Abstract
Objectives. We examined preventive care use by nonelderly adults (aged 18–64 years) before the Affordable Care Act (ACA) and considered the contributions of insurance coverage and other factors to service use patterns.
Methods. We used data from the 2005–2010 Medical Expenditure Panel Survey to measure the receipt of 8 recommended preventive services. We examined gaps in receipt of services for adults with incomes below 400% of the federal poverty level compared with higher incomes. We then used a regression-based decomposition analysis to consider factors that explain the gaps in service use by income.
Results. There were large income-related disparities in preventive care receipt for nonelderly adults. Differences in insurance coverage explain 25% to 40% of the disparities in preventive service use by income, but education, age, and health status are also important drivers.
Conclusions. Expanding coverage to lower-income adults through the ACA is expected to increase their preventive care use. However, the importance of education, age, and health status in explaining income-related gaps in service use indicates that the ACA cannot address all barriers to preventive care and additional interventions may be necessary.
The benefits of many preventive health care services are well-established.1 In the case of immunization, for instance, those who receive the recommended services are likely to avoid a variety of life-threatening diseases while promoting herd immunity and protecting individuals who are unable to be immunized.2 Those appropriately screened for cancer are likely to receive more timely diagnosis and treatment, which ultimately leads to better outcomes.3 Furthermore, early detection of heart disease, diabetes, and other chronic conditions can lead to the promotion of healthier lifestyles and better management of the diseases.4 Despite this evidence, many studies have shown the use of preventive services, including cholesterol checks, Papanicolaou (Pap) tests, mammograms, colon cancer screenings, and flu vaccines to be below recommended levels.5–9
In recent years, the growing prevalence of obesity and chronic conditions and the evidence that modifiable behaviors are among the leading causes of death have led to a renewed emphasis on promoting health and wellness as opposed to treating disease.10,11 This emphasis on prevention was particularly evident in the national conversation leading up to the passage of the Affordable Care Act (ACA) in March 2010. Increasing access to preventive care was one motivation for expanding coverage to the uninsured, and was the explicit goal of an additional provision in the ACA requiring private insurers to cover recommended preventive services without any cost-sharing obligations to consumers. The effects of these ACA policies on preventive service use will depend on the extent to which preventive services are currently underused and whether expanding coverage will increase the receipt of these services.
We examined the receipt of 8 preventive services by nonelderly adults in the years before the ACA (2005–2010), thus providing recent evidence on the extent of underuse of a variety of important services. Previous studies have found that lower rates of service use are generally associated with more limited education, low incomes, and a lack of insurance coverage12–14; we concentrated on the disparities in service use between the lower-income adults most likely to benefit from the ACA coverage expansion and their higher-income counterparts. Using a regression-based decomposition analysis, we identified the roles of insurance coverage, education, and other factors in explaining these income-related disparities. The results provide important insights on the potential of ACA efforts to increase the use of preventive care through coverage expansion as well as on the limitations of such efforts.
Our conceptual framework relies on human capital models, which suggest that the demand for medical care is derived from the demand for health.15,16 According to such models, critical factors that are expected to affect the demand for health and medical care include age, health status, education, and rate of time preference. In some cases, the effects of these factors on demand for preventive care may be distinct from their effects on demand for treatment. In the case of age, for example, the demand for treatment, or curative care, is expected to increase with age as an individual’s health depreciates, whereas investment in preventive medical care is expected to decrease with age as the payoff period for avoiding future illness shortens.13,17 This reflects a more general distinction between investment and consumption considerations in the demand for preventive care, which is also relevant with respect to the role of health status. From a consumption perspective, those in poor health are more likely to use preventive services, but healthy individuals and those who are future-oriented are also more likely to invest in health and preventive care.18,19 Lastly, although the effect of education on the demand for health and health care is theoretically ambiguous,15 considerable empirical evidence finds a positive relationship between education and prevention activities.13,20–22
Another critical consideration is the influence of insurance coverage on the demand for medical care. The direct effect of insurance is to lower the out-of-pocket cost of medical care and thus increase the demand for services. The RAND health insurance experiment provides the most rigorous evidence that this is the case,23 but many other studies provide empirical evidence that having health insurance is associated with increased utilization of medical care.24–27 The possibility exists, however, that because insurance coverage protects against the financial costs of adverse health events, it may reduce the incentive to invest in preventive care.17 Despite this potential for “ex ante moral hazard,” most empirical evidence finds that those with insurance coverage use more preventive care, including blood pressure screenings, mammograms, and other cancer screenings.28–30 Furthermore, those with more generous coverage and lower cost-sharing exhibit higher rates of preventive service use.31–33
The ACA includes several components that expand coverage and reduce cost-sharing and thus have the potential to increase the receipt of recommended preventive care. The ACA includes an optional expansion of Medicaid for those with incomes less than 138% of the federal poverty level (FPL) and federal subsidies to purchase coverage in the new health insurance exchanges for those with incomes up to 400% of the FPL. The law also includes penalties for not having health insurance coverage and enhanced enrollment and outreach efforts. When fully implemented, the ACA is expected to significantly expand coverage, particularly among adults with incomes less than 400% of the FPL.34 Many of those becoming newly insured under the ACA are expected to experience improved access to recommended preventive services, given that these services will be included at no or low cost in exchange plans and under most Medicaid plans.
