Abstract
Background: Previous observational studies of self-reported dairy product consumption and stroke risk have reported mixed findings. Few studies have used circulating biomarkers that provide objective measures of dairy fat intake.
Objectives: We tested the hypothesis that the circulating biomarkers of dairy fat, pentadecanoic acid (15:0), heptadecanoic acid (17:0), and trans palmitoleate (trans 16:1n−7), were associated with lower incidence of stroke, especially ischemic stroke. Secondarily, we evaluated 14:0, which is obtained from dairy products and beef, and also endogenously synthesized.
Design: In participants from 2 large US cohorts (the Health Professionals Follow-Up Study: 51,529 men; the Nurses’ Health Study: 121,700 women) with stored blood samples in 1993–1994 (n = 18,225) and 1989–1990 (n = 32,826), respectively, we prospectively identified 594 incident stroke cases (median follow-up: 8.3 y) and matched them 1:1 to risk-set–sampled control subjects by age, sex, race, and smoking. Total plasma and red blood cell (RBC) fatty acids were measured by using gas-liquid chromatography. Covariates were assessed by using validated questionnaires. Stroke events and subtypes were adjudicated by using medical records or other supporting documentation. We used conditional logistic regression to estimate associations of fatty acids with incident stroke, and cohort-specific findings were combined by inverse-variance weights.
Results: After adjustment for demographic characteristics, lifestyle, cardiovascular disease risk factors, diet, and other circulating fatty acids, no significant associations with total stroke were seen for plasma 15:0 (pooled HR for highest compared with lowest quartiles: 0.85; 95% CI: 0.54, 1.33), 17:0 (0.99; 0.67, 1.49), trans 16:1 n−7 (0.89; 0.55, 1.45), or 14:0 (1.05; 0.62, 1.78). Results were similar for ischemic and hemorrhagic stroke subtypes, for RBC fatty acids, and in several different sensitivity analyses.
Conclusion: In 2 large prospective cohorts, circulating biomarkers of dairy fat were not significantly associated with stroke.
Keywords: dairy fat, biomarkers, total plasma, red blood cell, pentadecanoic acid, heptadecanoic acid, trans-palmitoleate, stroke, ischemic stroke, hemorrhagic stroke
See corresponding editorial on page 1407
INTRODUCTION
Dairy products contribute 9.5% of the total energy in the U.S. food supply (1, 2) but their effects on many chronic conditions, including stroke, are not well established. Dairy fats, which are predominantly saturated fats, increase LDL cholesterol (3, 4), and are traditionally thought to induce insulin resistance and inflammation (4). These effects could increase risk of stroke, particularly ischemic stroke (5–8). Conversely, other evidence has suggested that dairy products or dairy fat could lower risk of both ischemic and hemorrhagic stroke, for example, by providing calcium, magnesium, potassium, phosphorus, and bioactive peptides (proteins) (9, 10) that could have antithrombotic, antihypertensive, or antiobesity effects (11). Dairy-specific fatty acids themselves could lower risk of ischemic stroke by raising HDL cholesterol (3) or of hemorrhagic stroke by reducing cerebral vascular fragility (12, 13). Therefore, biological mechanisms suggest both potential benefits and harms of dairy fat on risk of stroke and its subtypes.
Several previous individual studies have analyzed associations of self-reported dairy product consumption and stroke with inconsistent findings. Meta-analyses of these prospective observational studies have shown self-reported total dairy (14, 15) and both low-fat dairy product and cheese consumption (14) to be significantly inversely associated with total stroke; intake of whole-fat dairy foods was associated with trends toward lower risk (14). Notably, it is less certain if these associations were more specific for whole- or low-fat dairy foods to draw any conclusions about effects of dairy fat on stroke risk. Potential reasons included the relatively limited number of studies in these subgroups, significant statistical heterogeneity, and methodologic concerns such as the nonstandardization of exposure across studies. These limitations also restricted the interpretation of inverse associations or trends for total dairy products and subtypes of ischemic and hemorrhagic strokes. Insufficient studies precluded stratified analyses by fat content for dairy-food components such as milk and cheese (14, 16).
In addition, because each study in the meta-analyses was based on self-reported dietary estimates, findings may have been limited by both random and systematic errors. Compared with self-reported intakes, circulating fatty acid biomarkers of dairy fat may provide a more objective measure of consumption. These fatty acids include pentadecanoic acid (15:0) and heptadecanoic acid (17:0) (17–19), which are odd-chain SFAs, and trans palmitoleate (trans 16:1n−7) (20), which is a natural ruminant trans fat. Each of these fatty acids are obtained primarily from dairy fat and not endogenously synthesized (16), which make them reasonable biomarkers of dairy fat consumption (17–19, 21). Myristic acid (14:0), which is another fatty acid, is present in dairy fat and also obtained from beef and some plant oils (22), and can be directly endogenously synthesized by the liver (e.g., in response to excess carbohydrate intake). To our knowledge, only one previous study has evaluated dairy fatty acid biomarkers and stroke risk (23) and observed plasma phospholipid 17:0, but not 15:0 alone, to be significantly inversely associated with stroke overall with stronger associations in women and nonsignificant findings in men. This investigation was limited by a small sample size (108 cases) and has not been further replicated.
On the basis of this evidence, it is unclear how dairy product intake and dairy fat, in particular, influence stroke risk. An effect of dairy fat on stroke would inform the need for additional mechanistic and experimental studies to explore relevant biological pathways of effect and also have potential implications for dietary guidelines. To address this crucial research question, we conducted nested case-control studies of dairy fatty acid biomarkers and incident stroke in 2 large, prospective U.S. cohorts of men and women. Because of inverse associations of dairy products with incident stroke in meta-analyses of self-reported intake studies, we tested the hypothesis that total plasma and red blood cell (RBC)6 fatty acid biomarkers of dairy fat, 15:0, 17:0, and trans 16:1n−7, were associated with lower incidence of total stroke and its subtypes of ischemic and hemorrhagic strokes.
SUBJECTS AND METHODS
Study design and population
The current study was derived from the 2 large prospective cohorts, the Nurses’ Health Study (NHS) and Health Professionals Follow-Up Study (HPFS) (24, 25). In both cohorts, biennial questionnaires obtained information on demographics, health, medical history, and cardiovascular and lifestyle risk factors; validated diet questionnaires were obtained every 4 y. Blood samples were provided by 32,826 women in 1989–1990 (NHS) and 18,225 men in 1993–1994 (HPFS). Individuals who provided samples were very similar to those who did not provide samples in terms of age, BMI, parity, the percentage of current smokers, and duration of oral contraceptive use (21). Blood samples were collected in sodium heparin or EDTA, centrifuged, and distributed in aliquots of plasma, RBCs, and buffy coat fractions that were stored, after receipt, in liquid-nitrogen freezers from −130°C to −196°C until analysis.
We performed nested case-control studies of incident stroke that involved participants from both cohorts. From subjects who provided blood samples and were free of prevalent cardiovascular disease or cancer, we identified 603 cases of stroke who were matched 1:1 with 603 control subjects on the basis of the time of follow-up (risk-set sampling), age (±1 y), race, smoking status (current, former matched on years since stopping, or never), and date of blood collection. Matching variables were selected to increase efficiency of adjustment because of their role as major cardiovascular disease risk factors. We selected a limited number of matching factors to minimize potential challenges in matching a control for every case, overmatching (matching on variables related to exposure), and matching on mediators. Cases were identified prospectively until 2006 (NHS) and 2004 (HPFS). After the exclusion of individuals with missing fatty acid data, 594 cases of stroke (NHS: 472 cases; HPFS: 122 cases) and 594 matched controls were included in this analysis. This investigation was approved by the human subjects committees of all participating institutions, and all participants provided implied consent by giving blood samples and returning completed questionnaires.
Fatty acids
Fatty acid concentrations were measured in stored total plasma and RBC samples in the same laboratory by using gas-liquid chromatography for both cohorts. Detailed methods have been described (21, 26). Concentrations of individual circulating fatty acids were expressed as a percentage of total fatty acids in plasma or RBC membranes. Technicians and laboratory personnel were unaware of all clinical information, including the disease status, of participants. To minimize laboratory drift, each case-control pair was shipped in the same batch and analyzed in the same run in a random sequence and under identical conditions. Blinded quality-control samples were also included.
