, 2010 [PubMed] [Google Scholar]
- National Center for Cultural Competence, Georgetown University Center for Child and Human Development, Georgetown University Medical Center: Bridging the Cultural Divide in Health Care Settings: The Essential Role of Cultural Broker Programs. U.S. Department of Health and Human Services 2004. Available from http://nccc.georgetown.edu/documents/Cultural_Broker_Guide_English.pdf. Accessed 28 January 2013 [Google Scholar]
- Cadzow R, Craig M, Rowe J, Kahn L: Transforming community members into diabetes cultural health brokers: the Neighborhood Health Talker Project. Diabetes Educ 39:102–110, 2013 [DOI] [PubMed] [Google Scholar]
- Partnership for the Public Good: Key facts about poverty in Buffalo-Niagara metropolitan region. Available from http://www.ppgbuffalo.org/wp-content/uploads/2012/03/Key-Facts-About-Poverty-in-Buffalo-Niagara-Metropolitan-Region.pdf. Accessed 11 June 2012
- Health Resources and Services Administration Data Warehouse. 2012. Available from http://www.hrsa.gov/shortage. Accessed 28 June 2012
- Public Health Observatory, Department of Family Medicine: The Western New York Health Risk Assessment (HRA) Update, 2004–2005. Buffalo, N.Y., Western New York Public Health Alliance, 2005 [Google Scholar]
- American Diabetes Association: Living with diabetes. Available from http://www.diabetes.org/living-with-diabetes. Accessed 5 March 2009
- International Diabetes Federation: International Curriculum for Diabetes Health Professional Education. 2nd ed. Brussels, Belgium, International Diabetes Federation, 2008 [Google Scholar]
- Rubin AL: Diabetes for Dummies. 3rd ed. Hoboken N.J., Wiley Publishing, 2009 [Google Scholar]
- Borkan J: Immersion/crystallization. In Doing Qualitative Research. 2nd ed. Crabtree BF, Miller WL, Eds. Thousand Oaks, Calif, Sage Publications, 1999, p. 179–194 [Google Scholar]
- Division of Christian Education of the National Council of the Churches of Christ in the United States of America: Revised Standard Version of the Bible. 1952. University of Michigan Digital Collections. Available from http://quod.lib.umich.edu/r/rsv/browse.html. Accessed 10 June 2012 [Google Scholar]
- Spencer MS, Rosland A-M, Kieffer EC, Sinco BR, Valerio M, Palmisano G, Anderson M, Guzman JR, Heisler M: Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health 101:2253–2260, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanaya AM, Santoyo-Olsson J, Gregorich S, Grossman M, Moore T, Stewart AL: The Live Well, Be Well study: a community-based, translational lifestyle program to lower diabetes risk factors in ethnic minority and lower-socioeconomic status adults. Am J Public Health 102:1551–1558, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valen MS, Narayan S, Wedeking L: An innovative approach to diabetes education for a Hispanic population utilizing community health workers. J Cult Div 19:10–17, 2012 [PubMed] [Google Scholar]
- Halterman JS, Borrelli B, Conn KM, Tremblay P, Blaakman S: Motivation to quit smoking among parents of urban children with asthma. Patient Educ Couns 79:152–155, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen LJ, Noach MB, Winickoff JP, Hovell MF: Parental smoking cessation to protect young children: a systematic review and meta-analysis. Pediatrics 129:141–152, 2012 [DOI] [PubMed] [Google Scholar]
- Thomson G, Wilson N, Weerasekera D, Edwards R: Strong smoker interest in ‘setting an example to children’ by quitting: national survey data. Aust N Z J Public Health 35:81–84, 2011 [DOI] [PubMed] [Google Scholar]
- Casarez RLP, Engebretson JC, Ostwald SK: Spiritual practices in self-management of diabetes in African Americans. Holist Nurs Pract 24:227–237, 2010 [DOI] [PubMed] [Google Scholar]
- Harvey IS: Self-management of a chronic illness: an exploratory study on the role of spirituality among older African American women. J Women Aging 18:75–88, 2006 [DOI] [PubMed] [Google Scholar]
- Polzer RL: African Americans and diabetes: spiritual role of the health care provider in self-management. Res Nurs Health 30:164–174, 2007 [DOI] [PubMed] [Google Scholar]
- Polzer RL, Miles MS: Spirituality in African Americans with diabetes: self-management through a relationship with God. Qual Health Res 17:176–188, 2007 [DOI] [PubMed] [Google Scholar]
- Rahim-Williams B: Beliefs, behaviors, and modifications of type 2 diabetes self-management among African American women. J Natl Med Assoc 103:203–215, 2011 [DOI] [PubMed] [Google Scholar]
- Fitzgerald JT, Davis WK, Connell CM, Hess GE, Funnell MM, Hiss RG: Development and validation of the Diabetes Care Profile. Eval Health Prof 19:208–230, 1996 [DOI] [PubMed] [Google Scholar]