Abstract
Objectives. We estimated sodium intake, which is associated with elevated blood pressure, a major risk factor for cardiovascular disease, and assessed its association with related variables among New York City adults.
Methods. In 2010 we conducted a cross-sectional, population-based survey of 1656 adults, the Heart Follow-Up Study, that collected self-reported health information, measured blood pressure, and obtained sodium, potassium, and creatinine values from 24-hour urine collections.
Results. Mean daily sodium intake was 3239 milligrams per day; 81% of participants exceeded their recommended limit. Sodium intake was higher in non-Hispanic Blacks (3477 mg/d) and Hispanics (3395 mg/d) than in non-Hispanic Whites (3066 mg/d; both P < .05). Higher sodium intake was associated with higher blood pressure in adjusted models, and this association varied by race/ethnicity.
Conclusions. Higher sodium intake among non-Hispanic Blacks and Hispanics than among Whites was not previously documented in population surveys relying on self-report. These results demonstrate the feasibility of 24-hour urine collection for the purposes of research, surveillance, and program evaluation.
Cardiovascular disease (CVD) is the leading cause of death in the United States,1 and hypertension is a leading risk factor. A positive and continuous relationship between sodium intake and blood pressure (BP) is well established.2 Existing estimates of sodium intake measured by self-report show that US adults consume a daily average of 3400 milligrams, well above the recommended limit (1500–2300 mg/d),2 and public health efforts are aimed at reducing sodium consumption.3–5 In a simulation analysis of risk factor and outcome data from key CVD data sources, researchers estimated that up to 92 000 deaths could be averted annually by lowering the current mean adult intake by 1200 milligrams of sodium, resulting in intake closer to the recommended limit.6 Although reduced sodium intake decreases BP on average in all racial/ethnic groups and in individuals with normal and high BP, the BP-lowering effect of sodium reduction is greater in Blacks than in other racial/ethnic groups.7,8 National estimates of sodium intake derived from self-report do not demonstrate higher intake among Blacks.
The gold standard method for assessing sodium intake is measurement of sodium excretion in rigorously collected 24-hour urine samples, although this method has some limitations, such as undercollection.9 This method has been used to assess population intake in the United Kingdom, Finland, Portugal, and Barbados.10–14 In the United States, population intake has been assessed since 1971 through 24-hour dietary recall. Although adequate for understanding general trends and intake, estimates that rely on self-report are subject to reporting error and bias.9 Objective measures would avoid these problems; however, to date no representative assessment of sodium intake derived from 24-hour urine collections has been performed in the United States.
In the absence of nationally representative US surveys employing the gold standard method, we measured sodium excretion in urine over 24 hours in a representative sample of adults in New York City. Our objectives were to estimate mean population sodium intake, overall and by subgroup, particularly in different racial/ethnic groups; to understand sodium intake in relation to recommended limits; and to assess the relationship between sodium intake and other variables.
METHODS
We conducted the cross-sectional Heart Follow-Up Study in 2010 to assess sodium intake in a population-based representative sample of noninstitutionalized New York City adults (aged ≥ 18 years). Detailed study information is available elsewhere.15 We recruited study participants from the Community Health Survey (CHS), an annual telephone survey conducted by the city Health Department that recruits 8000 to 10 000 New Yorkers.16 To obtain a representative sample of noninstitutionalized adults, the CHS uses a dual-frame sample design consisting of random-digit-dial landline telephone exchanges and a second frame of cellular telephone exchanges that cover the city. The CHS also incorporates a disproportionate stratified random sample design to allow for analysis at the city, borough, and neighborhood levels. The CHS data track patterns in behavioral risk factors, such as diet and physical activity.
Sample
To ensure a representative sample to support population-level estimates, we approached a random selection of CHS participants (n = 6799) to participate in the Heart Follow-Up Study. We excluded participants who were pregnant, breastfeeding, lactating, or on current or past dialysis. Those who agreed to participate were slightly more likely than those who declined to be Hispanic and younger than 65 years; they also reported a slightly lower average income.15 Recruited participants answered additional survey questions related to CVD and nutrition. We then sent a urine collection kit with written instructions to their homes, and participants collected their urine for 24 hours.
Medical technicians visited the participants’ homes to pick up urine samples, measure anthropometry (height and weight), and take 3 seated BP measurements (according to the National Health and Nutrition Examination Survey protocol).17 The technicians used validated, clinic-grade BP monitors and standardized arm and body positions to measure BP.18 Participants were instructed not to consume caffeine or to exercise 30 minutes prior to the visit, and they rested for 5 minutes prior to measurement. During this home visit, if technicians determined that samples were undercollected (24-hour urine volume < 500 ml), or collected incorrectly (included the first urine void of the day), they asked participants to redo their collection; those who refused still received the $100 study incentive, but we excluded their samples from analysis. Technicians at a collaborating laboratory reviewed the volume and sodium level of the samples for potentially incongruous values.