In addition to the broader coverage expansions included in the ACA, the law includes new requirements for private health insurance coverage of a set preventive services rated “A” or “B” by the US Preventive Services Task Force.35 After September 2010, many private health plans were required to cover the specified services, and to do so at no cost to members. Although coverage for some of the ACA-mandated services is already relatively common, other services, such as diet and tobacco counseling, are likely to see expanded coverage under the law.36 Furthermore, with the notable exception of mammograms, few of the mandated services are currently required to be covered by private plans under state laws.37
METHODS
The theoretical and empirical findings outlined in the previous section provide a foundation for considering the potential impact of the ACA on the demand for preventive care. Most importantly, the evidence suggests that mandating or otherwise expanding coverage for preventive care is likely to increase demand for these services. Therefore, we expect that the ACA will increase use of preventive care by increasing rates of Medicaid and private coverage among the currently uninsured and by increasing access to free or low-cost preventive care among those who already have private coverage. This analysis considered the potential for the ACA to affect the use of preventive care by those most likely to gain coverage under the law by examining the contributions of insurance coverage and other factors to their service use patterns before the ACA.
We used data from the 2005–2010 Medical Expenditure Panel Survey (MEPS) to measure the receipt of several preventive services for nonelderly adults (aged 18–64 years). We measured the receipt of a routine checkup and 7 specific services recommended by the US Preventive Services Task Force or the Advisory Committee on Immunization Practices. The US Preventive Services Task Force does not always provide recommendations for screening intervals or at-risk populations, so we used the recommended intervals and populations as included in the Healthy People 2020 goals.5 Table 1 summarizes these services, populations, and screening intervals.
TABLE 1—
Receipt of Preventive Services for Nonelderly Adults (Aged 18–64 Years) by Income: 2005–2010 Medical Expenditure Panel Survey, United States
| Preventive Service | Target Population | Screening Interval | All Incomes, % | < 400% of the FPL,a % | ≥ 400% of the FPL,a % | Percentage Point Difference |
| Routine checkup | Adults aged 18–64 y | Every year | 57.7 | 53.0 | 65.1 | 12.1* |
| Cholesterol check | Adults aged 18–64 y | Every 5 y | 74.5 | 68.0 | 84.8 | 16.8* |
| Blood pressure checkb | Adults aged 18–64 y | Every 2 y | 88.7 | 85.6 | 94.1 | 8.5* |
| Pap test | Women aged 21–64 y | Every 3 y | 86.1 | 83.1 | 91.0 | 7.9* |
| Mammogram | Women aged 50–64 y | Every 2 y | 78.3 | 70.6 | 86.9 | 16.3* |
| Breast examination | Women aged 18–64 y | Every year | 64.3 | 58.7 | 73.7 | 15.0* |
| Flu vaccination | Adults aged 18–64 y | Every year | 28.1 | 24.1 | 34.6 | 10.5* |
| Colon cancer screening | Adults aged 50–64 y | Colonoscopy every 10 y, blood stool test every year, or a flexible sigmoidoscopy every 5 y and a blood stool test every 3 y | 49.9 | 42.6 | 57.4 | 14.8* |
Note. FPL = federal poverty level; Pap = Papanicolaou. Target populations and screening intervals are consistent with Healthy People 2020 guidelines. The American Cancer Society’s (ACS’s) screening recommendations vary from the Healthy People 2020 guidelines used in this article in some nontrivial ways. The ACS recommends yearly mammograms, beginning at age 40 years, whereas the Healthy People goal is for women aged ≥ 50 years to receive the screening every 2 years. The Healthy People recommendation for breast examinations is once a year, starting at age 18 years, whereas the ACS recommends a breast examination every 3 years for women aged 20–39 years and every year for women aged ≥ 40. The guidelines for colorectal cancer screenings are identical between the 2 organizations, although the ACS includes double-contrast barium enema every 5 years, virtual colonoscopy every 5 years, or fecal immunochemical test every year in its list of effective screening options. The recommendations for cervical cancer are the same in both sets of guidelines.
FPL was determined by using the Department of Health and Human Services poverty thresholds.
Blood pressure check is only available for 2008–2010.
*P ≤ .05 for difference between < 400% FPL and ≥ 400% FPL.
We classified each individual into 1 of 7 mutually exclusive coverage categories:
full-year employer-sponsored insurance,
full-year Medicare,
full-year Medicaid or other public insurance,
full-year nongroup insurance,
full-year insured by multiple coverage types,
part-year uninsured, and
full-year uninsured.
