Diabetes is a chronic disease characterized by high blood glucose levels and caused either by a deficiency of insulin or a defect in the way the body responds to insulin.1,2 The increased prevalence of type 2 diabetes is believed to be the consequence of an aging population, increased physical inactivity and obesity, and genetic factors.3,4 Diabetes is one of the leading causes of blindness and renal failure,5,6 and people with diabetes who have an increased A1C level and uncontrolled lipid levels have increased rates of morbidity and mortality. Complications usually fall into three main groups: acute metabolic abnormalities, microvascular anomalies, and long-term cardiovascular disorders specific to diabetes.7
The main treatment goals for diabetes are controlling blood glucose and cholesterol levels and maintaining a normal blood pressure.8 Tight control and management of blood glucose and blood pressure has been proven to prevent or delay complications of diabetes.9 Involving patients in their care through self-management is of utmost importance to achieving these goals. Yet, self-management is difficult to attain and maintain because of the complexity of the processes involved and the lack of motivation and skills on the part of some patients.10 Frequently reported barriers to self-management11,12 include knowledge deficits, poor patient-provider communication, low self-efficacy, limitations of time or resources, financial constraints, lack of individualized and coordinated care, and lifestyle differences among family members. An extensive review of 16 studies identified barriers from five different perspectives: psychosocial, socioeconomic, physical, environmental, and cultural.13
It is widely believed that educating patients about diabetes may be a mechanism to encourage and support them in assuming active responsibility for self-management. Based on this belief, several educational programs have been developed.14,15 Diabetes education, also known as diabetes self-management training (DSMT) or diabetes self-management education (DSME), has been defined as a collaborative process through which people with diabetes gain the knowledge and skills needed to modify behavior and successfully self-manage the disease and its related conditions.16,17 It is an ongoing, interactive process involving a person with diabetes and a team of educators, including nurses, dietitians, and pharmacists. Such interventions aim to help patients achieve optimal health and better quality of life, reducing the need for costly health care by preventing or postponing complications.
Despite the belief in, and popularity of, diabetes education, our current understanding is inconclusive regarding the effectiveness of an educational approach in patients with type 2 diabetes. A meta-analysis of 31 studies looking at the effect of self-management education on glycemic control found little evidence in support of such education programs.18 A recent qualitative review of 80 studies conducted from 2004 to 2007 revealed mixed results,19 but many studies reported positive changes. The reported positive results of diabetes education with regard to bioclinical factors included reductions in A1C (21 studies), blood glucose (10 studies), cholesterol (4 studies), blood pressure (8 studies), and BMI (8 studies). Negative results reported included unchanged or increased A1C levels after the education (3 studies), no effect on patients’ knowledge (2 studies), and no change in patients’ negative health beliefs (1 study). Some studies have reported mixed results, showing improvements in some areas and no effects in others. For example, one study20 found no significant improvement in A1C but significant weight loss, better understanding of diabetes, and lower depression scores.
To advance our understanding of this issue, further studies are needed. Some authors point out that the design and implementation of education programs may confound the findings. Few programs have been developed in a primary care setting, and none have been designed specifically for patients from the point of diagnosis.20 Additional studies that control for variation in program design, we believe, may shed light on why the findings are inconclusive. Programs designed on a theoretical basis tend to have positive outcomes.21
In addition to program design and development, we believe other factors such as culture differences may also have had an effect on reported findings. Most recent studies have been conducted in Europe, with primarily white populations. Some studies have dealt with barriers to education programs, and access in African-American and Latin communities has been the most cited concern.19 These communities are mostly located in metropolitan areas of the United States, and diabetes is widespread among them. In addition, there may be a difference in program guidelines (i.e., whether a program is recognized by the American Diabetes Association [ADA]), but recent studies, including meta-analyses, have not taken this variable into account as a potential moderator to the effectiveness of DSME.
This study aims to fill this gap in knowledge. Following a systematic approach, we evaluated the influence of a diabetes education program in a primary care setting: a large U.S. metropolitan clinic network that covers >2 million people and serves a large African-American population.
