Abstract
We describe the feasibility of a Web-based portal for training peer community health advisors (CHAs). We conducted a community-based implementation trial in African American churches between 2012 and 2014. The Web-based portal allows CHAs to log in and view 13 training videos, preparing them to deliver 3 cancer early detection workshops in their churches. Of 8 churches, 6 completed the training, each certifying 2 CHAs. These CHAs took an average of 26 days to complete the training, requiring little technical assistance. Additional technical assistance was required to implement the workshops. The Web-based system appears to be a feasible method for training lay individuals for the CHA role and has implications for increasing the reach of evidence-based interventions.
It has been well documented that many evidence-based health promotion interventions fail to achieve further implementation or use in the communities they are intended to serve.1 Such interventions, without intentional effort, do not disseminate themselves into practice.2 Interest in dissemination and implementation research is growing. Consistent with Rabin et al.,3 we use the term dissemination to refer to the active process of spreading evidence-based interventions to a particular audience using planned approaches and the term implementation to refer to the processes of integrating evidence-based interventions within a setting. We use the phrase dissemination and implementation to refer to the broader field in general.
Previous dissemination and implementation research has mainly focused on health care settings. More research is needed to identify optimal ways to translate research evidence into practice, including interventions in community settings that use community-based participatory methods.4 This includes research on successful implementation of interventions serving culturally and ethnically diverse populations.2 Peer health educators are viewed as a promising strategy to achieve this goal.5 Volunteer laypeople, such as those used in the community health advisor (CHA) model, have been used worldwide to promote health.6 This model for community health promotion recognizes that CHAs are cultural insiders and trusted sources of information and can help increase access to health care while naturally building capacity in the community for sustained positive health outcomes.6–10
ROLE OF TECHNOLOGY IN DISSEMINATION AND IMPLEMENTATION
Taking advantage of today’s continuously evolving technology landscape enhances the capacity to close the gap between research discovery and program delivery.11 The Pew Foundation Health Online 2013 report found that of the 81% of US adults who use the Internet, 59% indicated that they use it to obtain health information.12 With increased accessibility and technological outlets paving the way for an empowered and computer-literate public, there has been an ever-growing emphasis on eHealth, or the use of interactive technologies—the Internet, social media, personal digital assistants, cellular phones, and computer kiosks—to disseminate health information, promote health-related behavior change, and encourage informed decision-making.13–16 Effective health promotion interventions incorporating eHealth technologies have been reported in a variety of areas, including but not limited to smoking cessation, weight management, anxiety and depression, substance use disorders, diabetes self-management, HIV risk behavior, and asthma management.14,16
In addition, the focus on integrating eHealth tools in peer health education interventions to reach more diverse and broader audiences is increasing.17–27 One such intervention is the Centers for Disease Control and Prevention’s Web-based e-learning course for promoting the engagement of professional community health workers.25 The attraction of these eHealth interventions stems from a number of factors, including increasing access to technology, the potential for wide reach, reduced delivery costs, convenience to users, enhanced fidelity, and the reduction of geographically based, time-based, and mobility-based barriers.28–32 For example, using Web-based technology increases the potential for wider dissemination and implementation of efficacious programs through peer advisors in medically underserved communities.
Currently, a number of applications have been designed to train community health workers (also known as lay health workers or promotoras) via the Internet. However, these programs appear to cater to professional community health workers—health professionals seeking continuing education or supplemental education—or are offered as a formalized course with a dedicated instructor and applicable tuition fees.17–27 To our knowledge, the current project is one of the first applications of a Web-based training for a volunteer CHA curriculum that caters to individuals with little to no health background. This approach has the potential to be scalable to reach faith-based institutions both nationally and globally. It also has wider implications for use in other lay CHA training interventions that cover various geographic settings, health topics, or cultural settings.
PROJECT HEAL WEB-BASED TRAINING
In this article, we describe the feasibility of using a new Web-based portal for training lay CHAs. The training was done in the context of Project HEAL (Health through Early Awareness and Learning), a community-based implementation trial in African American churches. The Project HEAL intervention aims to increase early detection of breast, prostate, and colorectal cancer using an evidence-based approach.33–35 Project HEAL compares 2 types of training for lay CHAs: traditional classroom training (TC-CHA) versus technology-based training offered through a Web-based portal (TB-CHA). We compare implementation outcomes from these 2 training approaches, including feasibility of training completion, CHA implementation of the HEAL intervention, and data from CHA satisfaction and postintervention evaluation surveys. We conclude with lessons learned from this process and areas for future research.
