Abstract
Background:
With changing trends in treatment of displaced midshaft clavicle fractures (DMCF), plating remains the standard procedure for fixation. An attracting alternative method of fixation is the titanium elastic nailing (TEN). However, prospective randomized studies comparing the two methods of fixation are lacking. We assessed the effectiveness of minimally invasive antegrade TEN and plating technique for the treatment of DMCF.
Materials and Methods:
80 unilateral displaced midclavicular fractures operated between October 2010 and May 2013 were included in study. This prospective comparative study was approved by the local ethical committee. Followups were at 2nd and 6th weeks and subsequently at 3, 6, 12, 18 and 24 months postoperatively. Primary outcome was measured by the Constant score, union rate and difference in clavicular length after fracture union. Secondary outcome was measured by operative time, intraoperative blood loss, wound size, cosmetic results and complications.
Results:
During analysis, we had 37 patients in the plate group and 34 patients in the TEN group. There was no significant difference in Constant scores between the two groups. However, faster fracture union, lesser operative time, lesser blood loss, easier implant removal and fewer complications were noted in the TEN group.
Conclusion:
The use of minimally invasive antegrade TEN for fixation of displaced midshaft clavicle fractures is recommended in view of faster fracture union, lesser morbidity, better cosmetic results, easier implant removal and fewer complications; although for comminuted fractures plating remains the procedure of choice.
Keywords: Clavicle fractures, internal fixation of clavicle fractures, plate, titanium elastic nailing
MeSH terms: Fractures, clavicle, fracture fixation, internal, bone plates, intramedullary nailing
INTRODUCTION
Fractures of the clavicle are common injuries with an incidence of 2.6-10% of all fractures.1 About 80% fractures involve the midshaft and over half of these fractures are displaced.2,3 Traditionally, the midshaft clavicle fractures have been treated conservatively with a sling or figure-of-eight bandage.4,5,6
Functional outcome of midshaft clavicle fractures is not only related to its union, but also to its length.7 Clavicle acts as a “strut”, that keeps the upper limb away from the torso for efficient shoulder and upper limb function, while also transmitting forces from upper limb to the trunk. Thus, displaced or comminuted fractures carry a risk of symptomatic malunion, nonunion and poor functional outcome with cosmetic deformity.8,9,10 The recent trend is shifting towards internal fixation of these displaced midshaft clavicle fractures (DMCF).7,9,10,11,12,13
Two operative techniques are commonly used for internal fixation of DMCF: Plate fixation and intramedullary nailing with a titanium elastic nail (TEN).14 Functional results after both the techniques proved to be superior compared with conservative treatment of DMCF in some recently reported prospective randomized studies.8,15 Moreover, a recent meta-analysis revealed a significant lower nonunion rate after surgical treatment.13
However, prospective randomized studies comparing the two operative techniques for treatment of DMCF were lacking.16 The aim of this study was to assess the effectiveness of minimally invasive antegrade TEN for the treatment of DMCF and to compare its outcome with that of a standard anterosuperior plating technique.
MATERIALS AND METHODS
80 unilateral displaced midclavicular fractures operated between October 2010 and May 2013 were included in study. This prospective comparative study was approved by the local ethical committee. Inclusion criteria for this study were unilateral DMCFs (AO classification B1 and B2) with a displacement of more than shaft width, shortening by over 2 cm or threat of skin perforation at the fracture ends. Our exclusion criteria were (1) Patients with preexistent morbidity concerning arm, shoulder or hand (2) moderate to severe head injury (Glasgow coma scale <12) (3) multitrauma patients (4) open fractures (5) pathological fractures (6) fractures of >1 month duration (7) bilateral clavicle fractures (8) segmental fracture (9) fractures with associated neurovascular injury.
Allocation into plate fixation group or TEN fixation group was done alternatively (i.e. every even number patient underwent TEN fixation). Thus, each group was allocated 40 patients each. All the patients were operated within 4 weeks from the date of injury.
Operative procedure
(a) Plate fixation
After anesthesia, patients were positioned in a “beach-chair semi sitting” position. Involved shoulders were prepared and draped free. Incision was made transversely just under the fracture site. Supra clavicular nerves were identified and spared wherever possible. Soft tissue dissection was kept to a minimum. After reduction of fractures, a small fragment locking plate was fixed on the anterosuperior surface of the bone, starting medially using bicortical screws. In oblique or complex fractures, inter fragmentary lag screws were used to achieve compression [Figure 1]. The fascia and skin were closed in layers.
