Abstract
Linear growth failure is the most common form of undernutrition globally. With an estimated 165 million children below 5 years of age affected, stunting has been identified as a major public health priority, and there are ambitious targets to reduce the prevalence of stunting by 40% between 2010 and 2025. We view this condition as a ‘stunting syndrome’ in which multiple pathological changes marked by linear growth retardation in early life are associated with increased morbidity and mortality, reduced physical, neurodevelopmental and economic capacity and an elevated risk of metabolic disease into adulthood. Stunting is a cyclical process because women who were themselves stunted in childhood tend to have stunted offspring, creating an intergenerational cycle of poverty and reduced human capital that is difficult to break. In this review, the mechanisms underlying linear growth failure at different ages are described, the short-, medium- and long-term consequences of stunting are discussed, and the evidence for windows of opportunity during the life cycle to target interventions at the stunting syndrome are evaluated.
Keywords: Stunting, Malnutrition, Mortality, Neurodevelopment, Infections
INTRODUCTION
Linear growth failure in childhood is the most prevalent form of undernutrition globally.1 An estimated 165 million children under 5 years of age are stunted, with a height-for-age Z-score (HAZ) below −2 (i.e. more than two standard deviations below the population median), but a larger number of children with HAZ >−2 still have inadequate linear growth and are therefore experiencing stunting.1 Undernutrition underlies 45% of all child deaths among children <5 years,2 although mortality has been described as the ‘tip of the iceberg’ of malnutrition.3 Stunting more pervasively hinders developmental potential and human capital of entire societies due to its longer-term impact on cognitive function and adult economic productivity; it is therefore considered the best surrogate marker of child health inequalities.4,5
After many years of neglect, stunting has now been identified as a major global health priority.6 Ambitious World Health Assembly targets aim to reduce stunting by 40% between 2010 and 2025.7 Whilst impressive progress has been made in Asia, with a decline in the proportion of stunted children from 49% to 28% between 1990 and 2010, this is still the continent with the most stunted children globally (approximately 100 million); in Africa, stunting prevalence has remained stagnant around 40% and, owing to population growth, the absolute number of stunted children is increasing.8 Millennium Development Goal 1 (MDG 1), which focuses on eradicating extreme hunger and poverty, uses underweight rather than stunting as its target (http://www.un.org/millenniumgoals/). Weight is more frequently used to monitor growth than is height, because of ease of measurement; however, underweight (low weight-for-age) does not distinguish between stunting (low height-for-age) and wasting (low weight-for-height). In settings where stunting is highly prevalent and wasting is rare, underweight therefore underestimates the burden of malnutrition.9–11 Overall, developing countries have <5% chance of achieving MDG 1 (reducing the proportion of children with WAZ<−2 by half between 1990 and 2015), although 61 of 141 countries are estimated to have a 50–100% chance of success.12 Even regions such as the Caribbean and Latin America which are on target to reach MDG 1 when measured as WAZ would not achieve this target if using HAZ as the indicator.13
Although usually described separately, stunting, underweight and wasting frequently co-exist and children with multiple measures of anthropometric failure have a compounded risk of morbidity and mortality.14,15 For example, analysis of data on 53,767 children in Africa, Asia and Latin America demonstrated that mortality in those who were stunted and underweight was more than three times greater than in well nourished children [HR 3.4 (95% CI 2.6–4.3)]; this risk rose to >12-fold [HR 12.3 (7.7- 19.6)] in children who were stunted, underweight and wasted.15 Thus, although stunting and wasting have tended to be viewed separately, there is a growing impetus to consider both conditions together.16 Weight-for-height tends to reflect more short-term inadequacy of dietary intake or utilization; the effectiveness of therapeutic feeding for wasted children is well established.17 By contrast, the mechanisms underlying linear growth failure and interventions to prevent or ameliorate stunting are less clearly defined.16
THE STUNTING SYNDROME
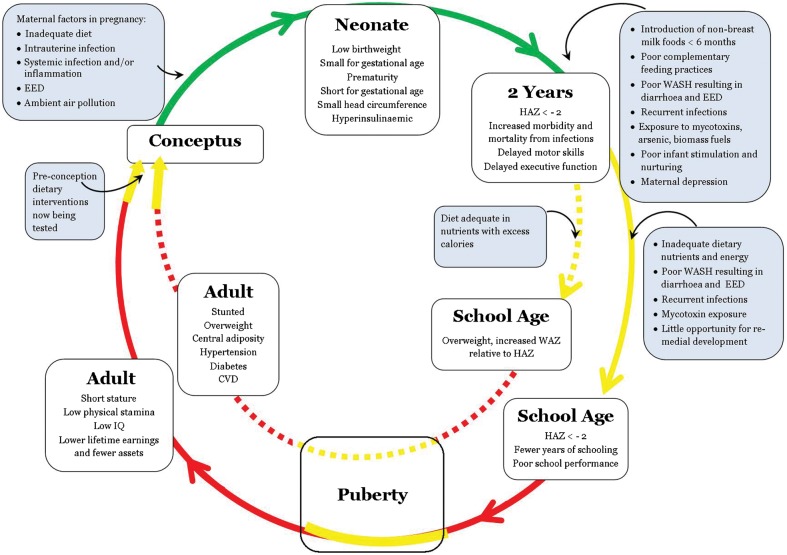
Although stunted children are identified by comparing their height to an age- and sex-matched reference population, short stature is not usually in itself problematic. Instead, we view this condition as a ‘stunting syndrome’ in which multiple pathological changes marked by linear growth retardation increase morbidity and mortality and reduce physical, neurodevelopmental and economic capacity. The short-, medium- and long-term sequelae of stunting, summarised in Figure 1, are discussed in detail later. Stunting is a cyclical process because women who were themselves stunted in childhood tend to have stunted offspring, creating an intergenerational cycle of poverty and reduced human capital that is difficult to break,18 although potential windows of opportunity have been identified (Fig. 1).
Figure 1.
The stunting syndrome. The green pathway denotes the period between conception and 2 years (‘the first 1000 days’) when stunting and probably all associated pathology are most responsive to, or preventable by, interventions. The yellow pathway denotes periods between age 2 years and mid-childhood and during the adolescent growth spurt when some catch-up in linear growth may occur, though effects during these periods on other components of the stunting syndrome (e.g. cognition and immune function) are less clear. The short yellow pathway before Conceptus reflects evidence that dietary interventions targeting stunted women during the pre-conception period improve birth outcomes. The red pathway denotes periods when the stunting syndrome appears unresponsive to interventions. Blue boxes list age-specific causative or aggravating factors. White boxes describe common age-specific outcomes. Between 2 years and adulthood, the pathways diverge to denote: dashed line, a stunted child whose environment becomes more affluent with abundant access to food, causing excessive weight gain; solid line: a stunted child whose environment remains resource-constrained/food insecure. Please see the text for citations
DETERMINANTS OF HEALTHY GROWTH
There are four interlinked phases of growth during the life-course: fetal, infant, childhood and pubertal, each governed by different regulatory mechanisms. A study of healthy children who were measured frequently during the first 21 months of life demonstrated that growth is an episodic phenomenon, with long periods of stasis (between 2 and 63 days) punctuated by short phases of saltation (growth spurts), so that there is no growth during 90–95% of healthy infancy.19 Although height is a highly heritable trait, with over 200 genes identified in genome-wide association studies, together they explain only about 10% of the variation in adult height.20,21 Children from different geographical areas grow at a remarkably similar rate during fetal life22 and the first few years of postnatal life23–25 if born to mothers whose nutritional and health needs are met and if raised in unconstrained conditions. Environmental factors such as maternal nutritional status, feeding practices, hygiene and sanitation, frequency of infections and access to healthcare are therefore the major determinants of growth in the first 2 years of life.18
Studies of variation in stunting prevalence across countries26 and between different populations within countries27,28 demonstrate the importance of socio-economic factors. Stunting prevalence is therefore a good indicator of inequalities in human development;29 across 80 countries, those with a high prevalence of stunting tended also to have larger socio-economic inequalities in children with stunting.30 An analysis for the Lancet Nutrition Series incorporating data from 79 countries showed that stunting prevalence was 2.47 (range 1.00–7.64) times higher in the poorest than in the richest quintile.2 In China, where there was marked economic development between 1975 and 2010, there was a parallel improvement in the growth of children and adolescents; height showed a strong positive correlation with GDP per capita (r 0.90, P<0.0001) and with urbanisation (r 0.92, P<0.0001), and a negative correlation with the under-5 mortality rate (r −0.95, P<0.0001).31 Using data from 7630 mother–child pairs enrolled in the COHORTS study in Brazil, Guatemala, Philippines, India and South Africa, children on average had better heights than their mothers owing to secular trends arising from improvements in economic and environmental conditions over time.32 Improvements in growth are seen when people migrate from poor nations to countries with better socio-economic conditions.18
THE TIMING OF GROWTH FALTERING
Stunting begins in utero and continues for at least the first 2 years of postnatal life; the period from conception to a child’s second birthday (the first thousand days) has therefore been identified as the most critical window of opportunity for interventions (www.thousanddays.org). The average length-for-age Z-score among newborns in developing countries is approximately −0.5 and continues to decline after birth to reach a nadir of around −2.0 by 18–24 months of age.33 Upon publication of new WHO growth standards in 2006,34 it became apparent that linear growth faltering in developing countries occurs sooner after birth that had been appreciated using prior National Center for Health Statistics (NCHS) data,35 which were based on the growth of predominantly formula-fed infants.36 Although stunting at a population level follows the trajectory described above, there are widespread between-child differences in stunting patterns when individual child growth curves are examined (Prendergast et al., unpublished data). There are some difficulties in interpreting the patterns of long-term linear growth from published data, because many studies are cross-sectional rather than longitudinal; most focus on children <5 years of age; and height is generally presented as Z-scores, which can be problematic when used to describe growth over time, as discussed later. Across multiple countries in sub-Saharan Africa it has been shown that boys are more likely to be stunted than girls (odds ratio 1.16, 95% CI 1.12–1.20) for reasons which remain unclear.37
THE PATHOGENESIS OF STUNTING
Despite the high global prevalence of stunting, the pathogenesis underlying linear growth failure is surprisingly poorly understood. For this reason, the most tractable pathways for effective interventions to promote healthy growth remain unclear,38 and no research study has ever normalised linear growth among children living in developing countries. From epidemiological studies it is apparent that suboptimal breastfeeding and complementary feeding practices, recurrent infections and micronutrient deficiencies are important proximal determinants of stunting.2,39 Linear growth failure also occurs within a complex interplay of more distal community and societal factors, such as access to healthcare and education, political stability, urbanisation, population density and social support networks, which have been captured in the WHO Conceptual Framework on Childhood Stunting, as recently reviewed.40 Below we review the current understanding of growth failure across the life-course and try to identify potential windows of opportunity for interventions (Fig. 1).
Antenatal period
Fetal growth is governed by complex interactions between maternal nutritional status, endocrine and metabolic signals and placental development. Newborn size is therefore a reflection of the intrauterine environment; prevalence of low birthweight (<2.5 kg) is approximately six times higher in developing compared to developed countries.41 The INTERGROWTH-21st Project, a population-based study of fetal growth across eight countries, showed that newborn length was very similar across sites among affluent, healthy, educated women.22 Low birthweight babies include those born too soon (preterm), too small (small for gestational age, SGA), or both. In 2010, 27% of liveborn infants globally were SGA and almost 3 million infants were born preterm and SGA;42 risks of poor growth43 and mortality44 are compounded among those born preterm-SGA. Using data from 19 birth cohorts, Christian et al. showed that, relative to infants born appropriate for gestational age and at term, the risk of postnatal stunting increased markedly among infants born preterm [OR 1.93 (95% CI 1.71–2.18)], SGA [2.43 (2.22–2.66)] and SGA-preterm [4.51 (3.42–5.93)].43 Overall, they estimated that 20% of stunting has in utero origins. In some settings, antenatal determinants of stunting appear to be even more important than postnatal determinants.45,46
Maternal undernutrition contributes to an estimated 20% of maternal deaths and increases the risk of adverse pregnancy outcomes, childhood mortality and stunting.47 Short maternal stature, low body mass index and poor weight gain during pregnancy are the major indices associated with low birthweight.41,48 Early pregnancy during adolescence, when mothers are themselves still growing, increases the risk of further maternal stunting49,50 and leads to adverse obstetric outcomes.51,52 Closely spaced births also increase nutritional demands on the mother.53 Maternal height is associated with size at birth and with postnatal stunting,32,54–57 which compounds the intergenerational cycle of stunting (Fig. 1). Birthweight and length are themselves related to subsequent growth in childhood. A longitudinal analysis of data from five birth cohorts32 which used a measure of conditional height across the life-course to account for the colinearity of multiple growth measures showed that maternal height was related to offspring height at all ages (correlations ranging from 0.15 to 0.55, P<0.001) and maternal height was strongly associated with stunting prevalence at 2 years, similar to findings from previous cross-sectional studies.54,56,57 The largest study to date55 incorporating data from 109 demographic and health surveys across 54 countries showed that maternal height was inversely associated with mortality, underweight and stunting during infancy and childhood.
Given these strong intergenerational effects, the concept of stunted families rather than stunted children has been proposed,58 particularly since paternal nutritional status can also influence childhood stunting.59 It has been argued that these intergenerational influences on health have been ignored in setting the Millennium Development Goals, which are unlikely to be attained if maternal health is not addressed.60 Since infants are entirely dependent on their mother for nutrition during the first 500 days of life,61 several trials have focused on improving maternal nutritional status. Prenatal multiple micronutrients62 and provision of balanced energy and protein to mothers63 reduce SGA by 9% and 31%, respectively. Daily iron supplementation during pregnancy reduces low birthweight by 20%64 but zinc supplementation has no significant effect on birthweight.65 Calcium supplementation in pregnant women increases birthweight by 85 g (95% CI 37–133) compared with controls,66 and three trials of vitamin D in pregnancy showed a borderline significant effect on low birthweight (relative risk 0.48, 95% CI 0.23–1.01).67
Various human and animal studies have shown that maternal diet can mediate epigenetic changes in the fetus.68–70 In a Gambian trial of multiple micronutrient supplementation during the peri-conception period, epigenetic changes were seen in several differentially methylated regions which govern growth or immune function.71,72 Prenatal interventions can therefore have an impact on postnatal growth,73–76 as was shown in the MINIMAT trial in Bangladesh76 in which early food supplementation during pregnancy reduced postnatal stunting in boys (but not girls), consistent with a fetal programming effect; however, not all antenatal interventions have demonstrated a long-term effect.73,77,78
Birth to 6 months
Healthy infants experience maximal growth velocity between birth and 6 months of age. Furthermore, the first few months of life appear particularly critical for long-term neurodevelopment.79 When linear growth among infants in developing countries was evaluated using 2006 WHO growth standards, the prevalence of stunting in the first half of infancy doubled compared to prior estimates;80 in some countries, such as India, 20% of infants are stunted before 6 months of age.81,82 There is therefore an increasing appreciation of undernutrition in infants under 6 months, who are often excluded from nutrition surveys and marginalised in nutrition programmes,83 and a realisation that interventions need to be targeted earlier than was previously appreciated.
