Abstract
Objectives. We examined the ways in which adolescents altered the type and size of their purchases of sugar-sweetened beverages (SSBs), together with whether the effects persisted after removing caloric information signs in stores.
Methods. We used a case-crossover design with 6 stores located in low-income Black neighborhoods in Baltimore, Maryland, from 2012 to 2013. The intervention used 1 of 4 randomly posted signs with caloric information: absolute calories, number of teaspoons of sugar, and number of minutes of running or miles of walking necessary to burn off a beverage. We collected data for 4516 purchases by Black adolescents, including both baseline and postintervention periods with no signs posted.
Results. We found that providing caloric information significantly reduced the number of total beverage calories purchased, the likelihood of buying an SSB, and the likelihood of buying an SSB greater than 16 ounces (P < .05). After removing the signs, the quantity, volume, and number of calories from SSB purchases remained lower than baseline (P < .05).
Conclusions. Providing caloric information was associated with purchasing a smaller SSB, switching to a beverage with no calories, or opting to not purchase a beverage; there was a persistent effect on reducing SSB purchases after signs were removed.
An important contributor to adolescent obesity1–4 is the consumption of sugar-sweetened beverages (SSBs). SSB consumption is highest among minority adolescents; it is approximately 15% of their daily caloric intake.5,6 Although American Health Association guidelines recommend that SSB consumption be limited to 8 to 12 ounces per day for children 7 to 18 years old,7 Black adolescents appear to consume at least twice that much of SSBs daily.6
Understanding the potential for environmental interventions, which are increasingly seen as essential for obesity prevention,8 to motivate reductions in SSB consumption among groups at high risk of obesity is important. Clinical obesity interventions are not easily accessible to all adolescents, and most adolescents who begin obesity treatment do not complete it,9 with poor and minority youths at even higher risk for discontinuing treatment.10
One promising environmental strategy to reduce consumption of SSBs is to provide consumers with easily interpretable caloric information; this is the result of the empirical evidence that suggests that consumers significantly underestimate the amount of calories in the foods they consume,11–13 and that consumer choices can be markedly affected by information.14,15 Moreover, relative caloric information, such as the running minutes required to burn off a particular beverage (as opposed to absolute calories), may be more effective in reducing consumption.16,17
Our previous work,17 which was the only study on caloric labeling to focus on low-income Black adolescents, examined the effect of providing caloric information and found that providing this information in the form of a physical activity equivalent (e.g., minutes of running required to burn off a bottle of soda), relative to no information, significantly reduced the likelihood that an observed beverage purchase was an SSB and increased the likelihood of a water purchase.17 However, our previous study was unable (1) to examine the decision to purchase any beverage or the size of beverage purchased; (2) to determine whether study participants understood or believed the caloric information, which was critical based on the research that suggested that information could only affect purchasing behavior if individuals noticed or perceived it13,18,19; (3) to examine which type of caloric information was most effective (because of the small sample size); or (4) to examine whether exposure to caloric information had a persistent effect postintervention. These key unanswered questions from our initial study are important areas of inquiry that have not been previously addressed in the research.
The previous literature related to the persistence or duration of information and behavior change is particularly scarce. A recently published theoretical framework that examined consumer responses to nutrition information on food labels posited that a label’s effect on purchasing might persist over time, even after the label was removed.20 By contrast, empirical evidence from the literature on mass media campaigns for tobacco cessation suggested that the removal of information was associated with a decline in beneficial effects.21–23
Our main purpose of this study was to identify the most effective modes of communicating SSB caloric information among Black adolescents to reduce the quantity, volume, and number of calories from SSB purchases. Our secondary aim was to examine whether providing caloric information had a persistent effect on behavior after it was removed. For our primary aim, we hypothesized that providing caloric information in an easily understandable format would reduce adolescent purchases of SSBs in 3 different ways: forgoing any beverage purchase, switching to a non-SSB, and switching to a smaller SSB. For our secondary aim, we hypothesized that caloric information would have an attenuated, but persistent effect, on beverage purchasing after the intervention ended.
METHODS
We designed an intervention to provide caloric information on SSBs in 6 stores and collected data on the purchases made both before and after the intervention. The design for this study is a variant of the case-crossover design, and allowed us to identify whether the change in SSB purchases after the intervention was greater than would be expected as a result of chance.24 The target population was low-income Black adolescents, aged 12 to 18 years, living in Baltimore, Maryland.
We identified 6 corner stores proximal to middle and high schools in Baltimore. We used Google Maps (Menlo Park, CA) rather than existing business databases to identify potential stores, because corner stores are less likely to be included in these listings.25 Corner stores were eligible for inclusion if they were within walking distance of a middle school or high school (5 city blocks or less), the population of the zip code was 70% or more Black, and if water and diet soda were available in the store’s beverage cases.
Caloric Information Intervention
We developed 4 different interventions to provide caloric information on SSBs: absolute caloric count, number of teaspoons of sugar, and the number of minutes of running and the number of miles of walking required to burn off the calories. The latter 3 signs were selected based on focus groups with Black adolescents in which we tested various physical activity equivalents. (Our previous study used 3 different signs: absolute calories, percent daily calories, and minutes of running.17)
We used 250 calories for the absolute caloric count by obtaining this number directly from the nutritional label on a typical soda bottle (20 ounces). To translate calories into teaspoons of sugar, we converted the grams of sugar in a bottle of soda into teaspoons (1 teaspoon = 4.2 g). To translate calories into physical activity equivalents, we used the energy balance equation, described in detail elsewhere.26 We calculated that a 15-year-old adolescent weighing 110 pounds (50 kg) would need to replace sitting with running for 50 minutes or walking for 5 miles to burn off 250 extra calories from a bottle of soda.