Forty fatty acids in total plasma and RBCs were identified by using these methods. For this investigation, primary biomarkers of interest were 15:0, 17:0, and trans 16:1n−7; 14:0 was secondarily analyzed. We measured both total plasma and RBC fatty acid concentrations to determine the consistency of findings across these different lipid compartments. These different compartments might represent varying temporal periods of dietary intake or variability in metabolic fatty acid handling (27, 28) affecting disease outcomes differentially, although limited findings have suggested that temporal changes in 15:0 may be similar in plasma compared with RBC fatty acids (29, 30). Overall intraassay CVs for plasma fatty acids in the 2 cohorts were 9.6% for 15:0, 9.9% for 17:0, 14.9% for trans 16:1n−7, and 18.2% for 14:0. RBC fatty acid measurements had higher intraassay CVs of 23.7%, 19.0%, 20.1%, and 45.0%, respectively. The reliability of RBC 15:0, 17:0, and trans 16:1n−7 over 1–2 y in a subset of 40 random participants from the NHS has been shown to be reasonable with intraclass correlation coefficients (ICCs), that represented between-person to total variation of 0.72, 0.52, and 0.57 (31). However, the within-person variation of 14:0 concentrations with time was relatively higher (ICC: 0.44). ICCs of these fatty acids in plasma over 6–9 mo were lower than those of RBCs (15:0: 0.25; 17:0: 0.15; trans 16:1n−7: 0.36; and 14:0: 0.21) in another small subset (n = 132) from the same cohort who were monitored for health, diet, and physical activity. Fatty acid contents in blood samples stored at low temperatures (−80°C or lower) were shown to be stable and had minimal degradation over more than a decade of storage (21, 32).
Incident stroke
In both cohorts, potential events were first identified through a self-report on biennial questionnaires of physician-diagnosed stroke or, for fatal events, by death certificates or contact with the next of kin. For each potential case, consents for a medical record review were requested and records were obtained to confirm the diagnosis of stroke for 95.6% of cases in this sample; remaining cases were corroborated by self-confirmation (2.5%) or death certificates only (1.9%). Medical records were reviewed by physicians who were unaware of the subject's fatty acid measures or other questionnaire data, and a diagnosis was made on the basis of the National Survey of Stroke criteria (33). Stroke was defined as a neurologic deficit of sudden or rapid onset of ≥24 h duration or until death with the exclusion of participants with only transient ischemic attacks. Strokes were subtyped as 1) ischemic [i.e., cerebral infarction caused by thrombi (thrombotic) or emboli from extracranial sources (embolic)]; 2) hemorrhagic (i.e., subarachnoid hemorrhage and intraparenchymal hemorrhage); or 3) unknown type when insufficient evidence was available to determine stroke type.
Covariates and other risk factors
In both cohorts, medical history, major risk factors, and lifestyle habits were obtained via validated self-administered questionnaires. We adjusted for smoking status assessed as never, former, and current smokers (34). Physical activity was assessed as the average time spent in different activities including, for example, walking, jogging, running, swimming, tennis, and aerobic exercises plus flights of stairs climbed and walking pace (35, 36) and used to calculate metabolic equivalent task–hours per week (37). Alcohol intake and usual dietary habits were assessed through a validated semiquantitative food-frequency questionnaire (38, 39) that obtained information on usual intakes of foods and beverages over the last year. We further adjusted for menopausal status, postmenopausal hormone use, and family history of myocardial infarction or diabetes that were assessed through a validated self-report.
Primary fatty acids evaluated in our analysis (15:0, 17:0, and trans 16:1n−7) were derived from dietary intake, and their concentrations could be partly confounded by other dietary habits that are also associated with risk of diabetes, such as intakes of fruit, vegetables, fish, meats, whole grains, polyunsaturated fat, sugar-sweetened beverages, or glycemic load. Thus, we adjusted for major dietary risk factors to reduce potential confounding. We also evaluated potential confounding by other circulating fatty acids that may be associated with these biomarkers (e.g., total trans 18:1 and trans 18:2, which may share common sources with trans 16:1n−7), and fatty acids derived from de novo lipogenesis (e.g., 16:0 and 18:0, the concentrations of which may influence relative concentrations of dietary fatty acids).
BMI, which is a risk factor for ischemic and hemorrhagic stroke (40), was considered as both a potential mediator and confounder. We and other authors have shown that the consumption of certain dairy products is related to weight gain (e.g., yogurt has been linked to less weight gain) (41), suggesting that this relation could be a mechanism for inverse associations. In addition, people with different BMIs may choose to eat different dairy products, making BMI a potential confounder. Therefore, we separately evaluated BMI at the time of fatty acid measurements together with its related risk factors of hypertension and hypercholesterolemia in the multivariable model. Height and weight were self-reported with high age-adjusted correlation coefficients with technician-measured values reported for weight (the NHS and HPFS: r = 0.97) (42). Hypercholesterolemia and hypertension were evaluated by self-report and validated through medical records in random subsamples (43, 44).
Statistical analysis
We used conditional logistic regression to evaluate associations of fatty acids with incident stroke, which, on the basis of risk set sampling in our cohorts, provided direct measures of HRs. Fatty acid concentrations were evaluated in quartiles as indicator variables and in standardized continuous forms. The linear trend was assessed by assigning the median value of each quartile to participants and assessing this as a continuous variable. We assessed 15:0, 17:0, and trans 16:1n−7 separately as well as their sum. In a secondary analysis, we assessed 14:0 and all 4 biomarkers combined. Analyses were first conducted separately in each cohort and combined by using fixed-effects meta-analysis.
Multivariable models adjusted for potential confounders with covariates selected on the basis of clinical interest, the strength of associations with exposure and outcome, or the percentage change in the risk estimate of interest (by ≥5%); covariates were included if any of these criteria were met. We also adjusted for matching factors. We explored an effect modification by age, which is a major cardiovascular disease risk factor, by using a multiplicative interaction term, with statistical significance tested by using Wald's test and adjusting for multiple comparisons as follows:
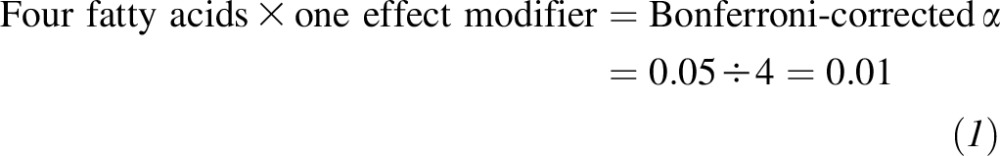 |
If a significant interaction was seen, we conducted additional stratified analyses. We also performed sensitivity analyses restricted to the first 6 y of follow-up to minimize misclassification that was attributable to exposure changes over time and after the exclusion of cases in the first 2 y of follow-up to avoid reverse causation because of unrecognized subclinical disease or the presence of risk factors. Multiple imputation (10-fold) was performed for missing continuous covariates by using predictors from the multivariate model, and missing indicator variables were used for missing categorical covariates.
We formally corrected for measurement error because of a random laboratory and biological variation in fatty acid concentrations by using ICCs from previous reliability studies in the same cohorts (see Fatty acids in Subjects and Methods). We also evaluated the 3 primary fatty acids as well as all 4 fatty acids by using a principal components analysis to derive fatty acid patterns (separately for plasma and RBC compartments) that best explained the maximal variation in these biomarkers. These analyses were conducted in each cohort but did not provide additional information beyond individual fatty acids because each identified factor very closely tracked with a single fatty acid and had a far higher factor loading (correlation) than other fatty acids did (data not shown). All analyses were conducted with SAS 9.3 software (SAS Software Inc.) with statistical significance that was based on a 2-tailed α = 0.05.
RESULTS
The 594 participants with incident stroke included 451 ischemic strokes, 122 hemorrhagic strokes, and 21 strokes of unknown type. The median follow-up interval from the time of blood collection to the stroke event was 8.3 y (IQR: 4.5–11.9); the follow-up time was identical for controls as expected on the basis of the risk-set sampling. The mean (±SD) age at the time of blood collection was 67.6 ± 7.8 y in men and 61.0 ± 6.1 y in women.