Exclusive breastfeeding (EBF) for the first 6 months has been recommended by WHO since 2001.84 Although the benefits of EBF for reduced morbidity and mortality47 and improved cognition85 are clear, evidence for an effect on linear growth is surprisingly weak.86 Promotion of EBF is effective at increasing EBF rates,86 but in a cluster-randomised trial of EBF promotion in three African countries, increased rates of EBF were not associated with improved HAZ scores at 6 months.87 In a secondary data analysis of national survey data from India, even among infants categorized as practicing EBF, stunting prevalence was 21% by 6 months, although the definition of EBF was based only on a 24-hour recall period.81 Growth failure that is continuous from fetal life through the first 6 months of postnatal life suggests the existence of common factors, which have not been well defined.88 In a study of Zimbabwean mother–infant pairs, there was evidence of chronic inflammation very early in life (by 6 weeks of age). Levels of inflammatory markers (e.g. CRP) were persistently higher in stunted than in non-stunted infants, and were associated with the level of maternal inflammation at birth, suggesting one potential common mechanism linking antenatal and postnatal growth failure.89
6–24 months of age
The period from 6 to 24 months of age is one of the most critical periods for linear growth;90 it is also the time of peak stunting prevalence in developing countries, due to high demand for nutrients coupled with limited quality and quantity of complementary foods.91 Complementary feeding refers to the timely introduction of safe and nutritious foods in addition to continued breastfeeding;92 the majority of stunting interventions have been targeted at improving infant and young child feeding (IYCF) practices, which are known to be poor in many settings.93 WHO has developed a set of IYCF indicators to evaluate feeding practices; although in some studies these show associations with stunting,94 in others they have been found to lack sensitivity and specificity.95
Interventions to improve IYCF have generally focused on nutrition counselling, providing complementary food with or without micronutrients, and increasing energy density of complementary foods through simple technology.91 A meta-analysis of 42 studies showed a modest impact of complementary feeding interventions; the best improvement in linear growth was around +0.7 gain in HAZ, which is around one-third of the average deficit.91 Generally, studies providing complementary foods in food-insecure regions showed some benefit; micronutrient fortification alone showed little or no impact on growth. Complementary feeding education improves linear growth, and leads to declines in stunting among food-insecure populations, but effect sizes are modest.96 Community-based supplementary feeding (i.e. giving additional food beyond the normal home diet) has a limited evidence base; the only impact on length was seen in children below 12 months of age in two trials.97
Lipid-based nutrient supplements (LNS), which are micronutrient-fortified ready-to-use products, have been used during the complementary feeding period in several trials. LNS showed a significant impact on linear growth in studies from Ghana,98 Congo99 and Haiti100 but not in two trials from Malawi.101,102 Another Malawian study103 showed an impact of LNS on severe stunting when provided to 6-month-old infants for 1 year, but not during a short 12 week intervention;104 the effect was sustained up to 3 years of age,105 although, of note, there was no control group in these trials. Taken together, despite differences in treatment duration, comparator groups, primary outcomes (use of absolute HAZ score vs proportion stunted) and length of follow-up, there is some evidence from trials for a small but measurable effect of LNS on linear growth.
Deficiencies of vitamin A, zinc, iron and iodine are common,47 and multiple micronutrient deficiencies are often found in the same child,106 affecting many aspects of physiology, including neural and immune function. Globally, two billion people are at risk of micronutrient deficiency, which has been termed ‘hidden hunger’ due to its impact on health and human capital.107 A systematic review of micronutrient powders108 found relatively few studies which evaluated growth; none suggested benefit and there was increased diarrhoea in some children taking micronutrient powders. An estimated 17.3% (95% CI 15.9–18.8) of the global population is at risk of zinc deficiency2 and country-specific prevalence of inadequate zinc intake correlated with stunting prevalence in 138 low- and middle-income countries (r 0.48, P<0.001).109 Daily zinc (10 mg/day) for 24 weeks leads to a mean (SD) height gain of approximately 0.38 cm (0.25).110 Studies investigating the impact of vitamin A on growth have reported mixed results.111–114
Several decades ago, detailed longitudinal studies in Guatemala showed that recurrent infections can impair growth, particularly during the second half of infancy;115 subsequent studies have confirmed this observation.90,116–119 However, there is a bidirectional relationship between infections and malnutrition; several studies show that malnourished children have an increased frequency, duration and severity of infections.116,120–123 It can therefore be difficult to distinguish cause and effect, although animal models provide a useful system to explore these interactions. Mice experimentally infected with Cryptosporidium, entero-aggregative Escherichia coli or Giardia lamblia develop enteropathy and growth impairment; when they are malnourished, they have a higher pathogen load and more severe enteropathy.124–127
Stunting and parasitic infections overlap geographically, and several studies have explored associations between them. Studies conducted over a 25-year period variously reported that malaria was associated with an increased risk of stunting,128–132 a decreased risk133 or no association;134–137 methodological differences, confounding and the possibility of reverse causality made it difficult to interpret these conflicting findings. A study that used Mendelian randomisation to explore associations between malaria and stunting has helped to clarify these associations.138 Children with sickle cell trait are asymptomatic but protected from malaria; using matching to control for unmeasured confounding, the authors showed a causal effect of malaria on stunting, since sickle cell trait can only influence stunting through its effect on malaria. Intestinal helminths affect two billion people worldwide and may affect nutritional status through reduced digestion and absorption, chronic inflammation and loss of nutrients. However, as for malaria, the impact of helminths on stunting is difficult to assess because of confounding and the possibility of reverse causality in published studies.139–140 Polyparasitism is common and is associated with adverse child health outcomes;141–143 there is a growing appreciation of the burden of helminths in pre-school children144–147 in whom infection may have the greatest impact on growth and development.148
Diarrhoea is one of the most frequent infections in childhood, particularly in conditions of poor sanitation and hygiene, although early studies varied in their conclusions as to whether diarrhoea did117,149,150 or did not116,151 affect stunting. Effects of diarrhoea may be short term152 because catch-up growth can occur between episodes.153 In an analysis of data from nine community-based studies with daily diarrhoea data and longitudinal anthopometric measurements, the odds of stunting by 24 months increased multiplicatively with each episode of diarrhoea; overall, 25% of stunting was attributed to five or more episodes of diarrhoea.154 In a more recent study of seven longitudinal infant cohorts, cumulative diarrhoeal burden had a smaller but measurable effect on linear growth; a child with the typical diarrhoea burden (equivalent to 23 days per year) was 0.38 cm shorter at 2 years of age than a child without diarrhoea.155
It is increasingly apparent that subclinical infection with enteric pathogens is common, even in the absence of diarrhoea.156 In conditions of poverty, where children experience frequent exposure to enteric pathogens due to faeco-oral transmission, a population shift in gut structure and function occurs.157,158 This subclinical pathology, characterised by villous atrophy and chronic inflammation of the small intestine, has been termed environmental enteric dysfunction (EED), and is associated with modest malabsorption and increased intestinal permeability.159 Even mild malabsorption may be important in the context of a marginal diet and rapid growth, and permeability enables translocation of microbial products from the lumen of the gut to the systemic circulation, where they can trigger chronic inflammation, which suppresses IGF-1.89,160 Early studies from The Gambia161–163 and elsewhere164,165 confirmed that abnormal intestinal permeability is common; linear growth in Gambian infants was inversely related to permeability.166 More recent studies89,167–169 and reviews159,160,170,171 have refocused attention on the plausible links between gut inflammation and stunting; given its chronic nature, it has been argued that EED may be a more important pathway to stunting than is diarrhoea.160 We therefore view stunting as an inflammatory disease arising, in part, from primary gut pathology. Since gut damage also occurs with recurrent (especially persistent) diarrhoea, severe acute malnutrition, HIV infection and micronutrient deficiencies, there are multiple overlapping causes of enteropathy in settings of poverty which may exacerbate the growth failure arising from EED.171
In the last few years, studies using next-generation sequencing have begun to characterise the composition and function of the intestinal microbiota during malnutrition (recently reviewed by Ahmed et al.172). Assembly of the microbiota occurs over the first 3 years of life,173 with a founding population acquired from the mother and subsequent composition shaped by environmental influences, including the diet.174–176 The microbiota has important roles in metabolism of macro- and micronutrients, immune development, integrity of the intestinal barrier and defence against enteric pathogens.172 A study of Malawian twin pairs discordant for kwashiorkor highlighted the importance of the gut microbiome (the genes expressed by the microbiota) in malnutrition.177 Kwashiorkor was characterised by a functionally immature microbiome, which matured during therapeutic feeding (with enrichment of potentially beneficial organisms, such as Bifidobacteria and Lactobacillus) but was not sustained once therapeutic feeding was stopped. In a subsequent study from Bangladesh,178 sequencing of monthly faecal samples from 50 children with healthy growth enabled ‘microbiota-for-age’ Z-scores to be developed. Children with acute malnutrition showed immaturity of their microbiota, and the microbiota-for-age Z score correlated with weight-for-height Z-score at 18 months of age. Whilst these studies provide emerging evidence for a role of the microbiota in malnutrition, no published studies to date have characterised the microbiota of children with stunting.
Recurrent infections, inflammation and gut damage are all potentially amenable to interventions. A meta-analysis of ten trials from low- and middle-income countries showed that antibiotics had a significant impact on both weight and height gain; although antibiotics were given for a range of indications (not specifically for growth), a side-benefit may have been growth-promoting modulation of the intestinal microbiota and/or resolution of subclinical infections.179 There is current interest in azithromycin, a broad-spectrum, long-acting, immunomodulatory antibiotic that is commonly used in mass drug administration programmes for trachoma and improves child survival.180 However, a comparison of one versus two doses of azithromycin in Niger showed no difference in height between groups, although the study was cross-sectional and underpowered for this outcome;181 other trials are underway. A trial of rifaximin, a non-absorbable broad-spectrum antibiotic, among 3–5 year old children in Malawi was designed to test the hypothesis that a short course of antibiotics would reduce EED.182 At baseline and after 7 days of rifaximin, children were administered a combination of lactulose and mannitol, and researchers measured the ratio of the two sugars in the urine (L:M ratio), which provides a measure of small intestinal absorption and permeability. Although changes in L:M (the primary endpoint) were similar between rifaximin and placebo groups, leading the authors to speculate that bacterial overgrowth was not important, the trial assessed only one domain of EED,159 and the treatment duration was short.182 The same researchers undertook a three-arm randomised trial among 1–3 year old asymptomatic Malawian children, comparing single-dose albendazole, 14 days of zinc, or placebo; increases in L:M ratio were greater in the placebo compared to intervention groups, providing some promise that a short intervention may modulate markers of EED, although growth was not assessed.183 Several studies have evaluated the impact of probiotics on growth at different ages; overall, results are conflicting due to differences in duration, strain and dose of probiotics,184 but some have suggested benefit, mostly in weight gain.185–188 A trial of probiotics (Lactobacillus GG) in Malawian children at risk of EED showed no difference in L:M ratio after 30 days of treatment compared to placebo.189 The first study to evaluate an immunomodulatory approach to EED randomised children with severe acute malnutrition to 28 days of mesalazine (an aminosalicylate) or placebo during nutritional rehabilitation; although designed as a safety study with a primary outcome of adverse events (which were similar between groups), there was a trend towards reduction in several systemic inflammatory markers, suggesting that anti-inflammatory interventions are safe and warrant further evaluation in larger trials including growth outcomes.190
Millennium Development Goal 7c aims to halve the proportion of the population without sustainable access to safe drinking water and basic sanitation by 2015. The benefits of improved water, sanitation and hygiene (WASH) have mostly been evaluated in terms of reducing diarrhoea191 and soil-transmitted helminth infections,192 but it has been argued that the potential impact of WASH on EED and stunting has been undervalued.160 Observational studies support an association between WASH conditions and child height,168,193–199 and a recent meta-analysis of five cluster-randomised controlled trials which evaluated water disinfection, provision of soap or improvement in water quality (although no trials of improved sanitation) showed a small but significant impact on HAZ (mean difference 0.08, 95% CI 0.00–0.16).200 It has also been argued that WASH has potential to improve early child development through effects on inflammation, anaemia and stunting.201 Interventions need to be targeted at the pathways through which faeco-oral transmission commonly occurs in infancy, such as exploratory behaviour leading to ingestion of animal faeces and soil,202 known to be highly contaminated in settings where people live with livestock;203,204 this infant-targeted approach has been termed ‘baby WASH’ [201]. Cluster-randomised trials are currently evaluating the impact of improved WASH on stunting in Zimbabwe (clinicaltrials.gov identifier NCT01824940), Kenya (NCT01704105) and Bangladesh (NCT01590095).
There are observational data supporting associations between other environmental exposures and stunting. Mycotoxins are fungal metabolites that frequently contaminate staple foods such as maize and ground nuts in developing countries; infants tend to be particularly vulnerable to exposure in the food chain.205 Levels of aflatoxin were related to stunting in a cross-sectional study of children aged 9 months to 5 years in Benin and Togo206 and in Tanzania, exposure to fumonisin was inversely associated with linear growth in infancy.207 Mycotoxins might mediate stunting through multiple pathways, including enteropathy, although further studies are needed to clarify causation.208 Arsenic exposure during pregnancy has been linked to low birthweight209 and urinary arsenic metabolites were inversely related to plasma IGF-1 levels in Bangladeshi pre-school children.210 Half the global population uses biomass fuels such as dung, coal, charcoal or wood, which give rise to indoor pollution. In some studies,211,212 but not others,213 exposure to biomass fuels was associated with stunting in children, after adjusting for covariates.