Of the 6799 CHS participants in 2010 who were screened for Heart Follow-Up Study participation, we identified 5830 eligible adults (Figure A, available as a supplement to the online version of this article at http://www.ajph.org), of whom 2333 agreed to provide a 24-hour urine sample; 1775 provided a sample that could be analyzed by the laboratory. To account for the possibility that a participant did not collect all urine voided during the collection period (an incomplete collection), we defined incomplete samples by biological implausibility criteria (total volume < 500 ml; creatinine < 6.05 mmol [688 mg] for men or < 3.78 mmol [430 mg] for women; Paul Elliott and Ian Brown, INTERMAP Study, personal communication, June 17, 2011) or by participant report of missing a collection (more detail is shown in Appendix A, available as a supplement to the online version of this article at http://www.ajph.org). Our final sample, after exclusion of incomplete collections (n = 116), comprised 1656 participants.
Covariates
The collaborating laboratory analyzed urine for sodium, potassium, albumin, and creatinine. Technicians determined sodium and potassium content by the ion-selective electrode potentiometric method on the Roche DPP modular analyzer. They measured creatinine by the Jaffe kinetic colorimetric method on the same analyzer. Participants self-reported demographics (age, gender, race/ethnicity, poverty, country of birth) and other characteristics (self-assessment of overall diet, smoking status, personal history of CVD, level of physical activity, alcohol use). We assessed poverty status as annual combined household income, grouped according to the 2010 federal poverty guidelines determined by the US Department of Health and Human Services.19 We determined nativity (US- vs non–US-born) by asking participants about their state and country of birth. Because sodium intake is related to diet, which in turn is heavily influenced by culture, we categorized participants who reported being born in Puerto Rico or other US territories as non–US-born.
We defined personal history of CVD as self-report of hypertension, congestive heart failure, coronary heart disease, angina pectoris, myocardial infarction, or transient ischemic attack. To assess physical inactivity, we used the validated question, “During the past 30 days, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?” We categorized anyone responding with no as physically inactive. We defined heavy drinking for men as more than 2 drinks per day and for women as more than 1 drink per day. We assessed overall quality of diet from the survey question, “In general, how healthy is your overall diet? Would you say excellent, very good, good, fair or poor?” This is a previously validated question that has been included on National Health and Nutrition Examination Surveys from 2005 to 2012.
The Dietary Guidelines for Americans recommends sodium intake of less than 2300 milligrams per day for those who are not at high risk. High-risk adults (aged ≥ 51 years, Black race/ethnicity, diagnosed with hypertension, diabetes, or chronic kidney disease) are recommended to limit sodium to less than 1500 milligrams per day.2 We defined hypertension by the average of our 3 BP measurements (systolic ≥ 140 mm Hg; diastolic ≥ 90 mm Hg) or self-reported antihypertensive medication use. We defined diabetes as a positive response to the question, “Have you ever been told by a doctor, nurse, or other health professional that you have diabetes?” We defined chronic kidney disease as having a 24-hour albumin excretion of more than 30 milligrams per day.
Statistical Methods
We performed all analyses with weights calculated for the Heart Follow-Up Study to account for survey design and nonresponse; all results were representative of the New York City noninstitutionalized adult population. Prior to analysis, we normalized laboratory values to a 24-hour period according to participants’ reported duration of collection. For example, if the duration of collection was 25 hours, we multiplied the sodium value by 24/25. We reported demographics of the city population, sample size, and weighted sample size resulting from application of survey weights. We calculated mean, median, and select percentiles for sodium, potassium, and the sodium-to-potassium ratio. We used the t test to assess statistical differences in mean sodium intake stratified by demographics, overall and by gender. We constructed a multivariable linear regression model with sodium as the dependent variable to assess factors associated with sodium intake after adjustment. The factors we considered were age, race/ethnicity, poverty, nativity, body mass index (BMI; defined as weight in kilograms divided by the square of height in meters and used as a proxy for caloric intake), markers of healthy diet (potassium intake, self-report of overall diet quality), personal CVD-related characteristics (tobacco use, history of CVD, physical inactivity, heavy drinking), and the interaction between race/ethnicity and gender (because of differing subgroup intakes). We calculated the percentage of the total sample who exceeded their recommended daily limit (either high risk or normal).
We used multivariable linear regression to assess the relationship of sodium and BP, adjusted for covariates (age, race/ethnicity, gender, BMI, heavy drinking) and potassium intake. Two additional multivariable linear regression models assessed the relationship between potassium and BP (adjusted for covariates and sodium) and the sodium-to-potassium ratio and BP (adjusted for covariates). Because the literature suggests a differential response of sodium on BP by race/ethnicity, we included interaction terms (sodium × race/ethnicity, potassium × race/ethnicity, sodium-to-potassium ratio × race/ethnicity) in each model. During data collection, we discovered that a technician was consistently using a BP cuff too large for the participants’ arms, leading to artificially low readings. Thus analyses with BP as the outcome did not include these individuals (n = 86). In light of the skewed nature of the sodium data, we repeated analyses with the exclusion of potential outliers and influential points and by log-normalizing sodium; results did not differ. We analyzed data with SUDAAN software version 10.0 (Research Triangle Institute, Research Triangle Park, NC).
RESULTS
We weighted the final sample of 1656 participants to be representative of the New York City population to estimate sodium intake in all city adults. More than 75% of participants were aged 25 to 64 years, about half were male, more than half were Black or Hispanic, almost half were non–US-born, and close to half had an income less than 200% of the 2010 federal poverty level of the US Department of Health and Human Services (Table 1). The population was evenly distributed as normal weight, overweight, and obese, and about 70% of participants rated their diet as good, very good or excellent. About 40% were current or former smokers, 37% had a history of CVD, 24% were physically inactive over the past 30 days, and 5% were heavy drinkers.