At baseline, cases and controls in the 2 cohorts were similar as expected in matching factors, including age, race, and smoking (Table 1). The prevalence of overweight and obesity was also relatively similar, with a slightly lower percentage in controls in the NHS. Other cardiovascular disease risk factors such as hypertension and hypercholesterolemia were more prevalent in case participants than controls as expected. The consumption of dairy products, meats, fruit, vegetables, fish, and alcohol was generally similar between cases and controls. In these unadjusted analyses, distributions of plasma and RBC dairy fatty acids were also similar in cases and controls in the 2 cohorts except for plasma 14:0 that was higher in cases.
TABLE 1.
Baseline characteristics of study participants in 2 prospective, nested, case-control studies of incident stroke (n = 594 cases and 594 matched controls) in the NHS, 1990, and HPFS, 19941
| NHSM |
HPFS |
|||
| Characteristics2 | Cases (n = 472) | Controls (n = 472) | Cases (n = 122) | Controls (n = 122) |
| Stroke types, n (%) | ||||
| Ischemic | 371 (78.6) | — | 80 (65.6) | — |
| Hemorrhagic | 101 (21.4) | — | 21 (17.2) | — |
| Undefined | 0 (0) | — | 21 (17.2) | — |
| Age, y [0]3 | 61.0 ± 6.14 | 61.0 ± 6.1 | 67.6 ± 7.9 | 67.6 ± 7.8 |
| Race-ethnicity,3 % [10] | ||||
| White | 98.1 | 98.9 | 94.3 | 94.3 |
| African-American | 0.9 | 0.4 | 0.0 | 0.0 |
| Asian/other | 1.1 | 0.6 | 5.7 | 5.7 |
| BMI, kg/m2 [12] | 25.7 ± 4.9 | 25.4 ± 4.8 | 26.2 ± 3.2 | 26.2 ± 3.2 |
| BMI, % [12] | ||||
| Normal | 50.5 | 55.2 | 35.8 | 33.6 |
| Overweight | 35.0 | 31.3 | 49.2 | 53.5 |
| Obese | 14.4 | 13.4 | 15.0 | 12.9 |
| Smoking status,3 % [11] | ||||
| Current smoker | 16.5 | 16.6 | 6.7 | 5.0 |
| Past smoker | 40.0 | 39.6 | 52.5 | 52.9 |
| Never smoker | 43.6 | 43.8 | 40.8 | 42.0 |
| Physical activity, MET-h/wk [10] | 15.2 ± 18.5 | 16.8 ± 18.8 | 32.5 ± 36.6 | 35.8 ± 44.6 |
| Medical history, % | ||||
| Hypertension [0] | 31.6* | 22.0 | 42.6* | 22.1 |
| Hypercholesterolemia [0] | 39.2 | 33.1 | 29.5 | 19.7 |
| Parental MI before 60 y [73] | 19.8 | 21.9 | 12.5 | 7.4 |
| Family history of diabetes [1] | 32.2 | 29.2 | 32.8 | 26.5 |
| Plasma fatty acids, % of total fatty acids (total n = 1188) | ||||
| 14:0 | 0.70 ± 0.40* | 0.66 ± 0.37 | 0.91 ± 0.42 | 0.85 ± 0.41 |
| 15:0 | 0.17 ± 0.05 | 0.17 ± 0.05 | 0.19 ± 0.06 | 0.19 ± 0.05 |
| 17:0 | 0.33 ± 0.08 | 0.33 ± 0.07 | 0.32 ± 0.06 | 0.34 ± 0.07 |
| trans 16:1n−7 | 0.22 ± 0.08 | 0.22 ± 0.08 | 0.20 ± 0.07 | 0.22 ± 0.07 |
| RBC fatty acids, % of total fatty acids (total n = 1150) | ||||
| 14:0 | 0.45 ± 0.34 | 0.46 ± 0.42 | 0.42 ± 0.27 | 0.41 ± 0.29 |
| 15:0 | 0.14 ± 0.09 | 0.13 ± 0.05 | 0.11 ± 0.05 | 0.11 ± 0.05 |
| 17:0 | 0.50 ± 0.19 | 0.50 ± 0.18 | 0.47 ± 0.15 | 0.48 ± 0.15 |
| trans 16:1n−7 | 0.17 ± 0.06 | 0.17 ± 0.06 | 0.14 ± 0.05 | 0.14 ± 0.05 |
| Diet, servings/d | ||||
| Total dairy [25] | 2.1 ± 1.5 | 2.2 ± 1.4 | 2.2 ± 1.8 | 2.3 ± 1.7 |
| Whole-fat dairy [29] | 0.93 ± 1.17 | 0.90 ± 1.02 | 1.1 ± 1.3 | 1.2 ± 1.4 |
| Low-fat dairy [28] | 1.2 ± 1.1 | 1.3 ± 1.1 | 1.2 ± 1.1 | 1.1 ± 1.1 |
| Processed meats [24] | 0.21 ± 0.29 | 0.22 ± 0.30 | 0.35 ± 0.40 | 0.41 ± 0.65 |
| Unprocessed meats [24] | 0.91 ± 0.50 | 0.91 ± 0.48 | 0.90 ± 0.59 | 0.98 ± 0.52 |
| Fruit and vegetables [24] | 5.5 ± 2.9 | 5.6 ± 2.7 | 5.8 ± 3.1 | 5.7 ± 3.2 |
| Fish [26] | 0.32 ± 0.27 | 0.31 ± 0.27 | 0.23 ± 0.21 | 0.24 ± 0.23 |
| Alcohol [29] | 0.45 ± 0.84 | 0.45 ± 0.84 | 0.97 ± 1.36 | 0.80 ± 1.21 |
*P < 0.05 for the difference in characteristics between cases and controls. The paired t test was used to compute P values for differences in continuous characteristics between cases and their matched controls. The McNemar-Bowker test was used to compare corresponding proportions for dichotomous 2-group variables, such as hypertension (yes or no), and 3-group variables, such as BMI (normal, overweight, or obese), respectively. HPFS, Health Professionals Follow-Up Study; MET-h, metabolic equivalent task-hours; MI, myocardial infarction; NHS, Nurses’ Health Study; RBC, red blood cell.
Few participants (n < 15) had missing values for each variable except for parental history of MI in the NHS (missing n = 70). Values in square brackets represent overall numbers missing for variables.
Matching factors; other matching factors included blood collection date and follow-up years.
Mean ± SD (all such values).
Intercorrelations of plasma and RBC fatty acids
Within each circulating compartment (plasma and RBCs), the different fatty acid biomarkers were modestly intercorrelated in plasma [adjusted correlation (r) = 0.21–0.61; Table 2], and more strongly intercorrelated in RBCs (r = 0.56–0.78; see Supplemental Table 1). Circulating concentrations of each fatty acid were not strongly intercorrelated across compartments; for comparisons of plasma to RBC concentrations, age- and sex-adjusted correlations were 0.13 for 14:0, 0.24 for 15:0, 0.17 for 17:0, and 0.23 for trans 16:1n−7.
TABLE 2.
Partial Spearman's correlations between plasma fatty acids and dietary factors in the NHS and HPFS1
| Plasma fatty acid intercorrelations (n = 594) |
||||
| 14:0 | 15:0 | 17:0 | trans 16:1n−7 | |
| Dietary factors2 | ||||
| Whole-fat dairy intake, servings/d | 0.05 | 0.19** | 0.12** | 0.10** |
| Low-fat dairy intake, servings/d | 0.04 | 0.11** | 0.11** | 0.07 |
| Dairy fat intake, % of total fat | 0.08* | 0.22** | 0.16** | 0.13** |
| Unprocessed meat, servings/d | −0.02 | 0.04 | 0.09** | 0.09** |
| Processed meat, servings/d | −0.01 | 0.03 | 0.03 | 0.04 |
| Plasma fatty acids | ||||
| 14:0 | 0.61** | 0.01 | 0.21** | |
| 15:0 | 0.46** | 0.45** | ||
| 17:0 | 0.44** | |||
| trans 16:1n−7 | ||||
Correlations were based on pooled individual-level data in controls from both cohorts. Correlations with diet (n = 577) were adjusted for age (y), sex, BMI (in kg/m2), smoking (never, current, former, or missing), fasting status at blood draw, date of blood collection (mo), and consumption of total energy (kcal/d), total fat (percentage of energy), low-fat dairy (servings/d; when whole-fat dairy was evaluated), and whole-fat dairy (servings/d; when low-fat dairy was evaluated). Fatty acid intercorrelations were adjusted for age and sex only. **P < 0.05, *P = 0.05–0.10. HPFS, Health Professionals Follow-Up Study; NHS, Nurses’ Health Study.