Beyond 24 months of age
Stunting has tended to be viewed as a condition determined in the first 1000 days, because linear growth failure begins antenatally43 and continues over the first 24 months, with little apparent recovery thereafter.33 However, recently it has been proposed that the window of opportunity for catch-up growth may extend beyond 24 months, using longitudinal data from the COHORTS study,214 from rural Gambia,214 and from the Young Lives study in Ethiopia, Peru, India and Vietnam.215–217 However, there has been debate about the use of height-for-age Z-scores to describe changes in growth over time, because HAZ calculations include the age- and sex-specific standard deviation for height as the denominator, which increases with age; for a constant absolute height deficit, therefore, the HAZ will tend to become less negative over time, leading to apparent recovery in linear growth.218 This was well demonstrated in a recent analysis in which HAZ among children from three birth cohorts (South Africa, Guatemala, The Philippines) appeared to improve from 24 months to mid-childhood whilst the absolute height deficit continued to accumulate.219 Leroy et al. in a comparison of absolute height-for-age differences (HAD) with HAZ in 51 nationwide surveys showed that whilst HAZ appeared to level off between 24 and 60 months, HAD continued to increase; 70% of the shortfall in height occurred in the first 1000 days and 30% between 2 and 5 years of age.220
The question of potential recovery beyond the first 1000 days remains important and windows of opportunity for different components of the stunting syndrome may open and close at different times (Fig. 1). What causes ongoing linear growth faltering beyond 24 months, and whether interventions would usefully improve lean mass rather than increasing the risk of long-term obesity, remain uncertain.220 Adolescence is the time beyond infancy when growth velocity is maximal and represents the last opportunity for catch-up growth,221 although to achieve full growth potential probably requires intergenerational catch-up growth.222
CONSEQUENCES OF THE STUNTING SYNDROME
Short stature is an easily measurable indicator of a syndrome that has far-reaching consequences across the life-course (Fig. 1).
Morbidity and mortality
Short-term, stunting is associated with increased morbidity and mortality from infections, in particular pneumonia and diarrhoea.47,223–225 In a recent large analysis including individual-level data from 10 studies in Asia, Africa and South America, there was a clear dose-response relationship between HAZ and mortality, although not all datasets had information on potential confounders.224 Even children who were stunting but not stunted (HAZ between −2 and <−1) had an elevated risk of respiratory infections (HR 1.55, 95% CI 1.02–2.37) and diarrhoea (HR 1.67, 95% CI 1.20–2.30); children who were severely stunted (HAZ <−3) had a much greater risk (HR 6.39, 95% CI 4.19–9.75 and 6.33, 4.64–8.65, respectively). Severely stunted children also had a three-fold increased risk of mortality from other infections including sepsis, meningitis, tuberculosis, hepatitis and cellulitis (HR 3.01, 95% CI 1.55–5.82), suggesting a generalised immune defect in children with poor linear growth.
Although undernutrition is the commonest global immunodeficiency, the specific immune defects associated with stunting have not been well characterised. A recent systematic review226 summarised the literature on immune function in malnutrition but highlighted that most are cross-sectional studies of hospitalised children with SAM, using varied definitions of malnutrition, and conducted several decades ago. Malnourished children have complex derangements in physiology, impaired mucosal integrity, poor macro- and micro-nutrient status and multiple co-infections, and picking apart these contributory factors is challenging. Undernutrition appears to affect both innate and adaptive immunity,226 but more carefully designed, contemporary studies of well characterised longitudinal cohorts, including well-nourished control children, using modern immunological techniques, would help to understand better the immunology of stunting.
Cognition and behaviour
In the medium-term, the cognitive, educational and behavioural components of the stunting syndrome impact child development.3 Stunting is one of the major risk factors, together with inadequate cognitive stimulation, iodine deficiency and iron-deficiency anaemia, for failure to attain full developmental potential.227 Stunted children have impaired behavioural development in early life,228 are less likely to enroll at school229 or enroll late,230 tend to achieve lower grades231 and have poorer cognitive ability232–235 than non-stunted children. Furthermore, stunted children are more apathetic, display less exploratory behaviour236 and have altered physiological arousal.237 Stunted children followed longitudinally in Jamaica were found to have more anxiety and depression and lower self-esteem than non-stunted children at age 17, after adjusting for age, gender and social background variables.238
Undernutrition affects areas of the brain involved in cognition,239 memory240 and locomotor skills.241 The brain has major energy demands in early childhood and most cerebral growth occurs in the first 2 years of life. However, the associations between poor linear growth and impaired neurodevelopment are not well understood.239 Whether there are defects in myelination, establishment of neural pathways or synaptic proliferation and subsequent pruning, or evidence for neuroinflammation is not clear, but field studies employing more sophisticated measures of brain structure and function are underway. Furthermore, malnutrition, micronutrient deficiencies (especially iron), recurrent infections, apathy, reduced exploration, poverty, low maternal education and decreased stimulation often co-exist in the same household, and all are likely to affect child development.242
The window of opportunity for improving cognitive outcomes remains uncertain. In long-term follow-up of a Guatemalan trial, individuals randomised to energy/protein supplementation had a 10% improvement in non-verbal cognitive ability, but only if supplements were given in the first 2–3 years of life.243 In the COHORTS study, growth in the first 2 years of life, but not later, was associated with higher school grades among adults.255 However, among children in the Young Lives study, those who caught up with physical growth after 8 years of age had improved cognitive testing scores compared with those who remained stunted;216 in Peru, these cognitive testing scores were very similar to those of children who had never been stunted.245 In the same Peruvian cohort, current rather than previous stunting was the more important factor associated with cognitive skills at school entry,246 and in Filipino children, change in HAZ from 2 to 11 years was associated with cognitive ability at 11 years.247 Taken together, studies suggest potential for catch-up in cognition, although the greatest improvements may be in those receiving interventions in early life before trajectories have been firmly established.227
Long-term health and disease
Children who become stunted between conception and 2 years of age are at greater risk of poor health and lower socio-economic attainment throughout their lifetime. The excess risk of infectious morbidity and mortality apparent during childhood extends into adulthood.248 Stunted children lose ∼3.2 cm in adult stature for each decrement in HAZ at age 2 years;249 these negative impacts on stature (which translate into physical stamina) and cognition result in lower economic productivity, earning 8–46% lower wages249,250 and owning up to 66% fewer assets.251 Additionally, these effects are intergenerational: low birthweight is more common among infants whose mothers and even grandmothers were themselves stunted during early childhood.249 For Africa and Asia where 36% and 27% of children are stunted, respectively,1 these socio-economic consequences have a profound impact on the developmental capacity of entire societies.
Paradoxically, the metabolic syndrome, usually associated with over-nutrition, is more common in adults who were stunted in early childhood compared to those who experienced normal child growth.249 The ‘Developmental Origins of Health and Disease’ hypothesis proposes that nutritional deprivation during fetal or infant life252–254 triggers permanent epigenetic changes in metabolism (e.g. of lipids253 and glucose252) and organ anatomy and function (e.g. of blood vessels, liver and kidney255–257). While these changes may provide some survival benefit during fetal life by diverting nutrients away from growth to preserve vital functions, these same changes result in heightened risks of hypertension, cardiovascular disease, and type 2 diabetes, especially when aggravated by rapid weight gain and obesity after age 2 years. Accordingly, populations who have undergone a rapid transition from poverty and food insecurity to abundant access to a high-energy Western diet, such as India, are experiencing epidemics of diabetes and coronary heart disease.258 Conversely, in The Gambia, where socio-economic growth has been modest, little association between child stunting and adult metabolic syndrome has been detected.259
Observational data from birth cohorts indicate these associations between child stunting and adult disease are complex. Reviews of studies conducted primarily among high-income populations report that low birthweight is associated with elevated blood pressure during adulthood.260,261 Similarly, in pooled analyses of five birth cohorts from low- and middle-income countries,244,249 birthweight was inversely associated with adult blood pressure levels in analyses adjusting for adult BMI and height;249 but rapid (i.e. ‘catch-up’) linear growth between birth and mid-childhood244 was positively associated with elevated systolic blood pressure during adulthood. In these same cohorts, higher birthweight249 and catch-up rates of linear and ponderal growth between birth and mid-childhood244 were also associated with adult overweight. Importantly, the adverse associations with better linear growth were modest while increases in schooling, adult stature and wealth were substantial. Accordingly, increase in birthweight and linear growth velocity between conception and 2 years of age in children in developing countries is likely to reduce morbidity and mortality and provide substantial increases in human capital, with only modest trade-offs.
POLICY AND PROGRAMME IMPLICATIONS
By current estimates, stunting prevalence is likely decline to 20% (or 127 million children) by 2025, which is some way off the World Health Assembly target.2 The current evidence base for interventions to improve maternal and child undernutrition has been comprehensively reviewed as part of the recent Lancet Nutrition series.86 These authors estimated that if a package of nutrition-specific interventions (provision of maternal folic acid, calcium, multiple micronutrients and balanced energy protein supplementation; promotion of breastfeeding and appropriate complementary feeding; management of moderate and severe acute malnutrition and preventive zinc and vitamin A supplementation) was scaled up to 90% coverage, stunting would be reduced by mean 20.3% (range 10.2–28.9%) and under-5 mortality would be reduced by 15% (range 9–19%).86
Most strategies targeting MDG 1 are health-related interventions focused on the immediate determinants of undernutrition.262 Trends in stunting reduction are uneven within regions, or even within countries;263,264 modelling suggests that an equity-based approach targeting the poorest and most marginalised communities would be more cost-effective and lead to more rapid declines in stunting prevalence.265 Many countries require policies that tackle the ‘dual burden’ of stunting and overweight that is emerging during the nutrition transition.266 Multi-sectoral approaches which combine nutrition-sensitive with nutrition-specific interventions are likely to have a greater impact on reducing stunting.267–269 For example, the Millennium Villages project in which simultaneous investments were made in agriculture, the environment, business, education, infrastructure and health showed reductions in stunting (from 36% to 28% among children <2 years) across nine countries after 3 years.268 In addition, an enabling environment needs to be built to address more distal factors causing stunting;2 these constitute long-term developmental goals that underlie the impressive reductions in stunting seen in some countries.270 In Brazil, for example, stunting declined from 37% in 1974–5 to 7% in 2006–7 following economic growth and reduced disparity, increased urbanisation, improved female education, decreased fertility rates, improved WASH and health service reform.271 Whilst awaiting such long-term national development, programmes should focus on implementing packages of evidence-based, multi-sectoral interventions which cover the life-course to achieve the intergenerational investment in human capital that stunting reduction could provide.
DISCLAIMER STATEMENTS
Contributors AJP wrote the first draft of the manuscript, which was critically revised by JHH.
Funding AJP is funded by the Wellcome Trust (093768/Z/10/Z).
Conflicts of interest AJP and JHH are both investigators on the SHINE trial.
Ethics approval None.
Acknowledgments
We thank Sarah Donahue for help with designing the figure.