Methods
From 2008 to 2011, > 1,000 adults ≥ 18 years of age with type 2 diabetes were originally referred to the Cleveland Clinic diabetes education programs, located in six primary care sites within the Cleveland Clinic health care network in Ohio: Stephanie Tubbs Jones Clinic, Hillcrest Hospital, Euclid Hospital, South Pointe Hospital, Solon Clinic, and Macedonia Clinic. All the programs are accredited by the American Association of Diabetes Educators (AADE). Of these patients, 380 finished three or four education sessions, and among them, 220 had sufficient laboratory data checked at the beginning of a program and within 3–6 months after finishing a program.
Intervention
All participants attended a series of comprehensive self-management classes taught by multidisciplinary teams of diabetes educators. Educators were all registered nurses and dietitians with the formal training to deliver the program, and all were certified diabetes educators. Each participant had an initial one-on-one assessment with a certified nurse or dietitian to develop an individualized plan, followed by either three or four group sessions that included 4–12 patients, depending on the site. Sessions were held once weekly and spread over 3 or 4 weeks, with each session lasting ∼ 2.5 hours. Thus, the total length of the program was ∼ 8–10 hours. The programs covered both medical nutrition therapy and DSME, but focused mostly on DSME. In particular, the classes covered all content areas required by ADA for education program recognition and by AADE for education program certification. These topics include healthy eating, exercise, acute and chronic complications, problem-solving, goal-setting, and ongoing support planning. The classes emphasized diabetes-specific and diabetes-related care, including blood glucose monitoring and medication use and engaged discussions on behavior-change strategies and self-management.
Social workers could be consulted and were available to the participants, but these professionals did not attend all sessions because their presence was not built into the program.
Data Collection
Data were extracted from the Cleveland Clinic Health System electronic medical record systems and included demographic, laboratory, and clinical data before and after participation in a diabetes education program. A1C, blood lipid levels, and creatinine values, measured within 3–6 months before and after the intervention, were obtained. Participants’ weight, blood pressure, and medication utilization at the time of the first diabetes education session and within 3–6 months after the intervention were recorded.
Statistical Analysis
All patients who attended at least three diabetes education sessions and had no missing data before or after the intervention were included. Standard descriptive statistics were used to depict baseline characteristics of the study participants.
McNemar’s χ2 test with Yates’s continuity correction22 were used for the categorical variables. Considering the finding that the continuity correction is often too conservative,23 we also conducted McNemar’s test without the correction for comparison. We compared the continuous outcome variables before and after the educational intervention using a paired-sample two-tailed t test.
We also analyzed the between-subject effects of sex and race using multivariate analysis of variance (ANOVA). We identified three clinical variables on which race and sex had significant moderating effects: total cholesterol, LDL cholesterol, and triglyceride levels. We then applied the univariate ANOVA to each of these three outcome variables to find out how race and sex moderate the effects on the variables.
Results
A total of 220 adults were included in the study. The mean (± SD) age of the patients was 65.7 ± 10.9 years, 60% were female, and there was a fair representation of minorities, with 60.5% being African American. Among the participants, 12.3 and 51.8% were, respectively, current or former smokers. The rate of current smokers was slightly less than the national average of 19% for all adults,24 but the rate of former smokers was representative of the adult population 40 years ago, when > 45% of adults were smokers.25
Table 1 presents the main outcome measures at baseline and after the educational intervention. The primary outcome variable A1C decreased by 1.2 percentage points (95% CI 0.9–1.6, P < 0.001). BMI decreased by 0.7 kg/m2 (95% CI 0.4–1.0, P < 0.001).
Table 1.