TABLE 1—
Sample Characteristics: Heart Follow-Up Study, New York City, 2010
| Characteristic | No. (%) | Weighted No. (Weighted %) |
| Total sample | 1656 (100) | 6 222 961 (100) |
| Age, y | ||
| 18–24 | 102 (6.2) | 821 000 (13.2) |
| 25–44 | 504 (30.5) | 2 698 000 (43.4) |
| 45–64 | 701 (42.4) | 1 739 144 (28.0) |
| ≥ 65 | 348 (21.0) | 962 000 (15.5) |
| Gender | ||
| Male | 692 (41.8) | 2 875 000 (46.2) |
| Female | 964 (58.2) | 3 348 000 (53.8) |
| Race/ethnicity | ||
| Non-Hispanic White | 612 (37.0) | 2 406 000 (38.7) |
| Non-Hispanic Black | 440 (26.6) | 1 429 000 (23.0) |
| Hispanic | 485 (29.3) | 1 538 000 (24.7) |
| Non-Hispanic Asian | 84 (5.1) | 627 000 (10.1) |
| Other | 35 (2.1) | 224 000 (3.6) |
| Poverty status,a % | ||
| < 200 | 720 (45.1) | 2 905 000 (48.0) |
| 200–399 | 267 (16.7) | 910 000 (15.0) |
| ≥ 400 | 520 (32.6) | 1 715 000 (28.3) |
| Country of birth | ||
| United States | 956 (57.9) | 3 319 000 (53.4) |
| Not United States | 696 (42.1) | 2 895 000 (46.6) |
| BMI, kg/m2 | ||
| Underweight (< 18.5) | 39 (2.4) | 174 000 (2.8) |
| Normal (18.5–24.9) | 521 (31.5) | 1 994 000 (32.1) |
| Overweight (25–29.9) | 566 (34.3) | 2 162 000 (34.8) |
| Obese (≥ 30) | 526 (31.8) | 1 885 000 (30.3) |
| Diet quality | ||
| Excellent | 233 (14.2) | 731 000 (11.9) |
| Very good | 416 (25.3) | 1 646 000 (26.8) |
| Good | 548 (33.3) | 2 024 000 (33.0) |
| Fair | 370 (22.5) | 1 487 000 (24.2) |
| Poor | 77 (4.7) | 251 000 (4.1) |
| Smoker | ||
| Never | 918 (55.7) | 3 698 000 (59.5) |
| Current | 287 (17.4) | 1 099 000 (17.7) |
| Former | 443 (26.9) | 1 413 000 (22.8) |
| Hypertension | ||
| Yes | 589 (35.6) | 1 838 000 (29.6) |
| No | 1064 (64.4) | 4 375 000 (70.4) |
| Diabetes | ||
| Yes | 219 (13.2) | 656 000 (10.5) |
| No | 1437 (86.8) | 5 567 000 (89.5) |
| Chronic kidney disease | ||
| Yes | 235 (14.2) | 822 000 (13.2) |
| No | 1421 (85.8) | 5 401 000 (86.8) |
| Personal history of CVD | ||
| Yes | 611 (36.9) | 1 930 000 (31.0) |
| No | 1045 (63.1) | 4 292 000 (69.0) |
| Physical activity in past 30 d | ||
| Yes | 1257 (75.9) | 4 624 000 (74.3) |
| No | 399 (24.1) | 1 599 000 (25.7) |
| Heavy drinker | ||
| Yes | 82 (5) | 357 000 (5.8) |
| No | 1559 (95) | 5 794 000 (94.2) |
Note. BMI = body mass index; CVD = cardiovascular disease.
According to 2010 federal poverty guidelines of US Department of Health and Human Services. “Don’t know” category not shown, so percentages do not sum to 100.