Income relative to the FPL is calculated for the health insurance unit by using information on individual and family earnings and income and the Department of Health and Human Services poverty thresholds. Health insurance units are created to more closely align with family definitions commonly used by public and private insurers.
We describe the receipt of each preventive service by the nonelderly adult population before the ACA. Because those below 400% of the FPL are targeted by the ACA Medicaid expansion and exchange subsidies, we examined the gaps in receipt of preventive care for this population compared with those with higher incomes. We then used a regression-based decomposition analysis popularized by Blinder38 and Oaxaca39 to consider the factors that explain the gaps by income. This approach has also been used to understand differences in health insurance coverage over time and racial differences in access and use.40,41 It is particularly useful in this analysis because it allows us to isolate the role of insurance coverage in explaining income-related disparities in service use. This is highly relevant in the context of the ACA coverage expansions targeted at specific income groups. The results of the analysis provide the proportion of the difference in service use by income that can be explained by differences in the coverage distribution. This allows for straightforward comparisons across services on the effects of insurance coverage.
The decomposition relies on the property of linear regression whereby the mean of the outcome variable (Y) is equal to the sum of the mean values of the independent variables (X) times their associated estimated coefficients (b), or  . Thus, the difference in preventive service receipt between higher- and lower-income individuals is
. Thus, the difference in preventive service receipt between higher- and lower-income individuals is
 |
By adding and subtracting  and rearranging the terms, we find
and rearranging the terms, we find
 |
The first term on the right-hand side represents the portion of the difference in preventive service use between lower- and higher-income individuals that can be explained by differences in their observable characteristics. Specifically, it reflects the expected change in service use for the lower-income population if they had the characteristics of the higher-income population. The second term on the right-hand side represents the portion of the difference that cannot be explained by differences in observed characteristics. This may reflect differences attributable to varying effects of the observable characteristics or caused by unobservable characteristics.
To implement the decomposition, we estimated separate linear probability models on each binary measure of preventive service use for lower-income and higher-income adults and calculated the component of the difference attributable to observable characteristics and that caused by other factors. These models produce the consistent parameter estimates necessary for the decomposition approach despite concerns about using linear models with binary outcomes.42 We built on the theoretical framework and included age, gender, race, citizenship, and marital status in our models. We also included individual education and employment status, as well as indicators for the largest firm size represented in the household. Firm size is correlated with more generous private insurance coverage and large, self-insured firms are more likely to provide preventive services such as flu vaccinations directly.17 We included indicators for 6 mutually exclusive coverage categories as well as measures of self-reported general and mental health status.
We controlled for preferences for risk and attitudes toward medical care by including whether an individual always or nearly always wears a seatbelt and indicators for those who reported that they were more likely to take risks than the average person and that they can overcome illness without medical help. We also included controls for census region and year dummies to capture secular trends in preventive service use over time. All estimates accounted for the complex survey design of the MEPS in calculating standard errors.
RESULTS
The rate of preventive care receipt varied considerably by type of service and income (Table 1). According to estimates from the period 2005 to 2010, more than 85% of adults were in compliance with blood pressure screening and Pap test recommendations, whereas only 28% of adults received a flu vaccine and just under 50% of the target population (aged 50–64 years) received recommended colon cancer screenings. In addition, adults with higher incomes were more likely than their lower-income counterparts to receive every preventive service examined here. Higher-income women were 7.9 percentage points more likely to have received a Pap test in the past 3 years and were 16.3 percentage points more likely to have received a mammogram. Older adults (aged 50–64 years) with high incomes were almost 15 percentage points more likely to be screened for colon cancer and rates of blood pressure and cholesterol screening were 8.5 and 16.8 percentage points higher, respectively, for those with high incomes.
The lower- and the higher-income populations varied greatly on most of the observed characteristics that were likely to influence preventive care receipt (Table 2). In particular, those with higher incomes were much more likely to be covered by employer-sponsored insurance and much less likely to be uninsured. Higher-income adults were also older, less likely to be Black or Hispanic, and more likely to be citizens. Adults with higher incomes were also much more likely to have finished college and to be working full-time. Finally, higher-income adults were generally healthier and less likely to take risks or to believe that they can overcome illness without medical care than their lower-income counterparts. These patterns by income held true for adults and women aged 18 to 64 years. Although the composition of the target populations for colon cancer screening (older adults aged 50–64 years) and mammograms (older women aged 50–64 years) differs from that of adults as a whole, the patterns across the higher- and lower-income groups were relatively consistent (Table A, available as a supplement to this article at http://www.ajph.org).
