Abstract
Objectives. We describe trends in receipt of preventive dental care among Medicaid-enrolled children in Pennsylvania between 2005 and 2010, comparing the US children of immigrants with their co-ethnic peers in nonimmigrant families.
Methods. We analyzed Pennsylvania Medicaid claims, birth records, and census data for children born in Pennsylvania and enrolled in Medicaid for 10 or more months during any of the calendar years assessed.
Results. Receipt of preventive dental care was more likely among Latino children in immigrant families than among their peers in nonimmigrant families; also, it was more likely among White children in immigrant families than among their peers in nonimmigrant families. Rates of preventive dental care use among African American and Asian children in immigrant and nonimmigrant families were comparable. From 2005 to 2010, the percentage of Latino children in nonimmigrant families who received preventive dental care increased from 33% to 61%. Changes in other groups were significant but less dramatic.
Conclusions. Receipt of preventive dental care has increased among Medicaid-enrolled children in Pennsylvania, with marked gains among Latino children. Within each racial/ethnic group, the children of immigrants were either more likely than or equally likely as children in nonimmigrant families to receive care.
Dental caries is the most common chronic pediatric disease in the United States and overwhelmingly affects poor and minority children.1–3 Data from the National Health and Nutrition Examination Survey show that, between 1999 and 2004, 67% of poor children aged 6 to 8 years had dental caries (teeth that had been damaged by decay).4 Among children aged 2 to 11 years, 55% of Mexican American, 43% of African American, and 39% of non-Latino White children have been shown to be affected by caries.5
Because childhood caries can be prevented with regular dental care, community water fluoridation, oral hygiene, and avoidance of cariogenic foods, improving children’s oral health is a public health priority.1,5–8 The Healthy People 2020 initiative aims to decrease caries in children and adolescents by 10% and to increase the proportion of low-income children and adolescents who receive preventive dental care by 10%.9 These goals are modest and achievable, particularly given that preventive dental care coverage is available for the majority (70%) of poor children in the United States through Medicaid’s Early and Periodic Screening, Diagnosis, and Treatment benefit.10
Despite this coverage level, there has not been wide-scale access to dental care among poor, insured children.11 In 2010, only 44% of Medicaid-enrolled children aged 3 to 5 years and 49% of Medicaid-enrolled children aged 6 to 14 years received preventive dental care.12 This represents a modest increase relative to previous years. In 2008, for example, 43% of children aged 3 to 6 years and 48% of children aged 7 to 11 years who had been enrolled in fee-for-service Medicaid for the entire year received preventive dental care.13 In 2005, 33% of Medicaid-enrolled children aged 3 to 5 years and 39% of Medicaid-enrolled children aged 6 to 14 years received any preventive dental care.14
Because states have variable procedures for collecting race and ethnicity data from enrollees, these analyses provide only limited insight into trends in receipt of oral health care among Medicaid-enrolled minority children.15 Prior Medicaid analyses have also failed to take into account the status of children in immigrant families, including children who are themselves immigrants or have at least one parent born outside of the United States or its territories.16 Children of immigrants are predominantly US citizens (89%) and account for 1 in 3 poor children, 78% of Asian children, and 58% of Latino children in the United States.17 They are less likely than their peers with nonimmigrant parents to use many types of medical services.18,19 For example, children in immigrant families are less likely to have a usual source of health care,18,20,21 to receive primary care in a patient-centered medical home,22 or to receive annual pediatric care.22,23 Barriers to care that are concentrated among the children of immigrants include limited English proficiency (only 56% of children in immigrant families have at least 1 English-proficient parent, as compared with 99% of other children) and lack of familiarity with the US health system.20,24,25
We sought to add to the literature by examining receipt of preventive dental care among Medicaid-enrolled children in Pennsylvania, with a specific focus on US-born children of immigrants. We used parent-identified race/ethnicity data derived from birth records to examine changes from 2005 to 2010 in dental care receipt and compare US-born children of immigrants with their co-ethnic peers in nonimmigrant families. We hypothesized that children of immigrants would be disadvantaged relative to other children within each racial/ethnic group.
METHODS
We used longitudinal Medicaid data from 2005 to 2010 to conduct an observational, repeated measures analysis of children aged 0 to 10 years in Pennsylvania. The study population was derived from the state’s Medicaid program. Income eligibility limits were 185% of the federal poverty level (FPL) for infants, 133% of the FPL for children aged 1 to 5 years, and 100% of the FPL for children aged 6 to 18 years during the study period.26–31 We linked 11 consecutive years of birth records (2000–2010) to Medicaid enrollment records for 2005 to 2010 via an algorithm in which records were linked sequentially through essential name and date of birth elements (e.g., last name, date of birth). Linkage was performed to obtain parental race and ethnicity data, as well as maternal nativity data, from the birth records. Forty-two percent of births during this period were linked to Medicaid enrollment records (see the Appendix, available as a supplement to the online version of this article at http://www.ajph.org). Given that 36% of Pennsylvanian children younger than 18 years and 47% of children aged 1 to 5 years were enrolled in Medicaid in 2009, this reflects a high linkage rate.32