Overview
The parent project providing the context for this article, Project HEAL, was a community-based implementation trial that compared 2 strategies for training CHAs to implement evidence-based cancer communication interventions in African American churches.36 This research was conducted in Prince George’s County, Maryland, which has the highest percentage of racial/ethnic minorities in Maryland (65.3% African American), a wide range in socioeconomic status, and a significant proportion of residents affected by health disparities.37
Project HEAL used a cluster randomized design in which CHAs in self-identified African American churches were randomly assigned by church to either the TC-CHA or the TB-CHA training approach. Both approaches used peer CHAs to implement a series of 3 educational workshops on early detection of breast, prostate, and colorectal cancer in their churches. The full Project HEAL intervention components are described in more detail elsewhere.36
Integrated Web-Based Training Curriculum
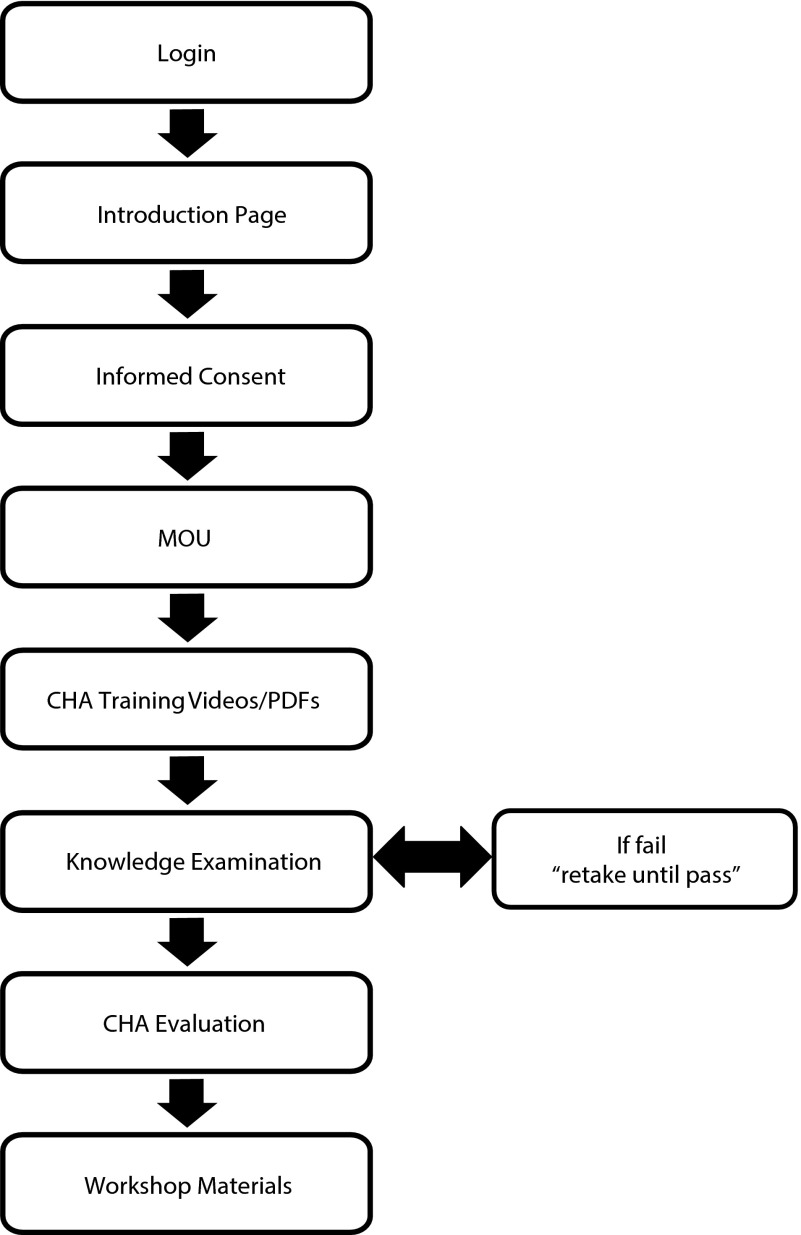
The technology-based approach to training CHAs is accessed via a Web-based portal that provides CHAs with a complete training curriculum consisting of informed consent, a memorandum of understanding, 13 content-specific training videos (e.g., overview of cancer, breast cancer, leadership skills, ethical issues) with corresponding PDFs, and CHA certification after passing a knowledge examination (Figure 1). Project intervention materials (e.g., cancer resource guide outlining local health care resources) and sets of PowerPoint slides for 3 workshops (i.e., cancer overview, breast and prostate cancer, and colorectal cancer) are provided in a downloadable format.
FIGURE 1—
Project HEAL Web-based training flow diagram: Prince George’s County, MD, 2012–2014.
Note. CHA = community health advisor; HEAL = Health through Early Awareness and Learning; MOU = memorandum of understanding.
Combining Microsoft Visual Studio tools (Microsoft, Redmond, WA), an SQL database, and Web tools (i.e., HTML, CSS, JavaScript), we developed the Web-based CHA training portal. All document-based materials were delivered in PDF format for ease of accessibility across various platforms (e.g., PC, Mac, iOS). In accordance with dual-coding theory,38 which postulates facilitated learning and enhanced recall with the combined use of nonverbal and verbal stimuli, the content-specific training modules were developed and narrated in Microsoft PowerPoint as multimedia files and then converted to MOV format. The MOV file container format is capable of holding different data types (e.g., animation, graphics, video, text) and is a common multimedia format compatible with QuickTime (Apple Inc., Cupertino, CA), a widely available multimedia platform. To decrease download time for each training video, we chose YouTube to host the video contents. For evaluation purposes, programming allowed the study team to track the progress of each CHA through the training, including (1) total number of logins and logouts, (2) length of time spent logged in, (3) amount of times the knowledge examination was taken and retaken, and (4) incorrect certification examination answers.