Outcome Measures Before and After the Diabetes Education Program Implementation
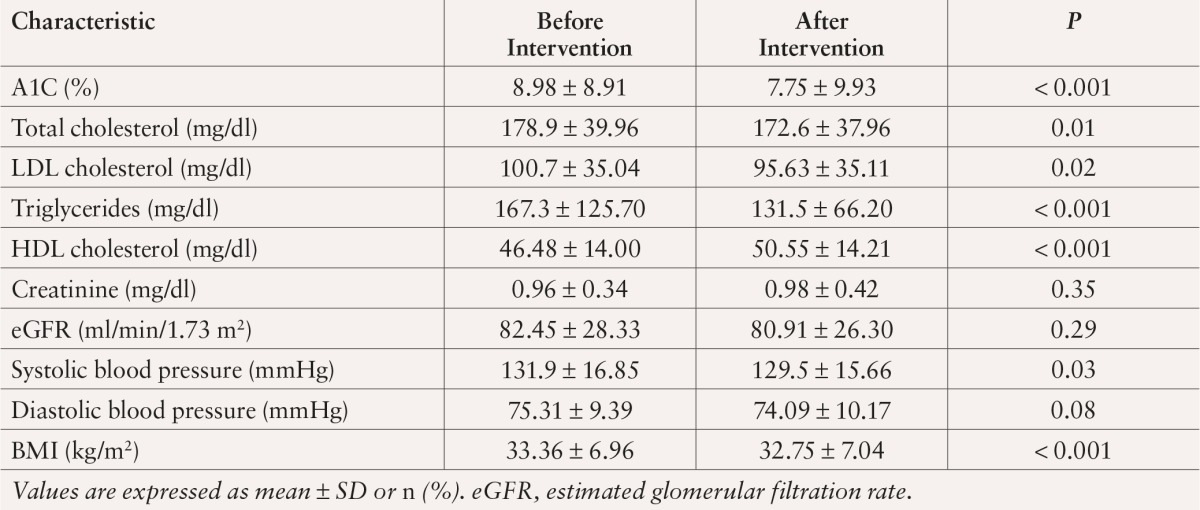
After the intervention, participants had an average decrease in systolic blood pressure of 2.7 mmHg (95% CI 0.3–5.1, P = 0.03) and improvements in their lipid profile, with an average decrease in total cholesterol of 6.9 mg/dl (95% CI 1.5–12.4, P = 0.01), a decrease in LDL cholesterol of 5.6 mg/dl (95% CI 0.8–10.5, P = 0.02), and an increase in HDL cholesterol of 3.9 mg/dl (95% CI 2.3–5.5, P < 0.001). Changes in creatinine and estimated glomerular filtration rate (eGFR) were not statistically significant.
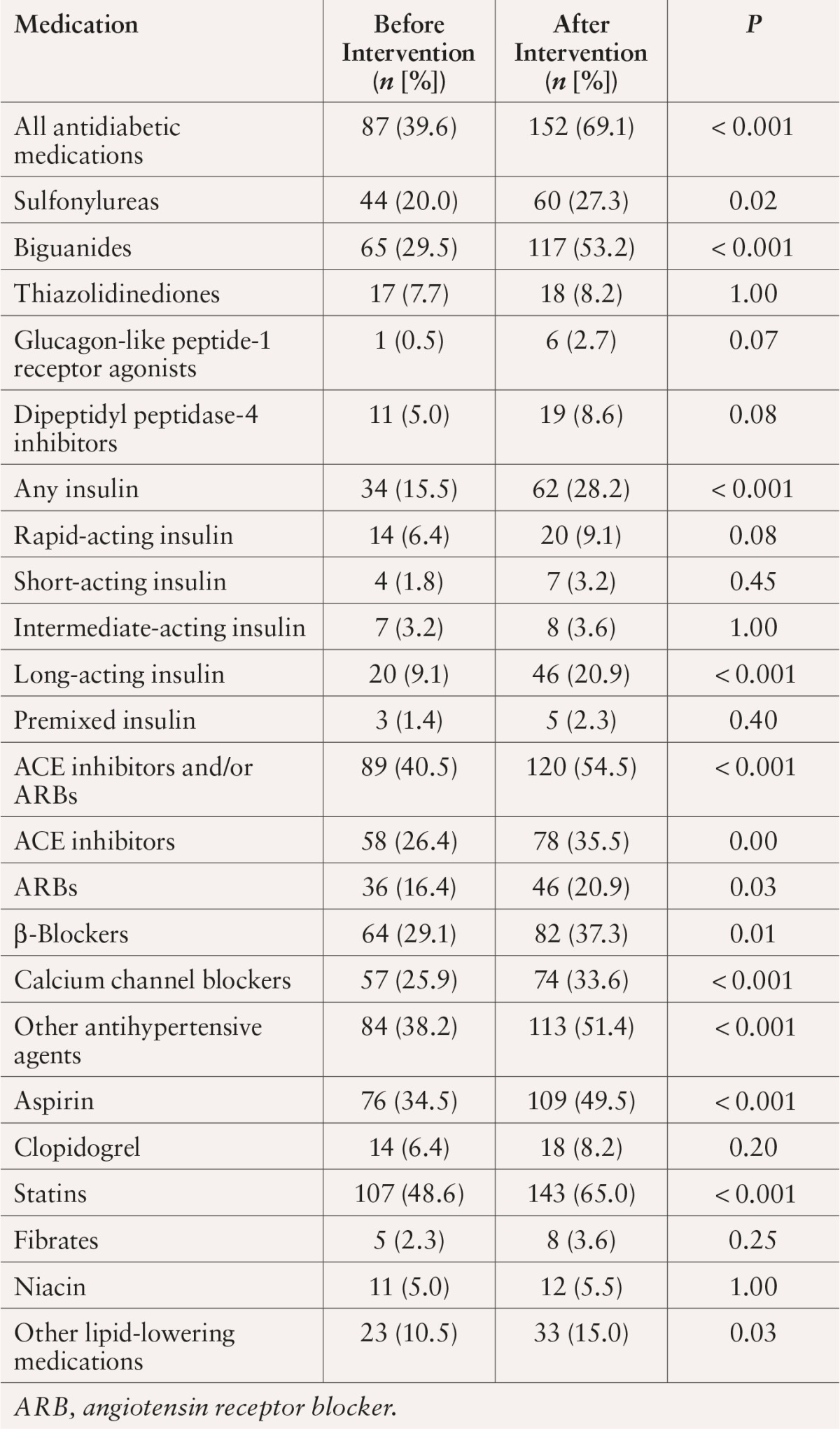
Table 2 shows the pattern of medication change after the intervention. Overall, the percentage of patients who took oral antidiabetic medications increased from 39.6 to 69.1%; insulin use increased from 15.5 to 28.2%; statin use increased from 48.6 to 65%; and use of ACE inhibitors or angiotensin receptor blockers increased from 40.5 to 54.5%. All of these changes were significant at P < 0.001.
Table 2.
Medication Changes After Diabetes Education Intervention
We also evaluated the impact of the diabetes education programs on attainment of recommended annual eye and foot examinations and microalbuminuria measurements as additional indicators of behavioral and motivational changes resulting from the intervention. At baseline, 82.3% of patients had an annual ophthalmological examination, 47.7% had a foot examination, and 39.1% had their urine checked for microalbuminuria. After the intervention, an additional 15.9% of participants received eye exams, 22.7% received foot exams, and 41.4% were evaluated for microalbuminuria. All of these changes were significant at P < 0.001.
Table 3 shows the results of the ANOVA with total cholesterol, LDL cholesterol, and triglyceride levels as dependent variables and race and sex as fixed factors. Race is a significant moderator of the improvement of LDL and total cholesterol at P = 0.02 and P = 0.01, respectively. Sex was a significant moderator of the improvement in LDL cholesterol at P = 0.04.
Table 3.