Dietary habits were assessed using the average of self-reported consumption in 1986 and 1990 in the NHS and 1990 and 1994 in the HPFS.
Plasma 15:0 modestly correlated with self-reported intakes of whole-fat dairy foods (r = 0.19), low-fat dairy foods (r = 0.11), and dairy fat (r = 0.22) (Table 2). Plasma 17:0 and trans 16:1n−7 were also correlated with lower magnitudes than for 15:0. Plasma 14:0 weakly correlated with self-reported dairy product intakes, which was consistent with multiple origins of 14:0 (e.g., endogenous fatty acid synthesis). Compared with plasma fatty acids, RBC fatty acids were less-strongly correlated with self-reported dairy product consumption (see Supplemental Table 1 under “Supplemental data” in the online issue).
Fatty acid biomarkers and risk of stroke
After adjustment for demographic characteristics, cardiovascular disease risk factors, lifestyle, dietary habits, and other circulating fatty acids, none of the plasma fatty acid biomarkers were significantly associated with total stroke in either cohort or overall (Table 3). With highest compared with lowest quartiles, the pooled multivariable adjusted HR was 0.85 (95% CI: 0.54, 1.33) for 15:0, 0.99 (0.67, 1.49) for 17:0, 0.89 (0.55, 1.45) for trans 16:1n−7, and 1.05 (0.62, 1.78) for 14:0. When stroke subtypes were evaluated, results were similar for ischemic (see Supplemental Table 2) and hemorrhagic (see Supplemental Table 3) strokes. Circulating RBC concentrations of these fatty acids were also not significantly associated with total stroke (Table 4) or stroke subtypes (P-trend = NS for each; data not shown).
TABLE 3.
Risk of total stroke according to plasma fatty acid biomarkers of dairy fat consumption in the NHS (n = 472 cases) and HPFS (n = 122 cases)1
| Cohort-specific fatty acid quartiles |
|||||
| Fatty acid | 1 | 2 | 3 | 4 | P-trend |
| 14:0 | |||||
| NHS | |||||
| Median percentage of total fatty acids | 0.26 | 0.50 | 0.72 | 1.05 | — |
| No. of cases | 115 | 107 | 107 | 143 | — |
| Multivariable HRs (95% CIs) | Reference | 0.88 (0.58, 1.35) | 0.79 (0.48, 1.31) | 1.02 (0.59, 1.79) | 0.77 |
| HPFS | |||||
| Median percentage of total fatty acids | 0.36 | 0.69 | 0.90 | 1.37 | — |
| No. of cases | 17 | 41 | 33 | 31 | — |
| Multivariable HRs (95% CIs) | Reference | 2.92 (1.01, 8.42) | 1.08 (0.30, 3.95) | 1.40 (0.27, 7.22) | 0.83 |
| Pooled | Reference | 1.04 (0.70, 1.54) | 0.82 (0.52, 1.31) | 1.05 (0.62, 1.78) | 0.73 |
| 15:0 | |||||
| NHS | |||||
| Median percentage of total fatty acids | 0.12 | 0.15 | 0.18 | 0.23 | — |
| No. of cases | 126 | 105 | 122 | 119 | — |
| Multivariable HRs (95% CIs) | Reference | 0.74 (0.48, 1.12) | 0.86 (0.56, 1.34) | 0.86 (0.53, 1.39) | 0.79 |
| HPFS | |||||
| Median percentage of total fatty acids | 0.13 | 0.17 | 0.20 | 0.24 | — |
| No. of cases | 27 | 27 | 42 | 26 | — |
| Multivariable HRs (95% CIs) | Reference | 0.80 (0.28, 2.25) | 1.84 (0.65, 5.21) | 0.77 (0.21, 2.87) | 0.72 |
| Pooled | Reference | 0.75 (0.51, 1.11) | 0.96 (0.64, 1.44) | 0.85 (0.54, 1.33) | 0.73 |
| 17:0 | |||||
| NHS | |||||
| Median percentage of total fatty acids | 0.27 | 0.31 | 0.34 | 0.41 | — |
| No. of cases | 142 | 96 | 116 | 118 | — |
| Multivariable HRs (95% CIs) | Reference | 0.68 (0.45, 1.01) | 0.88 (0.59, 1.32) | 1.04 (0.67, 1.60) | 0.62 |
| HPFS | |||||
| Median percentage of total fatty acids | 0.28 | 0.32 | 0.34 | 0.40 | — |
| No. of cases | 42 | 27 | 23 | 30 | — |
| Multivariable HRs (95% CIs) | Reference | 1.08 (0.45, 2.60) | 0.69 (0.27, 1.80) | 0.80 (0.29, 2.16) | 0.59 |
| Pooled | Reference | 0.74 (0.51, 1.07) | 0.85 (0.59, 1.23) | 0.99 (0.67, 1.49) | 0.87 |
| trans 16:1n−7 | |||||
| NHS | |||||
| Median percentage of total fatty acids | 0.14 | 0.19 | 0.23 | 0.31 | — |
| No. of cases | 114 | 95 | 151 | 112 | — |
| Multivariable HRs (95% CIs) | Reference | 0.90 (0.58, 1.41) | 1.41 (0.90, 2.20) | 0.94 (0.55, 1.63) | 0.97 |
| HPFS | |||||
| Median percentage of total fatty acids | 0.14 | 0.20 | 0.24 | 0.29 | — |
| No. of cases | 33 | 33 | 31 | 25 | — |
| Multivariable HRs (95% CIs) | Reference | 1.15 (0.46, 2.85) | 0.87 (0.32, 2.38) | 0.70 (0.23, 2.17) | 0.52 |
| Pooled | Reference | 0.94 (0.63, 1.41) | 1.30 (0.87, 1.96) | 0.89 (0.55, 1.45) | 0.94 |
Multivariable HRs from a conditional logistic model were adjusted for age (y); race (white or nonwhite); month of blood collection; smoking status (never, former, current, or missing); physical activity (metabolic equivalent tasks per week); alcohol (servings/d); family history of diabetes (yes, no, or missing); parental history of myocardial infarction (yes, no, or missing); menopausal status in the NHS (before and after); postmenopausal hormone use in the NHS (no, yes, or missing); consumption of fish (servings/d), processed meats (servings/d), unprocessed meats (servings/d), fruit (servings/d), vegetables (servings/d), whole grains (g/d), coffee (servings/d), sugar-sweetened beverages (servings/d), glycemic load (continuous), dietary calcium (mg/d), polyunsaturated fat (g/d), and total energy (kcal/d); plasma total trans 18:1 (percentage of total fatty acids); plasma total trans 18:2 (percentage of total fatty acids); plasma 16:0 (percentage of total fatty acids); and plasma 18:0 (percentage of total fatty acids). P-trend values within each cohort were computed by assigning the median concentration in each quartile to participants and evaluating this concentration as a continuous variable. Pooled P-trend values were computed by using a generalized least-squares trend analysis (45). HPFS, Health Professionals Follow-Up Study; NHS, Nurses’ Health Study.
TABLE 4.