Figure 1.
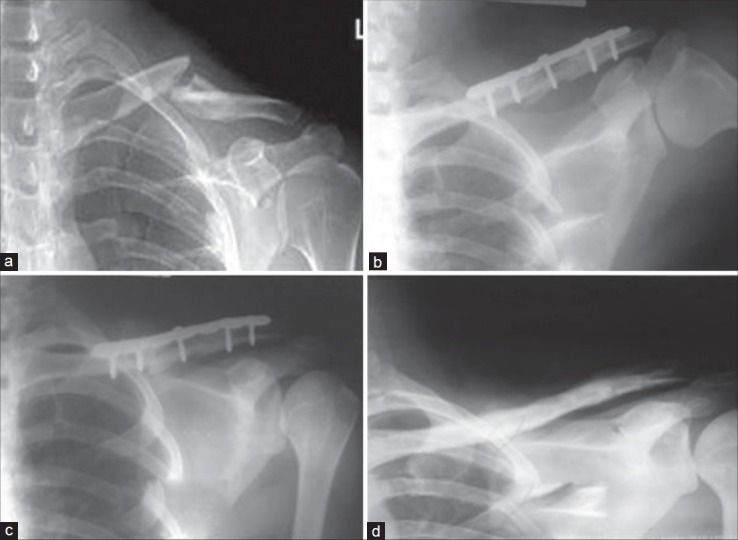
Skiagrams of a left clavicle of 20 years old male patient showing (a) midshaft clavicle fracture (b) immediate postoperative x-ray with plate in situ (c) 3 months postoperative with fracture union, (d) after implant removal
(b) TEN fixation
After anesthesia, patients were placed in supine position. The sternoclavicular joint was palpated and marked on the affected side. We used image intensification in 45°-cephalad and 45°-caudal directions. This provided us with images in two-planes, 90° apart. A small incision was made approximately 1 cm lateral to the sternoclavicular joint. The anterior cortex was opened using a sharp, pointed awl. A TEN was inserted (the diameter varied from 2 to 3 mm depending on the width of the bone). Before introduction, the original curvature of the small and flattened nail tip was straightened slightly to allow better gliding in the small medullary canal [Figure 2]. Closed reduction was performed under fluoroscopic control using two percutaneously introduced pointed reduction clamps [Figure 3]. If closed reduction failed, an additional incision (miniopen) was made above the fracture site for direct manipulation of the main fragments. The nail was then advanced manually until it was just medial to the acromioclavicular joint. Accurate maneuvering of the nail tip was necessary under fluoroscopic control to avoid penetration of the thin dorsal cortex. After reaching the end point, the fracture was compressed and the nail was cut close to the entry point to minimize soft tissue irritation, at the same time leaving sufficient length behind for easy extraction later on. The fascia and skin were closed in layers.
Figure 2.
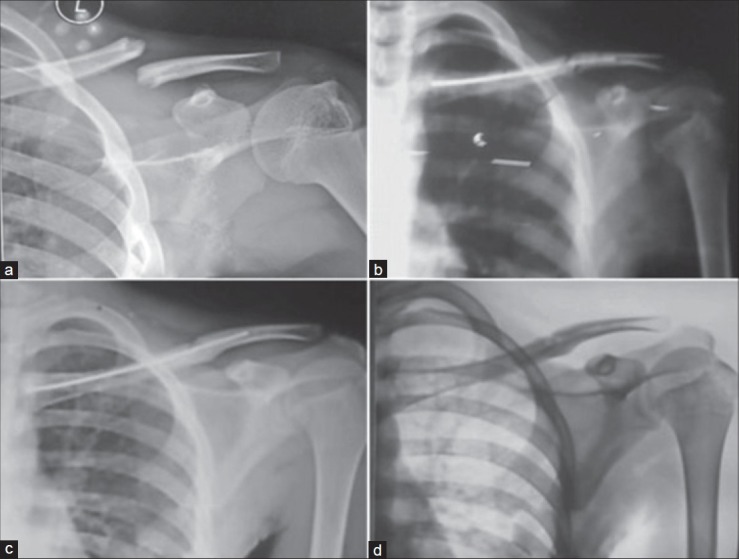
Skiagrams of left clavicle of a 15 years old male patient showing (a) clavicle fracture (b) immediate postoperative x-ray with IM TEN in situ (c) fracture united 3 months postoperatively, (d) after implant removal
Figure 3.