The TC-CHA training delivered the same curriculum as the TB-CHA approach; however, the TC-CHAs received 6 hours of training in a small-group classroom setting using a didactic and discussion format, with content module presentations given by Project HEAL team members and expert speakers. HEAL project staff members provided this training in churches to the TC-CHAs in 2 sessions, using the same content as for the TB-CHAs, described next.
Technology-Based Community Health Advisor Training Process
In the Project HEAL trial phase, 15 churches were randomly assigned to the TB-CHA training group (n = 7) or the TC-CHA training group (n = 8; Figure 2). The pastor at each church identified 2 potential CHAs (1 man, 1 woman) who met the CHA eligibility requirements:
self-identified as African American,
older than 21 years,
regularly attended the enrolled church,
able to complete Project HEAL training,
had regular access to the Internet and felt comfortable completing Web-based training activities,
able to recruit 30 participants for the 3-part workshop series, and
able to lead the 3-part workshop series.
After TB-CHAs were identified and recruited by their respective pastors, study staff e-mailed each CHA a personalized username and password.
FIGURE 2—
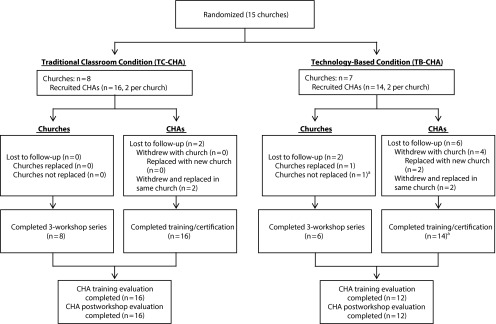
Flow diagram of Project HEAL church allocation and CHA recruitment: Prince George’s County, MD, 2012–2014.
Note. CHA = community health advisor; HEAL = Health through Early Awareness and Learning.
aCHAs trained and certified, but church dropped out before first workshop date; church not replaced because of late drop out.
Figure 1 depicts the Web-based training flowchart. CHAs had to complete each stage of the Web-based training before moving forward to the next stage. CHAs logged into the system, read an overview of the CHA training and curriculum (introduction page), and then read the informed consent and memorandum of understanding. A waiver of written informed consent was obtained from the institutional review board allowing CHAs to indicate agreement through an electronic acknowledgment system (i.e., “I agree” or “I do NOT agree”). Only on agreement could they proceed to the training materials. CHAs then had the option to view each of the 13 content-specific modules in 2 available formats to cater to varied learning styles or literacy levels: (1) a video of a narrated PowerPoint in MOV format, allowing CHAs to hear audio while reading the content, and (2) a downloadable PDF allowing CHAs to read and print the content.
Only when the CHAs downloaded all of the training modules could they proceed to the certification examination. This examination contained cancer-specific knowledge questions and questions related to conducting and leading the educational workshops. A score of 85% or higher was required for passing, and CHAs could retake the examination as many times as needed until they passed. With a passing score, CHAs could download their personalized certificate of training completion, a CHA training evaluation survey to be completed and returned to study staff via e-mail, and all materials necessary to conduct the Project HEAL 3-part educational workshop series (i.e., participant recruitment flyers, workshop sign-in sheets, workshop presentation slides, digital copies of the cancer educational booklets). CHAs could log in and out of the system as many times as needed until they reached training completion, and progress was saved at the last step completed. Contact information for study staff was provided should the CHAs have needed technical assistance at any point during the training.
WEB-BASED TRAINING IMPLEMENTATION OUTCOMES
The CHAs in both the TB-CHA training and TC-CHA training groups were of similar age (mean = 51.9 years; SD = 14.5; and mean = 51.0 years; SD = 11.8, respectively; Table 1). Most CHAs in both groups had Internet access at home and at work. However, the TB-CHAs had overall greater educational attainment than the TC-CHAs (83.3% vs 37.5% with a bachelor’s degree or higher, respectively).