Risk of total stroke according to RBC fatty acid biomarkers of dairy fat consumption in the NHS (n = 453 cases) and HPFS (n = 122 cases)1
| Cohort-specific fatty acid quartiles |
|||||
| Fatty acid | 1 | 2 | 3 | 4 | P-trend |
| 14:0 | |||||
| NHS | |||||
| Median percentage of total fatty acids | 0.13 | 0.25 | 0.43 | 0.91 | — |
| No. of cases | 89 | 120 | 128 | 116 | — |
| Multivariable HRs (95% CIs) | Reference | 1.52 (0.96, 2.42) | 1.52 (0.92, 2.51) | 1.12 (0.60, 2.10) | 0.68 |
| HPFS | |||||
| Median percentage of total fatty acids | 0.12 | 0.21 | 0.47 | 0.78 | — |
| No. of cases | 24 | 36 | 25 | 37 | — |
| Multivariable HRs (95% CIs) | Reference | 1.52 (0.46, 5.03) | 1.79 (0.44, 7.31) | 4.26 (0.76, 23.88) | 0.09 |
| Pooled | Reference | 1.52 (0.99, 2.34) | 1.55 (0.97, 2.48) | 1.31 (0.73, 2.36) | 0.88 |
| 15:0 | |||||
| NHS | |||||
| Median percentage of total fatty acids | 0.07 | 0.11 | 0.15 | 0.20 | — |
| No. of cases | 136 | 93 | 103 | 121 | — |
| Multivariable HRs (95% CIs) | Reference | 0.58 (0.38, 0.90) | 0.67 (0.43, 1.06) | 0.72 (0.42, 1.23) | 0.24 |
| HPFS | |||||
| Median percentage of total fatty acids | 0.06 | 0.09 | 0.12 | 0.16 | — |
| No. of cases | 29 | 26 | 27 | 40 | — |
| Multivariable HRs (95% CIs) | Reference | 1.24 (0.45, 3.48) | 1.64 (0.53, 5.08) | 3.60 (0.85, 15.23) | 0.08 |
| Pooled | Reference | 0.65 (0.44, 0.97) | 0.76 (0.50, 1.15) | 0.88 (0.53, 1.45) | 0.37 |
| 17:0 | |||||
| NHS | |||||
| Median percentage of total fatty acids | 0.34 | 0.40 | 0.50 | 0.75 | — |
| No. of cases | 136 | 95 | 103 | 119 | — |
| Multivariable HRs (95% CIs) | Reference | 0.74 (0.48, 1.13) | 0.71 (0.45, 1.11) | 0.68 (0.32, 1.45) | 0.33 |
| HPFS | |||||
| Median percentage of total fatty acids | 0.33 | 0.39 | 0.53 | 0.67 | — |
| No. of cases | 34 | 27 | 32 | 29 | — |
| Multivariable HRs (95% CIs) | Reference | 1.02 (0.39, 2.64) | 4.28 (0.88, 20.70) | 5.92 (0.70, 50.04) | 0.10 |
| Pooled | Reference | 0.78 (0.53, 1.15) | 0.81 (0.53, 1.26) | 0.87 (0.42, 1.76) | 0.61 |
| trans 16:1n−7 | |||||
| NHS | |||||
| Median percentage of total fatty acids | 0.11 | 0.15 | 0.18 | 0.25 | — |
| No. of cases | 115 | 109 | 108 | 121 | — |
| Multivariable HRs (95% CIs) | Reference | 0.83 (0.54, 1.26) | 0.88 (0.55, 1.40) | 0.96 (0.52, 1.78) | 0.96 |
| HPFS | |||||
| Median percentage of total fatty acids | 0.10 | 0.12 | 0.15 | 0.20 | — |
| No. of cases | 39 | 20 | 28 | 35 | — |
| Multivariable HRs (95% CIs) | Reference | 0.56 (0.22, 1.39) | 1.17 (0.34, 4.00) | 1.87 (0.45, 7.73) | 0.27 |
| Pooled | Reference | 0.78 (0.53, 1.14) | 0.91 (0.59, 1.41) | 1.07 (0.61, 1.88) | 0.85 |
Multivariable HRs from a conditional logistic model were adjusted for age (y); race (white or nonwhite); month of blood collection; smoking status (never, former, current, or missing); physical activity (metabolic equivalent tasks per week); alcohol (servings/d); family history of diabetes (yes, no, or missing); parental history of myocardial infarction (yes, no, or missing); menopausal status in the NHS (before and after); postmenopausal hormone use in the NHS (no, yes, or missing); consumption of fish (servings/d), processed meats (servings/d), unprocessed meats (servings/d), fruit (servings/d), vegetables (servings/d), whole grains (g/d), coffee (servings/d), sugar-sweetened beverages (servings/d), glycemic load (continuous), dietary calcium (mg/d), polyunsaturated fat (g/d), and total energy (kcal/d); RBC total trans 18:1 (percentage of total fatty acids); RBC total trans 18:2 (percentage of total fatty acids); RBC 16:0 (percentage of total fatty acids); and RBC 18:0 (percentage of total fatty acids). P-trend values within each cohort were computed by assigning the median concentration in each quartile to participants and evaluating this concentration as a continuous variable. Pooled P-trend values were computed by using a generalized least-squares trend analysis (45). HPFS, Health Professionals Follow-Up Study; NHS, Nurses’ Health Study; RBC, red blood cell.
When fatty acids were evaluated continuously per 1-SD increase, none of them were significantly associated with stroke (Table 5). Findings were not altered by additional mutual adjustment for each of the other dairy fat biomarkers or for potential mediators or confounders such as baseline BMI, hypertension, or hypercholesterolemia. Findings were similar in continuous analyses of ischemic or hemorrhagic stroke (data not shown).
TABLE 5.
Risk of total stroke according to plasma fatty acid biomarkers of dairy fat consumption as a standardized continuous variable in the NHS (n = 472 cases) and HPFS (n = 122 cases)1
| Fatty acid | NHS | HPFS | Pooled | P |
| 14:0 | 1 SD = 0.37 | 1 SD = 0.41 | — | — |
| Age | 1.16 (1.00, 1.33) | 1.18 (0.90, 1.53) | 1.16 (1.03, 1.32) | 0.02 |
| Multivariable HRs | 1.11 (0.91, 1.36) | 1.13 (0.62, 2.04) | 1.11 (0.92, 1.35) | 0.27 |
| Plus mediators | 1.11 (0.91, 1.35) | 1.11 (0.59, 2.08) | 1.11 (0.92, 1.34) | 0.28 |
| Plus other dairy biomarkers | 1.13 (0.91, 1.41) | 0.91 (0.45, 1.84) | 1.11 (0.90, 1.37) | 0.33 |
| 15:0 | 1 SD = 0.05 | 1 SD = 0.05 | — | — |
| Age | 1.01 (0.88, 1.17) | 1.02 (0.81, 1.28) | 1.01 (0.90, 1.14) | 0.84 |
| Multivariable HRs | 1.01 (0.85, 1.19) | 1.01 (0.69, 1.48) | 1.01 (0.87, 1.18) | 0.90 |
| Plus mediators | 1.05 (0.88, 1.24) | 0.99 (0.66, 1.50) | 1.04 (0.89, 1.22) | 0.62 |
| Plus other dairy biomarkers | 0.95 (0.76, 1.18) | 1.52 (0.83, 2.78) | 1.00 (0.82, 1.23) | 0.97 |
| 17:0 | 1 SD = 0.07 | 1 SD = 0.07 | — | — |
| Age | 0.96 (0.84, 1.09) | 0.81 (0.62, 1.06) | 0.93 (0.83, 1.05) | 0.22 |
| Multivariable HRs | 1.03 (0.86, 1.23) | 0.78 (0.54, 1.13) | 0.98 (0.83, 1.15) | 0.78 |
| Plus mediators | 1.04 (0.86, 1.25) | 0.76 (0.51, 1.13) | 0.98 (0.83, 1.16) | 0.84 |
| Plus other dairy biomarkers | 1.07 (0.85, 1.35) | 0.70 (0.42, 1.17) | 0.99 (0.81, 1.23) | 0.97 |
| trans 16:1n−7 | 1 SD = 0.08 | 1 SD = 0.07 | — | — |
| Age | 0.99 (0.83, 1.18) | 0.76 (0.55, 1.04) | 0.93 (0.80, 1.09) | 0.36 |
| Multivariable HRs | 0.94 (0.76, 1.17) | 0.69 (0.45, 1.06) | 0.88 (0.73, 1.07) | 0.21 |
| Plus mediators | 0.95 (0.76, 1.19) | 0.75 (0.47, 1.17) | 0.91 (0.74, 1.11) | 0.34 |
| Plus other dairy biomarkers | 0.93 (0.73, 1.18) | 0.68 (0.42, 1.09) | 0.87 (0.70, 1.08) | 0.21 |
| 15:0 + 17:0 + trans 16:1n−7 | 1 SD = 0.16 | 1 SD = 0.14 | — | — |
| Age | 0.98 (0.85, 1.13) | 0.85 (0.66, 1.08) | 0.95 (0.84, 1.07) | 0.37 |
| Multivariable HRs | 0.99 (0.82, 1.20) | 0.78 (0.55, 1.12) | 0.94 (0.79, 1.11) | 0.46 |
| Plus mediators | 1.02 (0.84, 1.24) | 0.79 (0.54, 1.15) | 0.97 (0.81, 1.15) | 0.70 |
| Plus other dairy biomarkers | 0.97 (0.80, 1.18) | 0.76 (0.53, 1.10) | 0.92 (0.77, 1.09) | 0.34 |
| 14:0 + 15:0 + 17:0 + trans 16:1n−7 | 1 SD = 0.44 | 1 SD = 0.47 | — | — |
| Age | 1.13 (0.97, 1.30) | 1.08 (0.84, 1.39) | 1.12 (0.98, 1.27) | 0.09 |
| Multivariable HRs | 1.09 (0.89, 1.34) | 0.92 (0.54, 1.57) | 1.07 (0.88, 1.29) | 0.51 |
| Plus mediators | 1.10 (0.89, 1.35) | 0.91 (0.51, 1.61) | 1.08 (0.89, 1.31) | 0.46 |
| Plus other dairy biomarkers | — | — | — | — |