In accord with the stepwise procedure outlined in Figure 1, children with linked birth and Medicaid records were eligible for the analytic sample if they resided within the state, they were enrolled in Medicaid for at least 10 months of any calendar year from 2005 to 2010, their last known address could be assigned to a 2010 American Community Survey Zip Code Tabulation Area (ZCTA), and they had no missing information regarding maternal nativity. If more than one child in the same family met these eligibility criteria, one of the children was randomly selected for inclusion. We used the 10-month Medicaid enrollment criterion rather than a full-year enrollment requirement because Pennsylvania had intermittently implemented 6-month (rather than 12-month) Medicaid renewal procedures during the study period, which could have led to brief gaps in coverage for a large number of children.26,33
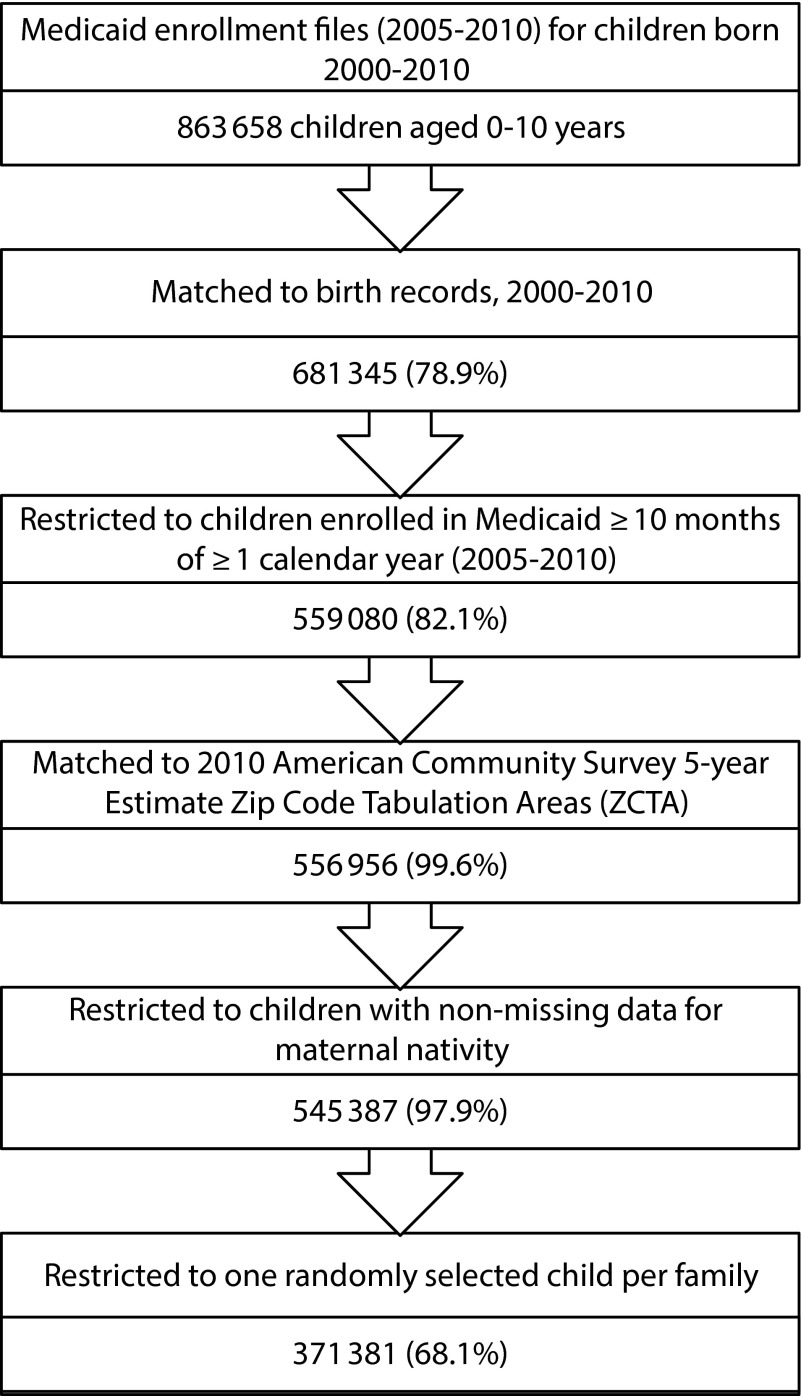
FIGURE 1—
Cohort development.
Requiring nonmissing maternal nativity data resulted in a small number of exclusions (2%). Children who were excluded for this reason were disproportionately likely to be African American, to be from urban ZCTAs in which a high proportion of residents were living below the FPL, and to have multiple missing data fields in their birth certificate (Table A, available as a supplement to the online version of this article at http://www.ajph.org). The final analytic sample included 371 381 children and 1 146 334 child-year observations.
Six consecutive years of Medicaid claims files (2005–2010) provided data on the primary outcome, annual receipt of preventive dental care. Annual receipt of preventive dental care was dichotomized according to the Centers for Medicare and Medicaid Services definition, which classifies preventive dental care as any Current Dental Terminology claim from D1000 through D1999.34 In this sample, nearly all (more than 98%) claims from these codes applied to prophylactic dental cleaning, fluoride varnish applied by an oral health provider, or sealants. This definition was selected to allow for comparisons with other state and federal data on use of preventive dental care and because it was comparable to definitions used by other authors.35–37 In the case of each child, the primary outcome was determined for each calendar year that she or he was included in the data set.
Variables
The primary independent variable combined race, ethnicity, and maternal nativity through data from state birth files.38 Each child’s race/ethnicity was derived from his or her parents’ self-reported race and ethnicity and categorized as follows: non-Latino White, non-Latino African American, non-Latino Asian, Latino (any race), mixed (indicating that the child’s mother and father differed from each other in their racial or ethnic heritage), and other (including children whose parents identified their ethnicity as non-Latino and their race as “other” or for whom race/ethnicity information was missing). Maternal nativity was dichotomized as US-born (including US territories) or non–US-born. We combined race/ethnicity and maternal nativity into a 12-level variable to compare children in immigrant and nonimmigrant families within the same racial/ethnic group.
The primary sources of data on the covariates assessed were birth files, 5-year estimates from the 2010 American Community Survey,39 the 2010 US census,40 and the Health Resources and Services Administration’s dental health provider shortage area (DHPSA) database (geographic DHPSAs are regions with limited access to dental professionals).41 Covariates were selected after a review of the pediatric oral health service literature.42 Adjusted models included both time-invariant (maternal education,43 neighborhood poverty,43 neighborhood density44,45) and time-varying (DHPSA,46,47 age,48 insurance49) covariates.
We categorized maternal educational attainment as less than high school, high school or equivalent, some college, bachelor’s degree or higher, and unknown (2.4%). We used the ZCTA of the child’s most recent address to assign neighborhood-specific covariates. Neighborhood poverty, a proxy for neighborhood socioeconomic status, was defined as the percentage of neighborhood residents living below the FPL50 and was categorized in quartiles as follows: 0% to 5.4% (level 1), 5.41% to 10.4% (level 2), 10.41% to 15.7% (level 3), and more than 15.7% (level 4).
Neighborhood density was categorized as high (> 1000 people per square mile), moderate (285–1000 people per square mile), or low (≤ 284 people per square mile). We selected these categories after mapping ZCTA-level population density as a continuous variable against designated rural and urban areas across the state51–53 via ArcGIS.54 The cutpoint for high density corresponded to the US Census Bureau’s definition, whereas that for low density corresponded to the definition used by the Commonwealth of Pennsylvania, allowing for comparisons with other Pennsylvania studies assessing urban–rural differences. Rural-Urban Commuting Area codes, which were designed to categorize degrees of rurality across the entire United States, were not used because they incorporate data on commuter behavior in addition to a community’s size and density. We believed that, in the case of children, it would be more important to use a system that would describe the immediate residential environment rather than parents’ work environments.55
We created time-varying variables for each calendar year. DHPSA status was dichotomized for each zip code area. Age was categorized as 1 year or younger, 2 years, 3 years, 4 years, and 5 to 10 years. Children aged 5 to 10 years were grouped together because, consistent with other research,48,49 preliminary analyses indicated that their rates of dental care use were nearly identical. A 7-level insurance variable was created to indicate whether children were enrolled in Medicaid fee for service, one of the state’s 5 largest Medicaid managed care organizations, or one of the many small Medicaid managed care organizations that each individually covered less than 3% of the sample.