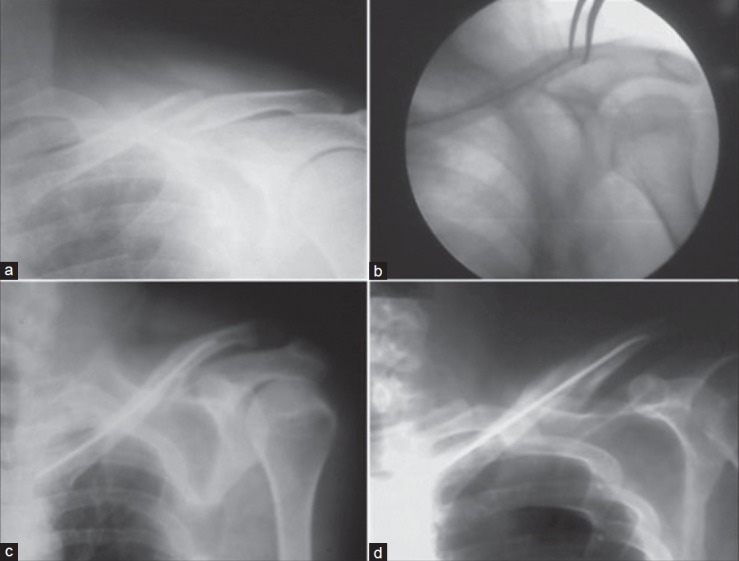
A 21 year old male patient with left clavicle fracture treated by titanium elastic nailing. (a) Preoperative x-ray showing fracture clavicle (b) peroperative fluoroscopic image showing closed reduction with percutaneous reduction clamps, (c) postoperative skiagram showing intramedullary implant (d) union achieved at 3 months postoperatively
Postoperatively, patients were given a sling, but were encouraged for early shoulder mobilization, (as tolerated), starting with pendular exercises from the second day. After 7 days, active range of movement exercises were started, however, overhead shoulder abduction was allowed only after 2 weeks. Activities of daily living were started thereafter, but those requiring lifting heavy objects were delayed until union was achieved. All patients were reviewed in the outpatient department at 2 and 6 weeks, 3, 6, 12, 18 and 24 months after surgery. At each visit, patients were assessed clinicoradiologically for primary and secondary outcome measures.
Functional outcome was assessed by the Constant score. Radiographic union was defined as evidence of bridging callus or obliteration of fracture lines. Clinical union was considered as absence of tenderness at the fracture site. Time to achieve union was recorded. After union, shortening of clavicular length was measured clinically as the linear difference of clavicle lengths from sternal end to acromial end between operated and normal side.
Secondary outcome measures include perioperative data like operative time, amount of blood loss and size of the surgical wound; complications such as neurovascular injury, wound infection, nonunion, malunion, implant migration, implant failure, soft tissue irritation, refracture after implant removal and cosmetic outcome with regards to visible deformity, hypertrophic scars and hardware prominence under the skin. Implant removal was not done routinely in our study. It was done as per need and will of the patient after fracture union. The number of days to return to normal activities after implant removal was noted.
Statistical analysis
During analysis of data, only those patients were considered who attended at least 4 of the 6 followup visits starting from 6 weeks after surgery. The differences between the two groups at the end of the followup period with regards to the primary and secondary outcome measures were evaluated for statistical significance using ‘independent group means comparison’ for analyzing the difference between the two proportions (P < 0.05 was considered significant). However, the data of our study has no external validity.