TABLE 1—
CHA Demographic Profile and Evaluation of Training: Prince George’s County, MD, 2012–2014
| Variable | Technology-Based CHAs (n = 12), No. (%) or Mean ±SD | Traditional Classroom CHAs (n = 16), No. (%) or Mean ±SD |
| CHA demographic profile | ||
| Age, y | 51.9 ±14.5 | 51 ±11.8a |
| Home Internet access | 11 (91.7) | 16 (100.0) |
| Work Internet access | 9 (75.0) | 13 (86.7)a |
| Education | ||
| < bachelor’s degree | 2 (16.7) | 10 (62.5) |
| ≥ bachelor’s degree | 10 (83.3) | 6 (37.5) |
| Employment status | ||
| Retired or receiving disability | 2 (18.2)b | 5 (38.5)c |
| Part time | 2 (18.2) | 0 (0.0) |
| Full time | 7 (63.6) | 8 (61.5) |
| CHA posttraining satisfaction survey | ||
| CHA training “very useful” or “useful” for | ||
| Breast or prostate cancer awareness | 12 (100.0) | 16 (100.0) |
| Ease of understanding objective for breast or prostate cancer workshop | 11 (91.7) | 14 (87.5) |
| Colorectal cancer awareness | 12 (100.0) | 15 (93.8) |
| Ease of understanding objective for colorectal cancer workshop | 11 (91.7) | 15 (93.8) |
| CHA postworkshop evaluation | ||
| “Strongly agree” or “agree” CHA training materials were | ||
| Well organized | 10 (83.3) | 16 (100.0) |
| Useful in preparing for the workshops | 10 (83.3) | 16 (100.0) |
| Easy to understand | 10 (83.3) | 15 (93.8) |
| CHA is “very confident” or “confident” to | ||
| Recruit participants | 8 (66.6) | 12 (75.0) |
| Promote HEAL workshops | 8 (66.7) | 13 (81.3) |
| Present breast or prostate cancer workshops | 11 (91.7) | 14 (87.5) |
| Present colorectal cancer workshops | 12 (100.0) | 14 (87.5) |
| Respond to cancer-related questions and answers | 11 (91.7) | 13 (81.3) |
| Engage HEAL participants | 12 (100.0) | 13 (81.3) |
| “Strongly agree” or “agree” in conducting future health activities | ||
| Continue delivering Project HEAL workshops to CHA’s congregation | 11 (91.7) | 15 (100.0)a |
| Lead a different health activity in CHA’s congregation | 12 (100.0) | 10 (76.9)c |
| Recommend becoming a CHA to a peer | 12 (100.0) | 14 (100.0)d |
| Recommend Project HEAL to men and women in CHA’s church | 12 (100.0) | 14 (100.0)d |
| “Strongly agree” or “agree” the CHA certification process was fair | 11 (91.7) | 16 (100.0) |
| No. CHA certification examination attempts before passing with 85% | 1.6 ±0.8 | 1.7 ±0.5 |
Note. CHA = community health advisor; HEAL = Health through Early Awareness and Learning. Results are from CHAs that completed evaluations and excludes CHAs that dropped out.
n = 15.
n = 11.
n = 13.
n = 14.
Web-Based Training Feasibility
After the initial church randomization and CHA recruitment, 8 of the total 36 CHAs dropped out of Project HEAL (6 TB-CHAs and 2 TC-CHAs; Table 2 and Figure 2). Fourteen TB-CHAs were trained and certified through the Web-based training portal; 12 of these TB-CHAs are still enrolled in Project HEAL (2 TB-CHAs [1 church] were not replaced because of late dropout; Table 2 and Figure 2). All of the TB-CHAs who started the training passed the certification examination, though it is possible that they did not all pass on the first attempt. We have since updated the programming to collect more detailed data (e.g., length of time logged in, total examination attempts). We later asked for a self-report of this information after the completion of the workshop series. Most of the CHAs reported passing the certification examination on the first attempt (n = 7), and 5 CHAs each passed on the second or third attempt (mean = 1.6; SD = 0.8; Table 1). These results are comparable to the TC-CHA training (mean = 1.7; SD = 0.5). Table 2 details the CHAs’ Web-based training activity. During the training process, the TB-CHAs logged on an average of 9.6 times (SD = 4.7; range = 3.0–21.0).
TABLE 2—
Implementation Outcomes from CHAs Trained Online: Prince George’s County, MD, 2012–2014
| Church and CHA | Total Logins Until Certified, No. | Days From E-mail to Certification, No. | Weeks From Certification to First Workshop, No. |
| 1 | |||
| Advisor 1 | 12 | 7 | 11.1 |
| Advisor 2 | 10 | 8 | 11.0 |
| 2 | |||
| Advisor 1 | 8 | 18 | 3.4 |
| Advisor 2 | 9 | 16 | 3.7 |
| 3 | |||
| Advisor 1 | 3 | 0 | 22.3 |
| Advisor 2 | 4 | 4 | 21.7 |
| 4 | |||
| Advisor 1 | 8 | 40 | 13.9 |
| Advisor 2 | 8 | 7 | 18.6 |
| 5 | |||
| Advisor 1 | 6 | 70 | 22.0 |
| Advisor 2a | 21 | 15 | 6.0 |
| 6b | |||
| Advisor 1 | NA | NA | NA |
| Advisor 2 | NA | NA | NA |
| 7c | |||
| Advisor 1 | 7 | 33 | NA |
| Advisor 2 | 12 | 29 | NA |
| 8 | |||
| Advisor 1 | 10 | 89 | 23.6 |
| Advisor 2 | 16 | 34 | 29.3 |
| Mean (SD) | 9.6 (4.7) | 26.4 (25.9) | 15.6 (8.6) |
Note. CHA = community health advisor; NA = not applicable.