For each of the 4 interventions (type of caloric information), a brightly colored 8.5- × 11-inch sign was placed in a prominent location on each beverage case in each corner store. The following text was used on the signs to depict the 4 different of caloric information. (1) “Did you know that a bottle of soda or fruit juice has about 250 calories?” (2) “Did you know that a bottle of soda or fruit juice has about 16 teaspoons of sugar?” (3) “Did you know that working off a bottle of soda or fruit juice takes about 50 minutes of running?” (4) “Did you know that working off a bottle of soda or fruit juice takes about 5 miles of walking?”
Data Collection
Information on all purchases at the register was obtained for a random sample of Black adolescents who appeared to be between the ages of 12 and 18 years; these purchases included those when a beverage was not selected. All study data were collected by 5 research assistants in the corner stores. For the baseline period, and the intervention and postintervention periods, a random sample of approximately 35 adolescent purchases was collected per store per week. For each recorded purchase, we collected information on whether the adolescent bought a beverage and the gender of the individual, along with the date, time, and store location. For each beverage sale, information was collected on the type and volume of beverage purchased. The type of SSBs included soda, fruit drink, sport drink, vitamin water, and “hug” (a fruit drink packaged in 8-ounce bottles); the type of non-SSBs included diet soda, water, and 100% juice. We recorded the volume in ounces and determined the number of calories for each purchase.
We collected the baseline data at each of the 6 corner stores for approximately 4 weeks. Following baseline data collection, we randomly assigned the corner stores to each type of caloric information for approximately a 2-week period, during which we collected beverage sales data. Before collecting data for each type of caloric information, we allowed for a week of “burn-in” time, in which the caloric information was posted but beverage sales were not recorded. Between each type of caloric information, we allowed for a week of “washout” time, in which caloric information was removed and beverage sales were not recorded. During the postintervention period, which lasted 6 weeks, all caloric information was removed. The study design can be found as data available as a supplement to the online version of this article at http://www.ajph.org.
We collected data on school days over 10 months, from August 2012 to June 2013. Data for 4516 purchases by Black adolescents, aged 12 to 18 years, were collected, 3098 of which were beverages. This included 816 purchases during the baseline period (601 beverage purchases), and 3433 purchases evenly spread across all 4 caloric information interventions (2311 beverage purchases), and 267 postintervention (186 beverage purchases). Study staff conducted site visits at least twice a week at each store to assure that the signs providing the caloric information were appropriately displayed on the beverage refrigerators.
Exit Interviews
We also conducted exit interviews among one quarter of the sample across all stores. We used the “street-intercept” method,27 in which adolescents were asked to answer: whether they had noticed the sign; if so, whether they understood the information; whether they believed the information; and whether the information influenced their purchase. Adolescents were compensated with at $5 Target gift card for participating.
We used text messages between the research assistants recording beverage purchases and the research assistants conducting the exit interviews to identify which adolescents to intercept for the exit interviews. This allowed us to ensure that the adolescents participating in the exit interviews were a subset of the entire study sample. All exit interviews were conducted during data collection for the last caloric condition (which varied randomly by store) to avoid possible contamination of the interviews on purchasing behavior. Also to address possible cross-contamination, the research assistants completing the exit interviews stood around the corner or at least 10 to 15 feet away from the store entrance.
Outcome Measures
We examined 3 main outcomes: total number of calories (calculated from the volume and beverage type), whether an SSB was purchased, and whether a large volume SSB was purchased. For the third measure, we dichotomized beverage volume into greater than 16 ounces or 16 ounces or less because of the recent efforts by New York City Former Mayor Bloomberg to ban SSBs greater than 16 ounces in food service establishments regulated by the city (e.g., restaurants and movie theaters).28 For the latter 2 outcomes, we also examined type-specific outcomes—for example, whether a water bottle was purchased and whether a large-volume soda was purchased.
We examined these 3 main outcomes for 3 different study samples: the full sample of 4516 purchases (including purchases without beverages); the subsample of 3098 beverage purchases; and the subsample of 2794 SSB purchases. Examining these samples allowed us to help distinguish the impact of the caloric information on 3 possible behavior changes: purchasing no beverage, switching from an SSB to a non-SSB, and purchasing a smaller SSB.
Statistical Analysis
For each of the outcome variables, we used multivariate regression models to examine the effects of the 4 types of caloric information on purchasing decisions compared with the baseline period, and to compare the effects of each of the 4 types of caloric information on purchasing decisions relative to each other. We also examined whether the postintervention period’s outcomes differed from the baseline. We controlled for the store where the beverage was purchased, the adolescent’s gender, and time of day (before 4 pm or after 4 pm) to capture whether purchases were made before, during, or after school, and average monthly temperature to adjust for seasonality. Each of these comparisons was made in the sample of all purchases, the sample of all beverage purchases, and the sample of all SSB purchases.