Data Analysis
For each age group and calendar year, we reviewed pairwise comparisons with respect to the primary independent variable and all covariates. Pearson χ2 and Fisher exact tests were used to compare children within each racial/ethnic group (Table 1). We used an unstructured matrix to construct generalized estimating equation (GEE) models for the binary outcome (preventive dental care or no care in the calendar year); models were constructed in Stata SE version 12.56 GEE modeling extends logistic regression by appropriately accounting for correlations within repeated measurements over time. This allowed us to include the same children in the data set for more than 1 calendar year, permitting a more accurate examination of changes over time. Excluding children with repeated measures (i.e., > 1 year of Medicaid enrollment) would have limited our results to an atypical population, as the mean duration of Medicaid enrollment within our analytic sample was more than 4 years. All models were adjusted for age group, year, the combined race/ethnicity and nativity variable, and the interactions between year and age group and between year and race/ethnicity and nativity. The fully adjusted model also included all other covariates.
TABLE 1—
Demographic Characteristics, by Race/Ethnicity and Maternal Nativity: Medicaid-Enrolled Children in Pennsylvania, 2005–2010
| White |
African American |
Asian |
Latino |
Mixed |
Other |
|||||||
| Characteristic | US-Born (n = 61 995), % | Immigrant (n = 1512), % | US-Born (n = 26 590), % | Immigrant (n = 1242), % | US-Born (n = 103), % | Immigrant (n = 1803), % | US-Born (n = 7379), % | Immigrant (n = 3757), % | US-Born (n = 12 240), % | Immigrant (n = 841), % | US-Born (n = 642), % | Immigrant (n = 371), % |
| Female | 45.1 | 45.8 | 48.0 | 47.7 | 46.6 | 45.1 | 47.7 | 47.8 | 47.6* | 43.7* | 47.2 | 49.6 |
| Maternal education | ||||||||||||
| Less than high school | 20.6** | 13.0** | 30.9** | 21.8** | 39.8 | 32.5 | 53.3** | 58.1** | 31.1** | 20.0** | 24.6** | 28.8** |
| High school or equivalent | 45.1 | 37.0 | 45.8 | 39.0 | 28.2 | 34.3 | 32.0 | 26.5 | 43.9 | 30.6 | 33.8 | 31.5 |
| Some college | 21.3 | 23.0 | 18.8 | 22.4 | 15.5 | 10.0 | 10.6 | 8.2 | 19.1 | 25.2 | 14.8 | 17.3 |
| Bachelor’s degree or above | 11.0 | 22.4 | 2.7 | 8.9 | 9.7 | 13.9 | 1.1 | 3.7 | 3.8 | 21.5 | 3.9 | 11.6 |
| Unknown | 2.1 | 4.6 | 3.8 | 8.0 | 6.8 | 9.4 | 3.0 | 3.5 | 2.1 | 2.7 | 22.9 | 10.8 |
| ZCTA poverty score | ||||||||||||
| 1 (0%–5.4%) | 16.6** | 23.4** | 2.7** | 5.4** | 15.5 | 16.9 | 3.8** | 11.8** | 10.1** | 16.8** | 10.0 | 13.2 |
| 2 (5.5%–10.4%) | 25.3 | 26.4 | 6.1 | 9.3 | 12.6 | 12.2 | 8.2 | 10.5 | 17.7 | 20.1 | 10.1 | 13.2 |
| 3 (10.5%–15.7%) | 31.2 | 26.3 | 13.1 | 17.6 | 6.8 | 12.1 | 9.5 | 19.6 | 22.2 | 17.8 | 15.1 | 13.2 |
| 4 (>15.7%) | 27.0 | 23.9 | 78.2 | 67.6 | 65.1 | 58.8 | 78.6 | 58.1 | 50.0 | 45.3 | 64.8 | 60.4 |
| ZCTA density | ||||||||||||
| High | 34.3** | 66.2** | 92.9* | 94.2* | 92.2 | 91.2 | 90.2** | 80.5** | 66.6** | 76.2** | 79.8** | 91.1** |
| Moderate | 30.0 | 20.9 | 6.4 | 4.9 | 4.9 | 6.9 | 7.6 | 15.8 | 22.2 | 15.8 | 12.9 | 8.4 |
| Low | 35.7 | 12.9 | 0.7 | 0.9 | 2.9 | 1.8 | 2.1 | 3.8 | 11.2 | 7.7 | 7.3 | 0.5 |
| DHPSA | 46.0** | 24.5** | 25.5** | 15.0** | 17.5 | 14.1 | 30.8** | 19.1** | 30.7** | 20.3** | 28.4** | 18.3** |
| Insurance provider identification no. | ||||||||||||
| 1 | 13.6** | 10.7** | 16.0** | 15.3** | 16.5 | 21.7 | 10.0** | 16.1** | 15.2** | 13.9** | 13.9** | 12.9** |
| 2 | 18.2 | 14.5 | 13.3 | 4.8 | 9.7 | 6.8 | 16.4 | 11.7 | 20.1 | 15.0 | 12.0 | 9.4 |
| 3 | 11.6 | 6.1 | 6.5 | 2.0 | 2.9 | 3.1 | 0.3 | 0.4 | 6.8 | 4.3 | 5.5 | 1.4 |
| 4 | 17.0 | 38.6 | 42.7 | 55.9 | 46.6 | 51.3 | 38.3 | 44.7 | 30.6 | 40.8 | 37.9 | 52.0 |
| 5 | 1.7 | 7.5 | 15.8 | 14.4 | 18.5 | 11.0 | 28.9 | 16.9 | 7.9 | 8.7 | 18.1 | 14.6 |
| 6 | 33.1 | 18.2 | 3.0 | 3.4 | 1.9 | 4.2 | 4.2 | 8.8 | 15.8 | 14.0 | 9.4 | 7.0 |
| 99 | 4.9 | 4.4 | 2.7 | 4.3 | 3.9 | 1.9 | 1.9 | 1.4 | 3.6 | 3.3 | 3.4 | 2.7 |
| Received preventive dental care | 51.0** | 62.4** | 58.0** | 63.0** | 70.9 | 73.0 | 64.4** | 77.8** | 58.9 | 60.4 | 60.0** | 70.9** |
Note. DHPSA = dental health provider shortage area; ZCTA = Zip Code Tabulation Area. Because many children in this repeated measures analysis were included in the sample across multiple years and different age groups, sample characteristics are presented for children aged 5–10 years in 2010. Pairwise comparisons are shown within each racial/ethnic group for each categorical variable. Insurance providers, which were not identified for this study, are numbered.