CHA replaced twice; both occurrences because of medical issues.
Church dropped out before CHAs trained and certified; replaced by church 8.
CHAs trained and certified, but church dropped out before first workshop date; church not replaced because of late dropout.
The protocol was modified after pilot testing to allow for a technical assistance meeting if CHAs had not logged into the training after the initial 2 weeks post-CHA recruitment. In the trial phase, however, none of the CHAs required such a technical assistance meeting to be initiated to move through the system. One church did request an in-person meeting after certification to discuss the workshop series format and other logistical questions. On average, the TB-CHAs took approximately 26 days from the time that they were granted access to the portal to the time that they became certified (SD = 25.9; range = 0.0–89.0; Table 2). All churches with certified TB-CHAs completed the workshop series (n = 6). Churches scheduled or completed their first workshop an average of 15 weeks after completing TB-CHA training (SD = 8.6; range = 3.4–29.3). These results are higher than the average 7 weeks it took for TC-CHAs to begin the workshop series (SD = 2.7; range = 3.4–12.1).
Community Health Advisor Posttraining Satisfaction Survey
After certifying as a Project HEAL CHA, TC-CHAs (n = 16) and TB-CHAs (n = 12) submitted a posttraining evaluation survey that assessed their satisfaction with the training. Four items assessed the usefulness of the CHA training materials on a 4-point Likert-type scale (ranging from 1 = “not useful” to 4 = “very useful”). Overall, CHAs in both groups were highly satisfied with the training, and we found minimal differences between groups (Table 1). For example, all of the CHAs in both groups felt the training was very useful or useful for creating breast and prostate cancer awareness (n = 28).
Postworkshop Evaluation of Community Health Advisor Training
We administered a separate CHA postworkshop survey after the CHAs delivered the 3-part workshop series. The purpose of this survey was to further evaluate the CHA training and assess CHA experiences in leading the workshops. Twelve of the TB-CHAs and 16 of the TC-CHAs completed the survey through self-administration (Table 1). The 2 groups of CHAs reported similar responses to 4-point Likert-type training evaluation items (ranging from 1 = “not at all confident” to 4 = “very confident”) such as confidence in recruiting participants and presenting the breast and prostate cancer workshops (Table 1). However, we found notable differences in that the TC-CHAs were more likely than the TB-CHAs to report that the training materials were well organized and useful in preparing for the workshops. In addition, the TB-CHAs were more likely than the TC-CHAs to report confidence in being able to engage workshop participants, presenting the colorectal cancer workshops, and responding to cancer-related questions. The TB-CHAs also had greater interest than the TC-CHAs in leading a subsequent health activity in their church in the future.
EVALUATION
This article suggests that use of a Web-based portal for training lay peer CHAs is feasible and presents implementation data that compare reasonably well with the data from classroom-trained CHAs. Both training methods ultimately led to (1) the successful training and certification of lay CHAs and (2) timely and successful delivery of CHA-led cancer educational workshops. Across both groups of CHAs, we saw similar responses on items assessing the usefulness of training and confidence in recruiting participants, indicating that integrating Internet technologies in a CHA training curriculum for lay individuals can have similar outcomes to an evidence-based traditional classroom training curriculum. An advantage of a Web-based CHA training is that it enables CHAs to complete the training at their own pace and reduces the scheduling challenges associated with a traditional classroom training approach.28 Our TB-CHAs were able to complete the training at their own pace and had the option to start and stop the training modules, a fundamental principle of effective Web-based trainings.16,28
Challenges and Lessons Learned
Even though the Web-based CHA training method was found to be feasible, it had some drawbacks compared with the traditional classroom training. The TB-CHAs took longer to complete training and twice as long to initiate the cancer educational workshops than the TC-CHAs. Dropout was higher among the TB-CHAs relative to the TC-CHAs. In addition, we saw some differences in ratings of the CHA training materials between the TC-CHAs and the TB-CHAs. Though a majority of the TB-CHAs responded favorably, a lower percentage of TB-CHAs than TC-CHAs found the training materials to be well organized, useful in preparing for the workshops, and easy to understand. The content and components of the CHA trainings were equivalent; the difference lay in the mode of delivery. Project HEAL was a robust and dynamic project that focused on 3 cancers, with a relatively complex intervention protocol. This may be an ambitious and complex design for a Web-based training with minimal technical assistance, designed for lay individuals with little to no health background. Future iterations of the Web-based materials may need to be simplified for ease of use with less technical assistance and greater scalability.
In the current trial, 6 TB-CHAs and 2 TC-CHAs did drop out. Of the 6 TB-CHAs, 4 dropped out because their respective churches (n = 2) chose to withdraw from the project, and another 2 could not complete the training for health reasons. The 2 churches that dropped out were smaller churches that were undergoing significant transitions, including a relocation process. The 2 TC-CHAs opted out of the project because of challenges scheduling an in-person CHA training session. They may have continued with the project had they been assigned to the TB-CHA group and been able to complete the training on their own schedule.