For our first outcome, measuring the total number of calories, we used a 2-part model to account for the high number of zero values where (1) a logistic regression was used to estimate the probability of purchasing any calories, and (2) a generalized linear model with a log-link function and a γ distribution of the error term was used to estimate the number of calories among those who purchased a drink with any calories. For these analyses, zero calorie outcomes included diet drinks and water among the beverage purchases, and no beverages among the full sample. For the 2 binary outcomes (SSB vs non-SSB and > 16 ounces vs ≤ 16 ounces), we used logistic regression analyses. In each of these regressions, the key explanatory variables were indicator variables for the information provided. One set of models used a single indicator variable for whether any information was provided, whereas a second set of models used 4 indicators for the type of calorie information. We then produced the predicted values (and SEs) for these 3 outcomes (i.e., number of calories, the probability of an SSB purchase, and the probability of an SSB purchases > 16 ounces) for each of the types of information provided (i.e., baseline, caloric information, and postintervention) to then illustrate the marginal effects of the intervention. We used the t-test and the χ2 test for the analysis of the exit interviews. In all models, we included store-fixed effects to mitigate concerns about any omitted variable biases resulting from unobservable characteristics correlated with both the outcomes and the stores. All analyses were conducted using STATA version 11.1 (StataCorp, College Station, TX).29
RESULTS
Table 1 reports the characteristics of the study sample, in the pre- and postintervention periods and by the type of caloric information. During the pre- and postintervention periods, most purchases included a beverage, with SSBs more commonly purchased than non-SSBs. In the baseline period, 73% of purchases included a beverage, 97% of all beverage purchases were SSBs, 53% of beverage purchases were large volume SSB beverages, and mean calories per beverage were 207 kilocalories. Characteristics of the entire study sample overall and by store, combining the pre- and postintervention periods, can be found as data available as a supplement to the online version of this article at http://www.ajph.org.
TABLE 1—
Study Sample Characteristics: Preintervention and Postintervention by Type of Caloric Information: Reducing Sugar-Sweetened Beverages Consumption by Providing Caloric Information; Baltimore, MD; 2012–2013
| Baseline |
Intervention |
Postintervention |
||||
| Variable | Stores With No Information Posted (n = 816) | Stores With Absolute Calories Posted (n = 845) | Stores With Teaspoons of Sugar Posted (n = 850) | Stores With Minutes of Running Posted (n = 861) | Stores With Miles of Walking Posted (n = 877) | Stores With No Information Posted (n = 267) |
| Any beverage, no. (%) | 601 (73.4) | 547** (64.7) | 595* (70.0) | 589* (68.4) | 580** (66.1) | 186** (69.7) |
| Any SSB purchase, no. (%)a | 584 (97.2) | 483** (88.3) | 525** (88.7) | 518** (88.0) | 518** (89.3) | 166** (89.3) |
| Any SSB > 16oz, no. (%)a | 321 (53.4) | 210** (38.3) | 254** (42.7) | 265* (45.0) | 263* (45.3) | 54** (29.0) |
| Calories, mean (SD), kcala | 207 (105) | 185** (84) | 188** (77) | 193** (94) | 187** (81) | 175** (79) |
| Gender, no (%)a | ||||||
| Male | 433 (53.1) | 406 (48.1) | 419 (49.3) | 402 (46.7) | 420* (47.9) | 138 (51.7) |
| Female | 383 (46.9) | 439 (51.9) | 431 (50.7) | 459 (53.3) | 457 (52.1) | 129 (48.3) |
| Time, no. (%)a | ||||||
| Before 4 pm | 239 (29.3) | 455** (54.9) | 520** (61.2) | 451** (52.4) | 655** (74.7) | 200** (74.9) |
| 4 pm or after | 577 (70.7) | 390 (46.2) | 330 (38.8) | 410 (47.6) | 222 (25.3) | 67 (25.1) |
| Average monthly temperature, F, mean (SD) | 78 (5.2) | 59 (10.6) | 65 (10.4) | 59 (10.7) | 60 (10.4) | 76 (1.0) |
Note. SSB = sugar-sweetened beverage. Numbers may not sum to 100% because of rounding. The P values were obtained from the χ2 test that compared the percentage of purchases at baseline and each type of caloric information.
These are the summary statistics for the subsample of all beverage purchases.
*P < .05; **P < .01; significantly different from baseline.
Adjusted Beverage Outcomes Based on the Type of Caloric Information
Table 2 presents the regression-adjusted outcomes comparing beverage purchases at baseline with purchases based on the 4 types of caloric information and with purchases during the postintervention period. The full models are available upon request. In each of the 3 samples (all purchases, all beverage purchases, and all SSB purchases), providing any caloric information relative to the baseline significantly reduced the number of total beverage calories purchased, the likelihood of buying an SSB, and the likelihood of buying an SSB greater than 16 ounces (if applicable), after adjusting for adolescent and store characteristics (P < .05). For instance, adolescent purchases averaged 149 calories in the baseline, but these purchases fell to an average of 121 calories across all 4 intervention conditions. Purchases that included a beverage with 203 calories in the baseline fell to an average of 184 calories across all 4 conditions. Moreover, in each of the 3 samples, changes in purchasing behavior persisted after the removal of calorie information postintervention, relative to baseline, after adjusting for covariates (P < .05). For instance, this 149-calorie baseline among all purchases fell to 127 calories postintervention. (The 121 vs 127 calorie comparison was insignificant.) In separate models (not shown), we also examined whether the impact of calorie information on SSB purchases differed for males and females, but we observed no significant differences in gender.