TABLE 2—
Characteristics of All Adults and Women (Aged 18–64 Years), by Income: 2005–2010 Medical Expenditure Panel Survey, United States
| Adults Aged 18–64 Years, % |
Women Aged 18–64 Years, % |
|||||
| Variable | < 400% FPLa | ≥ 400% FPLa | Percentage Point Difference | < 400% FPLa | ≥ 400% FPLa | Percentage Point Difference |
| Coverage | ||||||
| ESI, full-year | 41.5 | 82.8 | 41.3* | 42.4 | 84.1 | 41.8* |
| Nongroup, full-year | 3.7 | 3.9 | 0.2 | 3.8 | 3.9 | 0.1 |
| Medicaid or other public, full-year | 8.1 | 1.4 | –6.7* | 10.6 | 1.5 | –9.2* |
| Medicare, full-year | 3.7 | 0.2 | –3.5* | 3.7 | 0.2 | –3.4* |
| Part-year coverage, full-year insured | 1.2 | 0.8 | –0.4* | 1.4 | 0.7 | –0.6* |
| Part-year uninsured, part-year insured | 15.5 | 5.8 | –9.7* | 16.3 | 5.3 | –11.1* |
| Uninsured, full-year | 26.3 | 5.2 | –21.1* | 21.8 | 4.3 | –17.5* |
| Age, y | ||||||
| 19–29 | 31.3 | 14.2 | –17.1* | 30.0 | 14.3 | –15.8* |
| 30–39 | 21.9 | 20.5 | –1.4* | 22.0 | 20.1 | –1.9* |
| 40–49 | 21.5 | 26.3 | 4.8* | 21.8 | 26.8 | 5.0* |
| 50–64 | 25.2 | 39.0 | 13.8* | 26.2 | 38.8 | 12.7* |
| Gender | ||||||
| Male | 48.6 | 50.9 | 2.3* | |||
| Female | 51.4 | 49.1 | –2.3* | 100.0 | 100.0 | 0.0 |
| Race/ethnicity | ||||||
| White, non-Hispanic | 58.6 | 78.8 | 20.2* | 58.6 | 78.8 | 20.2* |
| Hispanic | 19.8 | 6.8 | –13.0* | 18.4 | 6.4 | –11.9* |
| Black, non-Hispanic | 14.9 | 7.1 | –7.7* | 16.1 | 7.2 | –8.9* |
| Other race, non-Hispanic | 6.7 | 7.3 | 0.6 | 6.9 | 7.6 | 0.6 |
| Citizenship status | ||||||
| Citizen | 87.9 | 95.4 | 7.4* | 88.9 | 95.7 | 6.8* |
| Noncitizen | 12.1 | 4.6 | –7.4* | 11.1 | 4.3 | –6.8* |
| Education status | ||||||
| < high school | 19.5 | 3.3 | –16.2* | 17.3 | 2.8 | –14.5* |
| High-school graduate | 38.4 | 22.2 | –16.2* | 37.7 | 20.0 | –17.7* |
| Some college | 26.1 | 25.3 | −0.9 | 27.9 | 25.8 | –2.1* |
| ≥ college degree | 15.9 | 49.2 | 33.3* | 17.1 | 51.4 | 34.2* |
| Employment status | ||||||
| Employed, full-time | 50.3 | 74.3 | 24.0* | 41.6 | 63.9 | 22.3* |
| Employed, part-time | 16.4 | 12.3 | –4.1* | 20.1 | 17.8 | –2.3* |
| Not employed | 33.3 | 13.5 | –19.9* | 38.3 | 18.3 | –19.9* |
| No worker in HIU | 19.1 | 2.1 | –17.0* | 19.7 | 2.4 | –17.4* |
| < 100 employees at main job in HIU | 51.2 | 42.9 | –8.3* | 49.5 | 41.5 | –8.0* |
| 100–499 employees at main job in HIU | 17.1 | 25.5 | 8.4* | 17.6 | 25.7 | 8.1* |
| ≥ 500 employees at main job in HIU | 12.6 | 29.5 | 16.9* | 13.1 | 30.4 | 17.3* |
| Family status | ||||||
| Married | 46.0 | 70.7 | 24.6* | 46.0 | 73.4 | 27.4* |
| Widowed, separated, or divorced | 18.5 | 11.5 | –7.0* | 22.6 | 11.3 | –11.4* |
| Never married | 35.5 | 17.8 | –17.6* | 31.4 | 15.4 | –16.0* |
| No children in HIU | 55.5 | 58.6 | 3.2* | 47.9 | 57.0 | 9.1* |
| Any child in HIU | 44.5 | 41.4 | –3.2* | 52.1 | 43.0 | –9.1* |
| General health status | ||||||
| Excellent or very good | 55.8 | 70.6 | 14.8* | 53.8 | 70.8 | 17.1* |
| Good | 29.5 | 23.7 | –5.8* | 30.7 | 23.1 | –7.6* |
| Fair or poor | 14.8 | 5.8 | –9.0* | 15.6 | 6.1 | –9.5* |
| Mental health status | ||||||
| Excellent or very good | 64.2 | 78.0 | 13.9* | 62.9 | 77.7 | 14.8* |
| Good | 26.9 | 18.8 | –8.1* | 27.6 | 19.0 | –8.6* |
| Fair or poor | 9.0 | 3.1 | –5.8* | 9.5 | 3.4 | –6.1* |
| Preferences for risk and medical care | ||||||
| More likely to take risks than average | 24.9 | 21.6 | –3.3* | 18.5 | 13.5 | –5.0* |
| Can overcome illness without medical help | 25.8 | 24.3 | –1.5* | 22.1 | 20.0 | –2.1* |
| Wears seatbelt nearly always or always | 91.3 | 95.1 | 3.8* | 93.9 | 97.6 | 3.7* |
Note. ESI = employer-sponsored insurance; FPL = federal poverty level; HIU = health insurance unit.