*P < .05; **P < .01.
We conducted a sensitivity analysis to confirm that our results did not change when the GEE models were modified to adjust the standard errors for clustering within the different geographic regions. In this analysis, we used an exchangeable correlation structure to model the pattern of association of measurements within each ZCTA. The findings were comparable, and thus we include only the results of the primary analysis.
Results are presented as predicted percentages and 95% confidence intervals (CIs). The predicted percentages were adjusted for repeated measures as well as covariates at the maternal, area, and health system levels. However, the results are comparable when presented as either raw or predicted percentages (data not shown). We focus on results for children aged 5 to 10 years with all covariates set to their mean values (Table 2); results for children younger than 5 years are presented in the Appendix. Statistical significance was set at P < .05 (2-sided).
TABLE 2—
Adjusted Use of Preventive Dental Care, by Race/Ethnicity and Maternal Nativity: Medicaid-Enrolled Children in Pennsylvania, 2005–2010
| 2005 |
2010 |
||||
| Race/Maternal Nativity | Predicted %a (95% CI) | Rankb | Predicted %a (95% CI) | Rankb | Change, %c |
| White | |||||
| US-born | 41.8 (40.8, 42.7) | 6 | 51.4 (51.0, 51.7) | 11 | 9.6 |
| Immigrant | 47.1 (43.6, 50.6) | 3 | 61.9 (60.2, 63.6) | 6 | 14.7 |
| African American | |||||
| US-born | 41.3 (40.2, 42.4) | 7 | 58.2 (57.7, 58.7) | 9 | 16.9 |
| Immigrant | 42.2 (38.3, 46.1) | 5 | 59.5 (57.7, 61.3) | 8 | 17.3 |
| Asian | |||||
| US-born | 48.0 (36.4, 59.7) | 2 | 63.1 (58.1, 68.2) | 4 | 15.1 |
| Immigrant | 49.3 (46.1, 52.5) | 1 | 68.9 (67.6, 70.3) | 2 | 19.6 |
| Latino | |||||
| US-born | 33.0 (31.3, 34.7) | 12 | 61.0 (60.2, 61.9) | 7 | 28.1 |
| Immigrant | 45.3 (42.7, 47.9) | 4 | 72.2 (71.4, 73.1) | 1 | 26.9 |
| Mixed | |||||
| US-born | 41.2 (39.8, 42.7) | 8 | 57.5 (56.9, 58.2) | 10 | 16.3 |
| Immigrant | 39.8 (34.2, 45.3) | 9 | 62.3 (60.2, 64.5) | 5 | 22.6 |
| Other | |||||
| US-born | 36.7 (31.7, 41.7) | 11 | 58.2 (55.3, 61.1) | 9 | 21.5 |
| Immigrant | 38.5 (30.0, 47.0) | 10 | 66.1 (63.3, 68.9) | 3 | 27.6 |
Note. CI = confidence interval.
Modeled via generalized estimating equations accounting for repeated measures over time and adjusted for all individual, area, and health system characteristics, as well as interactions between year and age group and between year and the combined race/ethnicity and nativity variable. Percentages were predicted for children aged 5–10 years with other covariates set to their mean values.
Assigned for each group and each year according to the predicted probability for the given year.
Predicted percentage for 2010 minus predicted percentage for 2005.
RESULTS
White children in immigrant families were less likely than their co-ethnic peers to live in impoverished neighborhoods or in DHPSAs; they were more likely to live in densely populated neighborhoods, and their mothers were more likely to be highly educated (Table 1). Relative to their co-ethnic peers, African American children in immigrant families were less likely to live in DHPSAs, and their mothers had higher levels of education. Asian children in immigrant families had mothers with higher levels of education but were otherwise similar to their co-ethnic peers. Latino children in immigrant families were less likely than their co-ethnic peers to live in areas that were impoverished or densely populated and less likely to live in DHPSAs.
The proportion of US-born, Medicaid-enrolled children who received preventive dental care rose significantly in all age groups over the study period, although dental care use remained below 60% overall and below 25% among children aged 2 years or younger (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). Among children aged 5 to 10 years, the percentage receiving annual preventive dental care rose from 41.1% in 2005 to 55.2% in 2010.