TABLE 2—
Adjusted Beverage Purchase Outcomes Comparing the Types of Caloric Information Provided at Baseline: Reducing Sugar-Sweetened Beverages Consumption by Providing Caloric Information; Baltimore, MD; 2012–2013
| Outcome |
|||
| Variable | Total Calories, kcal (95% CI) | Purchased Any SSB, % (95% CI) | SSB > 16 oz, % (95% CI) |
| Sample: all purchases (n = 4516) | |||
| Baseline | 149 (134.1, 164.1) | 71 (62.8, 79.7) | 39 (28.2, 49.4) |
| Any information | 121a (117.8, 124.9) | 59a (57.0, 61.2) | 25a (22.3, 26.7) |
| Type of information | |||
| Absolute calories | 121 (109.5, 133.0) | 58a (52.1, 63.2) | 24 (16.6, 31.2) |
| Teaspoons of sugar | 123 (112.7, 132.4) | 60 (55.3, 65.1) | 25 (19.5, 31.0) |
| Minutes of running | 123 (108.6, 138.1) | 59 (50.6, 66.4) | 25 (19.8, 30.8) |
| Miles of walking | 115a (107.5, 122.8) | 57a (53.8, 60.2) | 24a (21.6, 26.4) |
| Postintervention | 127a (116.4, 136.7) | 65 (59.2, 70.7) | 23a (15.9, 31.0) |
| Sample: all beverage purchases (n = 3098) | |||
| Baseline | 203 (195.8, 210.2) | 98 (94.3, 1.01) | 54 (42.7, 64.8) |
| Any information | 184a (178.0, 187.5) | 89 (88.1, 90.8) | 37a (33.8, 39.5) |
| Type of information | |||
| Absolute calories | 189 (178.3, 199.4) | 90a (88.2, 91.6) | 37 (27.4, 47.1) |
| Teaspoons of sugar | 182 (171.1, 192.5) | 89 (84.8, 93.7) | 37a (29.3, 44.0) |
| Minutes of running | 186 (175.8, 196.2) | 88a (83.9, 92.7) | 38a (31.8, 43.3) |
| Miles of walking | 179a (171.9, 187.3) | 89a (87.0, 92.0) | 37a (33.1, 40.6) |
| Postintervention | 178a (170.5, 185.6) | 91a (88.4, 94.1) | 33a (23.0, 42.1) |
| Sample: all SSB purchases (n = 2794) | |||
| Baseline | 206 (199.2, 212.7) | . . . | 55 (42.6, 66.9) |
| Any information | 196a (194.1, 198.3) | . . . | 34a (30.9, 37.9) |
| Type of information | |||
| Absolute calories | 202 (190.3, 213.5) | . . . | 35 (23.4, 46.3) |
| Teaspoons of sugar | 194 (184.9, 203.2) | . . . | 35a (27.9, 41.6) |
| Minutes of running | 201b (195.0, 206.9) | . . . | 36a (27.8, 44.5) |
| Miles of walking | 190a (185.5, 194.6) | . . . | 35a (31.0, 38.7) |
| Postintervention | 189a (183.8, 194.4) | 28a (14.1, 41.6) | |
Note. CI = confidence interval; SSB = sugar-sweetened beverage. The “Number of Total Calories” estimates were based on a 2-part model to account for the high number of zero values, where (1) a logistic regression was used to estimate the probability of purchasing any calories, and (2) a generalized linear model with a log-link function and a γ distribution of the error term was used to estimate the number of calories among those who purchased a drink with nonzero calories. The predicted probabilities for the “Purchased Any SSB” and “SSB Greater Than 16 oz” models are based on logistic regression models. These estimates are adjusted for gender, store, time of day (before or after 4 pm), and average monthly temperature.
Source. Purchases from 6 corner stores in a low-income, predominantly Black neighborhood of Baltimore, MD.
Significantly different from baseline, P < .05.
Significantly different from miles of walking, P < .05.
We also compared differences in the effects of the types of caloric information on outcomes relative to each other. We observed statistically significant differences between signs for calorie information presented as miles walking in the all SSB purchases sample, but the magnitude of the differences seemed modest. Providing caloric information as miles of walking necessary to burn off a bottle of soda resulted fewer calories purchased compared with teaspoons of sugar (190 kcal vs 194 kcal; P = .09) and significantly fewer calories purchased compared with minutes of running (190 kcal vs 201 kcal; P = .009).