RESULTS
At the end of the study, we had 37 patients in the Plate group and 34 in the TEN group for comparison. In the Plate group, we had 30 male and 7 female patients, whereas there were 30 male and 4 female patients in the TEN group. The mean age was 33.03 ± 12.64 years (range 15-58 years) in the Plate group and 33.32 ± 11.84 years (range 15-55 years) in the TEN group. The trauma surgery delay was 12.84 ± 5.90 days (range 3-27 days) in the Plate group and 13.79 ± 5.90 days (range 4-27 days) in the TEN group. In the Plate group 19 patients had AO class B1 and 18 had AO class B2 fractures, whereas it was 21 B1 and 13 B2 in the TEN group. There was no significant difference between the two groups with respect to age (P = 0.92), sex (P = 0.41) and trauma to surgery delay (P = 0.5). Out of the 34 patients in the “TEN” group, a nail diameter of 2 mm was used in 6 patients, 2.5 mm in 20 patients and 3 mm in 8 patients. Closed reduction and nailing was achieved in 20 patients while the remaining 14 cases required open reduction (miniopen). The mean followup period was 25.12 ± 3.28 months (range 18-30 months) for the plate group and 24.60 ± 2.42 months (range 18-30 months) for the TEN group.
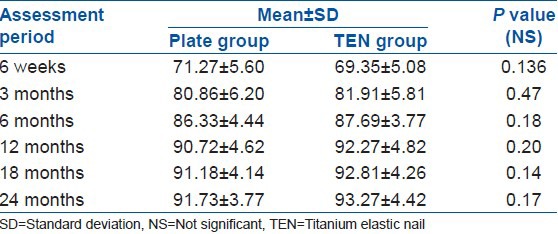
The constant scores were not significantly different between the two groups in the followup period [Table 1] and there was not much alteration after 1 year postoperatively. At final evaluation, the overall results using the constant score were 26 excellent, 9 good and 2 fair in the plate group; while in the TEN group it was 28 excellent and 6 good results.
Table 1.
Comparison of average constant scores
The average time to achieve union was significantly faster in the “TEN” group than in the “plate” group (P = 0.025). The mean difference of clavicular length after union was significantly higher in the ‘TEN’ group than in the “plate” group (P = 0.001) [Tables 2 and 3]. The mean operative time was significantly shorter in the TEN group than in the plate group (P < 0.001). The mean intraoperative blood loss was significantly lower in the TEN group than in the plate group (P < 0.001) [Table 2]. The average wound size was also much smaller in the TEN group (20 closed, 14 miniopen) than in the plate group.
Table 2.
Outcome comparisons
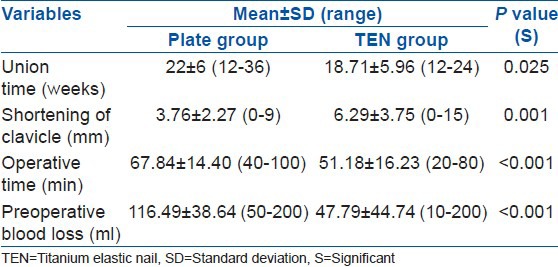
Table 3.
Comparison of clavicle length shortening (mm)
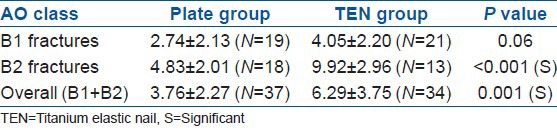
Complications
Major complications were noted in 5 patients [infection (n= 4) and nonunion (n = 1)] in the plate group, while none in the TEN group [Table 4]. Infections were controlled by debridement followed by intravenous antibiotics without removing the implants (as fixation was stable). The nonunion case in our series required revision surgery with bone grafting and healed thereafter uneventfully. In the plate group, subjective evaluation of cosmetic results was poor in 13 patients [ugly scar (n = 6), hardware prominence (n = 9)] [Figure 4] when compared to 12 patients in the TEN group [hypertrophic callus (n = 1) medial hardware prominence (n = 11) and lateral hardware prominence (n = 1)] [Figure 5].
Table 4.
Major and cosmetic complications
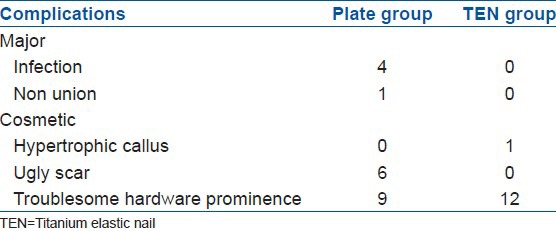
Figure 4.

Clinical photograph showing complications of plating in displaced midshaft clavicle fractures. (a) Prominent hardware, (b) ugly surgical scar
Figure 5.