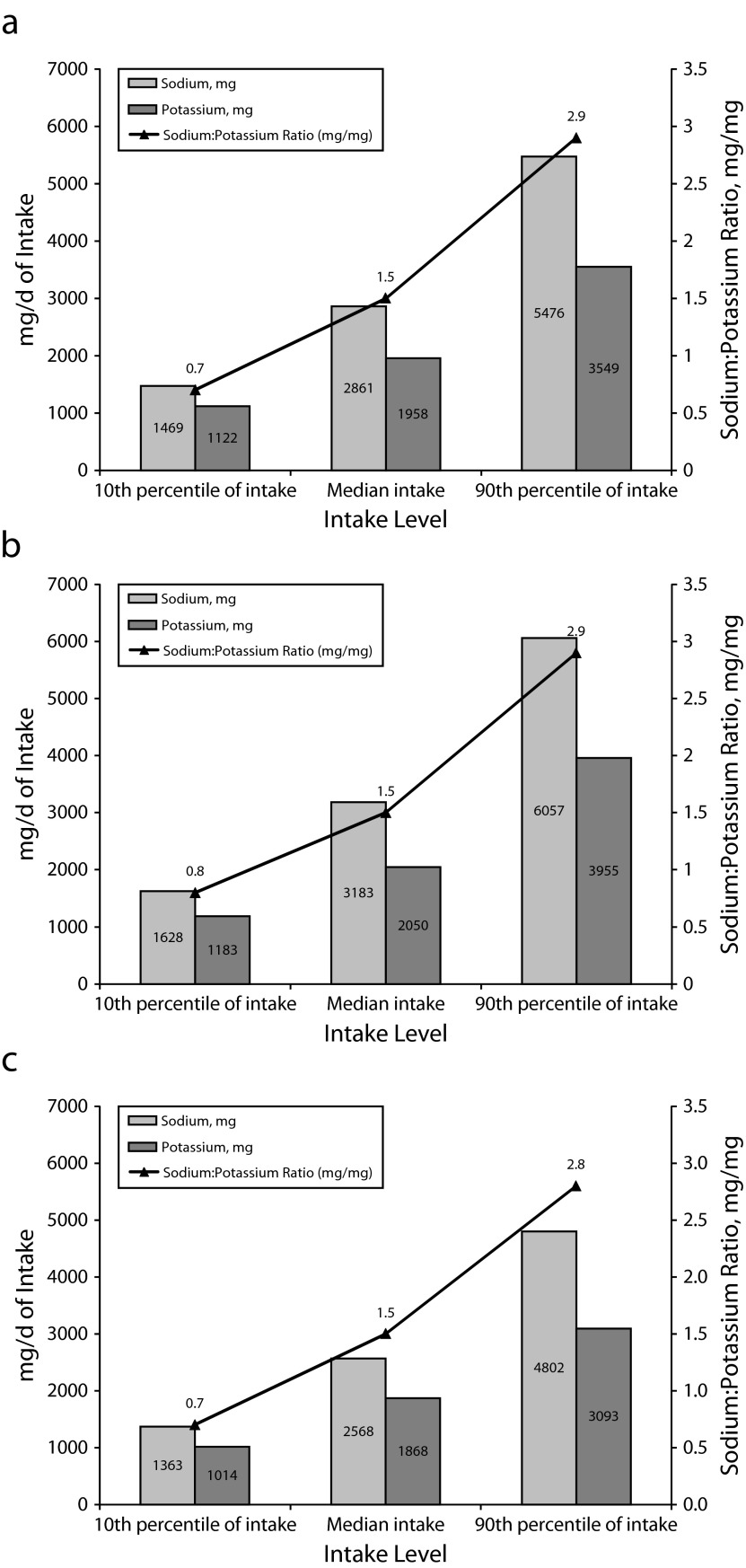
The unadjusted mean daily sodium intake was 3239 milligrams per day (median = 2861 mg/d). Ten percent of New Yorkers were consuming 1469 milligrams per day of sodium or less (Figure 1a); 10% of men were consuming 1628 milligrams per day or less, and 10% of women were consuming 1363 milligrams per day or less (Figure 1b and 1c). Mean sodium intake was higher in men than women (3583 mg/d vs 2944 mg/d; P < .001) and was lower in participants aged 65 years or older than in those aged 25 to 44 years (Table 2). Mean systolic BP was 121.6 millimeters of mercury; mean diastolic BP was 74.3 millimeters of mercury. Mean urinary creatinine excretion was 13 millimoles per day (1477 mg/d); 16 millimoles per day (1800 mg/d) in men and 11 millimoles per day (1250 mg/d) in women (data not shown).
FIGURE 1—
Percentiles of sodium and potassium intakes and sodium-to-potassium ratio in (a) adults, (b) men, and (c) women: Heart Follow-Up Study, New York City, 2010.
TABLE 2—
Weighted Mean Daily Sodium Intake by Gender and Demographic Characteristics: Heart Follow-Up Study, New York City, 2010
| Characteristic | Men, Unadjusted Sodium Intake (mg/d),a Weighted Mean (SE) | Women, Unadjusted Sodium Intake (mg/d),a Weighted Mean (SE) | Total Sample, Unadjusted Sodium Intake (mg/d),a Weighted Mean (SE) | Total Sample, Adjusted Sodium Intake (mg/d),ab Weighted Mean (SE) |
| Total sample | 3583 (98) | 2944 (74) | 3239 (98) | |
| Age, y | ||||
| 18–24 | 4069 (281) | 2849c (223) | 3445 (193) | 3718 (182) |
| 25–44 | 3484 (166) | 3026 (133) | 3248 (107) | 3241 (103) |
| 45–64 | 3821 (154) | 3169 (109) | 3467 (92) | 3305 (89) |
| ≥ 65 | 2906* (139) | 2459*** (117) | 2630*** (91) | 2757** (105) |
| Race/ethnicity | ||||
| Non-Hispanic White (Ref) | 3306 (122) | 2785 (132) | 3066 (89) | 2949 (94) |
| Non-Hispanic Black | 4191*** (214) | 2909 (141) | 3477* (139) | 3541 (116) |
| Hispanic | 3889* (238) | 3142 (125) | 3395* (123) | 3490* (110) |
| Non-Hispanic Asian | 3182c (318) | 2953c (323) | 3068 (225) | 3365 (227) |
| Other | 3043c (193) | 2944c (287) | 2992c (175) | 3039 (198) |
| Poverty status, % | ||||
| < 200 | 3710 (167) | 3032 (100) | 3306 (93) | 3275 (88) |
| 200–399 | 3807 (221) | 2914 (145) | 3350 (140) | 3370 (126) |
| ≥ 400 (Ref) | 3452 (150) | 2854 (165) | 3200 (110) | 3208 (109) |
| Country of birth | ||||
| United States (Ref) | 3562 (120) | 2993 (112) | 3299 (83) | 3330 (80) |
| Not United States | 3619 (165) | 2906 (98) | 3176 (90) | 3160 (77) |
| BMI, kg/m2 | ||||
| Underweight (< 18.5) | 4138c (1131) | 2603c (458) | 3130c (524) | 3292 (569) |
| Normal (18.5–24.9; Ref) | 3444 (162) | 2698 (128) | 3040 (104) | 3105 (94) |
| Overweight (25–29.9) | 3387 (143) | 2820 (124) | 3114 (96) | 3125 (97) |
| Obese (≥ 30) | 3988* (200) | 3342*** (133) | 3609*** (116) | 3549*** (107) |
| Diet quality | ||||
| Excellent (Ref) | 3236 (203) | 2378 (146) | 2779 (131) | 2758 (159) |
| Very good | 3377 (182) | 2877* (165) | 3132 (124) | 3268* (109) |
| Good | 3761 (178) | 2985*** (137) | 3345*** (114) | 3381*** (93) |
| Fair | 3686 (207) | 3116*** (140) | 3368*** (121) | 3233* (120) |
| Poor | 4200c (472) | 3563*** (206) | 3802*** (219) | 3599*** (202) |
| Smoker | ||||
| Never (Ref) | 3442 (128) | 2941 (93) | 3149 (76) | 3179 (75) |
| Current | 4009* (224) | 3022 (183) | 3496* (153) | 3397 (135) |