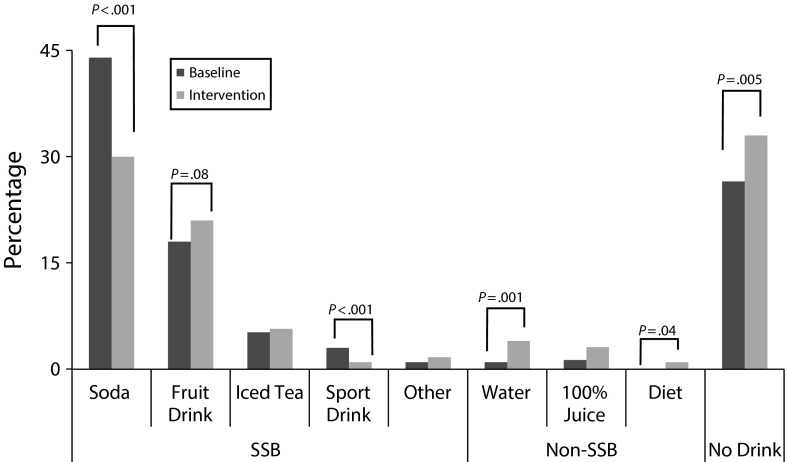
Adjusted Change in Beverage Purchases
Figure 1 illustrates the adjusted distribution of beverage purchases at baseline and the intervention period for the different types of beverage purchases. Among the SSBs, the frequency of soda purchases (44% baseline vs 30% intervention; P < .001) and sport drinks purchases (3% vs 1%; P < .001) were significantly lower after posting the signs, whereas the frequency of fruit drink purchases was higher, although not statistically significant (18% vs 21%; P = .08).
FIGURE 1—
Adjusted change in beverage purchases between baseline and intervention: Reducing Sugar-Sweetened Beverages Consumption by Providing Caloric Information; Baltimore, MD; 2012–2013.
Note. SSB = sugar-sweetened beverage. The sample for this analysis is all purchases (including purchases without beverages) from 6 corner stores in low-income, predominantly Black neighborhoods of Baltimore. These predicted probabilities were from logistic regression models in which any SSB binary outcome variable was replaced with the specific beverage type (and no drink) as the binary outcome variable. These estimates were adjusted for gender, store, time of day (before or after 4 pm), and average monthly temperature.
Among the non-SSBs, the frequency of water (1% vs 4%, P = .001) and diet soda (0.01% vs 1%; P = .04) purchases was significantly higher. Among all purchases, the frequency of not buying a beverage was significantly higher (27% vs 33%; P = .005).
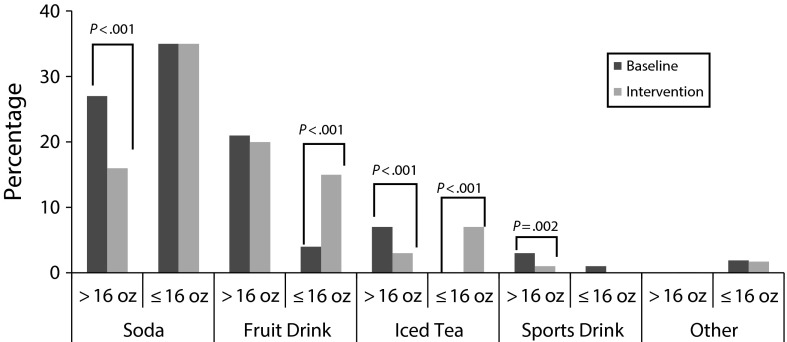
Adjusted Change in Sugar-Sweetened Beverage Purchases by Volume
Figure 2 shows the adjusted frequency of purchasing a large volume SSB (> 16 ounces) versus a small volume SSB (≤ 16 ounces) by beverage type at the baseline and the intervention period among the subsample of SSB purchases. The frequency of purchases was significantly lower for large volume sodas (27% baseline vs 16% intervention; P < .001), iced tea (7% vs 3%; P < .001), and sport drinks (3% vs 1%; P = .02). The frequency of purchases was significantly higher for low-volume fruit drinks (4% vs 15%; P < .001) and iced tea (0% vs 7%; P < .001).
FIGURE 2—
Adjusted change in sugar-sweetened beverage (SSB) purchases by volume between baseline and intervention: Reducing Sugar-Sweetened Beverages Consumption by Providing Caloric Information; Baltimore, MD; 2012–2013.
Note. These predicted probability results came from re-running the logistic regression models for the SSB subsample and replacing the outcome variable with the specific SSB type and size as the outcome variable. Estimates are adjusted for gender, store, time of day (before or after 4 pm), and average monthly temperature.
Exit Interviews
Exit interviews were conducted among one quarter of the study sample (n = 607; results not shown). Among the 35% who reported seeing the signs with caloric information, 95% reported understanding them, 59% reported believing them, and 40% reporting changing their purchase as a result of seeing them. The adjusted probability of purchasing an SSB was significantly lower among adolescents who reported seeing the signs (76% vs 94%; P < .001) and believing the signs (68% vs 94%; P < .001), and marginally more significant among adolescents who reported understanding the signs (77% vs 99%; P = .09). The adjusted probability of purchasing a large volume SSB (> 16 ounces) was significantly lower among adolescents who reported seeing the signs (32% vs 42%; P = .01). There were no differences in these responses by the type of caloric information or gender.
DISCUSSION
This study extended our earlier work that studied the impact of alternative modes of understandable caloric information on adolescent SSB purchases by examining the following: the decision to purchase any beverage or the size of beverage purchased, whether adolescents understood or believed the caloric information, the relative effectiveness of various types of caloric information, and whether exposure to caloric information had a persistent effect postintervention. Overall, we found that providing easily understandable caloric information might be an effective strategy for lowering calorie intake from SSBs among low-income Black adolescents and encouraging increased water and diet soda purchases. This intervention was associated with purchasing a smaller SSB, switching from an SSB to a beverage with no calories, or opting to not purchase a beverage, and it had a persistent effect on reducing SSB purchases for approximately 6 weeks after signs were removed (which is when the study period ended).
