The endocannabinoids have emerged as important intercellular signals in the nervous system. The fatty acid amide arachidonylethanolamide (anandamide) is the prototypical endocannabinoid, i.e., an endogenous ligand of the G protein-coupled cannabinoid receptor in the brain, CB1, which binds the main psychoactive component of marijuana and other derivatives of Cannabis sativa (1). After a rise in intracellular calcium or activation of certain neurotransmitter receptors, endocannabinoids are synthesized by cleavage of phospholipid precursors that are present in cellular membranes (2). They often act as retrograde messengers, emanating from morphologically undifferentiated regions of postsynaptic principal cells and traveling backwards across synapses, where they transiently inhibit the release of either the inhibitory neurotransmitter γ-aminobutyric acid (GABA) or the excitatory transmitter glutamate (see Fig. 1 and ref. 3 for a review). This powerful influence on synaptic transmission enables the endocannabinoids to help regulate behaviors, such as feeding (4), fear (5), and anxiety (6).
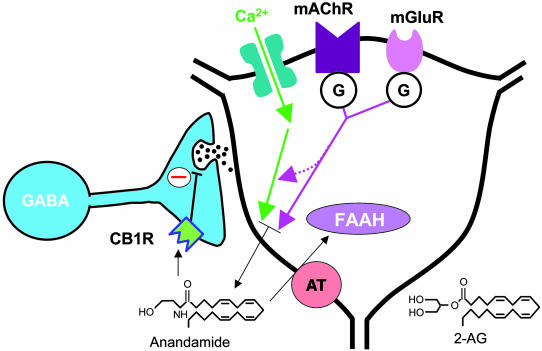
Fig. 1.
Retrograde signaling by endocannabinoids. The endocannabinoids anandamide and 2-AG are synthesized in postsynaptic target cells such as hippocampal pyramidal cells (right). Synthesis is initiated by calcium influx through voltage-gated calcium channels, or by the activation of G protein-coupled neurotransmitter receptors, including type I metabotropic glutamate receptors (mGluR) or muscarinic acetylcholine receptors (mAChR) (3). The endocannabinoids gain access to the extracellular space and activate CB1 cannabinoid receptors found concentrated on certain nerve terminals, e.g., of cholecystokinin-containing GABAergic interneurons in hippocampus (2). CB1 activation causes presynaptic inhibition of GABA or glutamate release by inhibiting calcium channels, interfering with vesicle release, and activating potassium channels. The endocannabinoids are taken up into postsynaptic or presynaptic cells by the anandamide transporter (AT). The degradative enzyme FAAH is present in postsynaptic cells, and monoglyceride lipase (not shown), which degrades 2-AG, is found in presynaptic terminals (2).
As is true of other intercellular messengers, the time course and magnitude of endocannabinoid actions are strongly influenced by their lifetime in the extracellular space. Anandamide is enzymatically degraded by fatty acid amide hydrolase (FAAH), but FAAH is an intracellular enzyme, so anandamide must be internalized to be hydrolyzed (7). Most evidence has pointed to a sodium- and energy-independent transporter operating by facilitated diffusion as the endocannabinoid uptake mechanism (8). Support for this model included saturability of the uptake process, its selectivity for certain fatty acids, and its inhibition by anandamide analogs. However, the topic has been controversial (9). It has been suggested that passive diffusion alone is sufficient for anandamide uptake, with intracellular hydrolysis by FAAH maintaining the concentration gradient (10, 11). An article by Fegley et al. (12) in this issue of PNAS neatly disposes of the major components of this model and, in addition, introduces a new transport inhibitor that could serve as a basis for therapeutic drug development, thereby adding strong support for the transporter hypothesis.
The Endocannabinoid Systems
Anandamide and 2-arachidonyl glycerol (2-AG) are the main endocannabinoids in the brain (2). Once released, they can activate CB1, which, as the most abundant G protein-coupled receptor in the brain, is widely, although heterogeneously, distributed on particular axon terminals (2). (CB2 receptors are found in the periphery, often in association with cells of the immune system.) Where CB1 receptors are found on inhibitory axons, endocannabinoids mediate depolarization-induced suppression of inhibition (13, 14), and, where they are found on excitatory axons, they mediate depolarization-induced suppression of excitation (15). Endocannabinoids typically do not travel far from their source, usually <1 μm, although distances up to 10 μm are possible under some conditions (e.g., refs. 13 and 16). They generally activate receptors on axon terminals that synapse on the releasing cell, thereby serving as spatially and temporally restricted messengers.