| Former | 3592 (194) | 2888 (164) | 3287 (133) | 3330 (111) |
| Personal history of CVD | ||||
| Yes | 3740 (206) | 2822 (108) | 3165 (106) | 3214 (117) |
| No (Ref) | 3531 (111) | 3013 (97) | 3273 (75) | 3268 (64) |
| Physically active in past 30 d | ||||
| Yes (Ref) | 3491 (114) | 2865 (85) | 3152* (70) | 3181 (60) |
| No | 3841 (181) | 3177 (148) | 3491 (120) | 3450* (113) |
| Heavy drinker | ||||
| Yes (Ref) | 4291c (393) | 3320c (431) | 3772 (305) | 3633 (264) |
| No | 3547 (101) | 2916 (73) | 3205 (62) | 3228 (56) |
Note. BMI = body mass index; CVD = cardiovascular disease.
Normalized to 24-hour collection time.
Adjusted for all other covariates listed in the table, gender, potassium, race × gender interaction in linear regression with sodium as the dependent variable. For race × gender interaction. P = .02.
Estimate’s relative SE (a measure of estimate precision) was > 30% or the sample size was < 50, making the estimate potentially unreliable.
*P < .05; **P < .01; ***P < .001.
Blacks had the highest sodium intake of all racial/ethnic groups, and both Blacks and Hispanics had higher intake than Whites (3477 mg/d, 3395 mg/d, and 3066 mg/d, respectively; P = .01 for Blacks and .03 for Hispanics; Table 2). The pattern differed by gender: Black men had a higher sodium intake than White men, but Black women's intake was not statistically significantly higher than White women's. Whites and Asians did not differ significantly in sodium intake. We also observed no differences by poverty status or nativity. Obese participants had higher daily sodium intake than their normal-weight counterparts (3609 mg/d vs 3040 mg/d; P < .001). Patterns varied by lifestyle factors (healthier diets, smoking, physical activity), as shown in Table 2; participants who reported healthier diets consumed lower amounts of sodium (excellent, 2779 mg/d vs poor, 3802 mg/d; P < .001) Multivariable linear regression reflected similar differences in sodium intake after adjustment (Table 2), although the higher sodium intake in Blacks than in Whites was no longer significant.
The majority of adults in New York City, 81%, exceeded recommended daily limits for sodium consumption. More than half of adults (62.1%; 95% confidence interval [CI ] = 58.0, 66.0) met criteria for high risk, but only 9.2% of these were consuming less than the recommended limit (< 1500 mg/d; Table 3). Among the rest of the population, 34.6% achieved the goal of not exceeding the recommended sodium intake (< 2300 mg/d).
TABLE 3—
Percentage of Adult New Yorkers Meeting Recommended Daily Sodium Intake Limits: Heart Follow-Up Study, New York City, 2010
| Characteristic | Mean Sodium Intake (mg/d), Weighted Mean (SE) | Consuming Recommended Limit for High Risk,a Weighted % (95% CI) | Consuming Recommended Limit for Normal Risk,b Weighted % (95% CI) |
| Persons at high riskc | |||
| Total | 3336 (76) | 9.2 (6.9, 12) | 29.1 (25.2, 33.5) |
| Aged ≥ 51 y | 3054 (73) | 12.1 (8.8, 16.3) | 34.7 (29.8, 39.9) |
| Black | 3477 (139) | 11.3 (6.9, 17.9) | 28.9 (22.3, 36.6) |
| Hypertension | 3375 (123) | 10.8 (7.3, 15.7) | 31.1 (25.2, 37.8) |
| Diabetes | 3557 (159) | 9.2 (5.3, 15.3) | 24.3 (17.2, 33.1) |
| Chronic kidney disease | 3683 (170) | 8.3d (4.5, 15.0) | 21.4 (14.6, 30.1) |
| All other New Yorkers | 3084 (104) | 13.3 (9.3, 18.7) | 34.6 (28.3, 41.5) |
Note. CI = confidence interval.