Subgroup Analysis of Effects by Race and Sex on Total Cholesterol, LDL Cholesterol, and Triglyceride Levels
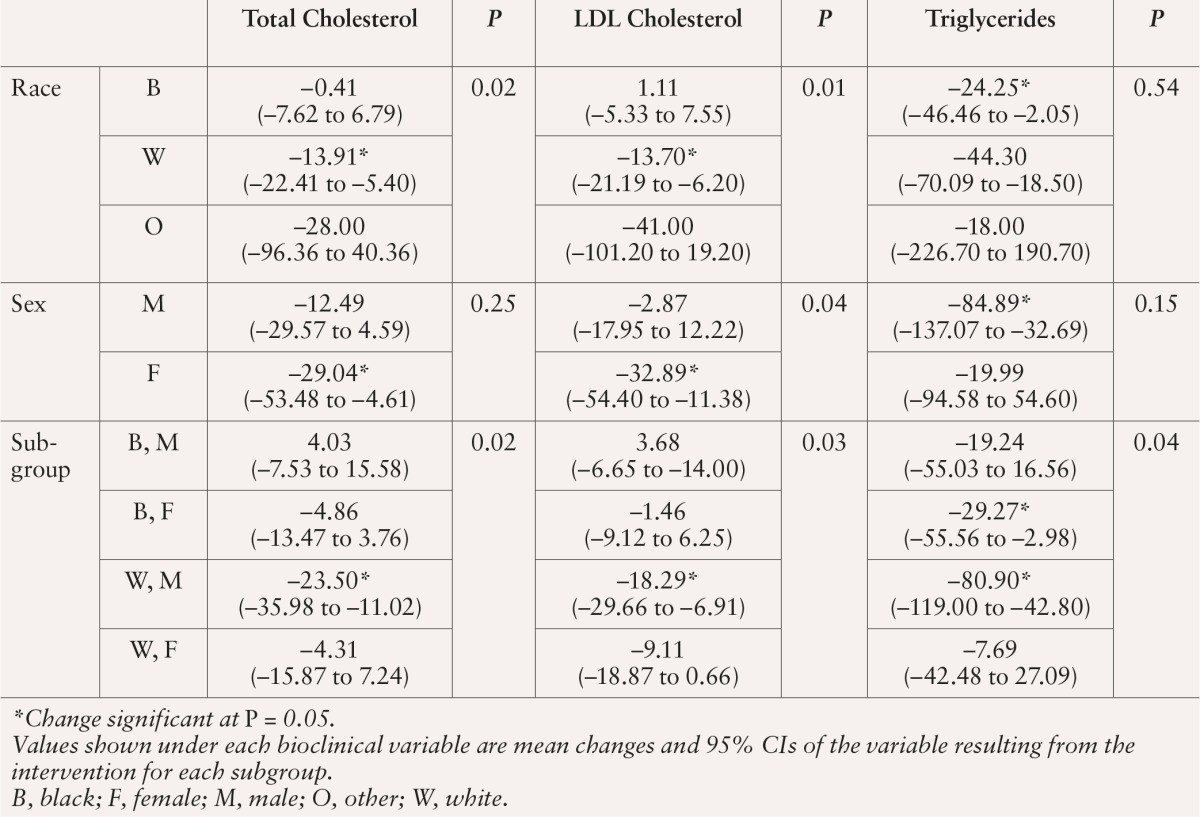
The detailed changes of these three outcomes in various subgroups were as follows. Total cholesterol was improved in all subgroups except for African-American males, who had a small, nonsignificant increase in mean value. LDL cholesterol was improved for all subgroups except for African Americans, African-American males, and males whose ethnicities were not recorded. These three subgroups had small, nonsignificant increases in LDL cholesterol after the intervention. Improvements in both total and LDL cholesterol were significant for white patients, female patients, white males, and those whose race was not recorded. Triglyceride levels were improved in all subgroups, but the improvements were significant only for African Americans, males, African-American females, white males, and males whose races were not recorded.
Discussion
In a cohort of adult patients with type 2 diabetes, we found that completion of three or four sessions of a diabetes education program for adults with type 2 diabetes resulted in improvements in metabolic parameters, lipid profiles, blood pressure clinical parameters, and weight loss and an increase in the number of diabetes, hypertension, and cholesterol medications used.
We observed a significant reduction in A1C (1.2 percentage points) that is likely to be associated with reduced risk of micro- and macrovascular complications. According to the U.K. Prospective Diabetes Study, each 1% reduction in mean A1C was associated with a 37% decrease in risk for microvascular complications and a 21% reduction in risk for any diabetes-related complication or death.26
Most diabetes medications can reduce A1C by 1 percentage point. This has been confirmed by a recent review27 of 166 clinical studies published between January 1996 and April 2010 on the effectiveness of medications for adults with type 2 diabetes. In our study, we found an overall reduction that is more than the medication effect. To further confirm this finding, we performed an additional analysis on the 49 patients who did not use any antidiabetic medications. Their A1C level was reduced by 0.53 percentage point, which was statistically significant (P = 0.001, 95% CI 0.23–0.83).