FPL was determined by using the US Department of Health and Human Services poverty thresholds.
*P ≤ .05 for difference between < 400% FPL and ≥ 400% FPL.
For lower-income individuals, our models indicate that many of the characteristics described previously are strongly associated with the use of preventive care and consistent with theoretical predictions (Table B, available as a supplement to this article at http://www.ajph.org). Having insurance coverage for all or some of the year and higher educational attainment were strongly associated with higher rates of use for every preventive service we examined. Age was positively associated with routine checkups, blood pressure and cholesterol checks, and flu vaccinations, but was negatively associated with Pap tests and breast examinations. Better general health status was associated with lower receipt of routine checkups, blood pressure and cholesterol checks, flu vaccinations, and colon cancer screenings, whereas better mental health status was associated with greater receipt of several services. Those reporting frequent seatbelt use were more likely to use each preventive service we examined, whereas those more likely to take risks and those who reported an ability to overcome illness without medical care were less likely to receive preventive care, other things equal. Similar associations between observed characteristics and preventive care receipt were evident for higher-income adults (Table C, available as a supplement to this article at http://www.ajph.org).
The results of the Blinder–Oaxaca decomposition indicated that, for all measures of preventive care examined here, differences in the observed characteristics discussed previously explained a large proportion of the difference in preventive care receipt across income groups, ranging from 46% for Pap tests to 78% for flu vaccines (Table 3). Furthermore, the characteristics that explain the differences were generally consistent with the theoretical predictions. The difference in the insurance coverage distribution by income was a strong contributor to the difference in preventive care receipt. The role of coverage did vary somewhat across measures, however. Differences in the coverage distribution explained only 24% of the variation in cholesterol checks by income, whereas more than 40% of the income gap was explained by coverage in the case of routine checkups and blood pressure checks.
TABLE 3—
Blinder-Oaxaca Decomposition of Differences in Preventive Service Use by Income: 2005–2010 Medical Expenditure Panel Survey, United States
| Variable | Routine Checkup in Past Year | Cholesterol Checked in Past 5 Years | Blood Pressure Checked in Past 2 Years | Flu Vaccination in Past Year | Pap Test in Past 3 Years | Mammogram in Past 2 Years | Breast Examination in Past Year | Recommended Colon Cancer Screening |
| Difference between adults ≥ 400% and < 400% of the FPLa | 0.120 | 0.169 | 0.083 | 0.104 | 0.079 | 0.158 | 0.150 | 0.143 |
| Percentage explained | ||||||||
| Difference not attributable to observable characteristics, % | 34 | 30 | 25 | 22 | 54 | 40 | 36 | 49 |
| Difference attributable to observable characteristics, % | 66 | 70 | 75 | 78 | 46 | 60 | 64 | 51 |
| Differences attributable to, % | ||||||||
| Coverageb | 46 | 24 | 45 | 31 | 35 | 40 | 34 | 29 |
| Age | 23 | 35 | 9 | 22 | –23 | –5 | ||
| Age ≥ 50 y | –1 | –3 | ||||||
| Other demographicsc | –7 | –6 | 7 | 9 | –18 | –1 | –1 | 11 |
| Educationd | 15 | 22 | 22 | 22 | 30 | 14 | 26 | 30 |
| Firm size and employment statuse | –8 | –1 | –2 | 1 | 10 | –1 | 3 | –10 |
| Self-reported health statusf | –7 | –5 | –9 | –7 | 6 | 4 | 3 | –7 |
| Preferences or risk behaviorsg | 3 | 2 | 2 | 3 | 3 | 3 | 3 | 1 |
| Region and year | 2 | 0 | 1 | –2 | 2 | 2 | 2 | 1 |
Note. FPL = federal poverty level. Blood pressure check is only available for 2008–2010.
FPL was determined by using the US Department of Health and Human Services poverty thresholds.
Coverage reflects indicators for 6 mutually exclusive coverage categories.
Other demographics included race/ethnicity, gender, citizenship, marital status, and family status.
The individual’s highest level of education.