< 1500 mg/d.
< 2300 mg/d.
Categories not mutually exclusive.
Estimate’s relative SE (a measure of estimate precision) was > 30% or the sample size was < 50, making the estimate potentially unreliable.
Multivariable regression analyses demonstrated a positive association between sodium and systolic BP overall (0.82 mm Hg higher systolic BP/1000 mg/d higher sodium intake; 95% CI = 0.02, 1.62; P = .04); the relationship between sodium and diastolic BP was not statistically significant (0.36 mm Hg higher diastolic BP/1000 mg/d higher sodium intake; 95% CI = −0.20, 0.93; P = .21). The association between sodium intake and BP was modified by race/ethnicity (P for interaction = .01). The association between sodium and BP was larger in Blacks than Whites; for every 1000 milligrams per day of sodium, systolic BP was 1.83 millimeters of mercury higher in Blacks than in Whites (95% CI = 0.52, 3.15; P = .01), after adjustment for covariates (continuous age, gender, BMI, heavy drinking, poverty status) and potassium intake (full results not shown). The effect was marginally significant in Hispanics versus Whites (1.43 mm Hg difference; 95% CI = 0.00, 2.87; P = .05) and did not differ between Asians and Whites (−0.30 mm Hg difference; 95% CI = −2.49, 1.88; P = .78; data not shown).
Potassium intake was not associated with BP (−0.57 mm Hg difference/1000 mg change in potassium; 95% CI = −2.52, 1.39; P = .57) after adjustment for covariates, including sodium intake, nor was it modified by race/ethnicity (P for interaction = 0.77). A 1-unit increase in the sodium-to-potassium ratio was associated with a 1.98 millimeters of mercury higher systolic BP (95% CI = 0.73, 3.23; P < .01) after adjustment for covariates; this association was not modified by race/ethnicity (P for interaction = .08). Diastolic BP was not significantly associated with either sodium or potassium intake separately in regression models, but was 1.20 millimeters of mercury higher (95% CI = 0.27, 2.13; P = .01) with a 1-unit increase in the sodium-to-potassium ratio (data not shown).
DISCUSSION
In a population-based sample with measurement of sodium intake by the 24-urine collection method rather than dietary self-report, intake greatly exceeded recommended limits in all demographic groups and was particularly high among non-Hispanic Blacks and Hispanics. Mean sodium intake was approximately twice the recommended limit for those at higher risk.
Although the estimate of 3239 milligrams sodium per day in New York City adults is similar to national estimates derived from dietary recall (3400 mg/d, not including salt added at the table),20 our finding of substantially higher sodium intake in non-Hispanic Blacks and Hispanics than in Whites has not been observed in previous studies.5 Bias in food intake surveys may partly explain the difference. People with a higher BMI are more likely than others to underreport caloric intake.21 Blacks and Hispanics have a higher prevalence of obesity and overweight than Whites,22 and because sodium intake tracks closely with calorie intake,23 self-reported sodium intake may be underestimated in Blacks and Hispanics. The association between race/ethnicity and intake persisted for Hispanics but became nonsignificant in Blacks after adjustment for other covariates, including BMI, suggesting that BMI or caloric intake may be an important mediator.
Multivariable regression analyses of the association between sodium and BP revealed that the relationship between sodium intake and systolic BP was modified by race, with a larger effect observed in Blacks than in Whites (P for interaction = .04). This finding corroborates previous studies, including clinical trials,20,24,25 and is of particular concern in light of the new observation that Black New Yorkers consume more sodium daily than do Whites and the fact that the prevalence of hypertension- and CVD-related mortality is higher in Blacks than Whites.26,27 These racial differences in sodium intake are important for New York City and possibly nationally. Although potassium intake itself was not associated with BP in our study sample after adjustment for sodium intake, we observed a striking relationship between the sodium-to-potassium ratio and BP. Aiming to reduce this ratio to an optimal level is a potential goal for all adults regardless of race/ethnicity, because the ratio may be a stronger predictor of cardiovascular morbidity and mortality than either nutrient alone.28,29 The current national and global attention on reducing sodium intake as a means to improve health can potentially contribute to favorable changes in the ratio in all adults.