All values are HRs; 95% CIs in parentheses (per 1-SD increase). Multivariable HRs from a conditional logistic model were adjusted for age (y); race (white or nonwhite); month of blood collection; smoking status (never, former, current, or missing); physical activity (metabolic equivalent tasks per week); alcohol (servings/d); family history of diabetes (yes, no, or missing); parental history of myocardial infarction (yes, no, or missing); menopausal status in the NHS (before and after); postmenopausal hormone use in the NHS (no, yes, or missing); consumption of fish (servings/d), processed meats (servings/d), unprocessed meats (servings/d), fruit (servings/d), vegetables (servings/d), whole grains (g/d), coffee (servings/d), sugar-sweetened beverages (servings/d), glycemic load (continuous), dietary calcium (mg/d), polyunsaturated fat (g/d), and total energy (kcal/d); plasma total trans 18:1 (percentage of total fatty acids); plasma total trans 18:2 (percentage of total fatty acids); plasma 16:0 (percentage of total fatty acids); and plasma 18:0 (percentage of total fatty acids). Plus mediators model HRs were derived from a conditional logistic model adjusted for the multivariable model plus potential mediators and confounders [baseline BMI (in kg/m2), hypercholesterolemia (yes or no), and hypertension (yes or no)]. Plus other dairy fatty acids model HRs were derived from a conditional logistic model adjusted for the multivariable model plus simultaneous mutual adjustment for other dairy fatty acid biomarkers (percentage of total fatty acids). HPFS, Health Professionals Follow-Up Study; NHS, Nurses’ Health Study.
Sensitivity analyses
Overall findings were also similar for the sum of 3 dairy fatty acids (15:0 plus 17:0 plus trans 16:1n−7) and when 14:0 was added to the sum (Table 5). Findings were also similar in analyses that did not include adjustment for other dietary factors (see Supplemental Table 4).
There was little evidence that associations of these plasma or RBC fatty acids with total stroke varied according to differences in age (P-interaction = NS for each). After we corrected for laboratory variation and biological changes in fatty acid concentrations over time, results remained nonsignificant; as expected, correction shifted the main risk estimates away from null and widened CIs (see Supplemental Table 5). For example, the risk of stroke per 1-SD increase for plasma 14:0 changed from an HR of 1.11 (95% CI: 0.92, 1.35) to 1.64 (0.64, 4.21) and, for RBC 17:0, from 0.81 (0.55, 1.19) to 0.67 (0.32, 1.40).
After the exclusion of cases that occurred within the first 2 y of follow-up to minimize reverse causation because of unrecognized subclinical disease or the presence of risk factors, results were similar to the main analyses (P-trend = NS for each fatty acid; data not shown). Findings were also similar after analyses were restricted to cases within the first 6 y to minimize effects of changes in fatty acid intake and concentrations over time (see Supplemental Tables 6 and 7).
DISCUSSION
In these 2 separate, prospective, nested case-control studies derived from large cohorts of U.S. men and women, we did not observe significant associations of total plasma or RBC 15:0, 17:0, trans 16:1n−7, or 14:0 with risk of stroke. Similar results were seen for stroke subtypes and in subgroups by sex and age. The absence of significant associations may have reflected the true lack of biologic effects of dairy fat on stroke or could have been related to an insufficient statistical power or measurement error. The statistical power to detect small differences in risk was limited; however, to our knowledge, this study was still the largest prospective evaluation of dairy fat biomarkers and incident stroke, and large effects could be excluded. In addition, although intraassay CVs for these fatty acids were not low, significant inverse associations of plasma 15:0, 17:0, and trans 16:1n−7 with incident diabetes were shown in these cohorts (Yakoob et al., personal communication, 2014). This indicates that associations can be detected despite measurement error, and misclassification alone does not prevent the identification of significant associations of these fatty acid biomarkers with disease outcomes in these cohorts.
In the biomarkers evaluated, plasma 15:0 was the best biomarker of dairy fat consumption in our cohorts compared with 17:0 and trans 16:1n−7; in RBC fatty acids, trans 16:1n−7 appeared to be a better biomarker. This result was in agreement with previous reports from a separate case-control study of myocardial infarction in these cohorts (21) and from a different cohort of multiethnic Americans (46). The modest correlations with self-reported dairy product intakes observed in our study may have been attributable to random or systematic errors in assessments of dietary habits by using a food-frequency questionnaire, laboratory error in fatty acid measurements, or the potential influence of unknown genetic or endogenous processes related to bioavailability, incorporation, or metabolism in the determination of circulating fatty acid concentrations. For example, emerging evidence has suggested that trans 16:1n−7 may be partly endogenously synthesized from vaccenic acid (trans 18:1n−7) (average conversion rate ∼17%), sources of which include both dairy and other ruminant products and partially hydrogenated vegetable oils (47).
For each of these fatty acids, the intercorrelation between the same fatty acid in plasma compared with RBCs was weak to modest, which suggested a meaningful role of other processes such as the incorporation or metabolism in determining lipid compartment-specific fatty acid concentrations. In addition, these 2 compartments may indicate different time-integrated measures of diet with, for example for dietary omega-3 fatty acids, total plasma reflecting 1–2 wk and RBC phospholipids reflecting 4–8 wk (27, 48). However, potential differences in the time integration between these lipid compartments have been less well-established for dairy fatty acids for which a limited number of studies have suggested more-comparable time frames of the response to dietary intakes (29, 30). In our cohorts, RBC concentrations of these fatty acids were also more reproducible over time than were plasma concentrations. Despite the possibility of differing biologic and temporal representations of these lipid compartments, our results were generally consistent between plasma and RBCs.
Our findings do not support a major association of dairy fatty acid biomarkers with incident stroke. Results were similar after we accounted for measurement error as a result of changes in fatty acid concentrations over time and reverse causation because of subclinical disease or presence of risk factors. The absence of effects on stroke of supplementation with other dairy components such as calcium or vitamin D (49, 50), as well as small effects of these components on blood pressure (51), is consistent with our findings. Limited animal intervention studies have suggested a delayed onset of stroke with the feeding of dairy proteins (casein and whey) than with soybean or egg-white protein (52). An observational analysis that evaluated self-reported dietary intake in the same 2 cohorts as in the current investigation showed modestly lower risk of stroke (10% and 11%, respectively) with estimated substitution of 1 serving red meat/d (7 servings red meat/wk) for whole-fat or low-fat dairy products (53); these findings require confirmation in additional studies. To our knowledge, only one previously published study (23) has reported on dairy fatty acid biomarkers and stroke. This nested case-control study in Sweden showed plasma phospholipid 17:0, but not 15:0 alone, to be inversely associated with stroke. Some limitations of this study included a small sample size (108 cases) and the availability of limited dietary factors for adjustment in only a subsample of the study.