Employment status reflects individual full-time or part-time employment, the largest firm size represented in the household, and an indicator for no worker in the household.
Self-reported general and mental health status.
Preferences and risk behaviors included indicators for (nearly) always wearing a seatbelt, taking more risks than the average person, and ability to overcome illness without medical care.
Differences in age and health status played significant roles in explaining the differences in screening by income. However, the proportion of the variation explained and the direction of the effect varied by service confirming the investment versus consumption considerations in the demand for preventive services as predicted by human capital models. The educational achievement of the lower-income population was a major contributor to their lower rates of service use, explaining between 14% of the gap in service use by income for mammograms and 30% for colon cancer screening. Attitudes toward risk and medical care of the lower-income population also contributed to their lower screening rates. The lower-income population was more likely to take risks and less likely to wear seatbelts and, although the proportion of the variation explained by these factors was relatively small, about 2% to 3% across all measures, the direction was consistent with theoretical predictions.
Figure 1 shows the actual receipt of each preventive service for higher- and lower-income adults. For lower-income adults, the figure also shows the expected increase in preventive care receipt if they had the coverage distribution of higher-income adults. On every measure, the results indicate that if the lower-income population had the coverage characteristics of the higher-income population, their use of preventive services would be significantly higher. However, the effect of changing the coverage distribution alone is not enough for rates of service use to reach those achieved by higher-income individuals. For example, receipt of mammograms among the lower-income population would be expected to increase by 6 percentage points if their insurance coverage distribution resembled the higher-income population, but this would still leave lower-income women 10 percentage points below the rate for those with higher incomes.
FIGURE 1—
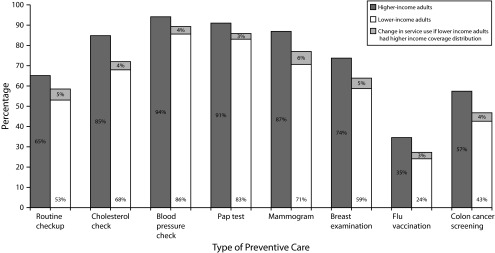
Receipt of recommended preventive care by nonelderly adults (aged 18–64 years): 2005–2010 Medical Expenditure Panel Survey, United States.
Note. Pap = Papanicolaou. Lower (higher) income adults have incomes below (at or above) 400% of the FPL. Blood pressure check is only available for 2008–2010. Recommended colon cancer screening consists of a colonoscopy in the past 10 years, or a blood stool test in the past year, or a flexible sigmoidoscopy in the past 5 years and a blood stool test in the past 3 years.
DISCUSSION
Increasing the use of recommended preventive services is a major public health priority. The Healthy People 2020 objectives seek increases in the receipt of screening services for cancer and chronic disease, as well as improved compliance with vaccine recommendations. By expanding health insurance coverage and reducing cost sharing for preventive care, the ACA addresses one potential barrier to preventive care receipt. The extent to which these ACA provisions will help to achieve the targets set in Healthy People 2020 depends on the underlying drivers of preventive service use.
We considered the role of insurance coverage and other factors in explaining differences in receipt of preventive care by income. Adults with incomes below 400% of the FPL, the group where we expect coverage gains to be concentrated under the ACA, were found to use preventive services at much lower rates than those with higher incomes. In general, our decomposition results suggest that insurance coverage does play a significant role in explaining the receipt of preventive services and that if those with incomes below 400% of the FPL had an insurance coverage distribution similar to that of the higher-income population, their rates of preventive service use would increase. These results are consistent with earlier studies that have found insurance coverage to be significantly associated with use of preventive services. However, our results provide more recent evidence and isolate the role of insurance coverage in explaining gaps for the population targeted by the ACA coverage expansions.
Moreover, although coverage explained a significant proportion of variation across income groups for the preventive services examined, our analysis found that differences in other observable characteristics also contributed. For example, differences in educational attainment contributed to disparities in preventive service use across income groups and the observed tendencies among the lower-income population to take more risks and be less receptive to medical care contributed to their lower rates of preventive service use.
This analysis had several limitations. First, we focused on the role of insurance coverage in preventive care receipt, but we were limited by the available survey information on both measures. We present information on coverage for a 12-month period and used that to explore differences in compliance with recommendations over multiple years, despite the fact that individuals could have experienced a change in their insurance status throughout the screening intervals we examined. Second, self-reported receipt of preventive care is likely to contain measurement error as individuals may not recall the timing of their recent screenings or may feel some pressure to indicate that they received the recommended care.43 Third, in this analysis, we were unable to assess the causal effect of insurance coverage on preventive care receipt because there were likely to be unmeasured factors that affect both receipt of care and the decision to be covered or not. Although we attempted to attenuate the potential bias by including several proxies for individuals’ tastes and preferences for risk and medical care, other unobservables may continue to bias the results. On balance, we expected this bias to result in an overestimate of the effects of coverage on use of preventive care.