We detected no significant difference in sodium intake by income, and others have not consistently observed an association between these variables.2,5 This may reflect a general reliance on packaged and restaurant foods across income strata and the presence of sodium in processed foods, often independent of cost or quality. However, we found a remarkably robust relationship between self-reported overall quality of diet and sodium intake; further exploration of this variable through validation studies is warranted. Even when we controlled for income and other relevant demographics, increases in reported quality of diet correlated with decreases in sodium intake. Because of the dominance of processed food, it is difficult to reduce sodium intake to recommended levels through knowledge alone. Broadscale reductions in population sodium intake have been achieved in other countries through national policy efforts,11 which have extended beyond public awareness campaigns to include changing the amount of sodium in processed foods.10–12
Limitations
Although meticulous 24-hour urine collection is the gold standard method of estimating sodium intake, it is not infallible.9 The potential for incomplete collection of urine by the participant is a primary limitation of this method. Inconsistent29,30 or paradoxical31,32 conclusions from other studies employing this method have been attributed to the inclusion of incomplete urine collections. From study design to implementation to laboratory and data analysis, we took this into consideration (Appendix A, available as an online supplement). For example, we investigated criteria for a complete urine collection, and we excluded samples that did not meet the criteria. Application of these criteria resulted in a study sample that was similar in demographic characteristics to the overall sample, suggesting that participants were excluded at random. We concluded that these excluded participants were therefore true undercollectors rather than participants who had low urine volume or creatinine excretion attributable to biological differences (i.e., female gender, small stature) or underlying chronic conditions. It is possible that a single 24-hour collection may not be representative of an individual’s typical intake because of the high intraperson variability of sodium excretion, although this is less problematic in population-level estimates.
We used the commonly employed approach of weighting to account for the complex survey design and nonresponse. We recognize that this is an imperfect method, resulting in limitations with respect to representativeness of the full New York City population and generalizability, although our stratified sample ensured representativeness across diverse parts of the city. Recruiting from a random-digit-dial sampling frame was a unique approach, and our study established follow-up recruitment from a random-digit-dial frame as a cost-effective means for conducting population-level surveillance, even with the inclusion of a 24-hour urine collection and an in-home visit.
Conclusions
Our findings illustrate the value of the 24-hour urine collection method, particularly to assess disparities that are potentially masked in self-report data. These data are a critical evaluation component to help understand the potential impact of population-wide sodium reduction activities, such as the US National Salt Reduction Initiative. This initiative and other programs,33 such as those in the United Kingdom and under development elsewhere, aim to achieve reductions in population sodium intake by working directly with the food industry to reduce sodium in processed foods. Our findings importantly demonstrate the feasibility of building a sample for 24-hour urine collection from an existing population-based data source and the way these data may be used to understand population risk, guide policy development, and, ultimately, measure the impact of our efforts.
Acknowledgments
The Heart Follow-Up Study was made possible by funding from the Robert Wood Johnson Foundation, the New York State Health Foundation, the National Association of County & City Health Officials, and the Centers for Disease Control and Prevention (grant 5U38HM000449-02), the W. K. Kellogg Foundation, the US Department of Health and Human Services, and New York City through taxes. This funding was administered by the Fund for Public Health in New York, a private nonprofit organization that supports innovative initiatives of the New York City Department of Health and Mental Hygiene.
We thank Michael Sanderson, MS, and Kristin Quitoni, MPH, New York City Department of Health and Mental Hygiene; Cheryl Anderson, PhD, Johns Hopkins Bloomberg School of Public Health; Daniel McConnell, PhD, University of Michigan; Kiang Liu, PhD, Northwestern University Feinberg School of Medicine; and Lorna Thorpe, PhD, Hunter College, City University of New York Graduate Center, for their helpful comments throughout the development of this project, data collection, and article preparation.
Note. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official view of the funders.
Human Participant Protection
The New York City Health Department’s institutional review board approved this study.
References
- 1.Kochanek KD, Xu JQ, Murphy SL, Miniño AM, Kung HC. Deaths: final data for 2009. Natl Vital Stat Rep. 2011;60(3):1–116. [PubMed] [Google Scholar]
- 2.Dietary Guidelines for Americans, 2010. 7th ed. Washington, DC: US Department of Agriculture and US Department of Health and Human Services; 2010. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Sodium intake among adults—United States, 2005–2006. MMWR Morb Mortal Wkly Rep. 59(24):746–749. [PubMed] [Google Scholar]
- 4.Healthy People 2020. Washington, DC: US Department of Health and Human Services; 2010. [Google Scholar]
- 5.Institute of Medicine. Strategies to Reduce Sodium Intake in the United States. Washington, DC: National Academies Press; 2010. [Google Scholar]
- 6.Bibbins-Domingo K, Chertow GM, Coxson PG et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362(7):590–599. doi: 10.1056/NEJMoa0907355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sacks FM, Svetkey LP, Vollmer WM et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344(1):3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 8.Vollmer WM, Sacks FM, Ard J et al. Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial. Ann Intern Med. 2001;135(12):1019–1028. doi: 10.7326/0003-4819-135-12-200112180-00005. [DOI] [PubMed] [Google Scholar]
- 9.Bentley B. A review of methods to measure dietary sodium intake. J Cardiovasc Nurs. 2006;21(1):63–67. doi: 10.1097/00005082-200601000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Food Standards Agency, United Kingdom. Impact assessment of the revised salt reduction targets. 2008 Available at: http://www.food.gov.uk/multimedia/pdfs/consultation/consultsalttargets.pdf. Accessed May 7, 2008. [Google Scholar]
- 11.National Centre for Social Research, United Kingdom. An assessment of dietary sodium levels among adults (aged 19–64) in the UK general population in 2008, based on analysis of dietary sodium in 24-hour urine samples. Available at: http://www.food.gov.uk/multimedia/pdfs/08sodiumreport.pdf. Accessed May 7, 2008.