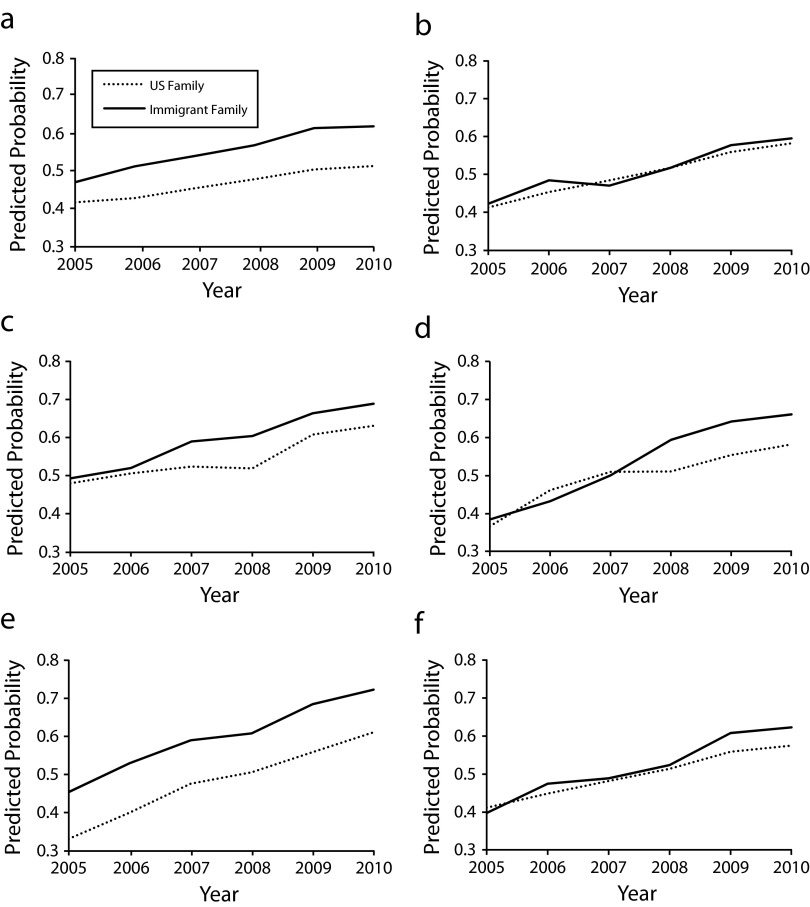
Disadvantage was not concentrated among US-born children of immigrants (Figure 2). Both before adjustment (Table C, available as a supplement to the online version of this article at http://www.ajph.org) and after adjustment for maternal, neighborhood, and health system characteristics, White children in immigrant families were more likely than White children in nonimmigrant families to have received preventive dental care at each time point (e.g., 61.9% and 51.4% of children in these groups, respectively, received care in 2010). Similarly, receipt of preventive dental care was more likely among Latino children in immigrant families (72.2% in 2010) than among their peers in nonimmigrant families (61.0% in 2010). Rates of preventive dental care use were moderate and comparable among African American children in immigrant and nonimmigrant families (e.g., 59.5% and 58.2%, respectively, in 2010). Rates of preventive dental care use were relatively high and comparable at each time point among Asian children in immigrant and nonimmigrant families (e.g., 68.9% and 63.1%, respectively, in 2010), although the confidence intervals around these estimates were wide owing to the small size of these subgroups (Table 2).
FIGURE 2—
Adjusted use of preventive dental care by Medicaid-enrolled children aged 5–10 years in nonimmigrant and immigrant families who self-identified as (a) White, (b) African American, (c) Asian, (d) other race/ethnicity, (e) Latino, and (f) mixed race/ethnicity: Pennsylvania, 2005–2010.
Note. Modeled using generalized estimating equations (link logit) accounting for repeated measures by child over time and adjusted for all individual, area, and health system characteristics, as well as interactions between year and age group and year and the combined variable for race/ethnicity and nativity. Probabilities were predicted for children aged 5–10 years with other covariates set to their mean values.
A review of trends over time revealed differences between groups (Figure 2). Latino children in nonimmigrant families demonstrated the largest gains over time, with 61% (95% CI = 60.2%, 61.9%) of these children receiving preventive dental care in 2010 in comparison with 33% (95% CI = 31.3%, 34.7%) in 2005 (Table 2). Substantial increases over the study period were also noted for Latino children in immigrant families (absolute difference = 26.9%). Receipt of dental care increased by approximately 17 percentage points among African American children, 15 percentage points among White children in immigrant families, and 10 percentage points among White children in nonimmigrant families during the study period. Trends over time were comparable among children younger than 5 years (Figure B, available as a supplement to the online version of this article at http://www.ajph.org).
DISCUSSION
Despite offering comprehensive dental coverage for children, state Medicaid programs have struggled to ensure that all enrolled children receive annual preventive care. However, our analysis shows that access to dental care among US-born, Medicaid-enrolled children has been improving in Pennsylvania, with increasing rates of dental care use among children in different age, racial/ethnic, and maternal nativity groups. These improvements are consistent with state and local initiatives to increase access to oral health care. During the study period, Pennsylvania increased Medicaid reimbursements, streamlined the provider enrollment process, and expanded the role of midlevel oral health providers by instituting the use of public health dental hygiene practitioners who could offer preventive services without supervision by a dentist in some settings.49,57,58 Pennsylvania has also seen increased benchmarking of managed care organizations; collaboration between oral health advocates, schools, and child-care providers; and sustained support for oral health access initiatives by philanthropic organizations and dental schools in the state’s largest urban centers.
In addition, we found that increasing access to care has resulted in gains for diverse groups of children, particularly Latino children and US-born children in immigrant families. This finding is surprising given that national survey data have consistently shown that Latino children and children in families of limited English proficiency are among those least likely to receive dental care.59–61 To our knowledge, Pennsylvania has not implemented large-scale programs specifically targeting Latino and immigrant families for oral health outreach. Furthermore, 34% of the foreign-born population in Pennsylvania has immigrated to the United States since 2000, often creating new communities of Latino, African, and Asian immigrants rather than joining well-established communities for whom bilingual dental care is already available.39,62,63
Additional mixed-methods research involving dental care providers and Latino and immigrant families is needed to better understand the situation in Pennsylvania, because there may be lessons learned that could be applied in other settings. We hypothesize that the dental workforce may be diversifying and hence may be increasingly open to caring for immigrant and minority families; in addition, increased attention to children’s oral health may have influenced the programs and policies of health, public health, and social service agencies targeting Latino and immigrant families (e.g., maternal–child home visitation programs) in ways that have not yet been documented. Another hypothesis is that Latino families may be highly receptive to dental services when they are accessible. This is suggested by a study in California in which receipt of insurance, including dental coverage, was associated with a doubling in rates of preventive dental care use among cohorts of predominantly Latino, immigrant children.64 However, we are also concerned that these changes may represent downstream effects of worsening oral health, as oral pain and visible disease may encourage families to seek care for their children, and dental caries remains common among poor children.1,4,5,65,66
Future research should also consider examining outcomes among specific Latino subgroups.67 In our study population, for example, 86% of Latino children in nonimmigrant families were of Puerto Rican heritage, whereas the majority of Latino children in immigrant families were of Mexican (54%) or “other” heritage (44%), meaning that their mothers did not self-identify as Mexican, Puerto Rican, or Cuban. Whether differences between Latino children in immigrant and nonimmigrant families are explained by family immigration status, cultural differences in attitudes toward oral health or oral health care, differences in parental English proficiency, or variations in the availability of services targeting specific ethnic subgroups remains to be explored.
Another surprising finding was the stagnation in use of preventive dental care services among White children in our sample. Although Medicaid-enrolled White children were more likely than other children to live in rural areas and DHPSAs and to have been enrolled in fee-for-service Medicaid, adjusting for these covariates did not account for the differences we observed. Future studies that seek to identify the factors responsible for increases in oral health care use among Latino children and children in immigrant families should also explore why these factors have been less influential among other children.