Overall, this analysis suggests that coverage is an important driver of preventive service use and that the ACA is likely to increase receipt of such services for those gaining new coverage or expanded benefits. This, in turn, should narrow the existing income gaps in receipt of preventive care. However, other factors that contribute to preventive service use, including education and preferences for risk, are not expected to change as a result of the ACA. Therefore, some important barriers to receipt of recommended services will still exist and preventive service use may remain below recommended levels.
Additional interventions may therefore prove useful to address barriers that are not related to coverage or cost-sharing. Primary care rate increases and funding to community health centers included in the ACA are intended to improve access for the Medicaid population, but additional efforts may be necessary.44 Moreover, even when individuals see a provider, they do not necessarily get all recommended care.45 Therefore, incentives for providers to adhere to screening guidelines, including pay-for-performance or other quality reporting programs, may also be important in eliminating remaining gaps in preventive care. Greater adherence to the screening recommendations could also help to ensure that preventive care does not contribute to rising health costs associated with overuse of care.46 Finally, information campaigns to educate individuals about the importance of particular services and how to obtain them are likely to be necessary.
Preventive care is critical to maintaining and improving the health and well-being of all Americans. Our results suggest that the ACA will help increase the receipt of preventive services by making those services more affordable. But achieving the vision of a nation focused on prevention and wellness rather than sickness and disease will require more fundamental efforts to educate the population and change their attitudes about health and health care.
Acknowledgments
This study was funded by the Robert Wood Johnson Foundation.
The authors appreciate the helpful advice and suggestions of Sharon Long, Samuel Kleiner, and 4 anonymous reviewers.
Human Participant Protection
No protocol approval was necessary because the study used anonymous data from a publicly available source.
References
- 1.Maciosek MV, Coffield AB, Flottemesch TJ, Edwards NM, Solberg LI. Greater use of preventive services in US health care could save lives at little or no cost. Health Aff (Millwood) 2010;29(9):1656–1660. doi: 10.1377/hlthaff.2008.0701. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. How vaccines prevent disease. 2009. Available at: http://www.cdc.gov/vaccines/vac-gen/howvpd.htm. Accessed December 21, 2012.
- 3.Curry SJ, Byers T, Hewitt M. Fulfilling the Potential of Cancer Prevention and Early Detection. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion. The power of prevention: chronic disease… the public health challenge of the 21st century. 2009. Available at: http://www.cdc.gov/chronicdisease/pdf/2009-Power-of-Prevention.pdf. Accessed December 21, 2012.
- 5.US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/default.aspx. Accessed December 21, 2012 [PubMed]
- 6.Maciosek MV, Coffield AB, Edwards NM, Flottemesch TJ, Goodman MJ, Solberg LI. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med. 2006;31(1):52–61. doi: 10.1016/j.amepre.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 7.Nelson DE, Bland S, Powell-Griner E et al. State trends in health risk factors and receipt of clinical preventive services among US adults during the 1990s. JAMA. 2002;287(20):2659–2667. doi: 10.1001/jama.287.20.2659. [DOI] [PubMed] [Google Scholar]
- 8.Lurie N, Manning WG, Peterson C, Goldberg GA, Phelps CA, Lillard L. Preventive care: do we practice what we preach? Am J Public Health. 1987;77(7):801–804. doi: 10.2105/ajph.77.7.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer, 2005. CA Cancer J Clin. 2005;55(1):31–44. doi: 10.3322/canjclin.55.1.31. [DOI] [PubMed] [Google Scholar]
- 10.Mokdad AH, Marks JS, Stroup DF, Gerbeding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 11.National Prevention Council. National Prevention Strategy. Washington, DC: US Department of Health and Human Services, Office of the Surgeon General; 2011. [Google Scholar]
- 12.Sambamoorthi U, McAlpine DD. Racial, ethnic, socioeconomic and access disparities in the use of preventive services among women. Prev Med. 2003;37(5):475–484. doi: 10.1016/s0091-7435(03)00172-5. [DOI] [PubMed] [Google Scholar]
- 13.Kenkel DS. The demand for preventive medical care. Appl Econ. 1994;26:313–325. [Google Scholar]
- 14.Sudano JJ, Baker DW. Intermittent lack of health insurance coverage and use of preventive services. Am J Public Health. 2003;93(1):130–137. doi: 10.2105/ajph.93.1.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grossman M. On the concept of health capital and the demand for health. J Polit Econ. 1972;80:223–255. [Google Scholar]
- 16.Cropper ML. Health, investment in health and occupational choice. J Polit Econ. 1977;85:1273–1294. [Google Scholar]