We originally envisioned that a Web-based training portal at which individuals would log in, complete training, and lead the 3-part workshop series in the relative absence of staff support would be a more efficient way to train CHAs and deliver an intervention than a traditional classroom training approach. However, during the piloting process we learned that it might be necessary to spend time building relationships and rapport with the CHAs before they initiated their Web-based training. It may be unrealistic to expect people to respond to an e-mail, log in to a Web-based system, and complete a lengthy training even if they are asked to do so by their church leadership. Having the option of an individual orientation and technical assistance meeting with the CHAs—though not used by the 6 TB-CHA churches during the trial phase—not only serves to familiarize them with the Web portal, but also gives them a human point of contact. This may be important when working in medically underserved populations in the context of a research study.
In addition, the need for staff support was particularly apparent in our trial phase when scheduling workshops on the church calendar. Our TB-CHAs and TC-CHAs took an average of 15 weeks and 7 weeks, respectively, to begin their workshop series after CHA training and certification. During this period, frequent contact was made between study staff and CHAs in both groups to assist churches and CHAs in the progression through the project timeline. Furthermore, 1 TB-CHA church requested an in-person meeting after certification to discuss the workshop series format and other logistical questions. However, none of the TB-CHAs required a technical assistance meeting to complete the training and certification independently, which suggests feasibility.
Limitations and Future Opportunities
The Project HEAL Web-based CHA training portal has a potentially large reach but is currently limited in generalizability to African American faith-based settings. This is because we used a culturally targeted approach involving content, graphics, and spiritual material, including religious themes and use of scripture. The training and intervention materials could be adapted for use with other populations using a cultural translation process. An example of an innovative solution to such a targeting issue is provided in Make It Your Own, which uses technology to provide customized small media health communication materials encouraging screening.39 This approach uses a library of graphics and targeted messages in various languages for individuals of different demographic subgroups.
Although technology may be more efficient and cost-effective than the traditional classroom training approach,29–32 reach is limited by the need for a minimal level of technical assistance and human contact, particularly when initiating the training and scheduling workshops on the church calendar. Whether a more passive diffusion approach of this portal would be adopted by faith-based organizations is not known; this is another potential avenue for future research. For example, the portal could be modified for direct access and could be advertised via church bulletins, social networks, church national organizations, or other existing avenues of communication in African American faith-based communities. With regard to cost-effectiveness, considerable start-up development and programming costs need to be considered. Future analyses should consider these costs in a systematic manner.
Finally, other issues such as general literacy, computer literacy, and receptivity to using and learning technology play a role in how easily individuals are able to interface with the Web-based training.14,40 Use of the training portal assumes computer access and a modest level of familiarity with computers and the Internet. This platform is not intuitive to all types of users, which was particularly relevant in our CHA population of African American middle-aged adults (mean age = 51 years) and for medically underserved populations.12,40,41 The Project HEAL training portal can be operated on a computer, smartphone, or tablet. These platforms make for greater access; however, the user still needs to be comfortable with the technology. Perhaps greater opportunities will arise to expand this type of project as these technologies diffuse through the younger generations of users—a population showing increased preference for Web-based applications.12,40
Although the digital divide resulting from race/ethnicity, age, income, and education is closing, disparities still exist in technology access.12 Indeed, our TB-CHAs were a small sample of relatively educated individuals, which may have contributed to their apparent comfort with Web-based training. Future research could examine individual characteristics that predict who is most likely to complete a Web-based CHA training (e.g., computer and Internet access, age, health factors). Future directions for the Project HEAL Web-based CHA training portal include expansion to other populations (e.g., Hispanic/Latino, Asian Americans, Native Americans), faiths (e.g., Islam), settings (e.g., CHAs trained through health care systems), and other chronic diseases (e.g., diabetes, hypertension). These may be promising ways to expand the reach and sustainability of this potentially effective method to train lay peer CHAs.
CONCLUSIONS
Using novel health communication strategies in today’s fast-changing technological environment can increase the capacity to close the gap between research discovery and program delivery.11 Even though we found the Project HEAL Web-based CHA training method to be feasible, it had limitations compared with the traditional classroom training in terms of efficiency in training completion, intervention implementation, and CHA dropout. These limitations may be reasonable in light of the potential for scalability and increased reach that the Web-based training may have, particularly to prepare lay individuals to educate underserved populations about chronic disease, thereby reducing health disparities. By building health capacity in the community through accessible and readily disseminated evidence-based interventions with high potential for sustainability, the impact on community health outcomes and positive societal change can increase greatly.
Acknowledgments
This work was supported by a grant from the National Cancer Institute (R01CA147313).
We acknowledge Janice Bowie, PhD, Muhiuddin Haider, PhD, and Tony Whitehead, PhD, for their extensive contributions to this study and Roxanne Carter and Rev. Alma Savoy, who conducted recruitment and data collection activities for the study.