Regarding the type of caloric information on the signs, our results showed that providing information in the form of miles of walking to burn off a 20 ounce bottle of soda or fruit juice had a modest, but significant, effect on reducing the number of calories purchased compared with other relative information in the form of minutes of running or teaspoons of sugar.
Regarding the specific type of beverage, we observed significantly fewer purchases of soda and sport drinks (with larger decreases for soda), significantly more purchases of water and diet soda, and significantly more purchases including no beverage at all. We also observed a significant increase in small volume fruit drink purchases, which suggested that adolescents might view these beverages as a healthy alternative although they have as much added sugar as soda.
Regarding the perceptions of the signs themselves, among the one third of the sample who participated in the exit interviews, the caloric information was understandable to virtually all, believable to two thirds, and was associated with a lower probability of purchasing an SSB among those who reported seeing the signs.
The results related to a reduced quantity of SSB purchases were consistent with our previous work and another recent study that suggested that presenting caloric information in the form of a physical activity equivalent might be more persuasive to consumers than absolute calories.16,17 These findings were also consistent with research that suggested that calorie information reduces calorie ordering and consumption.30–37 However, our results were inconsistent with a body of research that generally found that absolute calorie information did not affect purchasing behavior overall31,38–40 or among low-income minority individuals,41,42 although the absolute calorie signage reduced SSB purchases in our study. Mixed findings among these other studies might be caused by several factors, including small sample sizes, short time frames, and consumer difficulties in understanding the information contained in the presentation of absolute calories.43 The results related to our exit interviews were inconsistent with this earlier work, which focused on menu labeling in chain restaurants; we found that fewer adolescents reported seeing the signs, but that the percentage of adolescents who reported that the information changed their behavior was higher.41
Future research could continue testing these and additional physical activity equivalents for caloric information among high-risk groups for obesity to understand which are the most persuasive. Conducting more extensive exit interviews to better understand how caloric information is used, why caloric information is not believable to all adolescents, and whether these factors differ among groups at high risk for obesity would be valuable. In addition, future research could examine how caloric information targeted toward adolescents influences other consumers, such as adults; in particular, whether adults perceive calories presented as physical activity equivalents differently than adolescents. Future research should also explore the persistent effect of caloric information on SSB purchases using longer follow-up periods. Future research should also examine whether adolescents view fruit drinks as a healthy alternative to soda.
Study Limitations
There were several limitations to this study worth noting. First, the generalizability of the study results was limited by our focus on urban, Black neighborhoods in 1 city and the inclusion of only 6 corner stores. Moreover, the stores that agreed to participate might be different in unobserved ways from stores that did participate. Second, the translation of calories into physical activity equivalents was based on averages for male and female adolescents aged 12 to 18 years, as obtained from the literature,44,45 which might limit generalizability. Third, although we did collect a random sample of adolescent beverage sales from each store, it was possible that adolescents who frequented a corner store were sampled more than once. This analysis was not able to account for autocorrelation (i.e., similarities between observations over time) because we could not develop a unique identifier for each study participant. However, we did include store-fixed effects in our models to mitigate concerns about any omitted variable biases resulting from unobservable characteristics correlated with both the outcomes and the stores. In addition, our study design should have reduced confounding because of demographic characteristics, taste preferences, and other fixed characteristics. Fourth, we did not have a control store; rather we used a case-crossover design, where each person and store served as their own control. Although our design allowed us to identify whether the change in SSB purchases after the intervention was greater than would be expected as a result of chance, it might not entirely control for changes over time. We did, however, include store-fixed effects to address this potential limitation. Fifth, information on calories from food purchases was not collected, so it was not possible to examine the potential shift from purchases of beverage calories to purchases of food calories. Sixth, the “minutes of running” and “miles of walking” signs were not directly comparable because they used different frames; one used time and the other used distance. As a result, the difference we observed could have been driven by how one processes minutes of doing something versus miles to do something. Finally, it was possible that the latter caloric information in each store included some carryover effects from earlier caloric information. In other words, it was possible that the washout period did not totally eliminate the effect of previously posted signs. To test whether there was a cumulative effect, we compared the percentage of purchases that were SSBs during the intervention period providing caloric information by whether that information was provided first, second, third, or fourth. We found no difference in the percentage of SSB purchases based on the timing.
Conclusions
Overall, our results indicated that providing adolescents with caloric information was associated with 3 behavioral changes to reduce calorie purchases: not making a beverage purchase, switching from an SSB to another drink with no calories or one with no added sugar, and purchasing a smaller SSB. Understandable caloric information also appeared to have had a persistent effect on reducing SSB purchases for approximately 6 weeks after it was removed (which is when the study period ended). Because of the recent implementation of the Affordable Care Act’s calorie labeling requirements46 and their potential impact on the obesity epidemic,47 it will be important to explore the most effective strategies for presenting caloric information to consumers on chain restaurant menu boards. These results might also be relevant to other local or state initiatives in various settings (convenience stores, vending machines in schools, or workplaces) that require point-of-purchase information.