REFERENCES
- 1.UNICEF, WHO, World Bank. Levels and Trends in Child Malnutrition. Joint Child Malnutrition Estimates. New York, NY: United Nations International Children’s Fund; Geneva: WHO; Washington, DC: World Bank, 2012. Available from: http://www.who.int/nutgrowthdb/estimates/en/ [Google Scholar]
- 2.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 3.Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369:60–70. doi: 10.1016/S0140-6736(07)60032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Physical Status: the Use and Interpretation of Anthropometry. Report of a WHO Expert Committee. Technical Report Series No. 854. Geneva: WHO, 1995. Available from: http://www.who.int/childgrowth/publications/physical_status/en/ [PubMed] [Google Scholar]
- 5.Pradhan M, Sahn DE, Younger SD. Decomposing world health inequality. J Health Econ. 2003;22:271–93. doi: 10.1016/S0167-6296(02)00123-6. [DOI] [PubMed] [Google Scholar]
- 6.UNICEF. Tracking Progress on Child and Maternal Nutrition: A survival and development priority. UNICEF, 2009. Available from: http://www.unicef.org/publications/index_51656.html. [Google Scholar]
- 7.World Health Organization. Global Targets 2025. Available from: http://www.who.int/nutrition/topics/nutrition_globaltargets2025/en/ [Google Scholar]
- 8.de Onis M, Blossner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr. 2010;92:1257–64. doi: 10.3945/ajcn.2010.29786. [DOI] [PubMed] [Google Scholar]
- 9.Instituto de Nutrición de Centro América y Panamá. Food and nutritional situation and health in Central America. Guatemala: INCAP, 1992 (ME/003). Available from: http://pesquisa.bvsalud.org/portal/resource/pt/pah-11760 [Google Scholar]
- 10.Ruel MT, Rivera J, Habicht JP. Length screens better than weight in stunted populations. J Nutr. 1995;125:1222–8. doi: 10.1093/jn/125.5.1222. [DOI] [PubMed] [Google Scholar]
- 11.Simkiss D. Stunted growth. J Trop Pediatr. 2011;57:321–2. doi: 10.1093/tropej/fmr086. [DOI] [PubMed] [Google Scholar]
- 12.Stevens GA, Finucane MM, Paciorek CJ, Flaxman SR, White RA, Donner AJ, et al. Trends in mild, moderate, and severe stunting and underweight, and progress towards MDG 1 in 141 developing countries: a systematic analysis of population representative data. Lancet. 2012;380:824–34. doi: 10.1016/S0140-6736(12)60647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lutter CK, Chaparro CM, Munoz S. Progress towards Millennium Development Goal 1 in Latin America and the Caribbean: the importance of the choice of indicator for undernutrition. Bull WHO. 2011;89:22–30. doi: 10.2471/BLT.10.078618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nandy S, Irving M, Gordon D, Subramanian SV, Smith GD. Poverty, child undernutrition and morbidity: new evidence from India. Bull WHO. 2005;83:210–16. [PMC free article] [PubMed] [Google Scholar]
- 15.McDonald CM, Olofin I, Flaxman S, Fawzi WW, Spiegelman D, Caulfield LE, et al. The effect of multiple anthropometric deficits on child mortality: meta-analysis of individual data in 10 prospective studies from developing countries. Am J Clin Nutr. 2013;97:896–901. doi: 10.3945/ajcn.112.047639. [DOI] [PubMed] [Google Scholar]
- 16.Emergency Nutrition Network. Review of the Links Between Wasting and Stunting. ENN, 2014. Available from: http://www.ennonline.net/ourwork/reviews/wastingstunting. [Google Scholar]
- 17.Richard SA, Black RE, Checkley W. Revisiting the relationship of weight and height in early childhood. Adv Nutr. 2012;3:250–4. doi: 10.3945/an.111.001099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martorell R, Zongrone A. Intergenerational influences on child growth and undernutrition. Paediatr Perinat Epidemiol. 2012;26((suppl 1)):302–14. doi: 10.1111/j.1365-3016.2012.01298.x. [DOI] [PubMed] [Google Scholar]
- 19.Lampl M, Veldhuis JD, Johnson ML. Saltation and stasis: a model of human growth. Science. 1992;258:801–3. doi: 10.1126/science.1439787. [DOI] [PubMed] [Google Scholar]
- 20.Berndt SI, Gustafsson S, Magi R, Ganna A, Wheeler E, Feitosa MF, et al. Genome-wide meta-analysis identifies 11 new loci for anthropometric traits and provides insights into genetic architecture. Nat Genet. 2013;45:501–12. doi: 10.1038/ng.2606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lango Allen H, Estrada K, Lettre G, Berndt SI, Weedon MN, Rivadeneira F, et al. Hundreds of variants clustered in genomic loci and biological pathways affect human height. Nature. 2010;467:832–8. doi: 10.1038/nature09410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Villar J, Papageorghiou AT, Pang R, Ohuma EO, Ismail LC, Barros FC, et al. The likeness of fetal growth and newborn size across non-isolated populations in the INTERGROWTH-21 Project: the Fetal Growth Longitudinal Study and Newborn Cross-Sectional Study. Lancet Diab Endocrinol. 2014 doi: 10.1016/S2213-8587(14)70121-4. doi: 10.1016/S2213-8587(14)70121-4. [DOI] [PubMed] [Google Scholar]
- 23.WHO Working Group on the Growth Reference Protocol, WHO Task Force on Methods for the Natural Regulation of Fertility. Growth patterns of breastfed infants in seven countries. Acta Paediatr. 2000;89:215–22. doi: 10.1080/080352500750028861. [DOI] [PubMed] [Google Scholar]
- 24.Habicht JP, Martorell R, Yarbrough C, Malina RM, Klein RE. Height and weight standards for preschool children. How relevant are ethnic differences in growth potential? Lancet. 1974;1:611–14. doi: 10.1016/s0140-6736(74)92663-4. [DOI] [PubMed] [Google Scholar]
- 25.Bhandari N, Bahl R, Taneja S, de Onis M, Bhan MK. Growth performance of affluent Indian children is similar to that in developed countries. Bull WHO. 2002;80:189–95. [PMC free article] [PubMed] [Google Scholar]
- 26.Frongillo EA, Jr, de Onis M, Hanson KM. Socioeconomic and demographic factors are associated with worldwide patterns of stunting and wasting of children. J Nutr. 1997;127:2302–9. doi: 10.1093/jn/127.12.2302. [DOI] [PubMed] [Google Scholar]
- 27.Quinn VJ, Chiligo-Mpoma MO, Simler K, Milner J. The growth of Malawian preschool children from different socioeconomic groups. Eur J Clin Nutr. 1995;49:66–72. [PubMed] [Google Scholar]
- 28.Shen T, Habicht JP, Chang Y. Effect of economic reforms on child growth in urban and rural areas of China. N Engl J Med. 1996;335:400–6. doi: 10.1056/NEJM199608083350606. [DOI] [PubMed] [Google Scholar]
- 29.de Onis M, Frongillo EA, Blossner M. Is malnutrition declining? An analysis of changes in levels of child malnutrition since 1980. Bull WHO. 2000;78:1222–33. [PMC free article] [PubMed] [Google Scholar]
- 30.Bredenkamp C, Buisman LR, Van de Poel E. Persistent inequalities in child undernutrition: evidence from 80 countries, from 1990 to today. Int J Epidemiol. 2014;43:1328–35. doi: 10.1093/ije/dyu075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zong X-N, Li H. Physical growth of children and adolescents in China over the past 35 years. Bull WHO. 2014;92:555–64. doi: 10.2471/BLT.13.126243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Addo OY, Stein AD, Fall CH, Gigante DP, Guntupalli AM, Horta BL, et al. Maternal height and child growth patterns. J Pediatr. 2013;163:549–54. doi: 10.1016/j.jpeds.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Victora CG, de Onis M, Hallal PC, Blossner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics. 2010;125:e473–80. doi: 10.1542/peds.2009-1519. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization. Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/height-for-age, Weight-for-age, Weight-for-length, Weight-for-height and Body Mass Index-for-age: Methods and development. Geneva: WHO, 2006. Available from: http://www.who.int/childgrowth/standards/technical_report/en/ [Google Scholar]
- 35.Hamill PV, Drizd TA, Johnson CL, Reed RB, Roche AF, Moore WM. Physical growth: National Center for Health Statistics percentiles. Am J Clin Nutr. 1979;32:607–29. doi: 10.1093/ajcn/32.3.607. [DOI] [PubMed] [Google Scholar]
- 36.de Onis M, Onyango AW, Borghi E, Garza C, Yang H. Comparison of the World Health Organization (WHO) Child Growth Standards and the National Center for Health Statistics/WHO international growth reference: implications for child health programmes. Public Health Nutr. 2006;9:942–7. doi: 10.1017/phn20062005. [DOI] [PubMed] [Google Scholar]
- 37.Wamani H, Astrom AN, Peterson S, Tumwine JK, Tylleskar T. Boys are more stunted than girls in sub-Saharan Africa: a meta-analysis of 16 demographic and health surveys. BMC Pediatr. 2007;7:17. doi: 10.1186/1471-2431-7-17. doi: 10.1186/1471-2431-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Piwoz E, Sundberg S, Rooke J. Promoting healthy growth: what are the priorities for research and action? Adv Nutr. 2012;3:234–41. doi: 10.3945/an.111.001164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dewey KG, Mayers DR.Early child growth: how do nutrition and infection interact? Matern Child Nutr. 20117(suppl 3)129–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stewart CP, Iannotti L, Dewey KG, Michaelsen KF, Onyango AW. Contextualising complementary feeding in a broader framework for stunting prevention. Matern Child Nutr. 2013;9((suppl 2)):27–45. doi: 10.1111/mcn.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.de Onis M, Blossner M, Villar J. Levels and patterns of intrauterine growth retardation in developing countries. Eur J Clin Nutr. 1998;52((suppl 1)):S5–15. [PubMed] [Google Scholar]
- 42.Lee AC, Katz J, Blencowe H, Cousens S, Kozuki N, Vogel JP, et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health. 2013;1:e26–36. doi: 10.1016/S2214-109X(13)70006-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Christian P, Lee SE, Donahue Angel M, Adair LS, Arifeen SE, Ashorn P, et al. Risk of childhood undernutrition related to small-for-gestational age and preterm birth in low- and middle-income countries. Int J Epidemiol. 2013;42:1340–55. doi: 10.1093/ije/dyt109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Katz J, Lee AC, Kozuki N, Lawn JE, Cousens S, Blencowe H, et al. Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: a pooled country analysis. Lancet. 2013;382:417–25. doi: 10.1016/S0140-6736(13)60993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Neumann CG, Harrison GG. Onset and evolution of stunting in infants and children. Examples from the Human Nutrition Collaborative Research Support Program. Kenya and Egypt studies. Eur J Clin Nutr. 1994;48((suppl 1)):S90–102. [PubMed] [Google Scholar]
- 46.Schmidt MK, Muslimatun S, West CE, Schultink W, Gross R, Hautvast JG. Nutritional status and linear growth of Indonesian infants in west java are determined more by prenatal environment than by postnatal factors. J Nutr. 2002;132:2202–7. doi: 10.1093/jn/132.8.2202. [DOI] [PubMed] [Google Scholar]
- 47.Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–60. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 48.Neufeld LM, Haas JD, Grajeda R, Martorell R. Changes in maternal weight from the first to second trimester of pregnancy are associated with fetal growth and infant length at birth. Am J Clin Nutr. 2004;79:646–52. doi: 10.1093/ajcn/79.4.646. [DOI] [PubMed] [Google Scholar]
- 49.Gigante DP, Rasmussen KM, Victora CG. Pregnancy increases BMI in adolescents of a population-based birth cohort. J Nutr. 2005;135:74–80. doi: 10.1093/jn/135.1.74. [DOI] [PubMed] [Google Scholar]
- 50.Rah JH, Christian P, Shamim AA, Arju UT, Labrique AB, Rashid M. Pregnancy and lactation hinder growth and nutritional status of adolescent girls in rural Bangladesh. J Nutr. 2008;138:1505–11. doi: 10.1093/jn/138.8.1505. [DOI] [PubMed] [Google Scholar]
- 51.Gibbs CM, Wendt A, Peters S, Hogue CJ. The impact of early age at first childbirth on maternal and infant health. Paediatr Perinat Epidemiol. 2012;26((suppl 1)):259–84. doi: 10.1111/j.1365-3016.2012.01290.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kozuki N, Lee AC, Silveira MF, Victora CG, Adair L, Humphrey J, et al. The associations of birth intervals with small-for-gestational-age, preterm, and neonatal and infant mortality: a meta-analysis. BMC Public Health. 2013;13((suppl 3)):S3. doi: 10.1186/1471-2458-13-S3-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Merchant K, Martorell R, Haas JD. Consequences for maternal nutrition of reproductive stress across consecutive pregnancies. Am J Clin Nutr. 1990;52:616–20. doi: 10.1093/ajcn/52.4.616. [DOI] [PubMed] [Google Scholar]
- 54.Monden CW, Smits J. Maternal height and child mortality in 42 developing countries. Am J Hum Biol. 2009;21:305–11. doi: 10.1002/ajhb.20860. [DOI] [PubMed] [Google Scholar]
- 55.Ozaltin E, Hill K, Subramanian SV. Association of maternal stature with offspring mortality, underweight, and stunting in low- to middle-income countries. JAMA. 2010;303:1507–16. doi: 10.1001/jama.2010.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Subramanian SV, Ackerson LK, Davey Smith G, John NA. Association of maternal height with child mortality, anthropometric failure, and anemia in India. JAMA. 2009;301:1691–701. doi: 10.1001/jama.2009.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tiisala R, Kantero RL. Studies on growth of Finnish children from birth to 10 years. VII. Some parent-child correlations for height, weight and skeletal age up to 10 years. A mixed longitudinal study. Acta Paediatr Scandinavica. 1971;220:42–8. doi: 10.1111/j.1651-2227.1971.tb14993.x. [DOI] [PubMed] [Google Scholar]
- 58.Chusilp K, Somnasang P, Kirdpon W, Wongkham S, Sribonlue P, Mahaverawat U, et al. Observations on the development of stunting in children of the Khon Kaen region of Thailand. Eur J Clin Nutr. 1992;46:475–87. [PubMed] [Google Scholar]
- 59.Subramanian SV, Ackerson LK, Smith GD. Parental BMI and childhood undernutrition in India: an assessment of intrauterine influence. Pediatrics. 2010;126:e663–71. doi: 10.1542/peds.2010-0222. [DOI] [PubMed] [Google Scholar]