Anandamide Uptake
A key challenge to the anandamide transporter hypothesis arose from the observation that the initial rate of anandamide accumulation in certain cell lines is not saturable although accumulation at later times is (11). Moreover, inhibitors of FAAH slowed anandamide uptake (10), and, conversely, in some cells, inhibitors of anandamide transport can inhibit FAAH (11). This constellation of effects is consistent with a hypothesis that passive anandamide influx is driven by a transmembrane anandamide gradient that is maintained by the intracellular action of FAAH (which would keep intracellular concentrations low). In testing central tenets of this idea in primary neuronal cultures, Fegley et al. (12) find that anandamide uptake is the same in wild-type and FAAH–/– mutant mice, and that putative anandamide transporter blockers continue to slow the rate of uptake in the FAAH–/– mice. Thus, the action of FAAH cannot be responsible for maintaining the driving force for anandamide influx. They also constructed a novel anandamide analog, AM1172, that is not a substrate for FAAH and does not alter its activity. AM1172 was as effective in reducing anandamide uptake as were other transporter inhibitors, in both wild-type and FAAH–/– mice, which removes the possibility that interference with FAAH explained the decrease in uptake efficiency. Uptake by transporter is the best explanation for the movements of endocannabinoids across cellular membranes in neurons.
This work (12) eliminates the major aspects of the competing hypothesis and supports the existence of an anandamide transporter. There are additional reasons to think that a transporter must be real. The most persuasive of these comes from an electrophysiological bioassay: directly loading anandamide into a neuron through a whole-cell recording pipette quickly leads to anandamide efflux, activation of CB1 receptors on synapsing axonal terminals, and inhibition of synaptic transmission (16). Importantly, the anandamide efflux is prevented by a transporter blocker, despite the persistence of the (outward) anandamide gradient (17). Note also that, if the transporter blocker behaved as an FAAH inhibitor, the anandamide efflux should, if anything, have been greater (not less), so this experiment presents double difficulty for the passive diffusion model. Clearly, there is strong support for the facilitated diffusion carrier model although isolation of this elusive molecule is required to make the case air-tight.
Open Issues and Future Prospects
Unfortunately, even molecular cloning of the transporter will probably not entirely clarify all of the issues surrounding endocannabinoid handling. Neurons concentrate anandamide that is experimentally added to the extracellular environment, building up internal concentrations as much as three orders of magnitude greater than the external levels. A likely scenario is that the internal anandamide is not free but is either sequestered or bound to some site, perhaps a protein (9). Anandamide sequestration could help maintain the gradient for anandamide influx, and, if it is specific and saturable, then it could account for some of the effects attributed to the transporter. Hence, elucidation of the concentrating mechanisms is another pressing task.
Fegley et al.'s work supports the existence of an anandamide transporter.
Is the endocannabinoid uptake mechanism a physiologically important issue? It may be, for several reasons. On analogy with FAAH inhibitors, which cause a variety of physiological effects because they increase the overall levels of anandamide (2, 7), blockers of the anandamide transport could have similar effects. They should prolong the actions of released anandamide and, if anandamide is continually released and recycled at low levels, might induce an anandamide “tone.” Transporter blockers would also enhance the actions of exogenous cannabinoid drugs that are transporter substrates. Such actions are of potential therapeutic utility. 2-AG also is transported into cells, and, because 2-AG rather than anandamide may be the chief endocannabinoid in some brain regions, attention will have to be devoted specifically to its uptake, which may not be the same as that of anandamide (2).
A New Role for the Transporter
Recent discoveries have added an unexpected twist to the story of endocannabinoid transport. Brief synaptic stimulation of principal neurons in the striatum (16, 18) or nucleus accumbens (19) can cause a long-term depression (LTD, lasting many tens of minutes) of the same synapses by a presynaptic mechanism. LTD is a form of functional synaptic plasticity that is associated with cellular learning and memory processes, and it was therefore quite significant when this type of LTD was shown to be mediated by endocannabinoids released from the principal neurons (16, 19). Normally, brief stimulation would produce only a brief bout of endocannabinoid production and release. However, after a similar observation by Chevaleyre and Castillo (20) in the hippocampus, Ronesi et al. (17) reported that striatal LTD required activation of the presynaptic cannabinoid receptors that lasted at least 5 min, after which time LTD became independent of them. This lengthy period posed a problem. Given the speed with which endocannabinoids are cleared from the extracellular space, how could prolonged cannabinoid receptor activation occur? The answer, apparently, is that persistent cannabinoid receptor activation demands a persistent supply of endocannabinoids. Ronesi et al. (17) found that anandamide transport blockers prevent LTD induction when they are infused into the postsynaptic cell. It seems that, for many minutes after the appropriate stimulation, endocannabinoids can be transported out of the postsynaptic cells by the same mechanism that transports them in. How this transporter-dependent efflux is initiated and maintained, as well as the presynaptic mechanisms of LTD induction, remains to be elucidated. Nevertheless, the crucial role that the anandamide transporter plays in LTD ensures that it will continue to serve as the focus of much interest and attention in the future.