Lipid profiles improved in parallel with improvement in A1C. Total cholesterol, LDL cholesterol, and triglycerides decreased significantly. HDL cholesterol increased significantly, conferring a lower risk for coronary heart disease and other cardiovascular complications.
Creatinine and eGFR did not change significantly. This is consistent with previous findings from similar studies demonstrating no significant benefit of intensive blood glucose control on microvascular diseases.28
Implications and Limitations
These results provide evidence that structured education poses potential benefits to patients with diabetes and to clinical practices overall. The patient-centered approach to diabetes care in these programs demonstrates the importance of public awareness and education in health care in our society. This study has shown that involving patients in their own care through education is essential to the successful management and control of diabetes and, ultimately, to reducing risks for complications later on.
This study focused on improvements in clinical outcomes. To maintain these improvements in the long run, however, patients’ attitudes are as important as their knowledge and self-management skills. Encouraging and supporting patients to assume active responsibility for control of their diabetes-related conditions is crucial.29–33 Future studies may also take into account the quality of patients’ psychological life, as well as bioclinical variables such as those recommended by the World Health Organization.34
Although some studies have compared average outcome values between a control group and an intervention group using ANOVA, this study compared outcome measures before and after an intervention for each participant using a paired-sample test. There are some differences between the two methods. First, it is necessary but difficult to control the timing of measuring values for patients in the control group to match those of patients in the intervention group; observations made in 1 year cannot be compared with those made in 3–4 months. Second, when using ANOVA, outliers can potentially inflate or deflate group means, and the result becomes dependent on the selection of participants, rendering a randomized experiment design necessary. Neither of these issues was properly addressed in previous studies because of the difficulty in implementing such a design.
In contrast, when using a paired-sample test, we compared patients to themselves over time, and thus the results are less sensitive to the selection of participants. In particular, we tracked the change of each outcome variable for each subject at baseline and within 3–6 months after the intervention and then used McNemar’s χ2 and paired sample t tests to compute each participant’s changes. In this way, excessive improvement or deterioration in one patient does not offset intervention effects on others, and a significant number of patients must show improvement for the intervention to be declared effective as a whole.
This study was conducted on education programs in six primary care sites within the Cleveland Clinic health care network and focused equally on African-American (60.5%) and white populations. The subjects were demographically representative of the population of diabetes patients in metropolitan areas in the United States. This study found some significant moderating effects of race and sex on three clinical outcomes, including total cholesterol, LDL cholesterol, and triglyceride levels. In particular, it found that the intervention was effective for white and female patients of all races in improving total and LDL cholesterol and for African Americans and male patients of all races in improving triglycerides. This finding may suggest why previous studies have been inconclusive regarding the effectiveness of interventions. At the very least, it suggests that future studies should pay attention to populations with different ethnicities and cultural backgrounds.
The study is also important to future diabetes care practice because of its applicability to patients in typical U.S. metropolitan areas. It has two direct applications. First, its findings proving the benefits of diabetes education beyond medical therapy will encourage patients to participate in DSME programs. Second, our results will inform the development and design of future diabetes intervention programs. As we showed, the intervention helped white patients and female patients, but not African-American patients and male patients, in reducing total and LDL cholesterol. However, the latter groups showed significant improvements in triglycerides. Therefore, future programs should consider target bioclinical outcomes and be tailored to participants’ race and sex to improve effectiveness.
Finally, we recognize a limitation of the study: we did not track dropouts and analyze the effects of dropouts on the findings. Among the 1,000 patients referred to the education program, 170 did not participate, and among those who did, only 380 finished three or four sessions. The overall dropout rate was ∼ 60% of referred patients and 54% of those who initially participated. We did not survey the reasons for no-shows or attrition. A lack of involvement and support by the team social workers might have been a contributing factor. A recent study35 found that the most commonly cited reasons for dropping out were scheduling conflicts, patients’ confidence in their own knowledge and ability when managing their diabetes, apathy towards diabetes education, distance to the education site, forgetfulness, regular physician consultations, low perceived seriousness of diabetes, and lack of familiarity with the program and its services.