- 60.Ozaltin E, Subramanian SV. Why we need to rethink the strategy and time frame for achieving health-related Millennium Development Goals. Int Health. 2011;3:246–50. doi: 10.1016/j.inhe.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 61.Mason JB, Shrimpton R, Saldanha LS, Ramakrishnan U, Victora CG, Girard AW, et al. The first 500 days of life: policies to support maternal nutrition. Global Health Action. 2014 doi: 10.3402/gha.v7.23623. doi: 10.3402/gha.v7.23623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Haider BA, Yakoob MY, Bhutta ZA. Effect of multiple micronutrient supplementation during pregnancy on maternal and birth outcomes. BMC Public Health. 2011 doi: 10.1186/1471-2458-11-S3-S19. doi: 10.1186/1471-2458-11-S3-S19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Imdad A, Bhutta ZA. Effect of balanced protein energy supplementation during pregnancy on birth outcomes. BMC Public Health. 2011;11((suppl 3)):S17. doi: 10.1186/1471-2458-11-S3-S17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Imdad A, Bhutta ZA. Routine iron/folate supplementation during pregnancy: effect on maternal anaemia and birth outcomes. Paediatr Perinat Epidemiol. 2012;26((Suppl 1):168–77. doi: 10.1111/j.1365-3016.2012.01312.x. [DOI] [PubMed] [Google Scholar]
- 65.Mori R, Ota E, Middleton P, Tobe-Gai R, Mahomed K, Bhutta ZA. Zinc supplementation for improving pregnancy and infant outcome. Cochrane Database Syst Rev. 2012;7:CD000230. doi: 10.1002/14651858.CD000230.pub4. [DOI] [PubMed] [Google Scholar]
- 66.Imdad A, Bhutta ZA. Effects of calcium supplementation during pregnancy on maternal, fetal and birth outcomes. Paediatr Perinat Epidemiol. 2012;26((Suppl 1)):138–52. doi: 10.1111/j.1365-3016.2012.01274.x. [DOI] [PubMed] [Google Scholar]
- 67.De-Regil LM, Palacios C, Ansary A, Kulier R, Pena-Rosas JP. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst Rev. 2012;2:CD008873. doi: 10.1002/14651858.CD008873.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.McKay JA, Mathers JC. Diet induced epigenetic changes and their implications for health. Acta Physiol. 2011;202:103–18. doi: 10.1111/j.1748-1716.2011.02278.x. [DOI] [PubMed] [Google Scholar]
- 69.Suter M, Bocock P, Showalter L, Hu M, Shope C, McKnight R, et al. Epigenomics: maternal high-fat diet exposure in utero disrupts peripheral circadian gene expression in nonhuman primates. FASEB J. 2011;25:714–26. doi: 10.1096/fj.10-172080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cox J, Williams S, Grove K, Lane RH, Aagaard-Tillery KM. A maternal high-fat diet is accompanied by alterations in the fetal primate metabolome. Am J Obstet Gynecol. 2009;201:e281–9. doi: 10.1016/j.ajog.2009.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cooper WN, Khulan B, Owens S, Elks CE, Seidel V, Prentice AM, et al. DNA methylation profiling at imprinted loci after periconceptional micronutrient supplementation in humans: results of a pilot randomized controlled trial. FASEB J. 2012;26:1782–90. doi: 10.1096/fj.11-192708. [DOI] [PubMed] [Google Scholar]
- 72.Khulan B, Cooper WN, Skinner BM, Bauer J, Owens S, Prentice AM, et al. Periconceptional maternal micronutrient supplementation is associated with widespread gender related changes in the epigenome: a study of a unique resource in the Gambia. Hum Mol Genet. 2012;21:2086–101. doi: 10.1093/hmg/dds026. [DOI] [PubMed] [Google Scholar]
- 73.Roberfroid D, Huybregts L, Lanou H, Ouedraogo L, Henry MC, Meda N, et al. Impact of prenatal multiple micronutrients on survival and growth during infancy: a randomized controlled trial. Am J Clin Nutr. 2012;95:916–24. doi: 10.3945/ajcn.111.029033. [DOI] [PubMed] [Google Scholar]
- 74.Stewart CP, Christian P, LeClerq SC, West KP., Jr Khatry SK. Antenatal supplementation with folic acid + iron + zinc improves linear growth and reduces peripheral adiposity in school-age children in rural Nepal. Am J Clin Nutr. 2009;90:132–40. doi: 10.3945/ajcn.2008.27368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Huy ND, Le Hop T, Shrimpton R, Hoa CV. An effectiveness trial of multiple micronutrient supplementation during pregnancy in Vietnam: impact on birthweight and on stunting in children at around 2 years of age. Food Nutr Bull. 2009;30:S506–16. doi: 10.1177/15648265090304S405. [DOI] [PubMed] [Google Scholar]
- 76.Khan AI, Kabir I, Ekstrom EC, Asling-Monemi K, Alam DS, Frongillo EA, et al. Effects of prenatal food and micronutrient supplementation on child growth from birth to 54 months of age: a randomized trial in Bangladesh. Nutr J. 2011;10:134. doi: 10.1186/1475-2891-10-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lanou H, Huybregts L, Roberfroid D, Nikiema L, Kouanda S, Van Camp J, et al. Prenatal nutrient supplementation and postnatal growth in a developing nation: an RCT. Pediatrics. 2014;133:e1001–8. doi: 10.1542/peds.2013-2850. [DOI] [PubMed] [Google Scholar]
- 78.Wang W, Yan H, Zeng L, Cheng Y, Wang D, Li Q. No effect of maternal micronutrient supplementation on early childhood growth in rural western China: 30 month follow-up evaluation of a double blind, cluster randomized controlled trial. Eur J Clin Nutr. 2012;66:261–8. doi: 10.1038/ejcn.2011.190. [DOI] [PubMed] [Google Scholar]
- 79.Pongcharoen T, Ramakrishnan U, DiGirolamo AM, Winichagoon P, Flores R, Singkhornard J, et al. Influence of prenatal and postnatal growth on intellectual functioning in school-aged children. Arch Pediatr Adolesc Med. 2012;166:411–16. doi: 10.1001/archpediatrics.2011.1413. [DOI] [PubMed] [Google Scholar]
- 80.Martorell R, Young MF. Patterns of stunting and wasting: potential explanatory factors. Adv Nutr. 2012;3:227–33. doi: 10.3945/an.111.001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Patwari AK, Kumar S, Beard J. Undernutrition among infants less than 6 months of age: an underestimated public health problem in India. Matern Child Nutr. 2013 doi: 10.1111/mcn.12030. doi: 10.1111/mcn.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Young MF, Martorell R. The public health challenge of early growth failure in India. Eur J Clin Nutr. 2013;67:496–500. doi: 10.1038/ejcn.2013.18. [DOI] [PubMed] [Google Scholar]
- 83.Kerac M, Blencowe H, Grijalva-Eternod C, McGrath M, Shoham J, Cole TJ, et al. Prevalence of wasting among under 6-month-old infants in developing countries and implications of new case definitions using WHO growth standards: a secondary data analysis. Arch Dis Child. 2011;96:1008–13. doi: 10.1136/adc.2010.191882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.World Health Organization. The Optimal Duration of Exclusive Breastfeeding: Report of the Expert Consultation. Geneva: WHO, 2001. Available from: http://www.who.int/nutrition/publications/infantfeeding/WHO_NHD_01.09/en/ [Google Scholar]
- 85.World Health Organization. Long-term Effects of Breastfeeding: a Systematic Review. Geneva: WHO, 2013. Available from: http://www.who.int/maternal_child_adolescent/documents/breastfeeding_long_term_effects/en/ [Google Scholar]
- 86.Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. 2013;382:452–77. doi: 10.1016/S0140-6736(13)60996-4. [DOI] [PubMed] [Google Scholar]
- 87.Engebretsen IM, Jackson D, Fadnes LT, Nankabirwa V, Diallo AH, Doherty T, et al. Growth effects of exclusive breastfeeding promotion by peer counsellors in sub-Saharan Africa: the cluster-randomised PROMISE EBF trial. BMC Public Health. 2014;14:633. doi: 10.1186/1471-2458-14-633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Berngard SC, Berngard JB, Krebs NF, Garces A, Miller LV, Westcott J, et al. Newborn length predicts early infant linear growth retardation and disproportionately high weight gain in a low-income population. Early Hum Dev. 2013;89:967–72. doi: 10.1016/j.earlhumdev.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Prendergast AJ, Rukobo S, Chasekwa B, Mutasa K, Ntozini R, Mbuya MN, et al. Stunting is characterized by chronic inflammation in zimbabwean infants. PLoS One. 2014;9:e86928. doi: 10.1371/journal.pone.0086928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shrimpton R, Victora CG, de Onis M, Lima RC, Blossner M, Clugston G. Worldwide timing of growth faltering: implications for nutritional interventions. Pediatrics. 2001;107:E75. doi: 10.1542/peds.107.5.e75. [DOI] [PubMed] [Google Scholar]
- 91.Dewey KG, Adu-Afarwuah S. 2008. Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. In: Maternal and Child Nutrition. Davis, CA: Blackwell Publishing. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.World Health Organization. Implementing the Global Strategy for Infant and Young Child Feeding, meeting report, Geneva, 3–5 February 2003. Available from: http://www.who.int/nutrition/publications/infantfeeding/924159120X/en/ [Google Scholar]
- 93.Lutter CK, Daelmans BM, de Onis M, Kothari MT, Ruel MT, Arimond M, et al. Undernutrition, poor feeding practices, and low coverage of key nutrition interventions. Pediatrics. 2011;128:e1418–27. doi: 10.1542/peds.2011-1392. [DOI] [PubMed] [Google Scholar]
- 94.Marriott BP, White A, Hadden L, Davies JC, Wallingford JC. World Health Organization infant and young child feeding indicators: associations with growth measures in 14 low-income countries. Matern Child Nutr. 2012;8:354–70. doi: 10.1111/j.1740-8709.2011.00380.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Jones AD, Ickes SB, Smith LE, Mbuya MN, Chasekwa B, Heidkamp RA, et al. World Health Organization infant and young child feeding indicators and their associations with child anthropometry: a synthesis of recent findings. Matern Child Nutr. 2014;10:1–17. doi: 10.1111/mcn.12070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lassi ZS, Das JK, Zahid G, Imdad A, Bhutta ZA. Impact of education and provision of complementary feeding on growth and morbidity in children less than 2 years of age in developing countries: a systematic review. BMC Public Health. 2013;13((suppl 3)):S13. doi: 10.1186/1471-2458-13-S3-S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sguassero Y, de Onis M, Bonotti AM, Carroli G. Community-based supplementary feeding for promoting the growth of children under five years of age in low and middle income countries. Cochrane Database Syst Rev. 2012;6:CD005039. doi: 10.1002/14651858.CD005039.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Adu-Afarwuah S, Lartey A, Brown KH, Zlotkin S, Briend A, Dewey KG. Randomized comparison of 3 types of micronutrient supplements for home fortification of complementary foods in Ghana: effects on growth and motor development. Am J Clin Nutr. 2007;86:412–20. doi: 10.1093/ajcn/86.2.412. [DOI] [PubMed] [Google Scholar]
- 99.Bisimwa G, Owino VO, Bahwere P, Dramaix M, Donnen P, Dibari F, et al. Randomized controlled trial of the effectiveness of a soybean-maize-sorghum-based ready-to-use complementary food paste on infant growth in South Kivu, Democratic Republic of Congo. Am J Clin Nutr. 2012;95:1157–64. doi: 10.3945/ajcn.111.028704. [DOI] [PubMed] [Google Scholar]
- 100.Iannotti LL, Dulience SJ, Green J, Joseph S, Francois J, Antenor ML, et al. Linear growth increased in young children in an urban slum of Haiti: a randomized controlled trial of a lipid-based nutrient supplement. Am J Clin Nutr. 2014;99:198–208. doi: 10.3945/ajcn.113.063883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lin CA, Manary MJ, Maleta K, Briend A, Ashorn P. An energy-dense complementary food is associated with a modest increase in weight gain when compared with a fortified porridge in Malawian children aged 6–18 months. J Nutr. 2008;138:593–8. doi: 10.1093/jn/138.3.593. [DOI] [PubMed] [Google Scholar]
- 102.Mangani C, Maleta K, Phuka J, Cheung YB, Thakwalakwa C, Dewey K, et al. Effect of complementary feeding with lipid-based nutrient supplements and corn-soy blend on the incidence of stunting and linear growth among 6- to 18-month-old infants and children in rural Malawi. Matern Child Nutr. 2013 doi: 10.1111/mcn.12068. doi: 10.1111/mcn.12068 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Phuka JC, Maleta K, Thakwalakwa C, Cheung YB, Briend A, Manary MJ, et al. Complementary feeding with fortified spread and incidence of severe stunting in 6- to 18-month-old rural Malawians. Arch Pediatr Adolesc Med. 2008;162:619–26. doi: 10.1001/archpedi.162.7.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Phuka J, Thakwalakwa C, Maleta K, Cheung YB, Briend A, Manary M, et al. Supplementary feeding with fortified spread among moderately underweight 6–18-month-old rural Malawian children. Matern Child Nutr. 2009;5:159–70. doi: 10.1111/j.1740-8709.2008.00162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Phuka JC, Maleta K, Thakwalakwa C, Cheung YB, Briend A, Manary MJ, et al. Postintervention growth of Malawian children who received 12-mo dietary complementation with a lipid-based nutrient supplement or maize-soy flour. Am J Clin Nutr. 2009;89:382–90. doi: 10.3945/ajcn.2008.26483. [DOI] [PubMed] [Google Scholar]
- 106.Abu-Saad K, Fraser D. Maternal nutrition and birth outcomes. Epidemiol Rev. 2010;32:5–25. doi: 10.1093/epirev/mxq001. [DOI] [PubMed] [Google Scholar]
- 107.Muthayya S, Rah JH, Sugimoto JD, Roos FF, Kraemer K, Black RE. The global hidden hunger indices and maps: an advocacy tool for action. PLoS One. 2013;8:e67860. doi: 10.1371/journal.pone.0067860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Salam RA, MacPhail C, Das JK, Bhutta ZA. BMC Public Health. (Suppl 3) Vol. 13. S22; 2013. Effectiveness of micronutrient powders (MNP) in women and children. doi: 10.1186/1471-2458-13-S3-S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wessells KR, Brown KH. Estimating the global prevalence of zinc deficiency: results based on zinc availability in national food supplies and the prevalence of stunting. PLoS One. 2012;7:e50568. doi: 10.1371/journal.pone.0050568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Imdad A, Bhutta ZA. Effect of preventive zinc supplementation on linear growth in children under 5 years of age in developing countries: a meta-analysis of studies for input to the lives saved tool. BMC Public Health. 2011;11((Suppl 3)):S22. doi: 10.1186/1471-2458-11-S3-S22. doi: 10.1186/1471-2458-11-S3-S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Muhilal, Permeisih D, Idjradinata YR, Muherdiyantiningsih, Karyadi D. Vitamin A-fortified monosodium glutamate and health, growth, and survival of children: a controlled field trial. Am J Clin Nutr. 1988;48:1271–6. doi: 10.1093/ajcn/48.5.1271. [DOI] [PubMed] [Google Scholar]