See companion article on page 8756.
References
- 1.Devane, W. A., Hanus, L., Breuer, A., Pertwee, R. G., Stevenson, L. A., Griffin, G., Gibson, D., Mandelbaum, A., Etinger, A. & Mechoulam, R. (1992) Science 258, 1946–1949. [DOI] [PubMed] [Google Scholar]
- 2.Freund, T. F., Katona, I. & Piomelli, D. (2003) Physiol. Rev. 83, 1017–1066. [DOI] [PubMed] [Google Scholar]
- 3.Alger, B. E. (2002) Prog. Neurobiol. 68, 247–286. [DOI] [PubMed] [Google Scholar]
- 4.Di Marzo, V., Goparaju, S. K., Wang, L., Liu, J., Batkai, S., Jarai, Z., Fezza, F., Miura, G. I., Palmiter, R. D., Sugiura, T., et al. (2001) Nature 410, 822–825. [DOI] [PubMed] [Google Scholar]
- 5.Marsicano, G., Wotjak, C. T., Azad, S. C., Bisogno, T., Rammes, G., Cascio, M. G., Hermann, H., Tang, J., Hofmann, C., Zieglgansberger, W., et al. (2002) Nature 418, 530–534. [DOI] [PubMed] [Google Scholar]
- 6.Kathuria, S., Gaetani, S., Fegley, D., Valino, F., Duranti, A., Tontini, A., Mor, M., Tarzia, G., La Rana, G., Calignano, A., et al. (2003) Nat. Med. 9, 76–81. [DOI] [PubMed] [Google Scholar]
- 7.Bisogno, T., De Petrocellis, L. & Di Marzo, V. (2002) Curr. Pharm. Des. 8, 125–133. [DOI] [PubMed] [Google Scholar]
- 8.Giuffrida, A., Beltramo, M. & Piomelli, D. (2001) J. Pharmacol. Exp. Ther. 298, 7–14. [PubMed] [Google Scholar]
- 9.Hillard, C. J. & Jarrahian, A. (2003) Br. J. Pharmacol. 140, 802–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deutsch, D. G., Glaser, S. T., Howell, J. M., Kunz, J. S., Puffenbarger, R. A., Hillard, C. J. & Abumrad, N. (2001) J. Biol. Chem. 276, 6967–6973. [DOI] [PubMed] [Google Scholar]
- 11.Glaser, S. T., Abumrad, N. A., Fatade, F., Kaczocha, M., Studholme, K. M. & Deutsch, D. G. (2003) Proc. Natl. Acad. Sci. USA 100, 4269–4274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fegley, D., Kathuria, S., Mercier, R., Li, C., Goutopoulos, A., Makriyannis, A. & Piomelli, D. (2004) Proc. Natl. Acad. Sci. USA 101, 8756–8761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson, R. I. & Nicoll, R. A. (2001) Nature 410, 588–592. [DOI] [PubMed] [Google Scholar]
- 14.Ohno-Shosaku, T., Maejima, T. & Kano, M. (2001) Neuron 29, 729–738. [DOI] [PubMed] [Google Scholar]
- 15.Kreitzer, A. C. & Regehr, W. G. (2001) Neuron 29, 717–727. [DOI] [PubMed] [Google Scholar]
- 16.Gerdeman, G. L., Ronesi, J. & Lovinger, D. M. (2002) Nat. Neurosci. 5, 446–451. [DOI] [PubMed] [Google Scholar]
- 17.Ronesi, J., Gerdeman, G. L. & Lovinger, D. M. (2004) J. Neurosci. 24, 1673–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Calabresi, P., Maj, R., Pisani, A., Mercuri, N. B. & Bernardi, G. (1992) J. Neurosci. 12, 4224–4233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robbe, D., Kopf, M., Remaury, A., Bockaert, J. & Manzoni, O. J. (2002) Proc. Natl. Acad. Sci. USA 99, 8384–8388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chevaleyre, V. & Castillo, P. E. (2003) Neuron 38, 461–472. [DOI] [PubMed] [Google Scholar]