- 12.Henderson L, Irving K, Gregory J . The National Diet and Nutrition Survey: Adults Aged 19 to 64 Years. London, UK: Office for National Statistics, Medical Research Council Human Nutrition Research and Food Standards Agency; 2003. [Google Scholar]
- 13.Reinivuo H, Valsta LM, Laatikainen T, Tuomilehto J, Pietinen P. Sodium in the Finnish diet: II trends in dietary sodium intake and comparison between intake and 24-h excretion of sodium. Eur J Clin Nutr. 2006;60(10):1160–1167. doi: 10.1038/sj.ejcn.1602431. [DOI] [PubMed] [Google Scholar]
- 14.Strategies to monitor and evaluate population sodium consumption and sources of sodium in the diet. Report of a joint technical meeting convened by WHO and the Government of Canada. 2010. Available at: http://whqlibdoc.who.int/publications/2011/9789241501699_eng.pdf. Accessed November 6, 2013.
- 15.Sanderson M, Yi S, Bartley K . 2012. The Community Health Survey, Heart Follow-Up Study methodology report. Department of Health and Mental Hygiene. Available at: http://www.nyc.gov/html/doh/html/diseases/salt.shtml. Accessed January 1, 2014. [Google Scholar]
- 16.New York City Department of Health and Mental Hygiene. Community Health Survey. Available at: http://www.nyc.gov/html/doh/html/survey/survey.shtml. Accessed December 14, 2012.
- 17.National Health and Nutrition Examination Survey. Physician examination procedures manual. Available at: http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_pe.pdf. Accessed July 1, 2009.
- 18.Ostchega Y, Nwankwo T, Sorlie PD, Wolz M, Zipf G. Assessing the validity of the Omron HEM-907XL oscillometric blood pressure measurement device in a National Survey environment. J Clin Hypertens (Greenwich) 2010;12(1):22–28. doi: 10.1111/j.1751-7176.2009.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.US Department of Health and Human Services. Poverty guidelines for the remainder of 2010. Available at: http://aspe.hhs.gov/poverty/10poverty.shtml. Accessed September 1, 2010.
- 20.Institute of Medicine. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: National Academies Press; 2004. [Google Scholar]
- 21.Poslusna K, Ruprich J, de Vries JH, Jakubikova M, van’t Veer P. Misreporting of energy and micronutrient intake estimated by food records and 24 hour recalls, control and adjustment methods in practice. Br J Nutr. 2009;101(suppl 2):S73–S85. doi: 10.1017/S0007114509990602. [DOI] [PubMed] [Google Scholar]
- 22.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 23.Hoy MK, Goldman JD, Murayi T, Rhodes DG, Moshfegh AJ. Sodium Intake of the US Population: What We Eat in America, NHANES 2007–2008. Washington, DC: Food Surveys Research Group, US Dept of Agriculture; 2011. Dietary Data Brief 8. [Google Scholar]
- 24.Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension. 2006;47(2):296–308. doi: 10.1161/01.HYP.0000202568.01167.B6. [DOI] [PubMed] [Google Scholar]
- 25.He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009;23(6):363–384. doi: 10.1038/jhh.2008.144. [DOI] [PubMed] [Google Scholar]
- 26.Department of Health and Mental Hygiene. Summary of vital statistics 2010: the city of New York, population and mortality. 2012 Available at: http://www.nyc.gov/html/doh/downloads/pdf/vs/vs-population-and-mortality-report.pdf. Accessed April 1, 2012. [Google Scholar]
- 27.Angell SY, Garg RK, Gwynn RC, Bash L, Thorpe LE, Frieden TR. Prevalence, awareness, treatment, and predictors of control of hypertension in New York City. Circ Cardiovasc Qual Outcomes. 2008;1(1):46–53. doi: 10.1161/CIRCOUTCOMES.108.791954. [DOI] [PubMed] [Google Scholar]
- 28.Cook NR, Obarzanek E, Cutler JA et al. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: the Trials of Hypertension Prevention follow-up study. Arch Intern Med. 2009;169(1):32–40. doi: 10.1001/archinternmed.2008.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang Q, Liu T, Kuklina EV et al. Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2011;171(13):1183–1191. doi: 10.1001/archinternmed.2011.257. [DOI] [PubMed] [Google Scholar]
- 30.Cohen HW, Hailpern SM, Alderman MH. Sodium intake and mortality follow-up in the Third National Health and Nutrition Examination Survey (NHANES III) J Gen Intern Med. 2008;23(9):1297–1302. doi: 10.1007/s11606-008-0645-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O’Donnell MJ, Yusuf S, Mente A et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011;306(20):2229–2238. doi: 10.1001/jama.2011.1729. [DOI] [PubMed] [Google Scholar]
- 32.Stolarz-Skrzypek K, Kuznetsova T, Thijs L et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011;305(17):1777–1785. doi: 10.1001/jama.2011.574. [DOI] [PubMed] [Google Scholar]
- 33.Angell SY, Farley TA. Can we finally make progress on sodium intake? Am J Public Health. 2012;102(9):1625–1627. doi: 10.2105/AJPH.2012.300722. [DOI] [PMC free article] [PubMed] [Google Scholar]