- 112.Lie C, Ying C, Wang EL, Brun T, Geissler C. Impact of large-dose vitamin A supplementation on childhood diarrhoea, respiratory disease and growth. Eur J Clin Nutr. 1993;47:88–96. [PubMed] [Google Scholar]
- 113.Ramakrishnan U, Latham MC, Abel R. Vitamin A supplementation does not improve growth of preschool children: a randomized, double-blind field trial in south India. J Nutr. 1995;125:202–11. doi: 10.1093/jn/125.2.202. [DOI] [PubMed] [Google Scholar]
- 114.Hadi H, Stoltzfus RJ, Dibley MJ, Moulton LH, West KP, Jr, Kjolhede CL, et al. Vitamin A supplementation selectively improves the linear growth of indonesian preschool children: results from a randomized controlled trial. Am J Clin Nutr. 2000;71:507–13. doi: 10.1093/ajcn/71.2.507. [DOI] [PubMed] [Google Scholar]
- 115.Mata LJ, Kromal RA, Urrutia JJ, Garcia B. Effect of infection on food intake and the nutritional state: perspectives as viewed from the village. Am J Clin Nutr. 1977;30:1215–27. doi: 10.1093/ajcn/30.8.1215. [DOI] [PubMed] [Google Scholar]
- 116.Black RE, Brown KH, Becker S. Effects of diarrhea associated with specific enteropathogens on the growth of children in rural Bangladesh. Pediatrics. 1984;73:799–805. [PubMed] [Google Scholar]
- 117.Guerrant RL, Kirchhoff LV, Shields DS, Nations MK, Leslie J, de Sousa MA, et al. Prospective study of diarrheal illnesses in northeastern Brazil: patterns of disease, nutritional impact, etiologies, and risk factors. J Infect Dis. 1983;148:986–97. doi: 10.1093/infdis/148.6.986. [DOI] [PubMed] [Google Scholar]
- 118.Lima AA, Moore SR, Barboza MS., Jr Soares AM, Schleupner MA, Newman RD, et al. Persistent diarrhea signals a critical period of increased diarrhea burdens and nutritional shortfalls: a prospective cohort study among children in northeastern Brazil. J Infect Dis. 2000;181:1643–51. doi: 10.1086/315423. [DOI] [PubMed] [Google Scholar]
- 119.Moore SR, Lima AA, Conaway MR, Schorling JB, Soares AM, Guerrant RL. Early childhood diarrhoea and helminthiases associate with long-term linear growth faltering. Int J Epidemiol. 2001;30:1457–64. doi: 10.1093/ije/30.6.1457. [DOI] [PubMed] [Google Scholar]
- 120.Caulfield LE, de Onis M, Blossner M, Black RE. Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. Am J Clin Nutr. 2004;80:193–8. doi: 10.1093/ajcn/80.1.193. [DOI] [PubMed] [Google Scholar]
- 121.Guerrant RL, Schorling JB, McAuliffe JF, de Souza MA. Diarrhea as a cause and an effect of malnutrition: diarrhea prevents catch-up growth and malnutrition increases diarrhea frequency and duration. Am J Trop Med Hyg. 1992;47:28–35. doi: 10.4269/ajtmh.1992.47.28. [DOI] [PubMed] [Google Scholar]
- 122.Mata L. Diarrheal disease as a cause of malnutrition. Am J Trop Med Hyg. 1992;47:16–27. doi: 10.4269/ajtmh.1992.47.16. [DOI] [PubMed] [Google Scholar]
- 123.Schorling JB, McAuliffe JF, de Souza MA, Guerrant RL. Malnutrition is associated with increased diarrhoea incidence and duration among children in an urban Brazilian slum. Int J Epidemiol. 1990;19:728–35. doi: 10.1093/ije/19.3.728. [DOI] [PubMed] [Google Scholar]
- 124.Costa LB, Noronha FJ, Roche JK, Sevilleja JE, Warren CA, Oria R, et al. Novel in vitro and in vivo models and potential new therapeutics to break the vicious cycle of Cryptosporidium infection and malnutrition. J Infect Dis. 2012;205:1464–71. doi: 10.1093/infdis/jis216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Coutinho BP, Oria RB, Vieira CM, Sevilleja JE, Warren CA, Maciel JG, et al. Cryptosporidium infection causes undernutrition and, conversely, weanling undernutrition intensifies infection. J Parasitol. 2008;94:1225–32. doi: 10.1645/GE-1411.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Roche JK, Cabel A, Sevilleja J, Nataro J, Guerrant RL. Enteroaggregative Escherichia coli (EAEC) impairs growth while malnutrition worsens EAEC infection: a novel murine model of the infection malnutrition cycle. J Infect Dis. 2010;202:506–14. doi: 10.1086/654894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bartelt LA, Roche J, Kolling G, Bolick D, Noronha F, Naylor C, et al. Persistent G. lamblia impairs growth in a murine malnutrition model. J Clin Invest. 2013;123:2672–84. doi: 10.1172/JCI67294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Arinaitwe E, Gasasira A, Verret W, Homsy J, Wanzira H, Kakuru A, et al. The association between malnutrition and the incidence of malaria among young HIV-infected and -uninfected Ugandan children: a prospective study. Malaria J. 20121190.doi: 10.1186/1475-2875-11-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Bradley-Moore AM, Greenwood BM, Bradley AK, Kirkwood BR, Gilles HM. Malaria chemoprophylaxis with chloroquine in young Nigerian children. III. Its effect on nutrition. Ann Trop Med Parasitol. 1985;79:575–84. doi: 10.1080/00034983.1985.11811964. [DOI] [PubMed] [Google Scholar]
- 130.Deen JL, Walraven GE, von Seidlein L. Increased risk for malaria in chronically malnourished children under 5 years of age in rural Gambia. J Trop Pediatr. 2002;48:78–83. doi: 10.1093/tropej/48.2.78. [DOI] [PubMed] [Google Scholar]
- 131.Ehrhardt S, Burchard GD, Mantel C, Cramer JP, Kaiser S, Kubo M, et al. Malaria, anemia, and malnutrition in african children – defining intervention priorities. J Infect Dis. 2006;194:108–14. doi: 10.1086/504688. [DOI] [PubMed] [Google Scholar]
- 132.ter Kuile FO, Terlouw DJ, Kariuki SK, Phillips-Howard PA, Mirel LB, Hawley WA, et al. Impact of permethrin-treated bed nets on malaria, anemia, and growth in infants in an area of intense perennial malaria transmission in western Kenya. Am J Trop Med Hyg. 2003;68:68–77. [PubMed] [Google Scholar]
- 133.Genton B, Al-Yaman F, Ginny M, Taraika J, Alpers MP. Relation of anthropometry to malaria morbidity and immunity in Papua New Guinean children. Am J Clin Nutr. 1998;68:734–41. doi: 10.1093/ajcn/68.3.734. [DOI] [PubMed] [Google Scholar]
- 134.Crookston BT, Alder SC, Boakye I, Merrill RM, Amuasi JH, Porucznik CA, et al. Exploring the relationship between chronic undernutrition and asymptomatic malaria in Ghanaian children. Malaria J. 2010939.doi: 10.1186/1475-2875-9-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Deribew A, Alemseged F, Tessema F, Sena L, Birhanu Z, Zeynudin A, et al. Malaria and under-nutrition: a community based study among under-five children at risk of malaria, south-west Ethiopia. PLoS One. 2010;5:e10775. doi: 10.1371/journal.pone.0010775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Fillol F, Sarr JB, Boulanger D, Cisse B, Sokhna C, Riveau G, et al. Impact of child malnutrition on the specific anti-Plasmodium falciparum antibody response. Malaria J. 20098116.doi: 10.1186/1475-2875-8-116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Snow RW, Byass P, Shenton FC, Greenwood BM. The relationship between anthropometric measurements and measurements of iron status and susceptibility to malaria in Gambian children. Trans R Soc Trop Med Hyg. 1991;85:584–9. doi: 10.1016/0035-9203(91)90351-x. [DOI] [PubMed] [Google Scholar]
- 138.Kang H, Kreuels B, Adjei O, Krumkamp R, May J, Small DS. The causal effect of malaria on stunting: a Mendelian randomization and matching approach. Int J Epidemiol. 2013;42:1390–8. doi: 10.1093/ije/dyt116. [DOI] [PubMed] [Google Scholar]
- 139.Mupfasoni D, Karibushi B, Koukounari A, Ruberanziza E, Kaberuka T, Kramer MH, et al. Polyparasite helminth infections and their association to anaemia and undernutrition in Northern Rwanda. PLoS Negl Trop Dis. 2009;3:e517. doi: 10.1371/journal.pntd.0000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Koukounari A, Gabrielli AF, Toure S, Bosque-Oliva E, Zhang Y, Sellin B, et al. Schistosoma haematobium infection and morbidity before and after large-scale administration of praziquantel in Burkina Faso. J Infect Dis. 2007;196:659–69. doi: 10.1086/520515. [DOI] [PubMed] [Google Scholar]
- 141.Ezeamama AE, Friedman JF, Acosta LP, Bellinger DC, Langdon GC, Manalo DL, et al. Helminth infection and cognitive impairment among Filipino children. Am J Trop Med Hyg. 2005;72:540–8. [PMC free article] [PubMed] [Google Scholar]
- 142.Ezeamama AE, McGarvey ST, Acosta LP, Zierler S, Manalo DL, Wu HW, et al. The synergistic effect of concomitant schistosomiasis, hookworm, and trichuris infections on children's anemia burden. PLoS Negl Trop Dis. 2008;2:e245. doi: 10.1371/journal.pntd.0000245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Stephenson LS, Latham MC, Kurz KM, Kinoti SN, Oduori ML, Crompton DW. Relationships of Schistosoma hematobium, hookworm and malarial infections and metrifonate treatment to hemoglobin level in Kenyan school children. Am J Trop Med Hyg. 1985;34:519–28. doi: 10.4269/ajtmh.1985.34.519. [DOI] [PubMed] [Google Scholar]
- 144.Bosompem KM, Bentum IA, Otchere J, Anyan WK, Brown CA, Osada Y, et al. Infant schistosomiasis in Ghana: a survey in an irrigation community. Trop Med Int Health. 2004;9:917–22. doi: 10.1111/j.1365-3156.2004.01282.x. [DOI] [PubMed] [Google Scholar]
- 145.Garba A, Barkire N, Djibo A, Lamine MS, Sofo B, Gouvras AN, et al. Schistosomiasis in infants and preschool-aged children: Infection in a single Schistosoma haematobium and a mixed S. haematobium–S. mansoni foci of Niger. Acta Trop. 2010;115:212–19. doi: 10.1016/j.actatropica.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 146.Odogwu SE, Ramamurthy NK, Kabatereine NB, Kazibwe F, Tukahebwa E, Webster JP, et al. Schistosoma mansoni in infants (aged <3 years) along the Ugandan shoreline of Lake Victoria. Ann Trop Med Parasitol. 2006;100:315–26. doi: 10.1179/136485906X105552. [DOI] [PubMed] [Google Scholar]
- 147.Verani JR, Abudho B, Montgomery SP, Mwinzi PN, Shane HL, Butler SE, et al. Schistosomiasis among young children in Usoma, Kenya. Am J Trop Med Hyg. 2011;84:787–91. doi: 10.4269/ajtmh.2011.10-0685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Koski KG, Scott ME. Gastrointestinal nematodes, nutrition and immunity: breaking the negative spiral. Ann Rev Nutr. 2001;21:297–321. doi: 10.1146/annurev.nutr.21.1.297. [DOI] [PubMed] [Google Scholar]
- 149.Briend A, Hasan KZ, Aziz KM, Hoque BA. Are diarrhoea control programmes likely to reduce childhood malnutrition? Observations from rural Bangladesh. Lancet. 1989;2:319–22. doi: 10.1016/s0140-6736(89)90498-4. [DOI] [PubMed] [Google Scholar]
- 150.Rowland MG, Cole TJ, Whitehead RG. A quantitative study into the role of infection in determining nutritional status in Gambian village children. Br J Nutr. 1977;37:441–50. doi: 10.1079/bjn19770047. [DOI] [PubMed] [Google Scholar]
- 151.Rowland MG, Rowland SG, Cole TJ. Impact of infection on the growth of children from 0 to 2 years in an urban West African community. Am J Clin Nutr. 1988;47:134–8. doi: 10.1093/ajcn/47.1.134. [DOI] [PubMed] [Google Scholar]
- 152.Walker SP, Grantham-McGregor SM, Powell CA, Himes JH, Simeon DT. Morbidity and the growth of stunted and nonstunted children, and the effect of supplementation. Am J Clin Nutr. 1992;56:504–10. doi: 10.1093/ajcn/56.3.504. [DOI] [PubMed] [Google Scholar]
- 153.Briend A. Is diarrhoea a major cause of malnutrition among the under-fives in developing countries? A review of available evidence. Eur J Clin Nutr. 1990;44:611–28. [PubMed] [Google Scholar]
- 154.Checkley W, Buckley G, Gilman RH, Assis AM, Guerrant RL, Morris SS, et al. Multi-country analysis of the effects of diarrhoea on childhood stunting. Int J Epidemiol. 2008;37:816–30. doi: 10.1093/ije/dyn099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Richard SA, Black RE, Gilman RH, Guerrant RL, Kang G, Lanata CF, et al. Diarrhea in early childhood: short-term association with weight and long-term association with length. Am J Epidemiol. 2013;178:1129–38. doi: 10.1093/aje/kwt094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kotloff KL, Nataro JP, Blackwelder WC, Nasrin D, Farag TH, Panchalingam S, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet. 2013;382:209–22. doi: 10.1016/S0140-6736(13)60844-2. [DOI] [PubMed] [Google Scholar]
- 157.Desai HG, Borkar AV, Pathare SM, Dighe PK, Jeejeebhoy KN. 'Flat' jejunal mucosa in the tropics. Indian J Med Sci. 1969;23:1–5. [PubMed] [Google Scholar]
- 158.Schenk EA, Samloff IM, Klipstein FA. Morphology of small bowel biopsies. Am J Clin Nutr. 1968;21:944–61. doi: 10.1093/ajcn/21.9.944. [DOI] [PubMed] [Google Scholar]
- 159.Keusch GT, Rosenberg IH, Denno DM, Duggan C, Guerrant RL, Lavery JV, et al. Implications of acquired environmental enteric dysfunction for growth and stunting in infants and children living in low- and middle-income countries. Food Nutr Bull. 2013;34:357–64. doi: 10.1177/156482651303400308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Humphrey JH. Child undernutrition, tropical enteropathy, toilets, and handwashing. Lancet. 2009;374:1032–5. doi: 10.1016/S0140-6736(09)60950-8. [DOI] [PubMed] [Google Scholar]
- 161.Campbell DI, Elia M, Lunn PG. Growth faltering in rural Gambian infants is associated with impaired small intestinal barrier function, leading to endotoxemia and systemic inflammation. J Nutr. 2003;133:1332–8. doi: 10.1093/jn/133.5.1332. [DOI] [PubMed] [Google Scholar]
- 162.Campbell DI, Lunn PG, Elia M. Age-related association of small intestinal mucosal enteropathy with nutritional status in rural Gambian children. Br J Nutr. 2002;88:499–505. doi: 10.1079/BJN2002697. [DOI] [PubMed] [Google Scholar]
- 163.Campbell DI, Murch SH, Elia M, Sullivan PB, Sanyang MS, Jobarteh B, et al. Chronic T cell-mediated enteropathy in rural west African children: relationship with nutritional status and small bowel function. Pediatr Res. 2003;54:306–11. doi: 10.1203/01.PDR.0000076666.16021.5E. [DOI] [PubMed] [Google Scholar]