Limitations
This study is subject to certain limitations. Limitations on data access necessitated that the sample be restricted to children born from 2000 through 2010, and thus conclusions are not generalizable to older children. Nor are results applicable to foreign-born children, who represent a small overall percentage of children in immigrant families but are likely to be disproportionately affected by barriers to care, such as limited English proficiency. Similarly, our data were derived from a single state; given the many differences between state Medicaid programs, our results should not be generalized to other regions.
There are also limitations in our approach to cohort development. To ensure that we had relatively complete data on dental care use, we restricted the sample in each calendar year to children enrolled in Medicaid for at least 10 months. For this reason, our results are not representative of children enrolled for shorter periods. In addition, our sample may have suffered from selection bias. Specifically, by including only children with at least 10 months of enrollment, we may have captured an atypical group of immigrant families who were unusually skilled in navigating the health system, which would have allowed them to both maintain their Medicaid enrollment and obtain preventive care. However, we found that the median enrollment periods were very similar for children in immigrant and nonimmigrant families. In other words, our analytic sample may not be representative of all Medicaid-enrolled children, but selection bias is unlikely to explain our results.
Other limitations pertain to the definitions of key covariates. Neighborhood characteristics were derived from US census files linked to each child’s most recent home address and were treated as time-invariant characteristics, even though area characteristics may change over time and families may relocate. However, we found that 50% and 95% of children in the sample remained within 1 mile and 12 miles of their birth address, respectively, suggesting that relocation was not common. We did not include paternal nativity in our model because data on this variable were not collected in Pennsylvania until 2003 and were missing from 26% of birth records thereafter. However, in records without missing data, less than 3% of parental dyads consisted of a US-born mother and a foreign-born father, suggesting that including data on paternal nativity would not have significantly changed our results.
Also, our analysis focused on race and ethnicity, constructs that may not necessarily reflect meaningful social boundaries.68,69 For example, our data set did not include information on parental legal status, which may have a greater impact on health care use than race/ethnicity or the other covariates we were able to control for in our analysis.23,70 However, more nuanced approaches were not possible with claims data, and our approach is typical of health services research.
Finally, claims data may be vulnerable to misclassification bias. For example, dentists may provide preventive care without submitting appropriate dental claims, and as a result some children who have received preventive dental care may be misclassified as not having received care. However, we have no reason to believe that this kind of misclassification would be more or less common in different racial/ethnic and nativity groups, and thus it is less likely that misclassification of dental status substantially biased our results.
Conclusions
In Pennsylvania, receipt of preventive dental care has increased among Medicaid-enrolled children, including Latino children and US-born children in immigrant families. Future studies are needed to identify the factors responsible for these increases in dental care use and to understand why such factors have been more influential in the case of some children than others.
Acknowledgments
This work was supported by the University of Pennsylvania Leonard Davis Institute Pilot Grant Program and by the Agency for Healthcare Research and Quality (grant 1-K12-HS-021706-01). Data were provided by the Pennsylvania Department of Public Welfare and the Department of Health’s Bureau of Health Statistics and Research.
A poster based on this work was presented at the annual meeting of the Pediatric Academic Societies; May 3–6, 2014; Vancouver, British Columbia.
We are grateful to Victor Alos for his insight and feedback, Chris Feudtner for reviewing early drafts of the analytic plan, Zeinab Mohamad for her assistance with data linkage and management, Papia Paul for preparing the article for publication, and the anonymous reviewers for their time and expertise.
Note. The Pennsylvania Departments of Health and Public Welfare specifically disclaim responsibility for the analysis, interpretation, and conclusions of this article.
Human Participant Protection
This study was approved by the institutional review board of the Children’s Hospital of Philadelphia.
References
- 1.Dye BA, Tan S, Smith V . Trends in Oral Health Status: United States, 1988–1994 and 1999–2004. Hyattsville, MD: National Center for Health Statistics; 2007. [PubMed] [Google Scholar]
- 2.Dye BA, Arevalo O, Vargas CM. Trends in paediatric dental caries by poverty status in the United States, 1988–1994 and 1999–2004. Int J Paediatr Dent. 2010;20(2):132–143. doi: 10.1111/j.1365-263X.2009.01029.x. [DOI] [PubMed] [Google Scholar]
- 3.Vargas CM, Ronzio CR. Disparities in early childhood caries. BMC Oral Health. 2006;6(suppl 1):S3. doi: 10.1186/1472-6831-6-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dye BA, Thornton-Evans G. Trends in oral health by poverty status as measured by Healthy People 2010 objectives. Public Health Rep. 2010;125(6):817–830. doi: 10.1177/003335491012500609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edelstein BL, Chinn CH. Update on disparities in oral health and access to dental care for America’s children. Acad Pediatr. 2009;9(6):415–419. doi: 10.1016/j.acap.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 6.Sen B, Blackburn J, Morrisey M et al. Effectiveness of preventive dental visits in reducing nonpreventive dental visits and expenditures. Pediatrics. 2013;131(6):1107–1113. doi: 10.1542/peds.2012-2586. [DOI] [PubMed] [Google Scholar]
- 7.Oral Health in America: A Report of the Surgeon General. Washington, DC: US Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2000. [Google Scholar]
- 8.National Call to Action to Promote Oral Health. Rockville, MD: National Institute of Dental and Craniofacial Research; 2003. [PubMed] [Google Scholar]
- 9.Healthy People 2020. Washington, DC: US Department of Health and Human Services, Office of Disease Prevention and Health Promotion; 2013. [Google Scholar]
- 10.Henry J. Kaiser Family Foundation. Health insurance coverage of children 0–18 living in poverty. Available at: http://kff.org/other/state-indicator/poor-children. Accessed August 21, 2014.
- 11.Mofidi M, Rozier R, King R. Problems with access to dental care for Medicaid-insured children: what caregivers think. Am J Public Health. 2002;92(1):53–58. doi: 10.2105/ajph.92.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Annual EPSDT Participation Report: Form CMS-416 (National) Baltimore, MD: Centers for Medicare and Medicaid Services; 2010. [Google Scholar]
- 13.Bouchery E. Utilization of Dental Services Among Medicaid-Enrolled Children. Washington, DC: Mathematica Policy Research; 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Annual EPSDT Participation Report: Form CMS-416 (National) Baltimore, MD: Centers for Medicare and Medicaid Services; 2005. [Google Scholar]
- 15.Ulmer C, McFadden B, Nerenz DR. Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 16.Hernandez DJ. Children of Immigrants: Health, Adjustment, and Public Assistance. Washington, DC: National Academies Press; 1999. [PubMed] [Google Scholar]
- 17.Urban Institute. Children of Immigrants Data Tool. Available at: http://datatool.urban.org/charts/datatool/pages.cfm. Accessed August 21, 2014.