Acknowledgments
This article was supported by grant #69292 from the Robert Wood Johnson Foundation through its Healthy Eating Research program.
We thank Mary Story, PhD, RD, J. Michael Oakes, PhD, and Prabhu Ponkshe for helpful comments. We thank Desmond Flagg, Brenda Campos-Spitze, Natalie Reid, Annie Rushman, and Lauren Tanz for collecting the data.
Human Participant Protection
The study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board (#2412).
References
- 1.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357(9255):505–508. doi: 10.1016/S0140-6736(00)04041-1. [DOI] [PubMed] [Google Scholar]
- 2.Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health. 2007;97(4):667–675. doi: 10.2105/AJPH.2005.083782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr. 2006;84(2):274–288. doi: 10.1093/ajcn/84.1.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ebbeling CB, Feldman HA, Chomitz VR et al. A randomized trial of sugar-sweetened beverages and adolescent body weight. N Engl J Med. 2012;367(15):1407–1416. doi: 10.1056/NEJMoa1203388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999-2010. Am J Clin Nutr. 2013;98(1):180–188. doi: 10.3945/ajcn.112.057943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988-2004. Pediatrics. 2008;121(6):e1604–1614. doi: 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 7.Gidding SS, Dennison BA, Birch LL et al. Dietary recommendations for children and adolescents: a guide for practitioners: consensus statement from the American Heart Association. Circulation. 2005;112(13):2061–2075. doi: 10.1161/CIRCULATIONAHA.105.169251. [DOI] [PubMed] [Google Scholar]
- 8.Kopelman PG. Obesity as a medical problem. Nature. 2000;404(6778):635–643. doi: 10.1038/35007508. [DOI] [PubMed] [Google Scholar]
- 9.Skelton JA, Beech BM. Attrition in paediatric weight management: a review of the literature and new directions. Obes Rev. 2011;12(5):e273–e281. doi: 10.1111/j.1467-789X.2010.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wennberg JE, Fisher ES, Goodman DC, Skinner JS, Bronner KK, Sharp SM. Hanover, NH: Dartmouth Institute of Health Policy and Clinical Practice; 2008. Tracking the care of patients with severe chronic illness: the Dartmouth Atlas of Health Care 2008. [PubMed] [Google Scholar]
- 11.Backstrand J. Fat Chance. Washington, DC: Center for the Public Interest; 1997. [Google Scholar]
- 12.Burton S, Creyer EH, Kees J, Huggins K. Attacking the obesity epidemic: the potential health benefits of providing nutrition information in restaurants. Am J Public Health. 2006;96(9):1669–1675. doi: 10.2105/AJPH.2004.054973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bassett MT, Dumanovsky T, Huang C et al. Purchasing behavior and calorie information at fast-food chains in New York City, 2007. Am J Public Health. 2008;98(8):1457–1459. doi: 10.2105/AJPH.2008.135020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verbeke W. Impact of communication on consumers’ food choices. Proc Nutr Soc. 2008;67(3):281–288. doi: 10.1017/S0029665108007179. [DOI] [PubMed] [Google Scholar]
- 15.Jacoby J, Johar GV, Morrin M. Consumer behavior: a quadrennium. Annu Rev Psychol. 1998;49:319–344. doi: 10.1146/annurev.psych.49.1.319. [DOI] [PubMed] [Google Scholar]
- 16.Dowray S, Swartz JJ, Braxton D, Viera AJ. Potential effect of physical activity based menu labels on the calorie content of selected fast food meals. Appetite. 2013;62:173–181. doi: 10.1016/j.appet.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 17.Bleich SN, Herring BJ, Flagg DD, Gary-Webb TL. Reduction in purchases of sugar-sweetened beverages among low-income Black adolescents after exposure to caloric information. Am J Public Health. 2012;102(2):329–335. doi: 10.2105/AJPH.2011.300350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Diez-Roux AV. Bringing context back into epidemiology: variables and fallacies in multilevel analysis. Am J Public Health. 1998;88(2):216–222. doi: 10.2105/ajph.88.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lando AM, Labiner-Wolfe J. Helping consumers make more healthful food choices: consumer views on modifying food labels and providing point-of-purchase nutrition information at quick-service restaurants. J Nutr Educ Behav. 2007;39(3):157–163. doi: 10.1016/j.jneb.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 20.Grunert KG, Wills JM. A review of European research on consumer response to nutrition information on food labels. J Public Health. 2007;15(5):385–399. [Google Scholar]
- 21.Guenther PM, Cleveland LE, Ingwersen LA. Questionnaire development and data collection procedures. In: Tippett KS, Cypel YS, editors. Design and Operation: The Continuing Survey of Food Intakes by Individuals and the Diet and Health Knowledge Survey, 1994–96. Washington, DC: USDA, Agricultural Research Service; 1997. [Google Scholar]
- 22.Sly DF, Arheart K, Dietz N et al. The outcome consequences of defunding the Minnesota youth tobacco-use prevention program. Prev Med. 2005;41(2):503–510. doi: 10.1016/j.ypmed.2004.11.027. [DOI] [PubMed] [Google Scholar]
- 23.Niederdeppe J, Farrelly MC, Hersey JC, Davis KC. Consequences of dramatic reductions in state tobacco control funds: Florida, 1998–2000. Tob Control. 2008;17(3):205–210. doi: 10.1136/tc.2007.024331. [DOI] [PubMed] [Google Scholar]
- 24.Maclure M, Mittleman MA. Should we use a case-crossover design? Annu Rev Public Health. 2000;21:193–221. doi: 10.1146/annurev.publhealth.21.1.193. [DOI] [PubMed] [Google Scholar]
- 25.Bader MD, Ailshire JA, Morenoff JD, House JS. Measurement of the local food environment: a comparison of existing data sources. Am J Epidemiol. 2010;171(5):609–617. doi: 10.1093/aje/kwp419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cutler DM, Glaeser EL, Shapiro JM. Why have Americans become more obese? J Econ Perspect. 2003;17(3):93–118. [Google Scholar]
- 27.Bernard HR. Research Methods in Anthropology. Lanham, MD: Altamira Press; 2005. [Google Scholar]
- 28. Food Preparation and Food Establishments. New York City Department of Health and Mental Hygiene. NYC Health Code 81.53; 2013.