- 164.Fagundes Neto U, Martins MC, Lima FL, Patricio FR, Toledo MR. Asymptomatic environmental enteropathy among slum-dwelling infants. J Am Coll Nutr. 1994;13:51–6. doi: 10.1080/07315724.1994.10718371. [DOI] [PubMed] [Google Scholar]
- 165.Roy SK, Behrens RH, Haider R, Akramuzzaman SM, Mahalanabis D, Wahed MA, et al. Impact of zinc supplementation on intestinal permeability in Bangladeshi children with acute diarrhoea and persistent diarrhoea syndrome. J Pediatr Gastroenterol Nutr. 1992;15:289–96. doi: 10.1097/00005176-199210000-00010. [DOI] [PubMed] [Google Scholar]
- 166.Lunn PG, Northrop-Clewes CA, Downes RM. Intestinal permeability, mucosal injury, and growth faltering in Gambian infants. Lancet. 1991;338:907–10. doi: 10.1016/0140-6736(91)91772-m. [DOI] [PubMed] [Google Scholar]
- 167.Kosek M, Haque R, Lima A, Babji S, Shrestha S, Qureshi S, et al. Fecal markers of intestinal inflammation and permeability associated with the subsequent acquisition of linear growth deficits in infants. Am J Trop Med Hyg. 2013;88:390–6. doi: 10.4269/ajtmh.2012.12-0549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Lin A, Arnold BF, Afreen S, Goto R, Huda TM, Haque R, et al. Household environmental conditions are associated with enteropathy and impaired growth in rural Bangladesh. Am J Trop Med Hyg. 2013;89:130–7. doi: 10.4269/ajtmh.12-0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Liu JR, Sheng XY, Hu YQ, Yu XG, Westcott JE, Miller LV, et al. Fecal calprotectin levels are higher in rural than in urban Chinese infants and negatively associated with growth. BMC Pediatr. 201212129.doi: 10.1186/1471-2431-12-129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Korpe PS, Petri WA., Jr Environmental enteropathy: critical implications of a poorly understood condition. Trends Mol Med. 2012;18:328–36. doi: 10.1016/j.molmed.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Prendergast A, Kelly P. Review: Enteropathies in the developing world: neglected effects on global health. Am J Trop Med Hyg. 2012;86:756–63. doi: 10.4269/ajtmh.2012.11-0743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ahmed T, Auble D, Berkley JA, Black R, Ahern PP, Hossain M, et al. An evolving perspective about the origins of childhood undernutrition and nutritional interventions that includes the gut microbiome. Ann N Y Acad Sci. 2014 doi: 10.1111/nyas.12487. doi: 10.1111/nyas.12487 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, et al. Human gut microbiome viewed across age and geography. Nature. 2012;486:222–7. doi: 10.1038/nature11053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ley RE, Hamady M, Lozupone C, Turnbaugh PJ, Ramey RR, Bircher JS, et al. Evolution of mammals and their gut microbes. Science. 2008;320:1647–51. doi: 10.1126/science.1155725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Muegge BD, Kuczynski J, Knights D, Clemente JC, Gonzalez A, Fontana L, et al. Diet drives convergence in gut microbiome functions across mammalian phylogeny and within humans. Science. 2011;332:970–4. doi: 10.1126/science.1198719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Wu GD, Chen J, Hoffmann C, Bittinger K, Chen YY, Keilbaugh SA, et al. Linking long-term dietary patterns with gut microbial enterotypes. Science. 2011;334:105–8. doi: 10.1126/science.1208344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Smith MI, Yatsunenko T, Manary MJ, Trehan I, Mkakosya R, Cheng J, et al. Gut microbiomes of Malawian twin pairs discordant for kwashiorkor. Science. 2013;339:548–54. doi: 10.1126/science.1229000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Subramanian S, Huq S, Yatsunenko T, Haque R, Mahfuz M, Alam MA, et al. Persistent gut microbiota immaturity in malnourished Bangladeshi children. Nature. 2014;510:417–21. doi: 10.1038/nature13421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Gough EK, Moodie EEM, Prendergast AJ, Johnson SMA, Humphrey JH, Stoltzfus RJ, et al. The impact of antibiotics on growth in children in developing countries: a systematic review and meta-analysis of randomized controlled trials. Br Med J (in press) 2014. doi: 10.1136/bmj.g2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Porco TC, Gebre T, Ayele B, House J, Keenan J, Zhou Z, et al. Effect of mass distribution of azithromycin for trachoma control on overall mortality in Ethiopian children: a randomized trial. JAMA. 2009;302:962–8. doi: 10.1001/jama.2009.1266. [DOI] [PubMed] [Google Scholar]
- 181.Amza A, Kadri B, Nassirou B, Stoller NE, Yu SN, Zhou Z, et al. A cluster-randomized controlled trial evaluating the effects of mass azithromycin treatment on growth and nutrition in Niger. Am J Trop Med Hyg. 2013;88:138–43. doi: 10.4269/ajtmh.2012.12-0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Trehan I, Shulman RJ, Ou CN, Maleta K, Manary MJ. A randomized, double-blind, placebo-controlled trial of rifaximin, a nonabsorbable antibiotic, in the treatment of tropical enteropathy. Am J Gastroenterol. 2009;104:2326–33. doi: 10.1038/ajg.2009.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Ryan KN, Stephenson KB, Trehan I, Shulman RJ, Thakwalakwa C, Murray E, et al. Zinc or albendazole attenuates the progression of environmental enteropathy: a randomized controlled trial. Clin Gastroenterol Hepatol. 2014;12:1507–13. doi: 10.1016/j.cgh.2014.01.024. [DOI] [PubMed] [Google Scholar]
- 184.Braegger C, Chmielewska A, Decsi T, Kolacek S, Mihatsch W, Moreno L, et al. Supplementation of infant formula with probiotics and/or prebiotics: a systematic review and comment by the ESPGHAN committee on nutrition. J Pediatr Gastroenterol Nutr. 2011;52:238–50. doi: 10.1097/MPG.0b013e3181fb9e80. [DOI] [PubMed] [Google Scholar]
- 185.Saran S, Gopalan S, Krishna TP. Use of fermented foods to combat stunting and failure to thrive. Nutrition. 2002;18:393–6. doi: 10.1016/s0899-9007(01)00790-0. [DOI] [PubMed] [Google Scholar]
- 186.Silva MR, Dias G, Ferreira CL, Franceschini SC, Costa NM. Growth of preschool children was improved when fed an iron-fortified fermented milk beverage supplemented with Lactobacillus acidophilus. Nutr Res. 2008;28:226–32. doi: 10.1016/j.nutres.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 187.Sazawal S, Dhingra U, Hiremath G, Sarkar A, Dhingra P, Dutta A, et al. Effects of Bifidobacterium lactis HN019 and prebiotic oligosaccharide added to milk on iron status, anemia, and growth among children 1 to 4 years old. J Pediat Gastroenterol Nutr. 2010;51:341–6. doi: 10.1097/MPG.0b013e3181d98e45. [DOI] [PubMed] [Google Scholar]
- 188.Agustina R, Bovee-Oudenhoven IM, Lukito W, Fahmida U, van de Rest O, Zimmermann MB, et al. Probiotics Lactobacillus reuteri DSM 17938 and Lactobacillus casei CRL 431 modestly increase growth, but not iron and zinc status, among Indonesian children aged 1–6 years. J Nutr. 2013;143:1184–93. doi: 10.3945/jn.112.166397. [DOI] [PubMed] [Google Scholar]
- 189.Galpin L, Manary MJ, Fleming K, Ou CN, Ashorn P, Shulman RJ. Effect of Lactobacillus GG on intestinal integrity in Malawian children at risk of tropical enteropathy. Am J Clin Nutr. 2005;82:1040–5. doi: 10.1093/ajcn/82.5.1040. [DOI] [PubMed] [Google Scholar]
- 190.Jones KDJ, Hunten-Kirsch B, Laving AMR, Munyi CW, Ngari M, Mikusa J, et al. Mesalazine in the initial management of severely acutely malnourished children with environmental enteric dysfunction: a pilot randomized controlled trial. BMC Med. 201412133 doi: 10.1186/s12916-014-0133-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM., Jr Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis. 2005;5:42–52. doi: 10.1016/S1473-3099(04)01253-8. [DOI] [PubMed] [Google Scholar]
- 192.Strunz EC, Addiss DG, Stocks ME, Ogden S, Utzinger J, Freeman MC. Water, sanitation, hygiene, and soil-transmitted helminth infection: a systematic review and meta-analysis. PLoS Med. 2014;11:e1001620. doi: 10.1371/journal.pmed.1001620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Spears D. How Much International Variation in Child Height can Sanitation Explain? World Bank, 2013; Policy Research Working Paper no. WPS 6351. Available from: http://econ.worldbank.org/external/default/main?pagePK = 64165259&theSitePK = 469382&piPK = 64165421&menuPK = 64166093&entityID = 000158349_20130205082533. [Google Scholar]
- 194.Daniels DL, Cousens SN, Makoae LN, Feachem RG. A study of the association between improved sanitation facilities and children's height in Lesotho. Eur J Clin Nutr. 1991;45:23–32. [PubMed] [Google Scholar]
- 195.Fink G, Gunther I, Hill K. The effect of water and sanitation on child health: evidence from the demographic and health surveys 1986–2007. Int J Epidemiol. 2011;40:1196–1204. doi: 10.1093/ije/dyr102. [DOI] [PubMed] [Google Scholar]
- 196.Garcia S, Sarmiento OL, Forde I, Velasco T. Socio-economic inequalities in malnutrition among children and adolescents in Colombia: the role of individual-, household- and community-level characteristics. Public Health Nutr. 2013;16:1703–18. doi: 10.1017/S1368980012004090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Masibo PK, Makoka D. Trends and determinants of undernutrition among young Kenyan children: Kenya Demographic and Health Survey: 1993, 1998, 2003 and 2008–2009. Public Health Nutr. 2012;15:1715–27. doi: 10.1017/S1368980012002856. [DOI] [PubMed] [Google Scholar]
- 198.Merchant AT, Jones C, Kiure A, Kupka R, Fitzmaurice G, Herrera MG, et al. Water and sanitation associated with improved child growth. Eur J Clin Nutr. 2003;57:1562–8. doi: 10.1038/sj.ejcn.1601725. [DOI] [PubMed] [Google Scholar]
- 199.Spears D, Ghosh A, Cumming O. Open defecation and childhood stunting in India: an ecological analysis of new data from 112 districts. PLoS One. 2013;8:e73784. doi: 10.1371/journal.pone.0073784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Dangour AD, Watson L, Cumming O, Boisson S, Che Y, Velleman Y, et al. Interventions to improve water quality and supply, sanitation and hygiene practices, and their effects on the nutritional status of children. Cochrane Database Syst Rev. 2013;8:CD009382. doi: 10.1002/14651858.CD009382.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Ngure FM, Reid BM, Humphrey JH, Mbuya MN, Pelto G, Stoltzfus RJ. Water, sanitation, and hygiene (WASH), environmental enteropathy, nutrition, and early child development: making the links. Ann N Y Acad Sci. 2014;1308:118–28. doi: 10.1111/nyas.12330. [DOI] [PubMed] [Google Scholar]
- 202.Ngure FM, Humphrey JH, Mbuya MN, Majo F, Mutasa K, Govha M, et al. Formative research on hygiene behaviors and geophagy among infants and young children and implications of exposure to fecal bacteria. Am J Trop Med Hyg. 2013;89:709–16. doi: 10.4269/ajtmh.12-0568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.World Health Organization. Dufour A, Bartram J, Bos R, Gannon V, eds. Animal Waste, Water Quality and Human Health. WHO: IWA Publishing; 2012. p. ISBN 9781780401232. [Google Scholar]
- 204.Berrilli F, D'Alfonso R, Giangaspero A, Marangi M, Brandonisio O, Kabore Y, et al. Giardia duodenalis genotypes and Cryptosporidium species in humans and domestic animals in Cote d'Ivoire: occurrence and evidence for environmental contamination. Trans R Soc Trop Med Hyg. 2012;106:191–5. doi: 10.1016/j.trstmh.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 205.Etzel RA. Reducing malnutrition: time to consider potential links between stunting and mycotoxin exposure? Pediatrics. 2014;134:4–6. doi: 10.1542/peds.2014-0827. [DOI] [PubMed] [Google Scholar]
- 206.Gong YY, Cardwell K, Hounsa A, Egal S, Turner PC, Hall AJ, et al. Dietary aflatoxin exposure and impaired growth in young children from Benin and Togo: cross sectional study. Br Med J. 2002;325:20–1. doi: 10.1136/bmj.325.7354.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Kimanya ME, De Meulenaer B, Van Camp J, Baert K, Kolsteren P. Strategies to reduce exposure of fumonisins from complementary foods in rural Tanzania. Matern Child Nutr. 2012;8:503–11. doi: 10.1111/j.1740-8709.2011.00337.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Smith LE, Stoltzfus RJ, Prendergast A. Food chain mycotoxin exposure, gut health, and impaired growth: a conceptual framework. Adv Nutr. 2012;3:526–31. doi: 10.3945/an.112.002188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Rahman A, Vahter M, Smith AH, Nermell B, Yunus M, El Arifeen S, et al. Arsenic exposure during pregnancy and size at birth: a prospective cohort study in Bangladesh. Am J Epidemiol. 2009;169:304–12. doi: 10.1093/aje/kwn332. [DOI] [PubMed] [Google Scholar]
- 210.Ahmed S, Rekha RS, Ahsan KB, Doi M, Grander M, Roy AK, et al. Arsenic exposure affects plasma insulin-like growth factor 1 (IGF-1) in children in rural Bangladesh. PLoS One. 2013;8:e81530. doi: 10.1371/journal.pone.0081530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Kyu HH, Georgiades K, Boyle MH. Maternal smoking, biofuel smoke exposure and child height-for-age in seven developing countries. Int J Epidemiol. 2009;38:1342–50. doi: 10.1093/ije/dyp253. [DOI] [PubMed] [Google Scholar]
- 212.Tielsch JM, Katz J, Thulasiraj RD, Coles CL, Sheeladevi S, Yanik EL, et al. Exposure to indoor biomass fuel and tobacco smoke and risk of adverse reproductive outcomes, mortality, respiratory morbidity and growth among newborn infants in south India. Int J Epidemiol. 2009;38:1351–63. doi: 10.1093/ije/dyp286. [DOI] [PubMed] [Google Scholar]
- 213.Machisa M, Wichmann J, Nyasulu PS. Biomass fuel use for household cooking in Swaziland: is there an association with anaemia and stunting in children aged 6-36 months? Trans R Soc Trop Med Hyg. 2013;107:535–44. doi: 10.1093/trstmh/trt055. [DOI] [PubMed] [Google Scholar]
- 214.Prentice AM, Ward KA, Goldberg GR, Jarjou LM, Moore SE, Fulford AJ, et al. Critical windows for nutritional interventions against stunting. Am J Clin Nutr. 2013;97:911–18. doi: 10.3945/ajcn.112.052332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Lundeen EA, Behrman JR, Crookston BT, Dearden KA, Engle P, Georgiadis A, et al. Growth faltering and recovery in children aged 1–8 years in four low- and middle-income countries: Young Lives. Public Health Nutr. 2013:1–7.(Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Fink G, Rockers PC. Childhood growth, schooling, and cognitive development: further evidence from the Young Lives study. Am J Clin Nutr. 2014;100:182–8. doi: 10.3945/ajcn.113.080960. [DOI] [PubMed] [Google Scholar]