Note that the same limitation existed in similar studies, and the impact of dropouts is unclear. We believe the impact is smaller in our studies than that in other studies that used ANOVA. Paired t tests compare patients to themselves over time, whereas ANOVA compares patients in different groups, and dropouts constitute a source of selection bias by resulting in only compliant and self-conscious patients in one group. Of course, a further empirical study is needed to quantify the potential effects of dropouts. In particular, evaluation of the following groups is recommended: noncompliant patients, patients who were not referred to the education program, and patients who successfully finished the program.
Acknowledgments
The authors thank Sue Cotey and Melissa Lillash for their assistance in conducting this study, the Cleveland Clinic Foundation for its financial support, and the Stephanie Tubbs Jones Family Health Center for housing the research project. The first author also thanks the Cleveland Clinic Office of Civic Education Initiatives for providing an internship to conduct this research.
References
- 1.Gardner D, Shoback D: Greenspan’s Basic & Clinical Endocrinology. 9th ed. New York, McGraw-Hill Medical, 2011 [Google Scholar]
- 2.Kumar V, Fausto N, Abbas AK, Cotran RS, Robbins SL: Robbins and Cotran Pathologic Basis of Disease. 7th ed. Philadelphia, Pa, Saunders, 2005 [Google Scholar]
- 3.International Diabetes Federation: IDF Diabetes Atlas: Prevelence Estimates of Diabetes Mellitus. 4th ed. Brussels, Belgium, International Diabetes Federation, 2009. Available from www.idf.org/diabetesatlas. Accessed 22 May 2014 [Google Scholar]
- 4.Risérus U, Willett WC, Hu FB: Dietary fats and prevention of type 2 diabetes. Prog Lipid Res 48:44–51, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boussageon R, Bejan-Angoulvant T, Saadatian-Elahi M, Lafont S, Bergeonneau C, Kassaï B, Erpeldinger S, Wright JM, Gueyffier F, Cornu C: Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ 343:d4169, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ripsin CM, Kang H, Urban RJ: Management of blood glucose in type 2 diabetes mellitus. Am Fam Phys 79:29–36, 2009 [PubMed] [Google Scholar]
- 7.Melmed S, Polonsky KS, Larsen PR, Kronenberg HM: Williams Textbook of Endocrinology: Expert Consult. 12th ed. Philadelphia, Pa, Saunders, 2011 [Google Scholar]
- 8.National Institute for Health and Clinical Excellence: Clinical guideline 66: type 2 diabetes. London, National Health Service, 2008. Available from http://www.nice.org.uk/nicemedia/pdf/cg66niceguideline.pdf. Accessed 22 May 2014 [Google Scholar]
- 9.DCCT Research Group: The effect of intensive diabetes therapy on the development and progression of neuropathy. Ann Intern Med 122:561–568, 1995 [DOI] [PubMed] [Google Scholar]
- 10.Oftedal B, Bru E, Karlsen B: Motivation for diet and exercise management among adults with type 2 diabetes. Scand J Caring Sci 25:735–744, 2011 [DOI] [PubMed] [Google Scholar]
- 11.Nagelkerk J, Reick K, Meengs L: Perceived barriers and effective strategies to diabetes self-management. J Adv Nurs 54:151–158, 2006 [DOI] [PubMed] [Google Scholar]
- 12.Pinhas-Hamiel O, Zeitler P: Barriers to the treatment of adolescent type 2 diabetes: a survey of provider perceptions. Pediatr Diabetes 4:24–28, 2003 [DOI] [PubMed] [Google Scholar]
- 13.Pun S, Coates V, Benzie I: Barriers to the self-care of type 2 diabetes from both patients’ and providers’ perspectives: literature review. J Nurs Healthc Chronic Illn 1:4–19, 2009 [Google Scholar]
- 14.Wagner EH, Grothaus LC, Sandhu N, Galvin MS, McGregor M, Artz K, Coleman EA: Chronic care clinics for diabetes in primary care: a system-wide randomized trial. Diabetes Care 24:695–700, 2001 [DOI] [PubMed] [Google Scholar]