- 18.Ku L, Matani S. Left out: immigrants’ access to health care and insurance. Health Aff (Millwood) 2001;20(1):247–256. doi: 10.1377/hlthaff.20.1.247. [DOI] [PubMed] [Google Scholar]
- 19.Javier JR, Wise PH, Mendoza FS. The relationship of immigrant status with access, utilization, and health status for children with asthma. Ambul Pediatr. 2007;7(6):421–430. doi: 10.1016/j.ambp.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 20.Huang ZJ, Yu SM, Ledsky R. Health status and health service access and use among children in US immigrant families. Am J Public Health. 2006;96(4):634–640. doi: 10.2105/AJPH.2004.049791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin SC, Stella MY, Harwood RL. Autism spectrum disorders and developmental disabilities in children from immigrant families in the United States. Pediatrics. 2012;130(suppl 2):S191–S197. doi: 10.1542/peds.2012-0900R. [DOI] [PubMed] [Google Scholar]
- 22.BeLue R, Degboe A, Miranda P, Francis L. Do medical homes reduce disparities in receipt of preventive services between children living in immigrant and non-immigrant families? J Immigr Minor Health. 2012;14(4):617–625. doi: 10.1007/s10903-011-9540-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Javier JR, Huffman LC, Mendoza FS, Wise PH. Children with special health care needs: how immigrant status is related to health care access, health care utilization, and health status. Matern Child Health J. 2010;14(4):567–579. doi: 10.1007/s10995-009-0487-9. [DOI] [PubMed] [Google Scholar]
- 24.Baker DL, Miller E, Dang MT, Yaangh C-S, Hansen RL. Developing culturally responsive approaches with Southeast Asian American families experiencing developmental disabilities. Pediatrics. 2010;126(suppl 3):S146–S150. doi: 10.1542/peds.2010-1466I. [DOI] [PubMed] [Google Scholar]
- 25.Sanmartin C, Ross N. Experiencing difficulties accessing first-contact health services in Canada. Healthc Policy. 2006;1(2):103–119. [PMC free article] [PubMed] [Google Scholar]
- 26.Cohen Ross D, Cox L, Marks C. Resuming the Path to Health Coverage for Children and Parents: A 50 State Update on Eligibility Rules, Enrollment and Renewal Procedures, and Cost-Sharing Practices in Medicaid and SCHIP in 2006. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2007. [Google Scholar]
- 27.Cohen Ross D, Cox L. In a Time of Growing Need: State Choices Influence Health Coverage Access for Children and Families—A 50 State Update on Eligibility Rules, Enrollment and Renewal Procedures, and Cost-Sharing Practices in Medicaid and SCHIP for Children and Families. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2005. [Google Scholar]
- 28.Cohen Ross D, Marks C. Challenges of Providing Health Coverage for Children and Parents in a Recession: A 50 State Update on Eligibility Rules, Enrollment and Renewal Procedures, and Cost-Sharing Practices in Medicaid and SCHIP for Children and Families. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2009. [Google Scholar]
- 29.Cohen Ross D, Horn A, Marks C. Health Coverage for Children and Families in Medicaid and SCHIP: State Efforts Face New Hurdles—A 50 State Update on Eligibility Rules, Enrollment and Renewal Procedures, and Cost-Sharing Practices in Medicaid and SCHIP for Children and Families in 2008. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2008. [Google Scholar]
- 30.Cohen Ross D, Artiga S, Marks C. A Foundation for Health Reform: Findings of a 50 State Survey of Eligibility Rules, Enrollment and Renewal Procedures, and Cost-Sharing Practices in Medicaid and CHIP for Children and Parents During 2009. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2009. [Google Scholar]
- 31.Heberlein M, Brooks T, Guyer J, Artiga S, Stephens J. Holding Steady, Looking Ahead: Annual Findings of a 50-State Survey of Eligibility Rules, Enrollment and Renewal Procedures, and Cost-Sharing Practices in Medicaid and CHIP, 2010–2011. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2011. [Google Scholar]
- 32.Medicaid State Reports FY 2009: Pennsylvania. Washington, DC: American Academy of Pediatrics; 2009. [Google Scholar]
- 33.Fairbrother GL, Emerson HP, Partridge L. How stable is Medicaid coverage for children? Health Aff (Millwood) 2007;26(2):520–528. doi: 10.1377/hlthaff.26.2.520. [DOI] [PubMed] [Google Scholar]
- 34.Early and Periodic Screening, Diagnosis, and Treatment Report (CMS-416) Instructions. Baltimore, MD: Centers for Medicare and Medicaid Services; 2011. [Google Scholar]
- 35.Chi DL, Momany ET, Kuthy RA, Chalmers JM, Damiano PC. Preventive dental utilization for Medicaid-enrolled children in Iowa identified with intellectual and/or developmental disability. J Public Health Dent. 2010;70(1):35–44. doi: 10.1111/j.1752-7325.2009.00141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chi DL, Milgrom P. Preventive dental service utilization for Medicaid-enrolled children in New Hampshire: a comparison of care provided by pediatric dentists and general dentists. J Health Care Poor Underserved. 2009;20(2):458–472. doi: 10.1353/hpu.0.0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Savage MF, Lee JY, Kotch JB, Vann WF. Early preventive dental visits: effects on subsequent utilization and costs. Pediatrics. 2004;114(4):e418–e423. doi: 10.1542/peds.2003-0469-F. [DOI] [PubMed] [Google Scholar]
- 38.User Guide to the 2008 Natality Public Use File. Hyattsville, MD: Centers for Disease Control and Prevention, National Center for Health Statistics; 2008. [Google Scholar]
- 39.US Census Bureau. American Community Survey 5-year estimates. Available at: http://www.census.gov/acs. Accessed August 21, 2014.
- 40.US Census Bureau. 2010 US census. Available at: http://www.census.gov/2010census. Accessed August 21, 2014.
- 41.Health Resources and Services Administration. Health provider shortage areas by state and county. Available at: http://hpsafind.hrsa.gov. Accessed August 21, 2014.