Human Participant Protection
This work was approved by the University of Maryland institutional review board (no. 10-0691).
References
- 1.Glasgow RE, Marcus AC, Bull SS, Wilson KM. Disseminating effective cancer screening interventions. Cancer. 2004;101(5 suppl):1239–1250. doi: 10.1002/cncr.20509. [DOI] [PubMed] [Google Scholar]
- 2.National Institute of Mental Health. The Road Ahead: Research Partnerships to Transform Services—A Report by the National Advisory Mental Health Council’s Services Research and Clinical Epidemiology Workgroup. Bethesda, MD: National Institute of Mental Health; 2006. US Department of Health and Human Services. [Google Scholar]
- 3.Rabin BA, Brownson RC, Haire-Joshu D, Kreuter MW, Weaver NL. A glossary for dissemination and implementation research in health. J Public Health Manag Pract. 2008;14(2):117–123. doi: 10.1097/01.PHH.0000311888.06252.bb. [DOI] [PubMed] [Google Scholar]
- 4.Kerner JF, Guirguis-Blake J, Hennessey KD et al. Translating research into improved outcomes in comprehensive cancer control. Cancer Causes Control. 2005;16(suppl):27–40. doi: 10.1007/s10552-005-0488-y. [DOI] [PubMed] [Google Scholar]
- 5.Ellis P, Robinson P, Ciliska D . Diffusion and Dissemination of Evidence-Based Cancer Control Interventions. Rockville, MD: Agency for Healthcare Research and Quality; 2003. AHRQ Publication No. 03–E033. Available at: http://www.ncbi.nlm.nih.gov/books/NBK36992/#_ncbi_dlg_citbx_NBK36992. Accessed February 28, 2014. [PMC free article] [PubMed] [Google Scholar]
- 6.Witmer A, Seifer SD, Finocchio L, Leslie J, O’Neil EH. Community health workers: integral members of the health care work force. Am J Public Health. 1995;85(8 pt 1):1055–1058. doi: 10.2105/ajph.85.8_pt_1.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walt G. Community Health Workers in National Programmes: Just Another Pair of Hands? Philadelphia, PA: Open University Press; 1990. [Google Scholar]
- 8.Indian Health Service. Alaska Community Health Aide Program Description. Washington, DC: Government Printing Office; 1991. [Google Scholar]
- 9.Giblin PT. Effective utilization and evaluation of indigenous health care workers. Public Health Rep. 1989;104(4):361–368. [PMC free article] [PubMed] [Google Scholar]
- 10.Richter RW, Bengen B, Alsup PA, Bruun B, Kilcoyne MM, Challenor BD. The community health worker: a resource for improved health care delivery. Am J Public Health. 1974;64(11):1056–1061. doi: 10.2105/ajph.64.11.1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chou W-YS, Prestin A, Lyons C, Wen K-Y. Web 2.0 for health promotion: reviewing the current evidence. Am J Public Health. 2013;103(1):e9–e18. doi: 10.2105/AJPH.2012.301071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fox S, Duggan M. Health online 2013. Available at: http://www.pewinternet.org/files/old-media/Files/Reports/PIP_HealthOnline.pdf. Accessed May 31, 2013.
- 13.Eng TR. eHealth research and evaluation: challenges and opportunities. J Health Commun. 2002;7(4):267–272. doi: 10.1080/10810730290001747. [DOI] [PubMed] [Google Scholar]
- 14.Strecher V. Internet methods for delivering behavioral and health-related interventions (eHealth) Annu Rev Clin Psychol. 2007;3:53–76. doi: 10.1146/annurev.clinpsy.3.022806.091428. [DOI] [PubMed] [Google Scholar]
- 15.Turner-Lee N, Smedley BD, Miller JS. Minorities, mobile broadband, and the management of chronic diseases. Available at: http://jointcenter.org/sites/default/files/Minorities%20Mobile%20Broadband%20and%20the%20Management%20of%20Chronic%20Diseases_0.pdf. Accessed July 9, 2014.
- 16.Aronson ID, Marsch LA, Acosta MC. Using findings in multimedia learning to inform technology-based behavioral health interventions. Transl Behav Med. 2013;3(3):234–243. doi: 10.1007/s13142-012-0137-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Livestrong Foundation. Livestrong promotores program. Available at: http://www.livestrong.org/What-We-Do/Our-Actions/Professional-Tools-Training/LIVESTRONG-Promotores-Program. Accessed February 27, 2014.
- 18.Patient Navigator Training Collaborative. eLearning. Available at: http://patientnavigatortraining.org/courses/elearning-courses. Accessed February 11, 2014.
- 19.Texas Department of State Health Services. Community health workers: training information. Available at: http://www.dshs.state.tx.us/mch/chw/training.aspx. Accessed February 11, 2014.