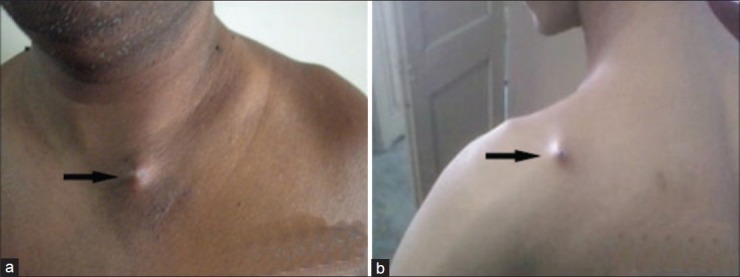
Clinical photograph showing complications of titanium elastic nailing in displaced midshaft clavicle fractures. (a) Medial hardware prominence, (b) lateral hardware prominence (black arrow)
DISCUSSION
Traditionally midshaft clavicle fractures had been treated nonoperatively. Neer4 and Rowe5 in the 1960's recommended conservative treatment for clavicular fractures in view of very small incidence of nonunion rates in their studies (0.1% and 0.8% respectively). No one has been able to reproduce these results so far. However, more recent studies have shown significantly higher nonunion rates in conservatively treated patients (ranging between 10% and 15%). Hence, current recommendation for treatment of displaced midshaft clavicle fractures is operative fixation.7,8,9,10,11,12,13 Plating is the standard operative procedure for DMCF. It can be done anterosuperiorly or anteroinferiorly. Another emerging mode of fixation is IM fixation with TENs (antegrade or retrograde). In this study, we compared the results of anterosuperior plating vs antegrade IM fixation with TEN.
In the plate group good to excellent results were achieved in 35 of 37 patients, compared with all good to excellent results in 34 patients of the TEN group. Overall, there were no unsatisfactory results in our study, whereas the incidence of unsatisfactory results after operative treatment of DMCFs is 5.3% in literature.17
The average time to achieve union in this study was significantly faster in the TEN group than in the plate group (P = 0.025). This can be explained by the less soft tissue dissection in the TEN group. The plating provides absolute stability resulting in primary bone healing, whereas TEN provides relative stability leading to secondary bone healing by callus formation.
Clavicular lengths were significantly better maintained by plating18 (P = 0.001) than by TEN in our study, especially in AO type-B2 fractures [Table 3]. However, this much of clavicular shortening does not affect functional outcome significantly, because as per Lazarides and Zafiropoulos, only final clavicular shortening of more than 18 mm in males and of more than 14 mm in females are significantly associated with unsatisfactory results.7 Eventually, in comminuted DMCF or those with large butterfly fragments plate fixation remains the operative procedure of choice as it offers better clavicular length maintenance.
We encountered 5 major complications in the plate group [infection (n = 4), nonunion (n = 1)]. The incidence of infection after plating in our study was 10.81%, whereas the reported rates in literature range from 0% to 18%.8,17
An important, although minor, complication of TEN group was the medial prominence of hardware [Figure 5] causing skin irritation or perforation, which was noted in 11 patients (32.35%). In the literature, it is reported to be in the range of 5.2-38.8%.15,19,20 Two causes for this problem are discussed in literature:7 Inadeuately cut medial end of the nail at primary surgery and nail displacement due to secondary clavicle shortening or telescoping. The first cause, being a surgeon related factor, may be tackled after primary surgery by adequately cutting the nail. The second cause is somewhat difficult to address however can be minimized by anatomical reduction, intraoperative compression and avoiding shoulder abduction beyond 90° in the first 2 weeks postoperatively.21 Another option for reducing medial protrusion is the use of medial end caps.20
The limitation of our study was a small sample size. However, from this study, we recommend the use of minimally invasive antegrade TEN for fixation of displaced midshaft clavicle fractures in view of faster fracture union, lesser morbidity, easier implant removal and fewer complications; although for comminuted fractures plating remains the procedure of choice.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.O’Neill BJ, Hirpara KM, O’Briain D, McGarr C, Kaar TK. Clavicle fractures: A comparison of five classification systems and their relationship to treatment outcomes. Int Orthop. 2011;35:909–14. doi: 10.1007/s00264-010-1151-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11:452–6. doi: 10.1067/mse.2002.126613. [DOI] [PubMed] [Google Scholar]