- 15.Trento M, Passera P, Borgo E, Tomalino M, Bajardi M, Cavallo F: A 5-year randomized controlled study of learning, probability solving ability, and quality of life modifications in people with type 2 diabetes managed by group care. Diabetes Care 27:670–675, 2004 [DOI] [PubMed] [Google Scholar]
- 16.American Association of Diabetes Educators: Position statement: AADE7TM self-care behaviors. Diabetes Educ 34:445–449, 2008. 18535317 [Google Scholar]
- 17.American Association of Diabetes Educators: Guidelines for the practice of diabetes education. Chicago, Ill, American Association of Diabetes Educators, 2009 [Google Scholar]
- 18.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM: Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 25:1159–1171, 2002 [DOI] [PubMed] [Google Scholar]
- 19.Albano MG, Crozet C, d’Ivernois JF: Analysis of the 2004–2007 literature on therapeutic patient education in diabetes: results and trends. Acta Diabetol 45:211–219, 2008 [DOI] [PubMed] [Google Scholar]
- 20.Davis MJ, Heller S, Skinner TC, Campbell MJ, Carey ME, Cradock S, Dallosso HM, Daly H, Doherty Y, Eaton S, Fox C, Oliver L, Rantell K, Reyman G, Khunti K: Effectiveness of the diabetes education and self-management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ 336:491–495, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ellis LE, Speroff T, Dittus RS, Brown A, Pichert JW, Elasy TA: Diabetes patient counseling: a meta-analysis and meta-regression. Patient Educ Couns 52:97–105, 2005 [DOI] [PubMed] [Google Scholar]
- 22.Yates F: Contingency tables involving small numbers and the chi-square test. J R Stat Soc 1 (Suppl.):217–235, 1934 [Google Scholar]
- 23.Newcombe RG: Interval estimation for the difference between independent proportions: comparison of eleven methods. Stat Med 17:873–890, 1998 [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention: Smoking & tobacco use. Available from http://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts. Accessed 22 April 2013
- 25.U.K. Office for National Statistics: ONS survey: smoking halves in 40 years. Available from http://www.bbc.co.uk/news/health-21698054. Accessed 22 April 2013
- 26.Stratton IM, Al Adler, Neil AW, Matthews DR, Manley SE, Cull CA: Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321:405–412, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bennett WL, Wilson LM, Bolen S: Oral Diabetes Medications for Adults With Type 2 Diabetes: An Update. Rockville, Md, Agency for Healthcare Research and Quality, 2011 [PubMed] [Google Scholar]
- 28.Gerstein HC, Miller ME, Byington RP, Goff DC, Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH, Jr, Probstfield JL, Simons-Morton DG, Friedewald WT: Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 358:2545–2559, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.U.K. Department of Health: National Service Framework for Diabetes: Standards. London, U.K. Department of Health, 2001 [Google Scholar]
- 30.U.K. Department of Health: National Service Framework for Diabetes: Delivery Strategy. London, U.K. Department of Health, 2002 [Google Scholar]
- 31.U.K. Audit Commission: Testing Times: A Review of Diabetes Services in England and Wales. Northampton, U.K, Belmont Press, 2000 [Google Scholar]
- 32.National Institute for Clinical Excellence: Guidance on the Use of Patient-Education Models for Diabetes: Technology Appraisal. 60. London, National Institute for Clinical Excellence, 2003 [Google Scholar]
- 33.Rutten G: Diabetes patient education: time for a new era. Diabet Med 22:671–673, 2005 [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization: Life Skills Education for Children and Adolescents in Schools. Rev. 2 Geneva, Switzerland, World Health Organization, 1997 [Google Scholar]
- 35.Gucciardi E, DeMelo M, Offenheim A, Stewart DE: Factors contributing to attrition behavior in diabetes self-management programs: a mixed method approach. BMC Health Serv Res 8:33–43, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]