Our study had several strengths. We measured both total plasma and RBC fatty acids, which provided 2 different lipid compartment measures to assess associations with disease risk. The prospective cohort design minimized reverse causation and selection bias, and risk-set sampling allowed for the direct estimation of HRs. Sensitivity analyses evaluated potential bias because of changes in biomarker concentrations over time and reverse causation from subclinical disease. The consistency of our findings was strengthened by the inclusion of 2 separate cohorts including both men and women. We evaluated a comprehensive set of covariates including demographics, cardiovascular disease risk factors, lifestyle, dietary factors, and other circulating fatty acids, which minimized the influence of confounding. Because there has been only a single previous study of dairy fat biomarkers and stroke, our findings add significant new evidence to the limited knowledge in this field.
Potential limitations should be considered. A random misclassification of fatty acid concentrations because of either laboratory variation or biologic changes over time might have attenuated results toward the null. However, we have observed significant associations of these dairy fatty acid biomarkers with incident diabetes in these same cohorts (Yakoob et al., personal communication, 2014), which suggested that meaningful relations can be detected. Although we adjusted for many key confounders, residual confounding by other nutrients in dairy products such as vitamin D, magnesium, phosphorus, and dairy protein could not be excluded. Finally, we had a relatively limited statistical power to test associations with stroke subtypes, particularly hemorrhagic stroke. These limitations highlight the need for additional biomarker studies of dairy fat and stroke to better inform dietary recommendations. Nonetheless, to our knowledge, ours is the largest study to date of these fatty acid biomarkers and incident stroke. Participants in these cohorts were educated U.S. health professionals, and absolute concentrations of these fatty acids and absolute rates of stroke may not be generalizable to other populations. However, there was no reason to expect a biological effect modification of the observed HR on the basis of differences in education, race, or geography. Relative associations of risk factors with disease events seen in many other specific population groups (e.g., the Framingham Heart Study and Physician's Health Study) have been generalizable to many other populations. Instead, the recruitment of educated participants enabled us to obtain especially valid and reliable data on diet, other covariates, and our outcomes of interest.
In conclusion, our results do not support associations of circulating biomarkers of dairy fat with risk of stroke in men or women.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—MYY, FBH, and DM: participated in the project conception and development of the research plan; FBH and DM: obtained funding and provided study oversight; MYY, PS, and EJO: analyzed data and performed the statistical analysis; MYY and DM: drafted the manuscript; and FBH, HC, KMR, EJO, WCW, and DM: provided critical intellectual input on methods and analyses and feedback on manuscript revisions. DM reported membership with the Unilever North America Scientific Advisory Board. Harvard University has filed a provisional patent application that has been assigned to Harvard University listing DM as a co-inventor to the US Patent and Trademark Office for use of trans palmitoleic acid to prevent and treat insulin resistance, type 2 diabetes, and related conditions. MYY, PS, FBH, HC, KMR, EJO, and WCW declared no conflicts of interest.
Footnotes
Abbreviations used: HPFS, Health Professionals Follow-Up Study; ICC, intraclass correlation coefficient; NHS, Nurses’ Health Study; RBC, red blood cell.
REFERENCES
- 1.Fleming KH, Heimbach JT. Consumption of calcium in the US: food sources and intake levels. J Nutr 1994;124(Suppl):1426S–30S. [DOI] [PubMed] [Google Scholar]
- 2.National Dairy Council. Role of Dairy Foods in a Healthy Diet: A Focus on Food Guide Pyramid Dairy Servings Recommendations [Internet]. [cited 2014 Sep 1]. Available from: http://www.nationaldairycouncil.org/SiteCollectionDocuments/footer/public_comments/nutrition_guidelines/DGACFinal3.pdf.
- 3.Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr 2003;77:1146–55. [DOI] [PubMed] [Google Scholar]
- 4.Micha R, Mozaffarian D. Saturated fat and cardiometabolic risk factors, coronary heart disease, stroke, and diabetes: a fresh look at the evidence. Lipids 2010;45:893–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khoury JC, Kleindorfer D, Alwell K, Moomaw CJ, Woo D, Adeoye O, Flaherty ML, Khatri P, Ferioli S, Broderick JP, et al. Diabetes mellitus: a risk factor for ischemic stroke in a large biracial population. Stroke 2013;44:1500–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lindsberg PJ, Grau AJ. Inflammation and infections as risk factors for ischemic stroke. Stroke 2003;34:2518–32. [DOI] [PubMed] [Google Scholar]
- 7.Banerjee C, Moon YP, Paik MC, Rundek T, Mora-McLaughlin C, Vieira JR, Sacco RL, Elkind MS. Duration of diabetes and risk of ischemic stroke: the Northern Manhattan Study. Stroke 2012;43:1212–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Stroke Association. Controllable risk factors - cholesterol [Internet]. [cited 2013 Sep 4]. Available from: http://www.stroke.org/site/PageServer?pagename=cholesterol.
- 9.Massey LK. Dairy food consumption, blood pressure and stroke. J Nutr 2001;131:1875–8. [DOI] [PubMed] [Google Scholar]
- 10.Alvarez-León EE, Roman-Vinas B, Serra-Majem L. Dairy products and health: a review of the epidemiological evidence. Br J Nutr 2006;96(suppl 1):S94–9. [DOI] [PubMed] [Google Scholar]
- 11.Phelan M, Kerins D. The potential role of milk-derived peptides in cardiovascular disease. Food Funct 2011;2:153–67. [DOI] [PubMed] [Google Scholar]
- 12.Rodrigues SF, Vital SA, Granger DN. Mild hypercholesterolemia blunts the proinflammatory and prothrombotic effects of hypertension on the cerebral microcirculation. J Cereb Blood Flow Metab 2013;33:483–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yamagishi K, Iso H, Kokubo Y, Saito I, Yatsuya H, Ishihara J, Inoue M, Tsugane S. Dietary intake of saturated fatty acids and incident stroke and coronary heart disease in Japanese communities: the JPHC Study. Eur Heart J 2013;34:1225–32. [DOI] [PubMed] [Google Scholar]
- 14.Hu D, Huang J, Wang Y, Zhang D, Qu Y. Dairy foods and risk of stroke: a meta-analysis of prospective cohort studies. Nutr Metab Cardiovasc Dis 2014;24:460–96. [DOI] [PubMed] [Google Scholar]
- 15.Elwood PC, Pickering JE, Givens DI, Gallacher JE. The consumption of milk and dairy foods and the incidence of vascular disease and diabetes: an overview of the evidence. Lipids 2010;45:925–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soedamah-Muthu SS, Ding EL, Al-Delaimy WK, Hu FB, Engberink MF, Willett WC, Geleijnse JM. Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr 2011;93:158–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smedman AE, Gustafsson IB, Berglund LG, Vessby BO. Pentadecanoic acid in serum as a marker for intake of milk fat: relations between intake of milk fat and metabolic risk factors. Am J Clin Nutr 1999;69:22–9. [DOI] [PubMed] [Google Scholar]
- 18.Wolk A, Furuheim M, Vessby B. Fatty acid composition of adipose tissue and serum lipids are valid biological markers of dairy fat intake in men. J Nutr 2001;131:828–33. [DOI] [PubMed] [Google Scholar]
- 19.Brevik A, Veierod MB, Drevon CA, Andersen LF. Evaluation of the odd fatty acids 15:0 and 17:0 in serum and adipose tissue as markers of intake of milk and dairy fat. Eur J Clin Nutr 2005;59:1417–22. [DOI] [PubMed] [Google Scholar]