- 3.Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;300:127–32. [PubMed] [Google Scholar]
- 4.Neer CS., 2nd Nonunion of the clavicle. J Am Med Assoc. 1960;172:1006–11. doi: 10.1001/jama.1960.03020100014003. [DOI] [PubMed] [Google Scholar]
- 5.Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res. 1968;58:29–42. [PubMed] [Google Scholar]
- 6.Jeray KJ. Acute midshaft clavicular fracture. J Am Acad Orthop Surg. 2007;15:239–48. doi: 10.5435/00124635-200704000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Lazarides S, Zafiropoulos G. Conservative treatment of fractures at the middle third of the clavicle: The relevance of shortening and clinical outcome. J Shoulder Elbow Surg. 2006;15:191–4. doi: 10.1016/j.jse.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 8.Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89:1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 9.Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79:537–9. doi: 10.1302/0301-620x.79b4.7529. [DOI] [PubMed] [Google Scholar]
- 10.Wild LM, Potter J. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg. 2006;88-A:35–40. doi: 10.2106/JBJS.D.02795. [DOI] [PubMed] [Google Scholar]
- 11.Smekal V, Oberladstaetter J, Struve P, Krappinger D. Shaft fractures of the clavicle: Current concepts. Arch Orthop Trauma Surg. 2009;129:807–15. doi: 10.1007/s00402-008-0775-7. [DOI] [PubMed] [Google Scholar]
- 12.McKee MD, Wild LM, Schemitsch EH. Midshaft malunions of the clavicle. J Bone Joint Surg Am. 2003;85-A:790–7. doi: 10.2106/00004623-200305000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD Evidence-Based Orthopaedic Trauma Working Group. Treatment of acute midshaft clavicle fractures: Systematic review of 2144 fractures: On behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19:504–7. doi: 10.1097/01.bot.0000172287.44278.ef. [DOI] [PubMed] [Google Scholar]
- 14.Denard PJ, Koval KJ, Cantu RV, Weinstein JN. Management of midshaft clavicle fractures in adults. Am J Orthop (Belle Mead NJ) 2005;34:527–36. [PubMed] [Google Scholar]
- 15.Smekal V, Irenberger A, Struve P, Wambacher M, Krappinger D, Kralinger FS. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures-a randomized, controlled, clinical trial. J Orthop Trauma. 2009;23:106–12. doi: 10.1097/BOT.0b013e318190cf88. [DOI] [PubMed] [Google Scholar]
- 16.Lenza M, Belloti JC, Gomes Dos Santos JB, Matsumoto MH, Faloppa F. Surgical interventions for treating acute fractures or nonunion of the middle third of the clavicle. Cochrane Database Syst Rev. 2009;7:CD007428. doi: 10.1002/14651858.CD007428.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Assobhi JE. Reconstruction plate versus minimal invasive retrograde titanium elastic nail fixation for displaced midclavicular fractures. J Orthop Traumatol. 2011;12:185–92. doi: 10.1007/s10195-011-0158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hartmann F, Hessmann MH, Gercek E, Rommens PM. Elastic intramedullary nailing of midclavicular fractures. Acta Chir Belg. 2008;108:428–32. doi: 10.1080/00015458.2008.11680255. [DOI] [PubMed] [Google Scholar]
- 19.Jubel A, Andermahr J, Schiffer G, Tsironis K, Rehm KE. Elastic stable intramedullary nailing of midclavicular fractures with a titanium nail. Clin Orthop Relat Res. 2003;408:279–85. doi: 10.1097/00003086-200303000-00037. [DOI] [PubMed] [Google Scholar]
- 20.Frigg A, Rillmann P, Perren T, Gerber M, Ryf C. Intramedullary nailing of clavicular midshaft fractures with the titanium elastic nail: Problems and complications. Am J Sports Med. 2009;37:352–9. doi: 10.1177/0363546508328103. [DOI] [PubMed] [Google Scholar]
- 21.Wijdicks FJ, Houwert M, Dijkgraaf M, de Lange D, Oosterhuis K, Clevers G, et al. Complications after plate fixation and elastic stable intramedullary nailing of dislocated midshaft clavicle fractures: A retrospective comparison. Int Orthop. 2012;36:2139–45. doi: 10.1007/s00264-012-1615-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