- 42.Fisher-Owens SA, Gansky SA, Platt LJ et al. Influences on children’s oral health: a conceptual model. Pediatrics. 2007;120(3):e510–e520. doi: 10.1542/peds.2006-3084. [DOI] [PubMed] [Google Scholar]
- 43.Larson K, Russ SA, Crall JJ, Halfon N. Influence of multiple social risks on children’s health. Pediatrics. 2008;121(2):337–344. doi: 10.1542/peds.2007-0447. [DOI] [PubMed] [Google Scholar]
- 44.Martin AB, Vyavaharkar M, Veschusio C, Kirby H. Rural-urban differences in dental service utilization among an early childhood population enrolled in South Carolina Medicaid. Matern Child Health J. 2012;16(1):203–211. doi: 10.1007/s10995-010-0725-1. [DOI] [PubMed] [Google Scholar]
- 45.Vargas CM, Ronzio CR, Hayes KL. Oral health status of children and adolescents by rural residence, United States. J Rural Health. 2003;19(3):260–268. doi: 10.1111/j.1748-0361.2003.tb00572.x. [DOI] [PubMed] [Google Scholar]
- 46.Bhagavatula P, Xiang Q, Eichmiller F, Szabo A, Okunseri C. Racial/ethnic disparities in provision of dental procedures to children enrolled in Delta Dental insurance in Milwaukee, Wisconsin. J Public Health Dent. 2014;74(1):50–62. doi: 10.1111/j.1752-7325.2012.00366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chi DL, Leroux B. County-level determinants of dental utilization for Medicaid-enrolled children with chronic conditions: a new conceptual model. Health Place. 2012;18(6):1422–1429. doi: 10.1016/j.healthplace.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hakim RB, Babish JD, Davis AC. State of dental care among Medicaid-enrolled children in the United States. Pediatrics. 2012;130(1):5–14. doi: 10.1542/peds.2011-2800. [DOI] [PubMed] [Google Scholar]
- 49.Costlow M, Lave JR. Dental Coverage for Children Under Pennsylvania Medical Assistance. Pittsburgh, PA: Pennsylvania Medicaid Policy Center; 2010. [Google Scholar]
- 50.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian S. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—the Public Health Disparities Geocoding Project. Am J Public Health. 2003;93(10):1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Census Redistricting Data (Public Law 940171) Summary File: Geographic Terms and Concepts. Washington, DC: US Census Bureau; 2010. [Google Scholar]
- 52.Center for Rural Pennsylvania. Demographics: rural/urban Pennsylvania. Available at: http://www.rural.palegislature.us/demographics_rural_urban.html. Accessed August 21, 2014.
- 53.Morrill R, Cromartie J, Hart G. Metropolitan, urban, and rural commuting areas: toward a better depiction of the United States settlement system. Urban Geogr. 1999;20(8):727–748. [Google Scholar]
- 54. ArcGIS [computer program]. Redlands, CA: ESRI.
- 55.Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005;95(7):1149–1155. doi: 10.2105/AJPH.2004.042432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Stata/SE Version 12 [computer program]. College Station, TX: StataCorp LP.
- 57.Franchi E, Bumgardner C. Importance of Access to and Utilization of Oral Health Care in Pennsylvania. Wormleysburg, PA: Pennsylvania Association of Community Health Centers; 2013. [Google Scholar]
- 58.Oral Health Strategic Plan for Pennsylvania. Harrisburg, PA: Pennsylvania Department of Health; 2002. [Google Scholar]
- 59.Flores G, Tomany-Korman SC. The language spoken at home and disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(6):e1703–e1714. doi: 10.1542/peds.2007-2906. [DOI] [PubMed] [Google Scholar]
- 60.Liu J, Probst JC, Martin AB, Wang J-Y, Salinas CF. Disparities in dental insurance coverage and dental care among US children: the National Survey of Children’s Health. Pediatrics. 2007;119(suppl 1):S12–S21. doi: 10.1542/peds.2006-2089D. [DOI] [PubMed] [Google Scholar]
- 61.Valencia A, Damiano P, Qian F, Warren JJ, Weber-Gasparoni K, Jones M. Racial and ethnic disparities in utilization of dental services among children in Iowa: the Latino experience. Am J Public Health. 2012;102(12):2352–2359. doi: 10.2105/AJPH.2011.300471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Singer A, Vitiello D, Katz M, Park D. Recent Immigration to Philadelphia: Regional Change and Response. Washington, DC: Brookings Institution; 2008. [Google Scholar]
- 63.Patusky C, Ceffalio J. Recent Trends in Immigration to Philadelphia, Pennsylvania: Who Came and Where Do They Live? Philadelphia, PA: Fels Institute of Government, University of Pennsylvania; 2004. [Google Scholar]
- 64.Howell E, Trenholm C, Dubay L, Hughes D, Hill I. The impact of new health insurance coverage on undocumented and other low-income children: lessons from three California counties. J Health Care Poor Underserved. 2010;21(2):109–124. doi: 10.1353/hpu.0.0293. [DOI] [PubMed] [Google Scholar]
- 65.Beil H, Rozier RG, Preisser JS, Stearns SC, Lee JY. Effects of early dental office visits on dental caries experience. Am J Public Health. 2014;104(10):1979–1985. doi: 10.2105/AJPH.2013.301325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dye BA, Li X, Thornton-Evans G. Oral Health Disparities as Determined by Selected Healthy People 2020 Oral Health Objectives for the United States, 2009–2010. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 67.Ramos-Gomez F, Cruz GD, Watson MR, Canto MT, Boneta AE. Latino oral health: a research agenda toward eliminating oral health disparities. J Am Dent Assoc. 2005;136(9):1231–1240. doi: 10.14219/jada.archive.2005.0339. [DOI] [PubMed] [Google Scholar]
- 68.Lee C. “Race” and “ethnicity” in biomedical research: how do scientists construct and explain differences in health? Soc Sci Med. 2009;68(6):1183–1190. doi: 10.1016/j.socscimed.2008.12.036. [DOI] [PubMed] [Google Scholar]
- 69.Kaplan J, Bennett T. Use of race and ethnicity in biomedical publication. JAMA. 2003;289(20):2709–2716. doi: 10.1001/jama.289.20.2709. [DOI] [PubMed] [Google Scholar]
- 70.Yun K, Fuentes-Afflick E, Curry L, Krumholz H, Desai M. Parents’ immigration history is associated with differences in children’s health care utilization: findings from the 2003 New Immigrant Survey. Matern Child Health J. 2013;17(10):1913–1921. doi: 10.1007/s10995-012-1217-2. [DOI] [PMC free article] [PubMed] [Google Scholar]