- 29.StataCorp. Stata Statistical Software: Release 11. College Station, TX: StataCorp; 2009. [Google Scholar]
- 30.Harnack LJ, French SA, Oakes JM, Story MT, Jeffery RW, Rydell SA. Effects of calorie labeling and value size pricing on fast food meal choices: results from an experimental trial. Int J Behav Nutr Phys Act. 2008;5:63. doi: 10.1186/1479-5868-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Swartz JJ, Braxton D, Viera AJ. Calorie menu labeling on quick-service restaurant menus: an updated systematic review of the literature. Int J Behav Nutr Phys Act. 2011;8:135. doi: 10.1186/1479-5868-8-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu PJ, Roberto CA, Liu LJ, Brownell KD. A test of different menu labeling presentations. Appetite. 2012;59(3):770–777. doi: 10.1016/j.appet.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 33.Morley B, Scully M, Martin J, Niven P, Dixon H, Wakefield M. What types of nutrition menu labelling lead consumers to select less energy-dense fast food? An experimental study. Appetite. 2013;67:8–15. doi: 10.1016/j.appet.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 34.Temple JL, Johnson K, Recupero K, Suders H. Nutrition labels decrease energy intake in adults consuming lunch in the laboratory. J Am Diet Assoc. 2010;110(7):1094–1097. doi: 10.1016/j.jada.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 35.Roberto CA, Larsen PD, Agnew H, Baik J, Brownell KD. Evaluating the impact of menu labeling on food choices and intake. Am J Public Health. 2010;100(2):312–318. doi: 10.2105/AJPH.2009.160226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tandon PS, Wright J, Zhou C, Rogers CB, Christakis DA. Nutrition menu labeling may lead to lower-calorie restaurant meal choices for children. Pediatrics. 2010;125(2):244–248. doi: 10.1542/peds.2009-1117. [DOI] [PubMed] [Google Scholar]
- 37.Chu YH, Frongillo EA, Jones SJ, Kaye GL. Improving patrons’ meal selections through the use of point-of-selection nutrition labels. Am J Public Health. 2009;99(11):2001–2005. doi: 10.2105/AJPH.2008.153205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Harnack LJ, French SA. Effect of point-of-purchase calorie labeling on restaurant and cafeteria food choices: a review of the literature. Int J Behav Nutr Phys Act. 2008;5:51. doi: 10.1186/1479-5868-5-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vadiveloo MK, Dixon LB, Elbel B. Consumer purchasing patterns in response to calorie labeling legislation in New York City. Int J Behav Nutr Phys Act. 2011;8:51. doi: 10.1186/1479-5868-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Finkelstein EA, Strombotne KL, Chan NL, Krieger J. Mandatory menu labeling in one fast-food chain in King County, Washington. Am J Prev Med. 2011;40(2):122–127. doi: 10.1016/j.amepre.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 41.Elbel B, Kersh R, Brescoll VL, Dixon LB. Calorie labeling and food choices: a first look at the effects on low-income people in New York City. Health Aff (Millwood) 2009;28(6):w1110–w1121. doi: 10.1377/hlthaff.28.6.w1110. [DOI] [PubMed] [Google Scholar]
- 42.Elbel B, Gyamfi J, Kersh R. Child and adolescent fast-food choice and the influence of calorie labeling: a natural experiment. Int J Obes (Lond) 2011;35(4):493–500. doi: 10.1038/ijo.2011.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Elbel B. Consumer estimation of recommended and actual calories at fast food restaurants. Obesity (Silver Spring) 2011;19(10):1971–1978. doi: 10.1038/oby.2011.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schofield WN, Schofield C, James WPT. Basal metabolic rate: review and prediction, together with an annotated bibliography of source material. Human Nutr Clin Nutr. 1985;39C(suppl 1):5–41. [PubMed] [Google Scholar]
- 45.Ainsworth BE, Haskell WL, Herrmann SD et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 46. Patient Protection and Affordable Care Act. HR 3590. Sec. 4205. March 23, 2010.
- 47.Kuo T, Jarosz CJ, Simon P, Fielding JE. Menu labeling as a potential strategy for combating the obesity epidemic: a health impact assessment. Am J Public Health. 2009;99(9):1680–1686. doi: 10.2105/AJPH.2008.153023. [DOI] [PMC free article] [PubMed] [Google Scholar]