- 20.Landon B, Loudon J, Selle M, Doucette S. Factors influencing the retention and attrition of community health aides/practitioners in Alaska. J Rural Health. 2004;20(3):221–230. doi: 10.1111/j.1748-0361.2004.tb00032.x. [DOI] [PubMed] [Google Scholar]
- 21.Massachusetts Department of Public Health. CHW training program details: community health worker online training. Available at: http://chwtraining.org/chw-training-program-details. Accessed February 27, 2014.
- 22.Indian Health Service. Education: Fundamentals of diabetes care. Available at: http://www.ihs.gov/chr/index.cfm?module=DiabetesFundamentals. Accessed July 9, 2014.
- 23.Minnesota Community Health Worker Alliance. CHW: Education. Available at: http://mnchwalliance.org/explore-the-field/education-2. Accessed February 24, 2014.
- 24.Rural Assistance Center. Community health workers toolkit. Available at: http://www.raconline.org/communityhealth/chw. Accessed February 24, 2014.
- 25.Brownstein JN, Mirambeau AM, Roland KB. News from the CDC: using Web-based training to translate evidence on the value of community health workers into public health action. Transl Behav Med. 2013;3(3):229–230. doi: 10.1007/s13142-013-0204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johns Hopkins Bloomberg School of Public Health. Training and learning programs for volunteer community health workers. Available at: http://www.coursera.org/course/commhealthworkers. Accessed February 19, 2014.
- 27.Center for Community Health Development. Center for Community Health Development’s Community Health Worker Training Center. Available at: http://www.cchd.us/pages/trainingcenter.html. Accessed February 10, 2014. [DOI] [PMC free article] [PubMed]
- 28.Glang A, Noell J, Ary D, Swartz L. Using interactive multimedia to teach pedestrian safety: an exploratory study. Am J Health Behav. 2005;29(5):435–442. doi: 10.5555/ajhb.2005.29.5.435. [DOI] [PubMed] [Google Scholar]
- 29.Griffiths F, Lindenmeyer A, Powell J, Lowe P, Thorogood M. Why are health care interventions delivered over the Internet? A systematic review of the published literature. J Med Internet Res. 2006;8(2):e10. doi: 10.2196/jmir.8.2.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bennett GG, Glasgow RE. The delivery of public health interventions via the Internet: actualizing their potential. Annu Rev Public Health. 2009;30:273–292. doi: 10.1146/annurev.publhealth.031308.100235. [DOI] [PubMed] [Google Scholar]
- 31.Lewis BA, Williams DM, Neighbors CJ, Jakicic JM, Marcus BH. Cost analysis of Internet vs. print interventions for physical activity promotion. Psychol Sport Exerc. 2010;11(3):246–249. doi: 10.1016/j.psychsport.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marsch LA. Technology-based interventions targeting substance use disorders and related issues: an editorial. Subst Use Misuse. 2011;46(1):1–3. doi: 10.3109/10826084.2011.521037. [DOI] [PubMed] [Google Scholar]
- 33.Holt CL, Klem PR. As you go, spread the word: spiritually based breast cancer education for African American women. Gynecol Oncol. 2005;99(3 suppl 1):S141–S142. doi: 10.1016/j.ygyno.2005.07.066. [DOI] [PubMed] [Google Scholar]
- 34.Holt CL, Wynn TA, Litaker MS, Southward P, Jeames S, Schulz E. A comparison of a spiritually based and non-spiritually based educational intervention for informed decision making for prostate cancer screening among church-attending African-American men. Urol Nurs. 2009;29(4):249–258. [PMC free article] [PubMed] [Google Scholar]
- 35.Holt CL, Litaker MS, Scarinci IC et al. Spiritually based intervention to increase colorectal cancer screening among African Americans: screening and theory-based outcomes from a randomized trial. Health Educ Behav. 2013;40(4):458–468. doi: 10.1177/1090198112459651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Holt CL, Tagai EK, Scheirer MA et al. Translating evidence-based interventions for implementation: experiences from Project HEAL in African American churches. Implement Sci. 2014;9:66. doi: 10.1186/1748-5908-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.US Census Bureau. Prince George’s County quickfacts. Available at: http://quickfacts.census.gov/qfd/states/24/24033.html. Accessed February 25, 2014.
- 38.Mayer R. Multimedia Learning. New York, NY: Cambridge University Press; 2001. [Google Scholar]
- 39.MIYO (Make It Your Own) [computer program] St. Louis, MO: Washington University in St. Louis, George Warren Brown School of Social Work, Health Communication Research Laboratory; Available at: http://www.miyoworks.org. Accessed July 9, 2014. [Google Scholar]
- 40.Greaney ML, Puleo E, Bennett GG et al. Factors associated with choice of Web or print intervention materials in the Healthy Directions 2 study. Health Educ Behav. 2014;41(1):52–62. doi: 10.1177/1090198113486803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Miller EA, West DM, Wasserman M. Health information Websites: characteristics of US users by race and ethnicity. J Telemed Telecare. 2007;13(6):298–302. doi: 10.1258/135763307781644852. [DOI] [PubMed] [Google Scholar]