- 20.Hirahatake KM, Slavin JL, Maki KC, Adams SH. Associations between dairy foods, diabetes, and metabolic health: potential mechanisms and future directions. Metabolism 2014;63:618–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun Q, Ma J, Campos H, Hu FB. Plasma and erythrocyte biomarkers of dairy fat intake and risk of ischemic heart disease. Am J Clin Nutr 2007;86:929–37. [DOI] [PubMed] [Google Scholar]
- 22.Hu FB, Stampfer MJ, Manson JE, Ascherio A, Colditz GA, Speizer FE, Hennekens CH, Willett WC. Dietary saturated fats and their food sources in relation to the risk of coronary heart disease in women. Am J Clin Nutr 1999;70:1001–8. [DOI] [PubMed] [Google Scholar]
- 23.Warensjö E, Smedman A, Stegmayr B, Hallmans G, Weinehall L, Vessby B, Johansson I. Stroke and plasma markers of milk fat intake–a prospective nested case-control study. Nutr J 2009;8:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Colditz GA, Manson JE, Hankinson SE. The Nurses’ Health Study: 20-year contribution to the understanding of health among women. J Womens Health 1997;6:49–62. [DOI] [PubMed] [Google Scholar]
- 25.Mozaffarian D, Ascherio A, Hu FB, Stampfer MJ, Willett WC, Siscovick DS, Rimm EB. Interplay between different polyunsaturated fatty acids and risk of coronary heart disease in men. Circulation 2005;111:157–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baylin A, Kabagambe EK, Siles X, Campos H. Adipose tissue biomarkers of fatty acid intake. Am J Clin Nutr 2002;76:750–7. [DOI] [PubMed] [Google Scholar]
- 27.Katan MB, Deslypere JP, van Birgelen AP, Penders M, Zegwaard M. Kinetics of the incorporation of dietary fatty acids into serum cholesteryl esters, erythrocyte membranes, and adipose tissue: an 18-month controlled study. J Lipid Res 1997;38:2012–22. [PubMed] [Google Scholar]
- 28.Klingler M, Klem S, Demmelmair H, Koletzko B. Comparison of the incorporation of orally administered DHA into plasma, erythrocyte and cheek cell glycerophospholipids. Br J Nutr 2013;109:962–8. [DOI] [PubMed] [Google Scholar]
- 29.Hodson L, Eyles HC, McLachlan KJ, Bell ML, Green TJ, Skeaff CM. Plasma and erythrocyte fatty acids reflect intakes of saturated and n−6 PUFA within a similar time frame. J Nutr 2014;144:33–41. [DOI] [PubMed] [Google Scholar]
- 30.Skeaff CM, Hodson L, McKenzie JE. Dietary-induced changes in fatty acid composition of human plasma, platelet, and erythrocyte lipids follow a similar time course. J Nutr 2006;136:565–9. [DOI] [PubMed] [Google Scholar]
- 31.Kotsopoulos J, Tworoger SS, Campos H, Chung FL, Clevenger CV, Franke AA, Mantzoros CS, Ricchiuti V, Willett WC, Hankinson SE, et al. Reproducibility of plasma and urine biomarkers among premenopausal and postmenopausal women from the Nurses’ Health Studies. Cancer Epidemiol Biomarkers Prev 2010;19:938–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeleniuch-Jacquotte A, Chajes V, Van Kappel AL, Riboli E, Toniolo P. Reliability of fatty acid composition in human serum phospholipids. Eur J Clin Nutr 2000;54:367–72. [DOI] [PubMed] [Google Scholar]
- 33.Walker AE, Robins M, Weinfeld FD. The National Survey of Stroke. Clinical findings. Stroke 1981;12(Suppl 1):I13–44. [PubMed] [Google Scholar]
- 34.Zhang L, Curhan GC, Hu FB, Rimm EB, Forman JP. Association between passive and active smoking and incident type 2 diabetes in women. Diabetes Care 2011;34:892–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wolf AM, Hunter DJ, Colditz GA, Manson JE, Stampfer MJ, Corsano KA, Rosner B, Kriska A, Willett WC. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol 1994;23:991–9. [DOI] [PubMed] [Google Scholar]
- 36.Chasan-Taber S, Rimm EB, Stampfer MJ, Spiegelman D, Colditz GA, Giovannucci E, Ascherio A, Willett WC. Reproducibility and validity of a self-administered physical activity questionnaire for male health professionals. Epidemiology 1996;7:81–6. [DOI] [PubMed] [Google Scholar]
- 37.Zhang X, Smith-Warner SA, Chan AT, Wu K, Spiegelman D, Fuchs CS, Willett WC, Giovannucci EL. Aspirin use, body mass index, physical activity, plasma C-peptide, and colon cancer risk in US health professionals. Am J Epidemiol 2011;174:459–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Feskanich D, Rimm EB, Giovannucci EL, Colditz GA, Stampfer MJ, Litin LB, Willett WC. Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc 1993;93:790–6. [DOI] [PubMed]
- 39.Salvini S, Hunter DJ, Sampson L, Stampfer MJ, Colditz GA, Rosner B, Willett WC. Food-based validation of a dietary questionnaire: the effects of week-to-week variation in food consumption. Int J Epidemiol 1989;18:858–67. [DOI] [PubMed] [Google Scholar]
- 40.American Stroke Association. American College of Physicians Special Report [Internet]. Don't wait for it to happen to you - reducing your risk of stroke. [Updated 2013; cited 2014 Sep 1]. Available from: http://www.acponline.org/patients_families/pdfs/health/stroke.pdf.
- 41.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med 2011;364:2392–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology 1990;1:466–73. [DOI] [PubMed] [Google Scholar]
- 43.Ascherio A, Rimm EB, Giovannucci EL, Colditz GA, Rosner B, Willett WC, Sacks F, Stampfer MJ. A prospective study of nutritional factors and hypertension among US men. Circulation 1992;86:1475–84. [DOI] [PubMed] [Google Scholar]
- 44.Colditz GA, Martin P, Stampfer MJ, Willett WC, Sampson L, Rosner B, Hennekens CH, Speizer FE. Validation of questionnaire information on risk factors and disease outcomes in a prospective cohort study of women. Am J Epidemiol 1986;123:894–900. [DOI] [PubMed] [Google Scholar]
- 45.Orsini N, Bellocco R, Greenland S. Generalized least squares for trend estimation of summarized dose-response data. The Stata J 2006;6(1):40–57. Available from: http://www.stata-journal.com/article.html?article=st0096.
- 46.de Oliveira Otto MC, Nettleton JA, Lemaitre RN, Steffen LM, Kromhout D, Rich SS, Tsai MY, Jacobs DR, Mozaffarian D. Biomarkers of dairy fatty acids and risk of cardiovascular disease in the multi-ethnic study of atherosclerosis. J Am Heart Assoc 2013;2:e000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. doi: 10.3945/ajcn.113.076117. Jaudszus A, Kramer R, Pfeuffer M, Roth A, Jahreis G, Kuhnt K trans. Palmitoleic acid arises endogenously from dietary vaccenic acid. Am J Clin Nutr 2014;99:431–5. [DOI] [PubMed] [Google Scholar]
- 48.Sun Q, Ma J, Campos H, Hankinson SE, Hu FB. Comparison between plasma and erythrocyte fatty acid content as biomarkers of fatty acid intake in US women. Am J Clin Nutr 2007;86:74–81. [DOI] [PubMed]
- 49.Mao PJ, Zhang C, Tang L, Xian YQ, Li YS, Wang WD, Zhu XH, Qiu HL, He J, Zhou YH. Effect of calcium or vitamin D supplementation on vascular outcomes: a meta-analysis of randomized controlled trials. Int J Cardiol 2013;169:106–11. [DOI] [PubMed] [Google Scholar]
- 50.Prentice RL, Pettinger MB, Jackson RD, Wactawski-Wende J, Lacroix AZ, Anderson GL, Chlebowski RT, Manson JE, Van Horn L, Vitolins MZ, et al. Health risks and benefits from calcium and vitamin D supplementation: Women's Health Initiative clinical trial and cohort study. Osteoporos Int 2013;24:567–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Guessous I, Bochud M, Bonny O, Burnier M. Calcium, vitamin D and cardiovascular disease. Kidney Blood Press Res 2011;34:404–17. [DOI] [PubMed] [Google Scholar]
- 52.Chiba T, Itoh T, Tabuchi M, Ooshima K, Satou T, Ezaki O. Delay of stroke onset by milk proteins in stroke-prone spontaneously hypertensive rats. Stroke 2012;43:470–7. [DOI] [PubMed] [Google Scholar]
- 53.Bernstein AM, Pan A, Rexrode KM, Stampfer M, Hu FB, Mozaffarian D, Willett WC. Dietary protein sources and the risk of stroke in men and women. Stroke 2012;43:637–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