- 217.Schott WB, Crookston BT, Lundeen EA, Stein AD, Behrman JR. Periods of child growth up to age 8 years in Ethiopia, India, Peru and Vietnam: key distal household and community factors. Soc Sci Med. 2013;97:278–87. doi: 10.1016/j.socscimed.2013.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Leroy JL, Ruel M, Habicht JP. Critical windows for nutritional interventions against stunting. Am J Clin Nutr. 2013;98:854–5. doi: 10.3945/ajcn.113.066647. [DOI] [PubMed] [Google Scholar]
- 219.Lundeen EA, Stein AD, Adair LS, Behrman JR, Bhargava SK, Dearden KA, et al. Height-for-age z scores increase despite increasing height deficits among children in 5 developing countries. Am J Clin Nutr. 2014;100:821–5. doi: 10.3945/ajcn.114.084368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Leroy JL, Ruel M, Habicht JP, Frongillo EA. Linear growth deficit continues to accumulate beyond the rirst 1000 days in low- and middle-income countries: global evidence from 51 national surveys. J Nutr. 2014;144:1460–6. doi: 10.3945/jn.114.191981. [DOI] [PubMed] [Google Scholar]
- 221.Coly AN, Milet J, Diallo A, Ndiaye T, Benefice E, Simondon F, et al. Preschool stunting, adolescent migration, catch-up growth, and adult height in young senegalese men and women of rural origin. J Nutr. 2006;136:2412–20. doi: 10.1093/jn/136.9.2412. [DOI] [PubMed] [Google Scholar]
- 222.Golden MH. Is complete catch-up possible for stunted malnourished children? Eur J Clin Nutr. 1994;48((suppl 1)):S58–70. discussion S71. [PubMed] [Google Scholar]
- 223.Kossmann J, Nestel P, Herrera MG, El Amin A, Fawzi WW. Undernutrition in relation to childhood infections: a prospective study in the Sudan. Eur J Clin Nutr. 2000;54:463–72. doi: 10.1038/sj.ejcn.1600998. [DOI] [PubMed] [Google Scholar]
- 224.Olofin I, McDonald CM, Ezzati M, Flaxman S, Black RE, Fawzi WW, et al. Associations of suboptimal growth with all-cause and cause-specific mortality in children under five years: a pooled analysis of ten prospective studies. PLoS One. 2013;8:e64636. doi: 10.1371/journal.pone.0064636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Pelletier DL, Frongillo EA, Jr, Schroeder DG, Habicht JP. The effects of malnutrition on child mortality in developing countries. Bull WHO. 1995;73:443–8. [PMC free article] [PubMed] [Google Scholar]
- 226.Rytter MJ, Kolte L, Briend A, Friis H, Christensen VB. The immune system in children with malnutrition-a systematic review. PLoS One. 2014;9:e105017. doi: 10.1371/journal.pone.0105017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Walker SP, Wachs TD, Grantham-McGregor S, Black MM, Nelson CA, Huffman SL, et al. Inequality in early childhood: risk and protective factors for early child development. Lancet. 2011;378:1325–38. doi: 10.1016/S0140-6736(11)60555-2. [DOI] [PubMed] [Google Scholar]
- 228.Lasky RE, Klein RE, Yarbrough C, Engle PL, Lechtig A, Martorell R. The relationship between physical growth and infant behavioral development in rural Guatemala. Child Dev. 1981;52:219–26. [PubMed] [Google Scholar]
- 229.Beasley NM, Hall A, Tomkins AM, Donnelly C, Ntimbwa P, Kivuga J, et al. The health of enrolled and non enrolled children of school age in Tanga, Tanzania. Acta Trop. 2000;76:223–9. doi: 10.1016/s0001-706x(00)00101-7. [DOI] [PubMed] [Google Scholar]
- 230.Moock PR, Lesiie J. Childhood malnutrition and schooling in the Terri region of Nepal. J Dev Econ. 1986;20:33–52. [Google Scholar]
- 231.Jamison D. Child malnutrition and school performance in China. J Dev Econ. 1986;20:299–309. [Google Scholar]
- 232.Casale D, Desmond C, Richter L.The association between stunting and psychosocial development among preschool children: a study using the South African Birth to Twenty cohort data. Child Care Health Dev. 2014doi: 10.1111/cch.12143 [DOI] [PubMed] [Google Scholar]
- 233.Crookston BT, Schott W, Cueto S, Dearden KA, Engle P, Georgiadis A, et al. Postinfancy growth, schooling, and cognitive achievement: Young Lives. Am J Clin Nutr. 2013;98:1555–63. doi: 10.3945/ajcn.113.067561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Sandjaja, Poh BK, Rojroonwasinkul N, Le Nyugen BK, Budiman B, Ng LO, et al. Relationship between anthropometric indicators and cognitive performance in Southeast Asian school-aged children. Br J Nutr. 2013110(Suppl 3)S57–64. [DOI] [PubMed] [Google Scholar]
- 235.Webb KE, Horton NJ, Katz DL. Parental IQ and cognitive development of malnourished Indonesian children. Eur J Clin Nutr. 2005;59:618–20. doi: 10.1038/sj.ejcn.1602103. [DOI] [PubMed] [Google Scholar]
- 236.Gardner JM, Grantham-McGregor SM, Himes J, Chang S. Behaviour and development of stunted and nonstunted Jamaican children. J Child Psychol Psychiatry. 1999;40:819–27. doi: 10.1111/1469-7610.00497. [DOI] [PubMed] [Google Scholar]
- 237.Fernald LC, Grantham-McGregor SM. Stress response in school-age children who have been growth retarded since early childhood. Am J Clin Nutr. 1998;68:691–8. doi: 10.1093/ajcn/68.3.691. [DOI] [PubMed] [Google Scholar]
- 238.Walker SP, Chang SM, Powell CA, Simonoff E, Grantham-McGregor SM. Early childhood stunting is associated with poor psychological functioning in late adolescence and effects are reduced by psychosocial stimulation. J Nutr. 2007;137:2464–9. doi: 10.1093/jn/137.11.2464. [DOI] [PubMed] [Google Scholar]
- 239.Levitsky DA, Strupp BJ. Malnutrition and the brain: changing concepts, changing concerns. J Nutr. 1995;125:2212–20S. doi: 10.1093/jn/125.suppl_8.2212S. [DOI] [PubMed] [Google Scholar]
- 240.Ranade SC, Rose A, Rao M, Gallego J, Gressens P, Mani S. Different types of nutritional deficiencies affect different domains of spatial memory function checked in a radial arm maze. Neuroscience. 2008;152:859–66. doi: 10.1016/j.neuroscience.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 241.Benitez-Bribiesca L, De la Rosa-Alvarez I, Mansilla-Olivares A. Dendritic spine pathology in infants with severe protein-calorie malnutrition. Pediatrics. 1999;104:e21. doi: 10.1542/peds.104.2.e21. [DOI] [PubMed] [Google Scholar]
- 242.Rosenberg M. Global child health: burden of disease, achievements, and future challenges. Curr Probl Pediatr Adolesc Health Care. 2007;37:338–62. doi: 10.1016/j.cppeds.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 243.Stein AD, Wang M, DiGirolamo A, Grajeda R, Ramakrishnan U, Ramirez-Zea M, et al. Nutritional supplementation in early childhood, schooling, and intellectual functioning in adulthood: a prospective study in Guatemala. Arch Pediatr Adolesc Med. 2008;162:612–18. doi: 10.1001/archpedi.162.7.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Adair LS, Fall CH, Osmond C, Stein AD, Martorell R, Ramirez-Zea M, et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. Lancet. 2013;382:525–34. doi: 10.1016/S0140-6736(13)60103-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Crookston BT, Penny ME, Alder SC, Dickerson TT, Merrill RM, Stanford JB, et al. Children who recover from early stunting and children who are not stunted demonstrate similar levels of cognition. J Nutr. 2010;140:1996–2001. doi: 10.3945/jn.109.118927. [DOI] [PubMed] [Google Scholar]
- 246.Crookston BT, Dearden KA, Alder SC, Porucznik CA, Stanford JB, Merrill RM, et al. Impact of early and concurrent stunting on cognition. Matern Child Nutr. 2011;7:397–409. doi: 10.1111/j.1740-8709.2010.00255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Cheung YB, Ashorn P. Continuation of linear growth failure and its association with cognitive ability are not dependent on initial length-for-age: a longitudinal study from 6 months to 11 years of age. Acta Paediatr. 2010;99:1719–23. doi: 10.1111/j.1651-2227.2009.01593.x. [DOI] [PubMed] [Google Scholar]
- 248.Moore SE, Cole TJ, Collinson AC, Poskitt EM, McGregor IA, Prentice AM. Prenatal or early postnatal events predict infectious deaths in young adulthood in rural Africa. Int J Epidemiol. 1999;28:1088–95. doi: 10.1093/ije/28.6.1088. [DOI] [PubMed] [Google Scholar]
- 249.Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;371:340–57. doi: 10.1016/S0140-6736(07)61692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Hoddinott J, Maluccio JA, Behrman JR, Flores R, Martorell R. Effect of a nutrition intervention during early childhood on economic productivity in Guatemalan adults. Lancet. 2008;371:411–16. doi: 10.1016/S0140-6736(08)60205-6. [DOI] [PubMed] [Google Scholar]
- 251.Hoddinott J, Alderman H, Behrman JR, Haddad L, Horton S.The economic rationale for investing in stunting reduction. Matern Child Nutr. 20139 (Suppl 2):69–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Barker DJ, Hales CN, Fall CH, Osmond C, Phipps K, Clark PM. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): relation to reduced fetal growth. Diabetologia. 1993;36:62–7. doi: 10.1007/BF00399095. [DOI] [PubMed] [Google Scholar]
- 253.Barker DJ, Martyn CN, Osmond C, Hales CN, Fall CH. Growth in utero and serum cholesterol concentrations in adult life. Br Med J. 1993;307:1524–7. doi: 10.1136/bmj.307.6918.1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Barker DJ, Osmond C, Golding J, Kuh D, Wadsworth ME. Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. Br Med J. 1989;298:564–7. doi: 10.1136/bmj.298.6673.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Cheung YF, Taylor MJ, Fisk NM, Redington AN, Gardiner HM. Fetal origins of reduced arterial distensibility in the donor twin in twin-twin transfusion syndrome. Lancet. 2000;355:1157–8. doi: 10.1016/s0140-6736(00)02068-7. [DOI] [PubMed] [Google Scholar]
- 256.Ozanne SE. Metabolic programming in animals. Br Med Bull. 2001;60:143–52. doi: 10.1093/bmb/60.1.143. [DOI] [PubMed] [Google Scholar]
- 257.Mackenzie HS, Brenner BM. Fewer nephrons at birth: a missing link in the etiology of essential hypertension? Am J Kidney Dis. 1995;26:91–8. doi: 10.1016/0272-6386(95)90161-2. [DOI] [PubMed] [Google Scholar]
- 258.Sachdev HS, Fall CH, Osmond C, Lakshmy R, Dey Biswas SK, Leary SD, et al. Anthropometric indicators of body composition in young adults: relation to size at birth and serial measurements of body mass index in childhood in the New Delhi birth cohort. Am J Clin Nutr. 2005;82:456–66. doi: 10.1093/ajcn.82.2.456. [DOI] [PubMed] [Google Scholar]
- 259.Moore SE, Halsall I, Howarth D, Poskitt EM, Prentice AM. Glucose, insulin and lipid metabolism in rural Gambians exposed to early malnutrition. Diabet Med. 2001;18:646–53. doi: 10.1046/j.1464-5491.2001.00565.x. [DOI] [PubMed] [Google Scholar]
- 260.Huxley RR, Shiell AW, Law CM. The role of size at birth and postnatal catch-up growth in determining systolic blood pressure: a systematic review of the literature. J Hypertens. 2000;18:815–31. doi: 10.1097/00004872-200018070-00002. [DOI] [PubMed] [Google Scholar]
- 261.Hardy R, Sovio U, King VJ, Skidmore PM, Helmsdal G, Olsen SF, et al. Birthweight and blood pressure in five European birth cohort studies: an investigation of confounding factors. Eur J Public Health. 2006;16:21–30. doi: 10.1093/eurpub/cki171. [DOI] [PubMed] [Google Scholar]
- 262.Fanzo JC, Pronyk PM. A review of global progress toward the Millennium Development Goal 1 Hunger Target. Food Nutr Bull. 2011;32:144–58. doi: 10.1177/156482651103200207. [DOI] [PubMed] [Google Scholar]
- 263.Adekanmbi VT, Uthman OA, Mudasiru OM.Exploring variations in childhood stunting in Nigeria using league table, control chart and spatial analysis. BMC Public Health. 201313361.doi: 10.1186/1471-2458-13-361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Amugsi DA, Mittelmark MB, Lartey A.An analysis of socio-demographic patterns in child malnutrition trends using Ghana demographic and health survey data in the period 1993-2008. BMC Public Health. 201313960.doi: 10.1186/1471-2458-13-960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Carrera C, Azrack A, Begkoyian G, Pfaffmann J, Ribaira E, O'Connell T, et al. The comparative cost-effectiveness of an equity-focused approach to child survival, health, and nutrition: a modelling approach. Lancet. 2012;380:1341–51. doi: 10.1016/S0140-6736(12)61378-6. [DOI] [PubMed] [Google Scholar]
- 266.Sunguya BF, Ong KI, Dhakal S, Mlunde LB, Shibanuma A, Yasuoka J, et al. Strong nutrition governance is a key to addressing nutrition transition in low and middle-income countries: review of countries' nutrition policies. Nutr J. 20141365 doi: 10.1186/1475-2891-13-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Casanovas Mdel C, Lutter CK, Mangasaryan N, Mwadime R, Hajeebhoy N, Aguilar AM, et al. Multi-sectoral interventions for healthy growth. Matern Child Nutr. 20139(suppl 2)46–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Pronyk PM, Muniz M, Nemser B, Somers MA, McClellan L, Palm CA, et al. The effect of an integrated multisector model for achieving the Millennium Development Goals and improving child survival in rural sub-Saharan Africa: a non-randomised controlled assessment. Lancet. 2012;379:2179–88. doi: 10.1016/S0140-6736(12)60207-4. [DOI] [PubMed] [Google Scholar]
- 269.Remans R, Pronyk PM, Fanzo JC, Chen J, Palm CA, Nemser B, et al. Multisector intervention to accelerate reductions in child stunting: an observational study from 9 sub-Saharan African countries. Am J Clin Nutr. 2011;94:1632–42. doi: 10.3945/ajcn.111.020099. [DOI] [PubMed] [Google Scholar]
- 270.Milman A, Frongillo EA, de Onis M, Hwang JY. Differential improvement among countries in child stunting is associated with long-term development and specific interventions. J Nutr. 2005;135:1415–22. doi: 10.1093/jn/135.6.1415. [DOI] [PubMed] [Google Scholar]
- 271.Victora CG, Aquino EM, do Carmo Leal M, Monteiro CA, Barros FC, Szwarcwald CL. Maternal and child health in Brazil: progress and challenges. Lancet. 2011;377:1863–76. doi: 10.1016/S0140-6736(11)60138-4. [DOI] [PubMed] [Google Scholar]