- 17.Kenkel DS. Prevention. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. Vol 1. Amsterdam, The Netherlands: Elsevier Science; 2000. [Google Scholar]
- 18.Ehrlich I, Chuma H. A model of the demand for longevity and the value of life extension. J Polit Econ. 1990;98(4):761–782. doi: 10.1086/261705. [DOI] [PubMed] [Google Scholar]
- 19.Carrieri V, Bilger M. Preventive care: underused even when free. Is there something else at work? Appl Econ. 2013;45:239–253. [Google Scholar]
- 20.Kenkel DS. Health behavior, health knowledge and schooling. J Polit Econ. 1991;99:287–305. [Google Scholar]
- 21.Kenkel DS. What you don’t know really won’t hurt you. J Policy Anal Manage. 1991;10:304–309. [Google Scholar]
- 22.Mullahy J. It’ll only hurt a second? Microeconomic determinants of who gets flu shots. Health Econ. 1999;8(1):9–24. doi: 10.1002/(sici)1099-1050(199902)8:1<9::aid-hec396>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 23.Newhouse J Insurance Experiment Group. Free for All? Lessons From the RAND Health Insurance Experiment. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- 24.Institute of Medicine. America’s Uninsured Crisis: Consequences for Health and Health Care. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 25.Howell EM, Kenney G. The Impact of Medicaid/CHIP expansions on children. Med Care Res Rev. 2012;69(4):372–396. doi: 10.1177/1077558712437245. [DOI] [PubMed] [Google Scholar]
- 26.McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87(2):443–494. doi: 10.1111/j.1468-0009.2009.00564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Finkelstein A, Taubman S, Wright B . 2011. The Oregon health insurance experiment: evidence from the first year. National Bureau of Economic Research. Working Paper No. 17190. Available at: http://www.nber.org/papers/w17190.pdf. Accessed December 21, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernstein J, Chollet D, Peterson GG. Encouraging Appropriate Use of Preventive Health Services. Princeton, NJ: Mathematica Policy Research Inc; 2010. [Google Scholar]
- 29.DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003;93(5):786–791. doi: 10.2105/ajph.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Malley AS, Forrest CB, Mandleblatt J. Adherence of low-income women to cancer screening recommendations: the roles of primary care, health insurance and HMOs. J Gen Intern Med. 2002;17(2):144–154. doi: 10.1046/j.1525-1497.2002.10431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bitler MP, Carpenter CS. Cambridge, MA: National Bureau of Economic Research; 2011. Insurance mandates and mammography. NBER Working Paper No. 16669. [Google Scholar]
- 32.Solanki G, Schauffler HH, Miller LS. The direct and indirect effects of cost-sharing on the use of preventive services. Health Serv Res. 2000;34(6):1331–1350. [PMC free article] [PubMed] [Google Scholar]
- 33.Meeker D, Joyce GF, Malkin J, Teutsch SM, Haddix AC, Goldman DP. Coverage and preventive screening. Health Serv Res. 2011;46(1 pt 1):173–184. doi: 10.1111/j.1475-6773.2010.01188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Buettgens M, Garrett AB, Holahan J. America Under the Affordable Care Act. Washington, DC: Urban Institute; 2010. [Google Scholar]
- 35.US Preventive Services Task Force. USPTF A and B recommendations. 2010. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsabrecs.htm. Accessed December 21, 2012.
- 36.Salinksy E. Clinical preventive services: when is the juice worth the squeeze? National Health Policy Forum Issue Brief No. 806; August 24, 2005. [PubMed] [Google Scholar]
- 37.Bunce VC, Wieske JP. Health Insurance Mandates in the States. Alexandria, VA: Council for Affordable Health Insurance; 2010. [Google Scholar]
- 38.Blinder AS. Wage discrimination: reduced form and structural estimates. J Hum Resour. 1973;8:436–455. [Google Scholar]
- 39.Oaxaca R. Male–female wage differentials in urban labor markets. Int Econ Rev. 1973;14:693–709. [Google Scholar]
- 40.Shen YC, Long S. What’s driving the downward trend in employer-sponsored health insurance? Health Serv Res. 2006;41(6):2074–2096. doi: 10.1111/j.1475-6773.2006.00590.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Serv Res. 2003;38(3):809–829. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Acs G. Explaining trends in health insurance coverage between 1988 and 1991. Inquiry. 1995;32(1):102–110. [PubMed] [Google Scholar]
- 43.Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev. 2006;63(2):217–235. doi: 10.1177/1077558705285298. [DOI] [PubMed] [Google Scholar]
- 44.Decker SL. Changes in Medicaid physician fees and patterns of ambulatory care. Inquiry. 2009;46(3):291–304. doi: 10.5034/inquiryjrnl_46.03.291. [DOI] [PubMed] [Google Scholar]
- 45.McGlynn EA, Asch SM, Adams J et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 46.Merenstein D, Daumit GL, Powe NR. Use and costs of nonrecommended tests during routine preventive health exams. Am J Prev Med. 2006;30(6):521–527. doi: 10.1016/j.amepre.2006.02.003. [DOI] [PubMed] [Google Scholar]


